Abstract
Background
Neuromuscular scoliosis is often treated with posterior spinal fusion, with or without anterior release, and either a same-day or staged, 2-day procedure.
Methods
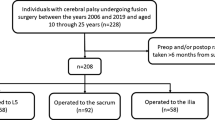
We retrospectively reviewed 222 patients from a prospectively collected, multi-center database of patients with cerebral palsy scoliosis with 2-year follow-up. Baseline characteristics, perioperative, radiographic, and HRQoL measures were compared in six sub-analyses: (1) staged versus same-day surgeries, (2) posterior-only fusion (PSF) versus anterior–posterior spinal fusion (APSF), (3) same-day versus staged PSF, (4) staged versus same-day APSF, (5) same-day PSF versus same-day APSF, (6) staged PSF versus staged APSF.
Results
Staged patients had larger curves and more pelvic obliquity, longer anesthesia and surgical times, longer hospital and ICU stays (p < 0.001), and more days intubated (p = 0.021). The staged PSF group had larger curves (p = 0.006), longer anesthesia (p = 0.020) and surgeries (p = 0.007), hospital (p = 0.009) and ICU stays (p = 0.028) compared to same-day PSF. The staged APSF group had longer hospital (p < 0.001) and ICU stays (p = 0.004) and anesthesia and surgeries (p < 0.001). Same-day APSF was associated with larger curves (p < 0.002), longer anesthesia (p = 0.012) and surgeries (p = 0.042), greater residual curves (p = 0.035), and greater absolute correction (p = 0.007) compared to same-day PSF. The staged APSF group had longer anesthesia times (p < 0.001) compared to the staged PSF group. No sub-analysis revealed significant differences in baseline characteristics, complications, or HRQoL.
Conclusion
Staged and circumferential approaches tend to be used for greater deformity, but were not associated with superior deformity correction, and were associated with longer operative time, hospital stays, ICU stays, and days intubated. However, for the most severe deformity, other patient factors may play more important roles in treatment decisions given that patients treated with a staged PSF or an APSF, whether staged or not, were similar at baseline.
Level of evidence
III.
Graphical abstract
These slides can be retrieved under Electronic Supplementary Material.

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
CP surgery is challenging owing to the large deformity and medical complexity in this population [1,2,3,4]. Staged (i.e., 2-day) surgery is common, but utilization of staged surgery is variable. Both staged and same-day procedures (Figs. 1, 2) yield acceptable deformity correction and may be performed with or without anterior release (Figs. 3, 4) [5,6,7,8]. However, there is debate regarding the utility of and indications for various approaches [5,6,7, 9,10,11].
Anterior approaches have been a common component of surgery for some neuromuscular patients [5, 6]. In recent years, alternative approaches have gained popularity to limit morbidity associated with extensive surgery in a frail population [1, 12, 13]. Some have advocated staged approaches, citing superior correction, lower morbidity, reduced complication rates, and limiting surgeon fatigue [5,6,7]. Yet others have found increased complications, blood loss, and hospital stays with staged compared to same-day procedures [7, 9,10,11].
With this investigation, we seek to evaluate what patient factors are associated with treatment of choice and to compare radiographic, perioperative and health related quality of life (HRQoL) outcomes in patients treated with various strategies, including circumferential and all-posterior approaches, whether same-day or staged. However, due to a paucity of prospective data on staged and anterior/posterior surgery in neuromuscular spinal deformity, we seek to address the following questions:
-
What patient factors may lead surgeons to select a same-day versus staged (2-day) surgical strategy?
-
What patient factors may lead a surgeon to perform an anterior–posterior procedure over a posterior-only fusion?
-
Do these different approaches result in different radiographic, perioperative, and HRQoL outcomes or complication rates?
Methods and materials
A retrospective review of a prospective, multi-center database on spinal deformity associated with cerebral palsy (CP). In total, 222 patients were evaluated. Inclusion criteria were surgical patients with scoliosis secondary to cerebral palsy treated with at least posterior fusion and a minimum 2-year postoperative follow-up. All anterior fusions were performed through an open approach, and anterior instrumentation was used in only three cases. Intraoperative halo traction was utilized in 76 patients (34%). Four of the patients treated with intraoperative traction had staged surgeries (17% of staged patients) and 72 had same-day surgeries (36% of same-day patients). A total of eleven sites and nineteen treating surgeons were involved. All surgical decisions were made at the treating surgeons’ discretion. All surgeries were performed over a 5-year period between 2008 and 2014. All data were collected on a prospective basis using a standardized data collection protocol and transmitted to a central database.
Multiple sub-groups, based on surgical approach and whether the procedures were staged or not, were compared. A total of six sub-analyses were undertaken. The first analysis compared all staged with all same-day patients. The subsequent sub-analyses aim to isolate the potential effects of staging as distinct from the approach (i.e., posterior-only versus circumferential):
-
1.
Same-day versus staged surgery: 222 patients; 199 same-day patients were compared to 23 staged patients.
-
2.
PSF versus APSF: 222 patients; 196 posterior-only patients were compared to 26 anterior/posterior patients.
-
3.
Same-day PSF versus staged PSF: 196 posterior-only patients; 190 same-day patients were compared to 6 staged patients.
-
4.
Same-day APSF versus staged APSF: 26 anterior/posterior patients; 9 same-day patients were compared to 17 staged surgery patients.
-
5.
Same-day PSF versus same-day APSF: 199 same-day patients; 190 posterior-only were compared to 9 anterior/posterior surgery patients.
-
6.
Staged PSF versus staged APSF: 23 staged patients; 6 patients treated posterior-only patients were compared to 17 anterior/posterior surgery patients.
The baseline characteristics, functional status, pre-operative and 2-year follow-up data for health related quality of life (HRQoL) and radiographic measures, and complication rates were compared. Only major complications were considered in our analysis, such as those that had a significant impact on the patients’ hospital course or outcomes, resulted in permanent further disability, risked mortality, or resulted in death or required invasive interventions. These complications included hardware failure, serious infections such as postoperative pneumonia or pancreatitis, as well as the need for invasive procedures, such as insertion tubes and drains or incision and drainage, or additional operations. Minor complications, such as pressure ulcers or superficial infections were not included. The included complications are detailed in Table 1. HRQoL data were collected by use of the Caregiver’s Priorities and Child Health Index of Life and Disabilities (CPCHILD). The CPCHILD questionnaire is a validated and reliable, disease-specific, patient-based outcomes questionnaire for CP and consists of six domains [14].
Standard descriptive summaries (e.g., means and standard deviations for continuous variables such as age and percentage for categorical variables such as gender) were used to summarize demographic variables. Comparisons of categorical variables between groups were made using the Chi-square test or the Fisher’s exact test in the case of a 2 × 2 table with expected count of any cell less than 5. Comparisons of continuous variables were completed using analysis of variance (ANOVA) or nonparametric tests depending on normality of distribution and homogeneity of variances. Alpha was set at p < 0.05 to declare significance. Statistics were performed utilizing SPSS v.24 (IBM Corp. Released 2016. IBM SPSS Statistics for Windows, Version 24.0. Armonk, NY: IBM Corp.)
Results
Baseline characteristics, HRQOL, and complications
Table 2 summarizes the baseline characteristics of age, gender, GMFCS level, seizure status, feeding status, pre-operative total protein and albumin levels, for each sub-analysis. None revealed a statically significant difference between any of the sub-groups. Overall, 105 (47.3%) of the patients in the sample were female and the average age of the entire sample was 14.2 years. 200 (93.9%) patients were GMFCS level IV or V, and 151 (68%) patients had seizures. The average total protein was 10.7 g/dL, and the average albumin was 6.74 g/dL (overall results not shown). Additionally, there were no significant differences between groups in any of the sub-analysis in terms of HRQOL outcomes, summarized in Table 3. We did not identify any differences in rates of complications among any of the sub-analyses. The comparisons of complications rates are summarized in Table 4.
Analysis 1: Same-day versus staged surgeries
Overall, 222 patients were included in this analysis. There were 199 same-day patients and 23 staged patients. Staged patients had larger curves (109.1° vs. 79.6°, p < 0.001) and more pelvic obliquity (POB) (40° vs. 26.8°, p < 0.001). Both groups had similar flexibility (36.9% vs. 29.4%, p = 0.086).
At 2-year follow-up, staged patients had larger deformity (36.6° vs. 28.8°, p = 0.021), more absolute correction for Cobb angle (72.5° vs. 50.9°, p < 0.001), but similar percent correction and POB. Staged patients have larger absolute pelvic obliquity correction (30.1° vs. 19.4°, p = 0.009), though percent correction was similar.
Staged patients also had longer anesthesia (862 vs. 468 min, p < 0.001) and surgical times (687 vs. 385 min, p < 0.001), hospital (21.7 vs. 11.5 days, p < 0.001) and ICU length of stay (10.0 vs. 5.3 days, p < 0.001), and days intubated (4.5 vs. 2.7 days, p = 0.021). There was similar EBL, cell saver transfused, and RBCs transfused (Table 5).
Analysis 2: Posterior-only versus anterior/posterior surgery
Overall, 222 patients were included in this analysis. There were 196 PSF patients and 26 APSF patients. The anterior/posterior group had more severe deformity with larger initial Cobb angles (110.4° vs. 79.0°, p < 0.001) and pelvic obliquity (37.1° vs. 29.6°, p = 0.004), though the curves had similar flexibility (29.6% vs. 37.1%, p = 0.068).
At 2-year follow-up, APSF patients also had larger residual deformity (37.7° vs. 28.5°, p = 0.004), but had greater absolute deformity correction (72.6° vs. 50.6°, p < 0.001). Although percent correction was similar (66% vs. 63%, p = 0.458), both groups had similar residual POB (11.2° vs. 7.6°, p = 0.059), absolute correction (25.7° vs. 19.7°, p = 0.114), and percent correction of POB (61% vs. 58.7%, p = 0.896).
Anterior/posterior patients had longer anesthesia (828 vs. 466 min, p < 0.001) and surgical times (637 vs. 385 min, p < 0.001), hospital (17.8 vs. 11.9 days, p < 0.001) and ICU stays (8.6 vs. 5.4 days, p < 0.020), but similar number of days spent intubated (3.9 days vs. 2.7 days, p = .055). Both groups had similar EBL (1777 cc vs. 2016 cc, p = 0.387), cell saver transfused (432 cc vs. 488, p = 0.606), and RBCs transfused (962 cc vs. 1160 cc, p = 0.345) (Table 5).
Analysis 3: Same-day PSF versus staged PSF
Overall, 196 patients were included in this analysis. There were 190 same-day PSF patients and 6 staged PSF patients. The staged group had larger initial Cobb angles (103° vs. 78.2°, p = 0.006), but similar flexibility, and pelvic obliquity.
At 2-year follow-up both groups had similar major curves, absolute correction, and percent correction. The staged group had larger residual pelvic obliquity (11.7° vs. 7.51°, p = 0.049), but similar absolute correction, and percent correction.
The staged group had longer hospital (21.5 vs. 11.9 days, p = 0.009) and ICU length of stay (7.8 vs. 5.3 days, p = 0.028), but similar days intubated. The staged group had longer anesthesia (586 vs. 462 min, p = 0.020) and surgical times (524 vs. 381 min, p = 0.007). Both groups had similar EBL, cell saver transfused, and RBCs (Table 5).
Analysis 4: Same-day APSF versus staged APSF
Overall, 26 patients were included in this analysis. There were 9 same-day APSF patients and 17 staged APSF patients. There was no significant difference between groups for major curve size, curve flexibility, or POB. At 2-year follow-up, there was no significant difference in all radiographic measures.
The staged group had longer hospital (21.8 vs. 9.1 days, p < 0.001) and ICU length of stay (10.7d vs. 4.3 days, p = 0.004), but similar days intubated did not reach statistical significance. The staged group had longer anesthesia (595 vs. 961 min, p < 0.001) and surgical times (464 vs. 741 min, p < 0.001). There was no significant difference total EBL, cell saver transfused, and RBCs (Table 5).
Analysis 5: Same-day PSF versus same-day APSF
Overall, 199 patients were included in this analysis. There were 190 same-day PSF patients and 9 same-day APSF patients. The APSF group had larger pre-operative major Cobb angles (108.7° vs. 78.2°, p = 0.002), but no significant difference in flexibility or pelvic obliquity.
At 2-year follow-up the APSF group had greater residual coronal deformity (39.2° vs. 28.3°, p = 0.035) and greater absolute correction (69.4° vs. 50.1°, p = 0.007). There were no significant differences in percent coronal correction, residual pelvic obliquity, absolute correction, and percent correction of pelvic obliquity.
The APSF group had longer anesthesia (595 vs. 462 min, p = 0.012) and surgical times (464 vs. 381 min, p = 0.042). There were no significant differences in total EBL, cell saver transfused, RBCs transfused, hospital length of stagy, ICU days, or days intubated (Table 5).
Analysis 6: Staged PSF versus staged APSF
Overall, 23 patients were included in this analysis. There were 6 staged PSF patients and 17 staged APSF patients. There was no significant difference between groups for major curve size, curve flexibility, or pelvic obliquity. At 2-year follow-up there was no significant difference in all radiographic measures.
The APSF group had longer anesthesia times (961 vs. 586 min, p < 0.001); however, the differences in surgical times did not reach significance (741 vs. 524 min, p = 0.066). There was no significant difference in total EBL, cell saver transfused, RBCs transfused, hospital length of stagy, ICU days, or days intubated (Table 5).
Discussion
A staged approach was traditionally advocated for neuromuscular scoliosis in an effort to limit the morbidity from an anterior and posterior approach attempted in a single, extensive operation [7]. More recently, there has been controversy over whether a same-day or a staged approach produces the optimal results with the least morbidity [5, 7, 9,10,11]. While the utility of an anterior approach has been questioned in recent literature, some argue that an anterior release may be required in particularly large, stiff or short angle curves, or those with hyperlordosis [1, 8, 15,16,17,18,19,20].
Our results indicate surgeons were more likely to pursue a staged approach for larger magnitude curves and pelvic obliquity (Table 5: Analysis 1). For posterior-only approaches, the staged patients overall had larger curves (103° vs. 78.2°, p = .006) and more POB (41° vs. 26.6°, p = 0.069) than their non-staged counterparts, although the difference in POB did not reach statistical significance (Table 5: Analysis 3). On the other hand, when evaluating only APSF patients, there was not a significant difference in curve magnitude between staged and same-day patients, as patients who were treated with anterior release had average coronal deformity > 100° and POB of > 30°, regardless if staged or same-day (Table 5: Analysis 4). Additionally, the average deformity in the staged patients was also > 100 degrees and POB of approximately 40 degrees, regardless if treated with PSF or APSF (Table 5: Analysis 6). This finding may indicate that factors other than deformity may play important roles in decision-making for patients with the worst deformity. Additionally, three of the staged procedures were unplanned and converted to staged procedures in response to unforeseen intraoperative complications. The operation was aborted and subsequently completed as a staged procedure for excessive blood loss, suspected anaphylactic reaction to blood products, and cardiac arrhythmia, respectively, in these three patients.
Our results have corroborated previous series showing that staged cases are associated with longer hospitalizations and longer ICU stays [7, 9, 11]. We also demonstrate that staged approaches were associated with longer operative times. This was found even when the groups were stratified by approach, implying that the extra operative time is primarily staging the procedure and not just from the added complexity of the anterior portion of the case (Table 5: analysis 4 and 6). However, even with overall longer operative times, considerations for surgeon stamina and fatigue prevention, as well as patient concerns about hemodynamic stability and coagulopathy, may sway surgeons toward returning for a second day of surgery [7]. Conversely, these considerations should be balanced against the additional costs to families and the healthcare system for the prolonged operations and hospitalization, such as costly ICU stays. Furthermore, potential harm from prolonged operations and hospitals stays should be balanced against potential harm resulting from surgeon and surgical team fatigue.
Furthermore, the benefits of a staged procedure are unclear, from deformity correction or HRQoL standpoint. When evaluating only patients with an anterior approach, staged procedures were associated with prolonged hospital stays and operative times, but not with improved deformity correction, despite the deformity being similar at baseline (Table 5: Analysis 4). Additionally, when controlling for staged procedures these data suggest no increase in deformity correction with anterior release, despite similar pre-operative and postoperative deformity and curve rigidity (Table 5: Analysis 6). However, these results are limited by a small sample size of staged PSF patients, some of who had an unplanned staged procedure.
Other retrospective series show no increase in correction from anterior approaches [8, 13, 16]. In a cohort of non-ambulatory, spastic quadriplegic CP patients all treated with intraoperative halo traction, Keeler et al. retrospectively compared PSF to APSF and found that the APSF group had longer operations (6.1 h compared to 10.3 h), more EBL (873 cc compared to 1361 cc) and more pulmonary complications, but similar radiographic outcomes [13]. There was no difference in pre-operative or postoperative Cobb angle, deformity correction, pelvic obliquity, or C7 plumb line [13]. However, this was in a cohort of patients who were all treated with the use of intraoperative halo traction, whereas only 34% of our patients had intraoperative traction. Given the medically frail nature of NMS patients, alternatives to an anterior approach have been advocated, including vertebral column resections (VCR), pre- and intraoperative halo traction, and osteotomies [1, 4, 9, 10, 13, 15, 21]. For patients in whom halo-gravity traction is contraindicated, such as patients with cervical instability, fixed cervical kyphosis [22], stenosis, hip flexion contractures, temporary internal distraction rods may be a viable alternative [23]. A review of ten children, with average Cobb angles of 104°, the use of internal distraction rods was associated with 80% deformity correction with no neurological deficits or infections [23].
Other retrospective studies have found anterior and staged approaches to increase complications [9, 11, 16], we found no difference in major complication rate between any of the sub-groups. Ferguson et al. found a 124% complication rate in staged patients compared to 88% complication rate in the same-day group (63% and 35% of patients having a major or minor complication, respectively [9]. However, they did find higher reintubation rates and pulmonary complications in the same-day group [9]. The staged group also had longer hospital stays, longer operative times, increased blood loss and transfusions, and decreased nutritional parameters [9]. Nishnianidze et al. found that patients with feeding tubes had higher rates of complications [24]. However, we did not find a higher rate of complications among patients with feeding tubes. Furthermore, there were no significant differences in the proportion of patients with feeding groups in any of our sub-analyses. Overall, our prospective study did not find significant differences in complication rates, implying that same-day procedures may be just as safe as staged procedures. Patients staying in hospital in anticipation of the second surgery may explain the difference in overall hospital length of stay, as well as ICU stay. Additional detail regarding the nature of the complications can be found in Table 1.
Limitations of our study include the non-randomized nature of the methodology. There may be increased variability in the data given differences in specific protocols used by the individual treating surgeons and centers included in the study. However, the inclusion of diversity may increase the generalizability of our findings. The use of any supplementary techniques, such as VCR, osteotomies, or halo traction, may confound the results. Additional factors, such as patient physiology, familiarity and skill of the post-op care team, or level of training of the first assistant may play a more important role than the degree or type of deformity in treatment decisions, particularly in the most severe curves. Further prospective studies may help control for those differences and further analyze which cases should be staged or performed as a single procedure and which patients would benefit most from the addition of an anterior approach.
The complexity of neuromuscular scoliosis and the litany of available treatment options compound the difficulty of therapeutic decision-making. There is little consensus concerning the determination to utilize a staged and/or combined circumferential approach or not. While a surgeon may consider a wide range of factors in these decisions, it seems that magnitude of deformity plays an important role. A same-day, posterior-only approach seems to be reserved for patients with relatively less severe deformity. However, it appears that there is much overlap in patients treated with staged, 2-day procedures and/or anterior releases. Given the similarities in baseline characteristics and radiographic measures for these most severe cases it appears that factors other than just radiographic parameters may be of greater importance when deciding between surgical options. In these most severe cases, it is not clear whether staged or anterior approaches produce superior deformity correction over same-day or posterior-only approaches.
Based on the results, no definitive recommendations can be made for which cases should or should not be staged or utilize an anterior approach in addition to an instrumented spinal fusion. The authors suggest that those patients who are low demand (GMFCS V, severe cognitive impairment, etc.) may be better served with a single-stage procedure. Conversely, those patients in whom large deformity is present and maximizing curve correction is more of a priority, a staged procedure may justify the additional burden of care (increased length of hospitalization, ICU stay, etc.). The best course of action is even less clear for patients with the most severe deformity, and improved understanding of the indications for staged and anterior approaches may help better target the patients who stand to benefit most, and limit unnecessary medicalization.
References
Hasler CC (2013) Operative treatment for spinal deformities in cerebral palsy. J Child Orthop 7:419–423
Vialle R, Thevenin-Lemoine C, Mary P (2013) Neuromuscular scoliosis. Orthop Traumatol Surg Res 99:S124–S139
Piazzolla A, Solarino G, De Giorgi S, Mori CM, Moretti L, De Giorgi G (2011) Cotrel–Dubousset instrumentation in neuromuscular scoliosis. Eur Spine J 20(Suppl 1):S75–S84. https://doi.org/10.1007/s00586-011-1758-x
Brown JC, Swank S, Specht L (1982) Combined anterior and posterior spine fusion in cerebral palsy. Spine 7:570–573
Tsirikos AI, Chang W-N, Dabney K, Miller F (2003) Comparison of one-stage versus two-stage anteroposterior spinal fusion in pediatric patients with cerebral palsy and neuromuscular scoliosis. Spine 28:1300–1305
Comstock CP, Leach J, Wenger DR (1998) Scoliosis in total-body-involvement cerebral palsy: analysis of surgical treatment and patient and caregiver satisfaction. Spine 23:1412–1424
O’Brien T, Akmakjian J, Ogin G, Eilert R (1992) Comparison of one-stage versus two-stage anterior/posterior spinal fusion for neuromuscular scoliosis. J Pediatr Orthop 12:610
Luhmann SJ, Lenke LG, Kim YJ, Bridwell KH, Schootman M (2005) Thoracic adolescent idiopathic scoliosis curves between 70 degrees and 100 degrees: is anterior release necessary? Spine (Phila Pa 1976) 30:2061–2067
Ferguson RL, Hansen MM, Nicholas DA, Allen BL Jr (1996) Same-day versus staged anterior-posterior spinal surgery in a neuromuscular scoliosis population: the evaluation of medical complications. J Pediatr Orthop 16:293–303
Gum JL, Lenke LG, Bumpass D, Zhao J, Sugrue P, Karikari I, Rahman R, Carreon LY (2016) Does planned staging for posterior-only vertebral column resections in spinal deformity surgery increase perioperative complications? Spine Deform 4:131–137. https://doi.org/10.1016/j.jspd.2015.08.005
Passias PG, Ma Y, Chiu YL, Mazumdar M, Girardi FP, Memtsoudis SG (2012) Comparative safety of simultaneous and staged anterior and posterior spinal surgery. Spine (Phila Pa 1976) 37:247–255. https://doi.org/10.1097/BRS.0b013e31821350d0
Reames DL, Smith JS, Fu K-MG, Polly DW Jr, Ames CP, Berven SH, Perra JH, Glassman SD, McCarthy RE, Knapp RD Jr (2011) Complications in the surgical treatment of 19,360 cases of pediatric scoliosis: a review of the Scoliosis Research Society Morbidity and Mortality database. Spine 36:1484–1491
Keeler KA, Lenke LG, Good CR, Bridwell KH, Sides B, Luhmann SJ (2010) Spinal fusion for spastic neuromuscular scoliosis: is anterior releasing necessary when intraoperative halo-femoral traction is used? Spine (Phila Pa 1976) 35:E427–E433. https://doi.org/10.1097/BRS.0b013e3181d9527e
Bowen RE, Abel MF, Arlet V, Brown D, Burton DC, D’Ambra P, Gill L, Hoekstra DV, Karlin LI, Raso J (2012) Outcome assessment in neuromuscular spinal deformity. J Pediatr Orthop 32:792–798
Modi HN, Hong JY, Mehta SS, Srinivasalu S, Suh SW, Yi JW, Yang JH, Song HR (2009) Surgical correction and fusion using posterior-only pedicle screw construct for neuropathic scoliosis in patients with cerebral palsy: a three-year follow-up study. Spine (Phila Pa 1976) 34:1167–1175. https://doi.org/10.1097/BRS.0b013e31819c38b7
Suk SI, Kim JH, Cho KJ, Kim SS, Lee JJ, Han YT (2007) Is anterior release necessary in severe scoliosis treated by posterior segmental pedicle screw fixation? Eur Spine J 16:1359–1365. https://doi.org/10.1007/s00586-007-0334-x
Zhang HQ, Wang YX, Guo CF, Tang MX, Chen LQ, Liu SH, Wang YF, Chen J (2011) Posterior-only surgery with strong halo-femoral traction for the treatment of adolescent idiopathic scoliotic curves more than 100°. Int Orthop 35:1037–1042. https://doi.org/10.1007/s00264-010-1111-8
Shi Z, Chen J, Wang C, Li M, Li Q, Zhang Y, Li C, Qiao Y, Kaijin G, Xiangyang C, Ran B (2015) Comparison of thoracoscopic anterior release combined with posterior spinal fusion versus posterior-only approach with an all-pedicle screw construct in the treatment of rigid thoracic adolescent idiopathic scoliosis. J Spinal Disord Tech 28:E454–E459. https://doi.org/10.1097/BSD.0b013e3182a2658a
Tokala DP, Lam KS, Freeman BJ, Webb JK (2007) Is there a role for selective anterior instrumentation in neuromuscular scoliosis? Eur Spine J 16:91–96. https://doi.org/10.1007/s00586-006-0105-0
Lonstein JE, Koop SE, Novachek TF, Perra JH (2012) Results and complications after spinal fusion for neuromuscular scoliosis in cerebral palsy and static encephalopathy using luque galveston instrumentation: experience in 93 patients. Spine (Phila Pa 1976) 37:583–591. https://doi.org/10.1097/BRS.0b013e318225ebd5
Takeshita K, Lenke LG, Bridwell KH, Kim YJ, Sides B, Hensley M (2006) Analysis of patients with nonambulatory neuromuscular scoliosis surgically treated to the pelvis with intraoperative halo-femoral traction. Spine (Phila Pa 1976) 31:2381–2385. https://doi.org/10.1097/01.brs.0000238964.73390.b6
Dove J, Hsu LC, Yau AC (1980) The cervical spine after halo-pelvic traction. An analysis of the complications of 83 patients. J Bone Joint Surg Br 62-B:158–161
Buchowski JM, Bhatnagar R, Skaggs DL, Sponseller PD (2006) Temporary internal distraction as an aid to correction of severe scoliosis. J Bone Joint Surg Am 88:2035–2041. https://doi.org/10.2106/JBJS.E.00823
Nishnianidze T, Bayhan IA, Abousamra O, Sees J, Rogers KJ, Dabney KW, Miller F (2016) Factors predicting postoperative complications following spinal fusions in children with cerebral palsy scoliosis. Eur Spine J 25:627–634. https://doi.org/10.1007/s00586-015-4243-0
Acknowledgements
Research grants from DePuy Synthes Spine and from K2M to Setting Scoliosis Straight Foundation for Harms Study Group research efforts were received in support of this work.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
Disclosures relevant to submitted: Grant from the Setting Scoliosis Foundation, with research grants from DePuy Synthes Spine and K2M in support of Harms Study Group research. Disclosures outside of submitted: Consultancy/Personal fee—DePuy Synthes Spine, DePuy Synthes Canada, Cubist, K2M, Ellipse Technologies Inc., NuVasive, Medtronic Inc., Orthopediatrics, Stryker, Globus Medical; Royalties—DePuy Synthes Spine, Thieme Publishing, K2M; Investments/Options—Electrocore; Board membership—Setting Scoliosis Straight Foundation, Rady Children’s Specialists, AAOS, Scoliosis Research Society, International Pediatric Orthopedic Think Tank, Cubist, POSNA; Editorial Boards—JBJS-American, Spine Deformity; Other Financial/Research/Institutional Support—DePuy Synthes Spine, EOS Imaging, NuVasive, Orthopediatrics, K2M, Alphatech, Medtronic Inc. Patents/Product Development—DePuy Synthes Spine, Inc., K2M.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Jackson, T., Yaszay, B., Sponseller, P.D. et al. Factors associated with surgical approach and outcomes in cerebral palsy scoliosis. Eur Spine J 28, 567–580 (2019). https://doi.org/10.1007/s00586-018-5745-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-018-5745-3