Abstract
Purpose
Anterior approach was extensively used in surgical treatment of multilevel cervical spondylotic myelopathy. Following anterior decompression, many different reconstructive techniques (multilevel ACDF, hybrid construct and long corpectomy) all had satisfied outcomes. However, there are few studies focusing on the comparison of these three reconstructed techniques. The aim of this retrospective study was to analyze the complications of these three different methods.
Methods
This study retrospectively reviewed the complications in 286 consecutive patients with multilevel CSM who underwent anterior cervical surgery from 2005 to 2010. This case series had 166 men and 120 women whose mean age at surgery was 53.8 years (range from 33 to 74 years). Radiographic evaluation was taken the day after surgery, and the flexion–extension X-rays were added 3, 12 and 24 months postoperatively to evaluate the fusion condition. Preoperative versus postoperative neurologic function and clinical outcome were evaluated using scoring systems such as the Japanese Orthopedic Association (JOA score), Neck Disability Index (NDI score) and 36-Item Short-Form Health Survey (SF-36 score).
Results
There were no significant differences in JOA scores, NDI scores and SF-36 scores of the pairwise comparison among the three groups. The complications in our series included graft migration, collapse or displacement, hoarseness, dysphagia, C5 palsy, cerebral fluid leakage and wound infection. Sixty-one patients developed complications after surgery and the rate of complication was 21.33 %. Patients in the long corpectomy group had the highest rate of complications; the other two groups had a much lower rate of complications by the latest follow-up. The patients in the multilevel ACDF group had the highest fusion rate by the last follow-up. Patients who had C2–3 and C3–4 segments involved had a higher rate of postoperative hoarseness and dysphagia.
Conclusions
Most of the complications of the three reconstructive techniques subsided gradually after conservative treatment; none of them needed revision surgery. The multilevel ACDF approach has the lowest rate of non-union, but a slightly higher morbidity of the laryngeal nerve-related complication if proximal segments were involved. The long corpectomy approach should be selected prudently because of the high rate of complication.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The formulation of optimal surgical treatment in multilevel cervical spondylotic myelopathy (MCSM) has been the subject of much controversy and debates. Anterior (corpectomy, multilevel discectomy), posterior (laminectomy, laminoplasty) and combined anterior and posterior surgical approaches for MCSM patients have all been advocated, and each approach had its own advantages and disadvantages [1, 2]. The aims of surgical treatment for MCSM are decompression of the spinal cord and nerve root, stabilization of the spinal column and restoration of disc space and lordotic alignment [3]. Anterior approach is suitable for patients who mainly have big anterior pathogenic structures and cervical kyphosis [4]. For patients with three-level CSM, two-level corpectomy plus graft fusion with plate fixation has been a longstanding and commonly used approach, but the fusion rate is far from satisfactory. Recently, good outcomes were reported in MCSM patients with other reconstruction techniques, such as multilevel anterior cervical decompression and fusion (ACDF) or corpectomy plus ACDF. However, there is little literature focusing on the comparison of these three reconstruction techniques. Thus, the aims of this retrospective study were analyzing the complications of these three different methods—multilevel ACDF, hybrid construct (one corpectomy plus one ACDF) and long corpectomy (Fig. 1)—and help to select an appropriate procedure for individual patients by understanding the superiority of one procedure over the others.
Materials and methods
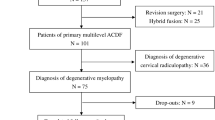
A total of 286 consecutive patients with multilevel CSM underwent anterior cervical surgery from 2005 to 2010 in our department. This case series had 166 men and 120 women, whose mean age at surgery was 53.8 years (range from 33 to 74 years). All patients underwent three-level surgeries. Exclusion criteria were as follows: prior cervical injury history or other neuromuscular diseases; previous cervical spine surgery history; and pending socioeconomic litigations. A classic Smith–Robinson decompression was performed followed by three different reconstructive methods to stabilize the cervical spine and realign the sagittal plane. Decision-making is up to the involved segments in the sagittal and axial planes of the MRI scan, which is associated with clinical symptoms. A total of 103 patients had multilevel ACDF procedure; 96 received a hybrid construct which included one corpectomy plus one ACDF, and 87 had two corpectomies. The titanium meshes or cages filled with autograft bone were used as fusion material. Semi-restricted plates were selected in our series, which included the Slim-loc (Johnson and Johnson Co., Depuy Spine Ltd., Ryhamn, MA) and Zephir plates (Medtronic Sofamor Danek Inc., Memphis, TN). All the patient history was collected; physical examination, anteroposterior and lateral view X-ray film, CT and MRI scans were routinely performed to evaluate the spine cord and/or nerve root compression. After surgery, all the patients were suggested to use a Philadelphia collar for 3 weeks. Patients took radiographic examination the day after surgery, and the flexion–extension X-rays were added in 3, 12 and 24 months post-operatively to evaluate the fusion condition. Based on the previously reported methods, the radiographic fusion was defined as no motion across the fusion site in the flexion–extension X-rays or CT scans and the presence of bridging bony trabeculae between the endplate and the graft [5, 6]. Graft migration was evaluated from the X-rays and MRI scans. All radiographic information was independently evaluated by one spine surgeon (Liu Yang). In addition, the postoperative hoarseness and dysphagia were particularly analyzed according to the different segments involved. Preoperative versus postoperative neurologic function and clinical outcome was evaluated using scoring system which consisted of the Japanese orthopedic association (JOA) score, neck disability index (NDI score) and 36-item short-form health survey (SF-36 score).
All the statistical analysis was performed with SPSS® software (version 16.0; SPSS Inc., Chicago, IL). The quantitative data such as the age, JOA scores, NDI scores and the SF-36 scores are presented as the mean ± standard deviation. Mean comparison in three groups was conducted with single-factor variance analysis, and the pairwise comparison was performed with LSD-t method. A P value less than 0.05 was considered statistically significant.
Results
The demographics of the patients are shown in Table 1. The mean ages of the patients in multilevel ACDF group (group A), hybrid construct group (group B) and long corpectomy group (group C) were 53.48 ± 8.50, 54.36 ± 7.82 and 53.68 ± 7.80, respectively (P > 0.05). The mean follow-up time was 3.6 years (range from 1.5 to 6 years). The detailed information regarding the three groups is shown in Table 1. All the patients in three groups achieved significant neurologic function and clinical outcome improvement, regardless of the different reconstructed techniques selected (Table 2). There were no significant difference in JOA scores, NDI scores and SF-36 scores of the pairwise comparison among the three groups.
The complications in our series include graft migration, collapse or displacement, hoarseness, dysphagia, C5 palsy, cerebral fluid leakage and wound infection during the follow-up time. As showed in Fig. 2, patients in group C had a highest rate of complications. Detailed information of these complications is listed in Table 3.
In group A, there was no case of graft migration or non-union at last follow-up. All the patients had a good solid fusion. Of 96 patients in the group that underwent the hybrid construct, four patients were observed to have a little graft migration at the latest follow-up (Fig. 3). However, these four patients did not have significative clinical symptoms and the graft did not migration unacceptable, none of them needed revision surgery. The fusion rate in group B was 95.83 %. In group C, graft collapse and non-union were observed in seven patients. Only three of them had progressive neck pain and radiculopathy; after using the NSAIDs for 2 weeks the symptoms were relieved. Two patients appeared severe graft migration and non-union, because they had no symptoms and no evidence of progression, they still have been followed (Fig. 4). 91.95 % of the patients in group C achieved radiographic fusion. The patients in multilevel ACDF group had the highest fusion rate at the last follow-up. Postoperative hoarseness was observed in ten patients. Four of these patients were in group A, three patients were in group B and the other three patients were in group C. The multilevel ACDF group had a higher rate of hoarseness than other two groups. Detailed information is listed in Table 3. The multilevel ACDF group also had a higher rate of dysphagia. After the conservative treatment by fog inhalation of 5 mg dexamethasone, chymotrypsin and humidity liquid four times daily, all of these patients’ symptoms subsided gradually. In addition, the patients whose surgical segments involved C2–3 and C3–4 segments had a higher rate of postoperative hoarseness and dysphagia (Table 4). Other complications included C5 palsy, cerebral fluid leakage and wound infection. Neurological deficits appeared in four patients in group A, eight patients in group B and ten patients in group C; they developed a bilateral C5 palsy and recovered by using NSAIDs and glucocorticoid 2 months later. Two patients in multilevel ACDF group and one patient in hybrid construct group had cerebral fluid leakage and recovered after 2 weeks by keeping the supine position and drainage. Two patients experienced wound infection, one of whom underwent hybrid construct and the other received long corpectomy. Both patients were smokers. Satisfactory healing was achieved 1 week after dressing change and wet packing with alcohol.
A 44-year-old male patient complained of difficulty of ambulation and numbness of lower limbs for 3 months. Preoperative cervical X-ray film (a) and MRI scan (b) showed C3/4, C4/5 and C5/6 disc herniation and high signal intensity at C5/6 level on T2-weighted image. He underwent a C3/4 discectomy and C5 corpectomy following anterior decompression. Postoperative radiography the day after surgery demonstrates a good position of implant (c). At 2-year follow-up, the lateral cervical plain film showed screw breakage. No revision surgery was required due to absence of severe clinical symptoms
A 55-year-old female patients complained of numbness of both hands and difficulty of ambulation for 10 years. Preoperative cervical X-ray film (a) and MRI scan (b) showed C3/4, C4/5 and C5/6 disc herniation combined with high signal intensity at C5/6 level on T2-weighted image. Two corpectomies of C4 and C5 were preformed following anterior decompression. Postoperative radiography the day after surgery showed a satisfactory position of instrumentation (c). Significant migration of titanium mesh was observed at 6-month follow-up (d). Because no severe clinical symptoms manifested, further follow-up is needed
Totally, 61 patients developed complications after surgery. The rate of complication was 21.33 %. Patients in long corpectomy group had a highest rate of complication, while the other two groups had comparatively much lower rate of complication at the last follow-up.
Discussion
Surgical treatment of multilevel cervical spondylotic myelopathy is recommended for patients who have progressive neurologic function impairment without remission of conservative treatment. The choice of surgical approach of MCSM has been a controversial subject. Until the 1960s, the principal means of surgical treatment of MCSM were posterior approaches which included laminectomy and laminoplasty [7]. In recent years, anterior approach was widely used in surgical treatment of MCSM as a radical procedure in decompressing the spinal cord and nerve root by directly removing the anterior pathogenic structures such as protruded discs, osteophyte or ossification lesion [4]. Nevertheless, the inevitable complications of anterior approach still deserve our attention. And the choice of reconstruction technique after multilevel anterior cervical decompression is also undefined [8]. In our series of 286 MCSM patients that underwent three different reconstructive techniques, by the latest follow-up time there were 61 patients that had different kinds of complications, the total rate of complications was 21.33 %. Complications in our series included graft migration, collapse or displacement, hoarseness, dysphagia, C5 palsy, cerebral fluid leakage and infection.
The essential purpose of surgical approach to MCSM is decompressing the spine cord and nerve root as well as maintaining the stability of cervical spine. Regardless of what reconstruction approach was taken, maximizing the fusion rate was the most fundamental goal. The inevitable complication of anterior approach of surgical treatment of MCSM was graft migration or non-union. Bohlman et al. [9] reported a solid fusion in 55 of 62 of the patients who underwent single-level ACDF operation (89 %), as compared with 43 of 59 multilevel ACDF (72 %). Previous researches also have proved that an increased number of treated segments are an important risk factor for non-union in multilevel anterior cervical fusion procedures [10, 12]. The controversy still exists as to which reconstruction approach can make the highest fusion rate. Hilibrand AS et al. [12] reported that 19 of 33 patients who underwent multilevel ACDF had a solid arthrodesis (58 %), as compared with 55 of 59 patients underwent long corpectomy (93 %). They proved the rate of successful fusion after long corpectomy with strut grafting was significantly higher than multilevel ACDF patients. And long corpectomy with strut grafting only requires two graft-to-host bony surfaces, but multilevel ACDF requires two bony surfaces for each level, they thought the increased number of bony surface may lead to the decreased of solid fusion rate. On the contrary, Khoueir P et al. [11] revealed there was no statistically significant difference in the rate of pseudarthrosis formation in terms of number of interfaces. Some researchers also studied the difference of fusion rate between hybrid construction patients and long corpectomy patients; they found insignificant difference between hybrid decompression group (100 %) and two-level corpectomy group (94 %) [13]. In our study, the fusion rate was different in accordance with the literature. We found the fusion rate was 100 % in multilevel ACDF group. In the hybrid construct group, four of 96 patients had graft migration at the latest follow-up; the fusion rate was 95.83 %. The fusion rate in long corpectomy group was lowest, only 91.95 %. We thought although there are many interfaces between the vertebral bodies and interbody grafts, multilevel ACDF provide more fixation points to hold the construct rigidly in place for longer constructs. In contrast, corpectomy and strut grafts provide only two interfaces between the vertebral bodies and the graft at the remaining cephalic and caudal vertebral bodies.
Dysphagia and hoarseness were recognized as common complications after multilevel anterior cervical surgery [14]. Direct surgical trauma, postoperative edema and neuropraxia caused by trachea and esophagus traction may be the possible mechanisms [15]. Beutler et al. [16] investigated 328 patients who underwent anterior cervical procedures and found the incidence of postoperative nerve injury was 2.1 % (four of 187) in anterior cervical discectomy group and 3.5 % (five of 141) in anterior cervical corpectomy group. Riley LH 3rd et al. [17] reported the incidence of self-reported post-ACDF dysphasia was 28 % (128 of 454) at the 3rd month after surgery. They also found the patients with longer duration of neck or shoulder pain and the multilevel ACDF procedure had a higher risk of postoperative dysphagia. In our research, the incidence of postoperative dysphagia was 5.82 % (six of 103) in multilevel ACDF group, 5.21 % (five of 96) in hybrid construct group and 2.30 % (two of 87) in long corpectomy group. The incidence of hoarseness in three groups was 3.88, 3.13 and 3.45 %, respectively. Patients in multilevel ACDF group had the highest incidence of dysphagia and hoarseness. During the procedure of multilevel ACDF, the stretch of soft tissue and nerve was severer than the other two reconstructed techniques. Our results were similar to that of previous literature. The cause of these complications were thought to be related with the time-consuming and sagittal alignment restoration, more operating time and better sagittal alignment restoration may lead to severer dysphagia and hoarseness. We also found surgical intervention involved C2–3 and C3–4 segments increase the rate of postoperative hoarseness and dysphagia. Laryngeal nerve mostly walks through C2–C4 level, so stretch of laryngeal nerve during the operation may cause this appearance. In our series, four patients in multilevel ACDF group, eight patients in hybrid construct group and ten patients in long corpectomy group appeared a bilateral C5 palsy symptom. Postoperative transient segmental motor palsy such as C5 palsy is developed as an important complication after cervical decompression surgery, the average incidence was reported as 4.6 % (range from 0 to 30 %) [18]. Despite that the pathogenesis of C5 palsy is not completely clear still now, we found most of the patients who appeared C5 palsy were in long corpectomy group and the procedure of multilevel corpectomy may lead to significant drift of spinal cord away ventral side.
Totally, the complications of the multilevel ACDF, hybrid construct and long corpectomy are still actual problems and should not be neglected. Most of the complications subsided gradually after the conservative treatment; none of them needed revision surgery. The multilevel ACDF approach has the lowest rate of non-union, but demonstrated a little bit higher morbidity of laryngeal nerve-related complication if proximal segments were involved. Long corpectomy approach should be selected prudently because of high rate of complication.
References
Hillard VH, Apfelbaum RI (2006) Surgical management of cervical myelopathy: indications and techniques for multilevel cervical discectomy. Spine J 6(6 Suppl):242S–251S
Lin Q, Zhou X, Wang X, Cao P, Tsai N, Yuan W (2011) A comparison of anterior cervical discectomy and corpectomy in patients with multilevel cervical spondylotic myelopathy. Eur Spine J (epub ahead of print)
Lian XF, Xu JG, Zeng BF, Zhou W, Kong WQ, Hou TS (2010) Noncontiguous anterior decompression and fusion for multilevel cervical spondylotic myelopathy: a prospective randomized control clinical study. Eur Spine J 19(5):713–719
Liu T, Xu W, Cheng T, Yang HL (2011) Anterior versus posterior surgery for multilevel cervical myelopathy, which one is better? A systematic review. Eur Spine J 20(2):224–235
Papadopoulos EC, Huang RC, Girardi FP, Synnott K, Cammisa FP Jr. (2006) Three-level anterior cervical discectomy and fusion with plate fixation: radiographic and clinical results. Spine 31(8):897–902
Chang SW, Kakarla UK, Maughan PH, DeSanto J, Fox D, Theodore N, Dickman CA, Papadopoulos S, Sonntag VK (2010) Four-level anterior cervical discectomy and fusion with plate fixation: radiographic and clinical results. Neurosurgery 66(4):639–646 discussion 646–7
Bapat MR, Chaudhary K, Sharma A, Laheri V (2008) Surgical approach to cervical spondylotic myelopathy on the basis of radiological patterns of compression: prospective analysis of 129 cases. Eur Spine J 17(12):1651–1663
Wei-bing X, Wun-Jer S, Gang L, Yue Z, Ming-xi J, Lian-shun J (2009) Reconstructive techniques study after anterior decompression of multilevel cervical spondylotic myelopathy. J Spinal Disord Tech 22(7):511–515
Bohlman HH, Emery SE, Goodfellow DB, Jones PK (1993) Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg Am 75(9):1298–1307
Emery SE, Bolesta MJ, Banks MA, Jones PK (1994) Robinson anterior cervical fusion comparison of the standard and modified techniques. Spine (Phila Pa 1976) 19(6):660–663
Khoueir P, Oh BC, DiRisio DJ, Wang MY (2007) Multilevel anterior cervical fusion using a collagen-hydroxyapatite matrix with iliac crest bone marrow aspirate: an 18-month follow-up study. Neurosurgery 61(5):963–970 discussion 970–971
Hilibrand AS, Fye MA, Emery SE, Palumbo MA, Bohlman HH (2002) Increased rate of arthrodesis with strut grafting after multilevel anterior cervical decompression. Spine (Phila Pa 1976) 27(2):146–151
Liu Y, Yu KY, Hu JH (2009) Hybrid decompression technique and two-level corpectomy are effective treatments for three-level cervical spondylotic myelopathy. J Zhejiang Univ Sci B 10(9):696–701
Baron EM, Soliman AM, Gaughan JP, Simpson L, Young WF (2003) Dysphagia, hoarseness, and unilateral true vocal fold motion impairment following anterior cervical discectomy and fusion. Ann Otol Rhinol Laryngol 112(11):921–926
Apfelbaum RI, Kriskovich MD, Haller JR (2000) On the incidence, cause, and prevention of recurrent laryngeal nerve palsies during anterior cervical spine surgery. Spine 25(22):2906–2912
Beutler WJ, Sweeney CA, Connolly PJ (2001) Recurrent laryngeal nerve injury with anterior cervical spine surgery risk with laterality of surgical approach. Spine (Phila Pa 1976) 26(12):1337–1342
Riley LH 3rd, Skolasky RL, Albert TJ, Vaccaro AR, Heller JG (2005) Dysphagia after anterior cervical decompression and fusion: prevalence and risk factors from a longitudinal cohort study. Spine (Phila Pa 1976) 30(22):2564–2569
Sakaura H, Hosono N, Mukai Y, Ishii T, Yoshikawa H (2003) C5 palsy after decompression surgery for cervical myelopathy: review of the literature. Spine (Phila Pa 1976) 28(21):2447–2451
Conflict of interest
The authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Author information
Authors and Affiliations
Corresponding author
Additional information
M. Qi contributed equally to the article.
Rights and permissions
About this article
Cite this article
Liu, Y., Qi, M., Chen, H. et al. Comparative analysis of complications of different reconstructive techniques following anterior decompression for multilevel cervical spondylotic myelopathy. Eur Spine J 21, 2428–2435 (2012). https://doi.org/10.1007/s00586-012-2323-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-012-2323-y