Abstract
Purpose
There are many reports about the risk factors for recurrence after lumbar disc surgery.
However, there are none about whether lumbosacral transitional vertebrae (LSTV) are associated with recurrent lumbar disc herniation (LDH). We investigated various risk factors for recurrent LDH after discectomy including LSTV.
Methods
A total of 119 patients who had undergone a discectomy for L4–5 disc herniation were evaluated with a minimum follow-up of two years. Clinical parameters including age, gender, body mass index (BMI), and smoking status, and radiological parameters including type of herniated disc, degree of disc degeneration, LSTV, and sagittal range of motion (SROM) in flexion-extension radiography were evaluated. SROM was measured by the difference of the lordotic angle between the flexion and extension view.
Results
Recurrent disc herniation at L4–5 developed in 21 (17.6%) of the 119 patients. The mean period between primary surgery and recurrence was 17.6 ± 21.1 months. LSTV was found in 11 (52.4%) of the 21 patients who had recurrence and seven (7.1%) of the 98 patients in the non-recurrent group. SROM at L4–5 was 11.68 ± 4.24° in the recurrent group and 9.04 ± 3.65° in the non-recurrent group with a significant difference (p = 0.004). Multiple logistic regression analyses confirmed that LSTV and a larger SROM were significant risk factors for recurrent disc herniation at L4–5.
Conclusions
Lumbosacral transitional vertebrae and a hypermobile disc in flexion-extension radiography were found to be risk factors for recurrent lumbar disc herniation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recurrent lumbar disc herniation (LDH) is a common complication after discectomy, with a reported frequency of up to 21% [1, 2]. The most frequent recurrence occurred at the previous operation site [2]. It may exacerbate pain in the back and legs, and even require a revision surgery for some patients. However, there has been controversy regarding the risk factors for recurrent LDH. Various risk factors have been reported, reflecting conflicting results for the same factors depending on the study. As clinical risk factors, age, smoking status, gender, and obesity could be associated with the recurrence of disc herniation [1,2,3,4,5]. Radiological factors such as disc degeneration, larger disc height, and larger sagittal range of motion (SROM) in flexion-extension radiography might also be risk factors for recurrence [6, 7].
Lumbosacral transitional vertebra (LSTV) is an anatomical variant, in which transverse processes of the last lumbar vertebra fuse with the sacrum. The prevalence of LSTV in the literature ranges from 4 to 35% of the general population [8, 9]. The clinical significance and its relation with other pathologies are still controversial. Recently, M. Tang et al. reported that specific LSTV types, namely types II and IV, were significantly associated with lower back pain (LBP) [8]. Studies have been reported that disc degeneration progressed at the level above the LSTV, contributing to relative hypermobility [9, 10].
To the best of our knowledge, there are no published reports about whether LSTV is a risk factor of recurrent LDH. Some radiological risk factors like larger SROM may contribute to segmental instability, and LSTV is related with hypermobility at the level above the LSTV. For this reason, theoretically, LSTV could be a risk factor for recurrent LDH. We conducted this study to determine whether LSTV is a risk factor, and investigate other various risk factors for recurrent LDH.
Materials and methods
One hundred nineteen patients who underwent partial laminectomy and discectomy at L4–5 were enrolled consecutively in this study with a minimum follow-up period of two years. The mean follow-up period was 24.6 ± 13.8 months. Only the patients who had L4–5 disc herniation were included in the study, excluding others with herniation at other levels, because LSTV mostly influences the disc just above the LSTV, which is the L4–5. This study was approved by institutional review board in the university hospital (INHAUH 2016-12-021).
The definition of what qualifies as “recurrent” LDH has not yet been determined in terms of the time period between primary surgery and recurrence. Swartz and Trost defined re-herniation as the experience of another disc herniation more than six months after the primary surgery on either an ipsilateral or contralateral location [11]. In this study, we defined recurrent LDH as re-herniation seen at the same level after a pain-free period of two months following the primary surgery. According to our post-operative management protocol, patients were instructed to wear a corset brace fortwo months post-operatively, and then encouraged to do back muscle exercises. All recurrences on the ipsilateral or contralateral sides at the same level were included in the study.
Surgery was performed by a senior surgeon using conventional partial laminectomy and discectomy techniques. Through a midline approach, the lamina bone was partially resected and a small incision was made at the annulus fibrosus to gain access to the herniated nucleus material. The hole was about 1 cm wide and oval shaped. After removing the fragmented disc, the annulotomy site was left open without any covering. Clinical parameters including age, gender, body mass index (BMI), and smoking status, and radiological parameters including LSTV, SROM at L4–5, type of herniated disc, and grade of disc degeneration were analyzed.
Based on the Castellvi classification [12], LSTV were classified into four types: type I, dysplastic transverse process; type II, incomplete lumbarization/sacralization; type III, complete lumbarization/sacralization; and type IV, mixed findings (Fig. 1). Sagittal range of motion (SROM) was calculated by the difference of lordotic angle between in the flexion and extension radiography, which was measured in relation to the lines of the L4 lower endplate and L5 upper endplate. Type of herniated disc was divided into protrusion, subligamentous extrusion, transligamentous extrusion, and sequestration in MR images. Grade of disc degeneration was evaluated in the sagittal T2WI MR images according to the Pfirrmann criteria [13].
Univariate analysis was performed using an independent t test, Mann-Whitney, and Fisher’s exact test for clinical and radiological parameters for all patients. Univariate analysis and multiple logistic regression analysis were performed to analyze independent risk factors for recurrent lumbar disc herniation. Variables with a p value of less than 0.2 on univariate analysis were included in the multiple logistic regression models. Statistical significance was defined as p < 0.05 and analyses were performed using SPSS (version 18.0, Inc.; Chicago, USA).
Results
Recurrent disc herniation at L4–5 was identified in 21 (17.6%) of the 119 patients who underwent laminectomy and discectomy. Among these 21 patients, 18 developed recurrence on the ipsilateral side and three on the contralateral side. The mean time duration between primary surgery and recurrence was 17.6 months, ranging from two months to five years.
There were no significant differences in age, gender distribution, smoking status, height, weight, and BMI between the recurrent and non-recurrent groups (Table 1). There was no difference between the two groups according to the type of herniated disc. The most common type of herniated disc was transligamentous extrusion, which occurred in 68 patients, followed by subligamentous extrusion in 46 patients, sequestration in three patients, and protrusion in two patients. Recurrent LDH was found in 13 (19.1%) of the 68 transligamentous extrusion cases and eight (17.3%) of the 46 subligamentous extrusion cases. Among the protrusion and sequestration cases, recurrent LDH was not found. We also investigated recurrence rate according to the grade of disc degeneration. Before surgery, the grades of disc degeneration were grade 3 in 87 patients and grade 4 in 32 patients. Recurrent LDH was found in 13 patients with grade 3 and eight patients in grade 4. There was no statistical difference according to the grades of disc degeneration (Table 2).
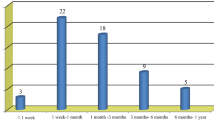
LSTV was identified in 18 patients, consisting of 11 patients in the recurrent group and seven patients in the non-recurrent group. Thus, the recurrence rate of disc herniation was much higher in the patients with LSTV, which was 52.4% (11 of the 21 patients) in the recurrent group compared to 7.1% (seven of 98 patients) in the non-recurrent group with a statistical difference between the two groups (p < 0.001). Among the 11 patients who had LSTV, the time period between primary surgeries to recurrence was 9.4 ± 5.3 months, ranging from two to 22 months. This period was much shorter than that for the patients who had no LSTV, which was 27.4 ± 28.5 months, ranging from four months to five years (p = 0.017).
Of the 18 patients with LSTV, LSTV type II was found in ten patients, type III in seven patients, and type I in one patient. In the recurrent group, there were seven patients with type II, three patients with type III, and one patient with type I. In the non-recurrent group, LSTV type II was found in three patients and type III in four patients (Table 3). This result showed that recurrent LDH was more common with respect to type II LSTV than other types.
Sagittal range of motion in flexion-extension radiography turned out to be another significant risk factor of recurrent LDH. In the recurrent group, SROM was 11.68 ± 4.24° in flexion-extension radiography, compared to 9.04 ± 3.65° in the non-recurrent group. The difference was also statistically significant (p = 0.004). Univariate analysis demonstrated that LSTV and a large SROM were significantly related to the recurrence of LDH. Any variable with a p value of less than 0.2 in univariate analysis was included in the multiple logistic regression analysis. Multiple logistic regression analyses also showed that LSTV and a large SROM were significant risk factors for recurrence of LDH (Table 4).
Regarding treatment for the 21 patients with recurrent LDH, three patients were treated conservatively, nine with revision discectomy, and nine with discectomy and fusion surgery.
Discussion
The clinical significance of LSTV is still controversial, although Bertolotti’s syndrome refers to the association between LSTV and LBP [14]. Bertolotti first reported in 1917 that unilateral or bilateral enlargement of the transverse process of the lower lumbar vertebra may articulate with the sacrum or ilium, likely leading to arthritic changes. Early disc degeneration just above the LSTV occurs in young patients, which may be accompanied by LBP [15]. The LSTV may irritate nerve roots between the enlarged transverse process and sacral ala [16, 17]. Wiltse et al. [18] reported that the L5 nerve root may be compressed by impingement of the transverse process of L5 against the sacral ala in spondylolisthesis. Elster et al. [19] found that the incidence of degenerative disc disease, spinal stenosis, and L5 radiculopathy were nearly nine times higher at the level adjacent to the transitional vertebrae.
Recurrent disc herniation is a common complication after discectomy and lead to unsatisfactory outcomes. This study hypothesized that LSTV could be related with re-herniation given that, as an anatomical variant, the LSTV may affect biomechanical stress at the disc just above the LSTV. Therefore, this study included L4–5 disc herniation because the disc at other segments except L4–5 is less likely to be influenced by LSTV.
Biomechanical stress on the disc may be different depending on the type of LSTV. LSTV type II is incomplete sacralization or lumbarization with pseudarticulation between the transverse process and sacrum, which may cause increased mobility after discectomy. On the other hand, LSTV type III is complete fusion of the transverse process with the adjacent sacrum. Thus, discectomy at the level above LSTV type II is more likely to cause mechanical stress on the disc than other types of LSTV. In a population-based study of 5860 individuals with LSTV, LSTV type II turned out to be significantly associated with LBP [8]. In the present study, LSTV type II was found to be more common in the recurrent group than other types. Although the clinical significance of this LSTV remains controversial, it is known that the disc above the LSTV is prone to disc degeneration due to hypermobility [10]. This may be analogous to adjacent segment degeneration after spinal fusion surgery. Inability to distribute a load evenly and an increase in local stress of congenital lumbosacral malformation cause lumbar instability [19,20,21,22]. A large sagittal range of motion in flexion extension radiography signifies hypermobile disc space. Therefore, the risk factor LSTV and larger SROM contribute to instability in the corresponding disc, causing the development of recurrent disc herniation.
Numerous studies were conducted to investigate risk factors for recurrent LDH. Suk et al. [3] reported that young age, male gender, smoking, and traumatic events might be risk factors. Kim KT et al. [5] reported that a larger SROM and low iliac crest can be risk factors for recurrent LDH at L5-S1. In the current study, LSTV and a large SROM were found to be significant risk factors for recurrent disc herniation, although no clinical factors of recurrent LDH were identified. To the best of our knowledge, this study is the first to investigate LSTV as a risk factor of recurrent disc herniation.
Recently, minimally invasive discectomy (MID) using endoscopy has been performed instead of traditional discectomy. According to a meta-analysis of 2139 patients and 16 studies, post-operative clinical efficacy was similar between MID-treated patients and standard discectomy patients [23]. Furthermore, MID has an advantage of shorter incision length, lower bleeding, and shorter hospital stay; however, there is a disadvantage of higher recurrence rate and longer operation time [24]. MID has a long learning curve and is difficult for beginners to access; however, currently navigation, system is helpful for beginners and to achieve shorter operation time and lower fluoroscopy time [25]. Because surgical cases using MID technique have not been enrolled in this study, a large multi-centre study with MID using such as endoscopy will be necessary.
This study has some limitations. This is a retrospective study conducted at a single research centre and the study has relative low cases to prove a risk factor of recurrent LDH. However, all surgeries were performed by a single surgeon, and evaluation and rehabilitation were performed in the same way before and after surgery.
In conclusion, recurrent disc herniation at L4–5 developed in 21 (17.6%) of 119 patients who underwent conventional laminectomy and discectomy. A lumbosacral transitional vertebra was found in 52.4% of the patients in the recurrent group and 7.1% of the patients in the non-recurrent group. Lumbosacral transitional vertebra and a larger sagittal range of motion in flexion-extension radiography were found to be significant risk factors for recurrent disc herniation. The findings in this study suggest that surgeons should consider the possibility of recurrent disc herniation in patients with a lumbosacral transitional vertebra and hypermobile disc.
References
Shin BJ (2014) Risk factors for recurrent lumbar disc herniations. Asian Spine J 8:211–215
Cheng J, Wang H, Zheng W, Li C, Wang J, Zhang Z, Huang B, Zhou Y (2013) Reoperation after lumbar disc surgery in two hundred and seven patients. Int Orthop 37:1511–1517
Suk KS, Lee HM, Moon SH, Kim NH (2001) Recurrent lumbar disc herniation: results of operative management. Spine (Phila Pa 1976) 26:672–676
Cinotti G, Roysam GS, Eisenstein SM, Postacchini F (1998) Ipsilateral recurrent lumbar disc herniation: a prospective, controlled study. J Bone Joint Surg Br 80:825–832
Kim KT, Lee DH, Cho DC, Sung JK, Kim YB (2015) Preoperative risk factors for recurrent lumbar disc herniation in L5-S1. J Spinal Disord Tech 28:E571–E577
Axelsson P, Karlsson BS (2004) Intervertebral mobility in the progressive degenerative process. A radiostereometric analysis. Eur Spine J 13:567–572
Kim KT, Park SW, Kim YB (2008) Disc height and segmental motion as risk factors for recurrent lumbar disc herniation. Spine (Phila Pa 1976) 34:2674–2678
Tang M, Yang XF, Yang SW, Han P, Ma YM, Yu H, Zhu B (2014) Lumbosacral transitional vertebra in a population-based study of 5860 individuals: prevalence and relationship to low back pain. Eur J Radiol 83:1679–1682
Ver Verergauwen S, Parizel PM, Van Breusegem L, Van Goethem JW, Nackaerts Y, Van den Hauwe L, De Schepper AM (1976) Distribution and incidence of degenerative spine changes in patients with a lumbo-sacral transitional vertebra. Eur Spine J 6:168–172
Paajanen H, Erkintalo M, Kuusela T, Dahlstrom S, Kormano M (1989) Magnetic resonance study of disc degeneration in young low-back pain patients. Spine (Phila Pa 1976) 14:982–985
Swartz KR, Trost GR (2003) Recurrent lumbar disc herniation. Neurosurg Focus 15:E10
Castellvi AE, Goldstein LA, Chan DP (1984) Lumbosacral transitional vertebrae and their relationship with lumbar extradural defects. Spine (Phila Pa 1976) 9:493–495
Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N (2001) Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976) 26:1873–1878
Bertolotti M (1917) Contribution to the knowledge of the defects as it relates to regional differences in the spine with regards to the as simulation of L5 and the sacrum. Radiol Med 4:113–114
Quinlan JF, Duke D, Eustace S (2006) Bertolotti’s syndrome. A cause of back pain in young people. J Bone Joint Surg Br 88:1183–1186
Otani K, Konno S, Kikuchi S (2001) Lumbosacral transitional vertebrae and nerve-root symptoms. J Bone Joint Surg Br 83:1137–1140
Hashimoto M, Watanabe O, Hirano H (1996) Extraforaminal stenosis in the lumbosacral spine. Efficacy of MR imaging in the coronal plane. Acta Radiol 37:610–613
Wiltse LL, Guyer RD, Spencer CW, Glenn WV, Porter IS (1984) Alar transverse process impingement of the L5 spinal nerve: the far-out syndrome. Spine (Phila Pa 1976) 9:31–41
Elster AD (1989) Bertolotti’s syndrome revisited. Transitional vertebrae of the lumbar spine. Spine (Phila Pa 1976) 14:1373–1377
Luoma K, Vehmas T, Raininko R, Luukkonen R, Riihimaki H (2004) Lumbosacral transitional vertebra: relation to disc degeneration and low back pain. Spine (Phila Pa 1976) 29:200–205
Taskaynatan MA, Izci Y, Ozgul A, Hazneci B, Dursun H, Kalyon TA (2005) Clinical significance of congenital lumbosacral malformations in young male population with prolonged low back pain. Spine (Phila Pa 1976) 30:E210–E213
Bron JL, van Royen BJ, Wuisman PI (2007) The clinical significance of lumbosacral transitional anomalies. Acta Orthop Belg 73:687–695
Chang X, Chen B, Li HY, Han XB, Zhou Y, Li CQ (2014) The safety and efficacy of minimally invasive discectomy: a meta-analysis of prospective randomized controlled trials. Int Orthop 38:1225–1234
Du J, Tang X, Jing X, Li N, Wang Y, Zhang X (2016) Outcomes of percutaneous endoscopic lumbar discectomy via a translaminar approach, especially for soft, highly down-migrated lumbar disc herniation. Int Orthop 40:1247–1252
Fan G, Han R, Gu X, Zhang H, Guan X, Fan Y, Wang T, He S (2017) Navigation improves the learning curve of transforamimal percutaneous endoscopic lumbar discectomy. Int Orthop 41:323–332
Funding
This work was supported by an INHA University Research Grant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Shin, EH., Cho, KJ., Kim, YT. et al. Risk factors for recurrent lumbar disc herniation after discectomy. International Orthopaedics (SICOT) 43, 963–967 (2019). https://doi.org/10.1007/s00264-018-4201-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-4201-7