Abstract
Purpose
To describe normal variations in sagittal spinal radiographic parameters over an interval period and establish physiological norms and guidelines for which these images should be interpreted.
Methods
Data were prospectively collected from a continuous series of adult patients with first-episode mild low back pain presenting to a single institution. The sagittal parameters of two serial radiographic images taken 6-months apart were obtained with the EOS® slot scanner. Measured parameters include CL, TK, TL, LL, PI, PT, SS, and end and apical vertebrae. Chi-squared test and Wilcoxon Signed Rank test were used to compare categorical and continuous variables, respectively.
Results
Sixty patients with a total of 120 whole-body sagittal X-rays were analysed. Mean age was 52.1 years (SD 21.2). Mean interval between the first and second X-rays was 126.2 days (SD 47.2). Small variations (< 1°) occur for all except PT (1.2°), CL (1.2°), and SVA (2.9 cm). Pelvic tilt showed significant difference between two images (p = 0.035). Subgroup analysis based on the time interval between X-rays, and between the first and second X-rays, did not show significant differences. Consistent findings were found for end and apical vertebrae of the thoracic and lumbar spine between the first and second X-rays for sagittal curve shapes.
Conclusions
Radiographic sagittal parameters vary between serial images and reflect dynamism in spinal balancing. SVA and PT are predisposed to the widest variation. SVA has the largest variation between individuals of low pelvic tilt. Therefore, interpretation of these parameters should be patient specific and relies on trends rather than a one-time assessment.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
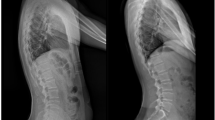
Weight-bearing, lateral whole-body X-rays are increasingly performed for the evaluation of spinal deformity [1, 2]. This is made possible with the advent of EOS® slot scanning technology which produces true-to-proportion and true-to-dimension images for the accurate assessment of whole-body alignment [3]. Although a recent study showed the reproducibility of these images performed serially in patients with adolescent idiopathic scoliosis (AIS) [4], little is known of its reproducibility in adult patients.
Image reproducibility is dependent on several factors including (1) the condition of the patient, (2) the way that they were instructed to stand, and (3) the normal physiological variations. Assuming that the first two factors are controlled for, understanding of the physiological variations in sagittal spinal alignment is crucial when interpreting these images. Knowledge of these variations may influence that the way patients are managed [4,5,6].
Therefore, the aim of this study is to describe variations in sagittal spinal radiographic parameters within a relatively short period of 6 months, in adult patients with low back pain, using serial images obtained by the EOS slot scanner. This will establish reference norms and allow differentiation between patients that have progressive spinal deformity and those that do not.
Materials and methods
Study design
This was a longitudinal study which reviewed prospectively collected data looking at the variability of serial whole-body lateral radiographs in a continuous series of adult patients presenting with mild, low back pain from a single institution.
With reference to the previous similar studies which looked at radiographic alignment differences within the same individual [4, 7, 8], and a pilot data of 10 patients, a post hoc power analysis was performed with an alpha of 0.05 and a beta of 80. To detect a clinically significant difference in SVA of 2 cm, lumbar lordosis (LL), and pelvic tilt of 5° each, a total of 60 patients were deemed necessary.
Approval by the local ethics board committee was obtained prior to commencing the study.
Patient cohort
The study recruited a continuous series of patients who presented with the first episode of mild low back pain [visual analogue scale (VAS) of < 3] which lasted less than 3 months. Patients who have had any previous spinal intervention or obvious spinal deformities, as well as those with clinical features that suggest a traumatic, infective, or malignant spine condition involving both bony or soft tissue structures were excluded for this study. Patients who have contraindications for radiographs due to proven or suspected pregnancy are also excluded from the study.
The choice of patients with mild low back pain instead of asymptomatic volunteers is twofold. First, it gives clinical relevance to the study. Second, we considered that it would not be ethical to perform serial imaging in asymptomatic volunteers just to observe variations in radiographic parameters. This careful choice of healthy individuals with mild low back pain (VAS < 3), therefore, reflects our best efforts to provide clinically useful information while minimising negative effects on the validity of the results. There should not be any new symptoms or signs between serial imaging.
Methodology
A detailed clinical assessment was conducted for all patients and pertinent information such as age and gender was collected. In addition, each patient had two whole-body lateral radiographs taken. Lateral imaging was repeated again within 6 months of follow-up for all patients based on clinical protocol. The choice of this duration was also to reduce the likelihood of substantial progression of any existing spinal condition if present. A follow-up rate of 100% was achieved.
Radiographic examination
All imaging were performed using an EOS® slot scanner (EOS® imaging, Paris, France) [3], which obtains true-to-proportion and true-to-dimension images in the lateral view.
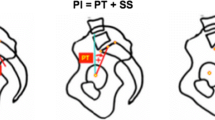
Pictorial charts demonstrating how to stand (Fig. 1a) were available next to the EOS® machine to allow better standardization. This was further reinforced through standardized verbal instructions given by the radiographer. Patients were instructed to “keep [their] eyes horizontal and look straight ahead, stand as straight as possible without leaning forwards or backwards, and touch [their] collar bones with [their] fingers”.
All images were taken by trained radiographers with more than 2 years of experience using EOS® technology. Radiographs were then stored in the hospital’s server and accessed using Centricity Enterprise Web V3.0 (8.0.1400.128) (GE Medical Systems Information Technologies, Barrington, IL, USA) for measurement of spinal parameters.
Radiographic measurements
Sagittal radiographic parameters measured include cervical lordosis (CL), thoracic kyphosis (TK), thoracolumbar angle (TL), lumbar lordosis (LL), sagittal vertical axis (SVA), standard spinopelvic parameters—pelvic incidence (PI), pelvic tilt (PT), and sacral slope (SS), as well as end and apical vertebrae.
CL was measured by the Harrison posterior tangent method using C2 and C7. All other sagittal curves were measured using the Cobb method. TK was measured from the inferior endplate of C7 to the inferior endplate of T12. TL was measured from the superior endplate of T11 to the inferior endplate of L2. LL was measured from the inferior endplate of T12 to the superior endplate of S1. Sagittal vertical axis (SVA) was recorded as the horizontal distance between the posterosuperior corner of S1 and the C7 plumbline. End and apical vertebrae were taken as the most tilted and most horizontally displaced vertebrae on the sagittal profile of each curve, respectively [9]. PI, PT, and SS were measured using the standard methods described in the literature [10].
A lateral radiograph on how spinal parameters—SVA (blue), T1–T12 (purple), TL (red), and LL (yellow) markings—were measured is shown in Fig. 1b. All measurements were made by two independent fellowship-trained, practising orthopaedic specialists and an average of their readings was recorded.
Statistical analyses
All categorical variables are described as frequencies with percentages and continuous variables as means with the standard deviations. Baseline characteristics of all patients are shown in Table 1. Statistical package for the social sciences (SPSS) version 24.0 was used to analyse the data. Significance was set at p < 0.05 as per power calculation.
Comparisons between sagittal radiographic parameters were performed using the Chi-squared test and Wilcoxon Signed Rank test for categorical and continuous variables, respectively. Similar tests were repeated after stratification of patients into those who have had interval imaging less than 3 months apart versus those who had interval imaging more than 3 months apart, as well as between first and second radiographs, to ascertain potential confounders.
Results
Sixty patients (28 males and 32 females) participated in the study and a total of 120 whole-body sagittal X-rays were analysed. Their mean age was 52.1 years (SD 21.2). The first and second X-rays were taken at a mean of 126.2 days (SD 47.2) apart. All measurements achieved high inter- and intra-class correlation coefficients of 0.95 and 0.98, respectively. Table 1 shows the baseline characteristics of all patients and X-rays taken. The mean pelvic incidence of this group was 46.6° (SD 12.3) and their corresponding lumbar lordosis was 42.18° (SD 15.6). The mean values of SVA, PT, and T1 slope were − 19 mm (SD 31.7), 18.26° (SD 9.1), and 22.85° (SD 10.4), respectively.
Collating the radiographic parameters, small variations (< 1°) occur for all except pelvic tilt (PT) (1.2°), C2–T1 alignment (1.2°), and SVA (2.9 cm) (Table 2). When comparing the means of both X-rays, only pelvic tilt showed borderline significant difference between both images (p = 0.035). This was an isolated finding.
Subgroup analysis based on the time interval between X-rays showed only borderline significance in SVA for patients with X-rays taken < 3 months apart (p = 0.056) and near significance in PT for patients with X-rays taken 3–6 months apart (p = 0.085) (Table 3).
In terms of the sagittal curve shapes, consistent findings were found for the end and apical vertebrae of the thoracic and lumbar spine between the first and second X-rays (Table 4).
Discussion
Health-related quality-of-life scores are closely influenced by sagittal spinal alignment (SVA) [11, 12]. Specifically, loss of normal alignment and consequentially body imbalance result in poor patient reported outcomes scores (PROs) [11, 13,14,15]. This realisation has driven adult spinal deformity corrective surgeries which are increasingly practised today [11, 14, 16,17,18]. The key radiographic parameters to restore include lumbar lordosis [17], which should match one’s unique pelvic incidence (PI) [10], and a normal SVA [17]. These results are often accompanied by a reduction in pelvic tilt [17] which reflects resolution of spinopelvic compensation [16].
The basis of sagittal deformity corrections has to rely on the accurate assessment of sagittal alignment, which is in turn dependent on good imaging and consistent patient posturing. Recent studies have shown the possibility of postural variations in standing for patients with adolescent idiopathic scoliosis (AIS). These results suggest that similar inconsistencies may also occur in adult patients over a short span of time during serial imaging [4, 8]. It is, therefore, important to establish reference norms for common radiographic sagittal parameters, such that appropriate clinical decisions can be based on. Large variations within each individual, if found, will prompt the need to rely on trends following multiple assessments rather than a single assessment.
Our study showed that small mean variations (< 1°) occur within individuals for all sagittal radiographic parameters with the exception of pelvic tilt (PT) (1.2°), C2–T1 alignment (1.2°), and SVA (2.9 cm). These findings highlight the reliability of imaging, but at the same time suggest the dynamic nature of PT and SVA. Standing sagittal balance is a dynamic, self-adjusting, and continuous process which involves various physiological mechanisms such as visual, vestibular, proprioception, and neuromuscular systems [19]. It is, therefore, not surprising to have inconsistent radiographic parameter readings during radiograph snapshots. SVA being the final global marker of balance [11], cervical alignment being a highly variable parameter dependent on both caudal spine alignment and horizontal gaze [7], and PT being the most versatile mechanism in spinopelvic compensation linked to the mobile hip joint, thus demonstrate the greatest variation [16, 20].
Compared to a similar study performed by Hey et al. [4] in patients with adolescent idiopathic scoliosis (AIS), this study did not show a predictable difference in radiographic parameters between the first and second X-rays performed serially. Hey et al. [4] mentioned that the second X-ray has a higher tendency to show a more negative SVA, larger TK, smaller LL, and higher PT, representing a form of relaxed standing posture. We believe that the differences could be due to two reasons: (1) the posture described by Hey et al. uses ligament to achieve balance while conserving energy; potential ligament laxity may predispose AIS patients to stand in this posture to achieve full ligament stretch which may not be seen in our population comprising normal individuals of all age groups and (2) most patients in the study by Hey et al. [4] had serial images performed 1 day apart; this may have conditioned the patients to stand in a more relaxed posture. In our study, images are performed within 6 months apart. It is, therefore, unlikely for the second image to be confounded by the first image. Our subgroup analysis of patients with imaging performed 3 months apart also did not show any significant differences in these radiographic parameters.
Similar to coronal deformity, spinal alignment morphology should be described based on curve magnitudes and forms. The assessment of sagittal profile of the spine should include end and apical vertebrae [8]. Under the Roussouly classification [21], different natural curve types have been shown. This ranges from type-1 curves which have a short lordotic segment and a more caudally located thoracolumbar inflexion points, to type-4 curves with a longer lordotic segment and more cranially located thoracolumbar inflexion points. It has been proposed that correction of sagittal deformity should also consider these radiographic findings [8, 22]. In our study, no difference was found for the end and apical vertebrae between images.
Large standard deviations are observed in most of the radiographic parameters particularly SVA (mean = 19.0 mm, SD = 31.7 mm). In the presence of low PT (mean = 18.3°, SD = 9.1°) signifying a balanced spine [11], this suggests that normal SVA falls within a wide range [2, 11, 21, 23]. Coupled with the finding that SVA varies substantially within each individual (mean = 2.9 cm), treatment strategies based on SVA should be patient-specific and rely on readings at multiple timepoints. In fact, SVA has been shown to vary also with the patient’s activities such as after prolonged standing [1] or exertion [24]. These phenomena reflect the importance of postural muscles in maintaining sagittal spinal imbalance [24] and may account for the variations in SVA and PT seen in different individuals during dynamic balancing.
There are several limitations to this study. First, the interval between serial X-rays ranges up to 6 months. This could allow, though unlikely, sufficient time for substantial degeneration to set. As such, only patients with no obvious spinal deformities are involved in the study. It may also be argued that patients’ symptoms may have changed during this period. However, we have attempted to address this issue by (1) including only patients with low back pain (VAS < 3), (2) ensuring that all patients were able to position themselves comfortably for both imaging processes, and (3) stratified analysis of patients with < 3 or 3–6 months of interval imaging. Second, the sample size is relatively small and may not be able to show a difference between the first and second X-rays. While several results showed borderline significance, they do not follow any known trends and are, therefore, more likely to be false positives. Moreover, the clinically observable differences in these parameters appear small, hence reducing their relevance. Future studies should be performed prospectively and on larger groups of patients to confirm our findings. The concepts derived from this study if applied to patients with true adult spinal deformity should also be done with caution.
In conclusion, this is the first study to compare serial whole-body sagittal alignment images in adults taken using the EOS® Slot Scanning Technology, which represents the current gold standard modality [25]. Radiographic sagittal parameters vary between serial images, which are likely a reflection of the dynamism in spinal balancing. Of all parameters, SVA and PT are predisposed to the widest physiological variation. SVA is also shown to have the largest variation between individuals of low pelvic tilt suggesting a wide range of normality. Considering the aforementioned findings, interpretation of these parameters, if in doubt, should be patient-specific and rely on trends rather than a one-time assessment. The dynamism of the spine, which must be appreciated prior to spinal realignment surgeries, should also be investigated using snapshot images taken in key postures rather than relying on a single standing image.
References
Roussouly P, Nnadi C (2010) Sagittal plane deformity: an overview of interpretation and management. Eur Spine J 19(11):1824–1836
Berthonnaud E, Dimnet J, Roussouly P, Labelle H (2005) Analysis of the sagittal balance of the spine and pelvis using shape and orientation parameters. J Spinal Disord Tech 18(1):40–47
EOS Imaging. http://www.eos-imaging.com/us/homepage-6.html. Accessed 2 Apr 2017
Hey HW et al (2017) Reproducibility of sagittal radiographic parameters in adolescent idiopathic scoliosis-a guide to reference values using serial imaging. Spine J 17(6):830–836. https://doi.org/10.1016/j.spinee.2017.01.001
Iyer S et al (2016) Variations in sagittal alignment parameters based on age: a prospective study of asymptomatic volunteers using full-body radiographs. Spine (Phila Pa 1976) 41(23):1826–1836
Le Huec JC, Demezon H, Aunoble S (2015) Sagittal parameters of global cervical balance using EOS imaging: normative values from a prospective cohort of asymptomatic volunteers. Eur Spine J 24(1):63–71
Hey HW et al (2017) Cervical alignment variations in different postures and predictors of normal cervical kyphosis—a new understanding. Spine (Phila Pa 1976) 42(21):1614–1621
Hey HW et al (2016) How the spine differs in standing and in sitting-important considerations for correction of spinal deformity. Spine J 17(6):799–806
Scoliosis Research Society. Revised glossary of terms. https://www.srs.org/professionals/online-education-and-resources/glossary/revised-glossary-of-terms. Accessed 13 Mar 2017
Legaye J, Duval-Beaupere G, Hecquet J, Marty C (1998) Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J 7(2):99–103
Lafage V, Schwab F, Patel A, Hawkinson N, Farcy JP (2009) Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine (Phila Pa 1976) 34(17):E599–E606
Roguski M et al (2014) Postoperative cervical sagittal imbalance negatively affects outcomes after surgery for cervical spondylotic myelopathy. Spine (Phila Pa 1976) 39(25):2070–2077
Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F (2005) The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976) 30(18):2024–2029
Van Royen BJ, De Gast A, Smit TH (2000) Deformity planning for sagittal plane corrective osteotomies of the spine in ankylosing spondylitis. Eur Spine J 9(6):492–498
Glassman SD, Berven S, Bridwell K et al (2005) Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine 30:682–688
Lazennec JY, Ramare S, Arafati N, Laudet CG, Gorin M, Roger B, Hansen S, Saillant G, Maurs L, Trabelsi R (2000) Sagittal alignment in lumbosacral fusion: relations between radiological parameters and pain. Eur Spine J 9(1):47–55
Schwab F, Patel A, Ungar B, Farcy JP, Lafage V (2010) Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976) 35(25):2224–2231
Lamartina C et al (2012) Criteria to restore the sagittal balance in deformity and degenerative spondylolisthesis. Eur Spine J 21(Suppl 1):S27–S31
Imagama S, Ito Z, Wakao N, Seki T, Hirano K, Muramoto A, Sakai Y, Matsuyama Y, Hamajima N, Ishiguro N, Hasegawa Y (2013) Influence of spinal sagittal alignment, body balance, muscle strength, and physical ability on falling of middle-aged and elderly males. Eur Spine J 22(6):1346–1353
Yoshimoto H, Sato S, Masuda T (2005) Spinopelvic alignment in patients with osteoarthrosis of the hip: a radiographic comparison to patients with low back pain. Spine 30:1650–1657
Roussouly P, Gollogly S, Berthonnaud E, Dimnet J (2005) Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine (Phila Pa 1976) 30(3):346–353
Hey HW et al (2017) Differences in erect sitting and natural sitting spinal alignment-insights into a new paradigm and implications in deformity correction. Spine J 17(2):183–189
Dolphens M, Cagnie B, Coorevits P, Vleeming A, Danneels L (2013) Classification system of the normal variation in sagittal standing plane alignment: a study among young adolescent boys. Spine (Phila Pa 1976) 38(16):E1003–E1012
Bae J, Theologis A, Jang JS, Lee SH, Deviren V (2016) Impact of fatigue on maintenance of upright posture: dynamic assessment of sagittal spinal deformity parameters after walking 10 minutes. Spine (Phila Pa 1976) 42(10):733–739
Wade R, Yang H, McKenna C, Faria R, Gummerson N, Woolacott N (2013) A systematic review of the clinical effectiveness of EOS 2D/3D X-ray imaging system. Eur Spine J 22(2):296–304. https://doi.org/10.1007/s00586-012-2469-7
Acknowledgements
We would like to thank Darren Koh Zhi-Sheng and Jonathan Tan Jiong-Hao for their help in applying for ethics approval for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Hey, H.W.D., Tan, K.L.M., Moorthy, V. et al. Normal variation in sagittal spinal alignment parameters in adult patients: an EOS study using serial imaging. Eur Spine J 27, 578–584 (2018). https://doi.org/10.1007/s00586-017-5459-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-017-5459-y