Abstract
Purpose
To analyse the clinic-radiological factors associated with neurological deficit following lumbar disc herniation.
Methods
A prospective, cross-sectional study was performed in 140 cases of micro-discectomy following lumbar disc herniation. Group 1 included 70 consecutive patients with motor deficit and group 2 (controls) included 70 patients with intact neurology. Motor deficit was defined as the occurrence of motor power ≤3/5 in L2–S1 myotomes. Multiple clinical and radiological parameters were studied between the two groups.
Results
Patients with diabetes (p 0.004), acute onset of symptoms (p 0.036), L3–4 discs (p 0.001), sequestrated discs (p 0.004), superiorly migrated discs (p 0.012) and central discs (p 0.004), greater antero-posterior disc dimension (p 0.023), primary canal stenosis (p 0.0001); and greater canal compromise (p 0.002) had a significant correlation with the development of neurological deficit. The presence of four or more of these risk factors showed a higher chance of the presence of motor deficit (sensitivity of 74%, specificity of 77%). Age, sex, previous precipitating events, severity of pain, smoking, and number of herniations levels did not affect the occurrence of deficit (p > 0.05 for all). Patients with or without bladder symptoms were similar with respect to all clinico-radiological parameters. However, the time delay since the occurrence of deficit was significantly shorter in patients with bladder involvement (p 0.001).
Conclusion
Patients with diabetes, acute presentation, central, sequestrated and superiorly migrated discs, high lumbar disc prolapse, and greater spinal canal compromise are predisposed to the presence of motor deficit.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lumbar disc herniation (LDH) is the most common cause of low back pain and sciatica [1, 2]. The natural history of radiculopathy in most patients is clinical resolution [3]. 90% of acute sciatica respond to conservative management [3] and indications for surgical intervention include severe, intractable pain, pain unresponsive to conservative treatment, and neurological deficit [4, 5].
Neurological deficit is the most dreaded complication following lumbar disc herniation [6], although rare it can lead to long-lasting disabilities [7]. The current literature is unclear about, why morphologically similar-appearing disc prolapses result in different neurological manifestations. While certain studies have indicated higher incidence of neurological complications in large disc prolapse with greater canal compromise [8], Cribb et al. [9] had reported no neurological deficits in 15 patients with massive lumbar disc prolapse who were managed conservatively. Bozzao et al. [10] described complete resolution of 70% of massively herniated discs and indicated that such herniations may not be as catastrophic as commonly believed. It is also controversial if multilevel root compressions have greater association with neurodeficit [11].
We conducted a prospective case control study to understand the role of different clinical and radiological factors which might be associated with the presence of motor deficit in patients with lumbar disc prolapse.
Materials and methods
The current study was a prospective, cross-sectional study involving patients who underwent microscopic discectomy following lumbar disc herniations between December 2013 and March 2015 (after obtaining approval of Institutional Review Board). Written informed consent was obtained from all patients. During this period, a total of 556 patients underwent microscopic discectomy. Any patient with obvious evidence of inter-vertebral instability, concurrent stenosis at cervical or thoracic levels or suspected infective or inflammatory pathologies was excluded from the study. 70 consecutive patients who had presented with motor deficit (with or without bladder symptoms) were included under Group 1 (Cases). Among the remaining patients, the control group (Group 2) which included 70 patients without any pre-operative neurological deficit was selected through random allocation. The indications for surgery were severe, unrelenting radicular pain, not responding to conservative management, or occurrence of neurological deficit, in the form of motor deficit or bladder involvement.
Motor deficit was defined as the occurrence of motor power ≤3/5 (MRC grading) in L2, 3, 4, 5, and S1 myotomes. Associated bladder symptoms at presentation were also recorded. Patients with isolated sensory deficits (hypo- or paresthesia) motor grade ≥4 were excluded. Complete motor deficit was defined as the motor power of 0/5 in the concerned myotome.
On admission, patients underwent detailed clinical examination, including examination of spine, nerve root stretch signs, and motor, sensory, and reflex examination. Functional assessment of the disability status was performed using Oswestry Disability Index score both pre-operatively and post-operatively at the second and sixth month follow-up. The symptom duration was separately classified under three categories: (1) the duration since initial presenting symptom was defined as the time lag between the first symptom experienced by the patent related to back and the surgical lumbar decompression. (2) Onset of the current symptomatology (acute, if the present symptomatic episode is shorter than 3 month duration; or chronic if the symptoms are longer; or acute on chronic if the symptoms of longer duration have acutely worsened). (3) Number of the previous symptomatic episodes (number of symptomatic episodes prior to the current episode, with asymptomatic intervening periods). All patients underwent radiological investigations, including lumbar radiographs and magnetic resonance imaging scan.
All patients underwent surgical microlumbar discectomy under general anesthesia. If the disc herniation was unilaterally accessible, fenestration and discectomy alone were performed. Large, central disc fragments which might otherwise need a significant dural retraction for excision or disc prolapses causing bilateral symptoms were removed after wide, midline laminectomy. Post-operative mobilisation was started early, as tolerated by the patient.
Statistical analysis was performed using IBM SPSS (Statistical Package for Social Sciences) Version 20:0. To compare the association of various factors in groups 1 and 2, Chi-square test or Fisher exact test was used. ROC curve was used to find the cut-off values and sensitivity/specificity for various variables studied. p < 0.05 was considered as significant.
Results
During the study period, 556 patients underwent microscopic lumbar discectomy. Eleven cases excluded from the study were as follows: eight cases with concomitant stenosis in the cervical spine, two cases which had an incidental spondylolysis at the distal level (L5–S1) and underwent L4–5 microscopic discectomy, and one case with incidental features of sacroiliitis with suspected seronegative arthropathy. None of the excluded cases presented with motor or sensory neurodeficit (Fig. 1).
545 remaining cases were considered for analysis. 70 consecutive cases presenting with motor deficit ≤3/5 MRC grade were considered as Group 1(Deficit Group). There were 475 cases which did not meet the criteria for motor deficit. There were 135 cases which had isolated sensory disturbances or mild motor deficit and were excluded from selection into the control group. There were 340 cases which underwent micro-discectomy without clinical findings of any neurological deficit. Based on a random number generator sequence, we selected 70 cases from these 340 to form the control group for the statistical analysis.
The mean age of patients in our study was 41.5 years, with 108 males and 32 females. Most of our patients generally presented to us quite late after the occurrence of neurological deficit (Mean 40.4 days). Among the patients with motor deficit, seven presented with isolated L5 weakness, 18 patients had associated bladder involvement, and 18 had associated complete sensory loss at the concerned dermatome. Among the patients with bladder symptoms, 11 had decreased anal tone and perianal sensation at presentation.
General profile of patients (group 1 vs group 2: Table 1)
There was a significantly greater incidence of diabetes mellitus in the patients who developed neurological deficit [20% diabetics in neurodeficit group and 4.3% in the non-deficit population (odd’s ratio: 5.6, CI 1.52–20.41)]. Age, sex, body mass index, occupation, smoking history, and other co-morbidities showed no significant difference in distribution between the groups.
Symptomatology at presentation (group 1 vs group 2: Table 2)
Fifty-seven percent had an acute onset of symptoms in the neurodeficit group (group 1), as against 27% in the non-deficit population [p 0.036; odd’s ratio 3.57, CI 1.76–7.26]. The patients with neurodeficit also had significantly lesser number of previous symptomatic episodes (mean number of 0.47 previous episodes in group 1 vs 1.03 in group 2: p 0.001; cutoff ≥2 episodes; odd’s ratio 2.45; CI 0.93–6.45). No other factor (including initial presenting symptom, presence of any precipitating event, unilaterality of symptoms, localization of pain at admission, and nerve root tension) showed any significant difference in distribution between the groups.
Comparison of radiological parameters (group 1 vs group 2: Table 3)
Eighty-five percent of patients with L3–4 disc prolapse presented with neurological deficit (p 0.001; odd’s ratio 5.95, CI 2.1–16.86). Similarly, 74% of our superiorly migrated [p 0.012; odd’s ratio 3.42, CI 1.25–9.29] and 85% of sequestrated disc prolapse [p 0.004; odd’s ratio 11, CI 2.13–56.56 (sequestrated vs protruded); odd’s ratio 4.89, CI 1.02–23.39 (sequestrated vs extruded)] developed neurodeficit. 69% of our patients with central disc prolapse developed deficit (p 0.004; odd’s ratio 3.49, CI 1.7–7.18). Other morphological factors, including Pfirmann grading, Modic changes, nerve root compression at the neural foraminal level, disc height, and facet dimensions (length, width, and tropism) did not affect the presence of neurological complications.
The mean antero-posterior disc dimension was 8.7 mm in the neurodeficit group, in comparison with 7.5 mm in the non-deficit patients (p 0.023; cutoff 5.8, sensitivity: 87, and specificity: 35.7). The mean canal compromise was 63.5% in the neurodeficit group, in comparison with 52.3% in the non-deficit patients (p 0.002; cutoff: 59.4%; sensitivity: 58.6 and specificity: 67.1). The mean bony canal dimension was also significantly smaller in the neurodeficit population when compared to the non-deficit patients (p 0.0001).
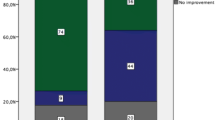
We could thus identify ten risk factors, which were significantly associated with the presence of motor deficit (Table 4): diabetes mellitus, acute onset of current symptomatology, primary level L3–4 and above, central disc prolapse, superiorly migrated disc prolapse, sequestrated disc prolapse, mean AP disc dimension >5.9 mm, mean canal compromise >59.4%, decreased Bony canal dimension—AP (in mm), and decreased Bony canal dimension—Lateral (in mm). When four or more of these risk factors were present, the chances of the presence of motor deficit were significantly increased in a patient with lumbar disc prolapse (sensitivity of 74.3, specificity of 77.1, positive likelihood ratio—3.25, and negative likelihood ratio—0.33).
Among patients with motor deficit, when the patients with bladder involvement (18 patients) were compared with those without associated bladder symptoms, we could observe that the two subsets were similar with respect to all studied parameters (age—p: 0.161, sex—p: 0.99, occupation—p: 0.07, duration since initial symptom—p: 0.17, onset of symptom—p: 0.1, number of previous symptomatic episodes—p: 0.34, smoking—p: 0.53, initial symptom—p: 0.47, precipitating event—p: 0.05, pain localisation at admission—p: 0.76, diabetics p: 0.33, other medical co-morbidities—p: 0.69, Oswestry Disability index—p: 0.56, type of disc prolapse—p: 0.57, location of herniation—p: 0.89, migration of herniated disc—p: 0.61, number of herniation levels—p: 0.53, primary level of disc herniation—p: 0.44, mean antero-posterior dimension of disc—p: 0.81, and mean canal compromise—p: 0.98 or facetal morphology). The only parameter in which the patients with associated bladder involvement differed from the other subset was the earlier presentation since occurrence of neurological deficit (16 ± 21.7 days in patients with bladder symptoms vs 48.8 ± 80.7 days (p 0.001).
Discussion
Neurological deficit following lumbar disc herniation is a rare event, with a reported incidence of less than 2% [12]. It is a serious adversity, with major functional and medico-legal implications; and urgent surgical lumbar decompression is advocated as the ideal management. Although the literature has discussed the role of various factors in the development of this complication, our understanding on this issue is still unclear [12–16]. There is paucity of prospective studies in the existing literature, which have analyzed the development of neurological impairment in lumbar disc prolapse or recovery following surgery [12].
In general, neurological deficit includes three components: motor, sensory, and autonomic (including bladder and bowel functions) deficits. Of these three faculties, the most disabling components of the neurological impairment are motor and autonomic deficits, which inflict serious functional restrictions. Therefore, we did not include isolated sensory deficit as an inclusion criteria for neurodeficit in our study. Majority of our patients presented to us quite late after the occurrence of neurological deficit, which is the usual scenario in the developing nations (mean 40.4 days).
We observed that diabetes mellitus was significantly associated with greater development of motor deficit. The poorer ability of neural elements to recuperate (due to compromised healing or associated neuropathy and vasculopathy) could be the possible reason behind such an association. Certain authors have observed that diabetics have overall higher recurrences, greater chances of developing neurodeficit, and poorer surgical outcome [17, 18]. Our findings too showed greater incidence of neurological impairment in diabetics. However, the possibilities of mis-diagnosis exist, as diabetic sequelae like neuropathy and amyotrophy too may present with motor deficit. [17–19]. Age over 45 years has broadly been associated with poorer prognosis in patients with lumbar disc herniation, although there is no evidence in the literature which indicates an increased incidence of neurological deficit in elderly patients [20]. Even in our patients, although it was observed that patients with neurological impairment showed a slight tendency towards older age group distribution, there was no statistically significant association.
We observed that the patients with neurodeficit had significantly lesser number of previous symptomatic episodes. It was also observed that motor deficit developed more in patients who had an acute course of current symptomatology. In fact, in a majority of our patients in group 1, the deficit was the initial presenting feature. This is in contrary to common belief that neurodeficit happens more in the chronically and repetitively compromised nerve roots [12]. Our observations suggest that acutely compromised neural elements suffer more grievous damage than chronically decompensated nerve roots.
Among radiological parameters studied, L3–4 involvement was significantly more associated with motor deficit, while L5–S1 disc prolapse was the least associated. In view of the smaller cross-sectional areas, disc herniations at higher lumbar levels tend to be more symptomatic [21]. Lurie et al. demonstrated that higher level lumbar disc herniations were more far-laterally or foraminally located than lower disc prolapse [22]. Although they did not show any correlation between the occurrence neurological impairment and level of disc herniation, the patients with higher level disc herniation had significantly greater asymmetric reduction of deep tendon reflexes [22]. Our observations indicate that although the overall incidence of higher level disc herniations was much lower (19.3%), the proportion of these patients who developed neurological impairment was significantly greater (81%).
We observed that superiorly migrated, sequestrated, and central disc prolapses significantly increased the chances of developing neurological deficit. The existing literature is far from lucid on the correlation between various morphological features of herniated lumbar discs and clinical manifestations [23, 24]. Although the phenomenon of spontaneous disappearance of sequestrated disc herniations has been demonstrated in the literature [9], certain studies have also shown poorer prognosis following such prolapses [8]. Suzuki et al. [24] described that non-contained and migrated disc prolapses were significantly associated with increased incidence of motor deficit. Kalemci et al. [25] suggested that neurodeficit could be the resultant of secondary venous congestion following large central disc prolapse compromising the canal.
We also assessed the correlation between the size of disc herniation, canal, and foraminal dimensions and percentage of canal compromise, as observed on MRI scan, and the presence of motor deficit. Disc herniations larger than 5.9 mm antero-posterior dimensions, canal compromise greater than 59.4%, and narrower (Antero-posterior and lateral) bony canals were significantly associated with neurodeficit. Sutheerayongprasert et al. [8] showed that larger mean antero-posterior disc dimension and greater mean compromise of the spinal canal significantly correlated with poorer outcome in patients with lumbar disc prolapse. The controversies regarding massive disc herniations and their clinical implications are well known [8, 9, 14–16]. Large discs definitely inflict a significant mechanical compromise of the neural elements [15, 22, 23]; although the possibilities of gradual, complete resolutions of such discs have also been demonstrated [9]. Nevertheless, our study definitely indicated that physical compromise of the neural elements (as described by these parameters) was definitely associated with adverse neurological outcomes. Other radiological factors, including multilevel disc herniations, ligamentum flavum thickness, facetal morphology, foraminal size/compromise, disc height, Pfirmann grades, or Modic changes, did not significantly correlate with the presence of neurological deficit.
Patients with associated bladder involvement were similar to the other subset of patients without bladder involvement in all observed clinico-radiological aspects, except for significantly earlier presentation following the development of deficit in the former category of patients.
Conclusion
The etiology for development of motor deficit in disc herniation has been shown to be multi-factorial. When a combination of these factors occurs simultaneously, the critical compensatory capability of the vital neural elements is lost, leading to the adverse neurological manifestation. We have postulated the criteria for predicting the presence of neurological deficit in lumbar disc prolapse (Table 4). Of the ten risk factors identified, when a combination of four or more was present, the possibility of presence of neurodeficit should be considered.
References
Hoy D, Brooks P, Blyth F, Buchbinder R (2010) The epidemiology of low back pain. Best Pract Res Clin Rheumatol 24(6):769–781
Frymoyer JW (1988) Back pain and sciatica. N Engl J Med 318(5):291–300
Weber H (1983) Lumbar disc herniation: a controlled, prospective study with 10 years of observation. Spine 8(2):131–140
Gibson JNA, Waddell G (2007) Surgical interventions for lumbar disc prolapse: updated Cochrane Review. Spine 32(16):1735–1747
Blamoutier A (2013) Surgical discectomy for lumbar disc herniation: surgical techniques. Orthop Traumatol Surg Res 99(1):S187–S196
Kostuik JP, Harrington I, Alexander D, Rand W, Evans D (1986) Cauda equina syndrome and lumbar disc herniation. J Bone Jt Surg Am 68(3):386–391
Kostuik JP (2004) Medicolegal consequences of cauda equina syndrome: an overview. Neurosurg Focus 16(6):39–41
Sutheerayongprasert C, Paiboonsirijit S, Kuansongtham V, Anuraklekha S, Hiranyasthiti N, Neti S (2012) Factors predicting failure of conservative treatment in lumbar-disc herniation. J Med Assoc Thai 95(5):674
Cribb GL, Jaffray DC, Cassar-Pullicino VN (2007) Observations on the natural history of massive lumbar disc herniation. Bone Jt J 89(6):782–784
Bozzao A, Gallucci M, Masciocchi C, Aprile I, Barile A, Passariello R (1992) Lumbar disk herniation: MR imaging assessment of natural history in patients treated without surgery. Radiology 185(1):135–141
Iizuka Y, Iizuka H, Tsutsumi S, Nakagawa Y, Nakajima T, Sorimachi Y et al (2009) Foot drop due to lumbar degenerative conditions: mechanism and prognostic factors in herniated nucleus pulposus and lumbar spinal stenosis. J Neurosurg Spine 10(3):260–264
Gitelman A, Hishmeh S, Morelli BN, Joseph SA Jr, Casden A, Kuflik P et al (2008) Cauda equina syndrome: a comprehensive review. Am J Orthop (Belle Mead NJ) 37(11):556–562
Lavy C, James A, MacDonald JW, Fairbank J (2009) Cauda equina syndrome. Br Med J 338:881–884
Weinstein JN, Tosteson TD, Lurie JD, Hanscom B, Skinner JS, Abdu WA et al (2006) Surgical vs nonoperative treatment for lumbar dis herniation. the spine patient outcome research trial (SPORT): a randomised trial. JAMA 296(20):2441–2450
Haugen AJ, Brox JI, Grovle L, Kellers A, Natvig B, Soldal D et al (2012) Prognostic factors for non-success in patients with sciatica and disc herniation. BMC Musculoskelet Disord 13:183
Nascone JW, Lauerman WC, Wiesel SW (1999) Cauda Equina syndrome: is it a surgical emergency? Univ Pa Orthop J 12:73–76
Simpson JM, Silveri CP, Balderston RA, Simeone FA, An HS (1993) The results of operations on the lumbar spine in patients who have diabetes mellitus. J Bone Jt Surg Am 75(12):1823–1829
Sakellaridis N (2006) The influence of diabetes mellitus on lumbar intervertebral disk herniation. Surg Neurol 66(2):152–154
Epstein NE (2002) Foraminal and far lateral lumbar disc herniations: surgical alternatives and outcome measures. Spinal Cord 40(10):491–500
Ahn Y, Lee SH, Park WM, Lee HY, Shin SW, Kang HY (2004) Percutaneous endoscopic lumbar discectomy for recurrent disc herniation: surgical technique, outcome, and prognostic factors of 43 consecutive cases. Spine 29(16):E326–E332
Dora C, Wälchli B, Elfering A, Gal I, Weishaupt D, Boos N (2002) The significance of spinal canal dimensions in discriminating symptomatic from asymptomatic disc herniations. Eur Spine J 11(6):575–581
Lurie JD, Faucett SC, Hanscom B, Tosteson TD, Ball PA, Abdu WA et al (2008) Lumbar discectomy outcomes vary by herniation level in the Spine Patient Outcomes Research Trial. J Bone Jt Surg Am 90(9):1811–1819
Shapiro S (1993) Cauda equina syndrome secondary to lumbar disc herniation. Neurosurgery 32(5):743–747
Suzuki A, Matsumura A, Konishi S, Terai H, Tsujio T, Dozono S, Nakamura H (2011) Risk factor analysis for motor deficit and delayed recovery associated with L4/5 lumbar disc herniation. J Spinal Disord Tech 24(1):1–5
Kalemci O, Kizmazoglu C, Ozer E, Arda MN (2013) Lumbar disc herniation associated with contralateral neurological deficit: can venous congestion be the cause? Asian Spine J 7(1):60–62
Acknowledgements
Funding was provide by Ganga Orthopaedic Research and Education Foundation, Coimbatore, India.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical standards
The study was approved by the institutional review board. The study was conducted in accordance with 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Krishnan, V., Rajasekaran, S., Aiyer, S.N. et al. Clinical and radiological factors related to the presence of motor deficit in lumbar disc prolapse: a prospective analysis of 70 consecutive cases with neurological deficit. Eur Spine J 26, 2642–2649 (2017). https://doi.org/10.1007/s00586-017-5019-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-017-5019-5