Abstract
Purpose
Although many meta-analyses have been performed to compare total disc replacement (TDR) and fusion for treating lumbar degenerative disc disease (LDDD), their findings are inconsistent. This study aimed to conduct a systematic review of overlapping meta-analyses comparing TDR with fusion for treating LDDD, to assist decision makers in selection among conflicting meta-analyses, and to provide treatment recommendations based on the best available evidence.
Methods
This study was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement. Multiple databases were comprehensively searched for meta-analyses comparing TDR with fusion for treating LDDD. Meta-analyses only comprising randomised controlled trials (RCTs) were included. Two authors independently assessed meta-analysis quality and extracted data. The Jadad decision algorithm was used to ascertain which meta-analyses represented the best evidence.
Results
A total of five meta-analyses were included. All these studies only included RCTs were determined as Level-II evidence. The scores of Assessment of Multiple Systematic Reviews (AMSTAR) ranged from 6 to 9 (median 7). A high-quality Cochrane review was chosen according to the Jadad algorithm. This best available evidence found that statistical significances were observed between TDR and fusion for LDDD regarding disability, pain relief, and pain in the short term, but it was not over clinically important differences. The prevent effects on adjacent segment and facet joint degeneration, as the primary goal of adopting TDR stated by the manufacturers, were not appropriately evaluated.
Conclusions
There is discord in results from meta-analyses that assessed TDR and fusion for LDDD. According to this systematic review of overlapping meta-analyses comparing TDR and fusion for LDDD, the current best available evidence suggests that TDR may be an effective technique for the treatment of selected patients with LDDD, and is at least equal to lumbar fusion in the short term. However, considering that disadvantages may appear after years, spine surgeons should be cautions about performing TDR on a large scale.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Lumbar degenerative disc disease (LDDD) is the leading reason for low back pain, which is a major health problem with significant economic burden [1, 2]. Lumbar fusion has been a gold standard procedure for treating LDDD unresponsive to conservative treatment. However, stiffness and adjacent segment degeneration may lead to poor clinical outcomes and more complications in the long term [3, 4]. As an alternative technique, total disc replacement (TDR) has received more and more attentions in recent years. This procedure is designed to maintain the motion of the operated level and to prevent adjacent segment degeneration [5, 6]. However, whether TDR or lumbar fusion is the optimal procedure for treating LDDD is still unclear.
Several randomised clinical trials (RCTs) have been conducted to compare TDR with lumbar fusion, but their findings are conflicted regarding which procedure is better [7–14]. In light of this, many meta-analyses of RCTs, representing the highest level of evidence, have been published to compare these two procedures for the treatment of LDDD. However, these overlapping meta-analyses also showed discordant findings [15–19]. For example, Nie et al. [17] concluded that TDR shows a significant superiority for treating LDDD compared with fusion. However, Yajun et al. [18] did not demonstrate the significant superiority of TDR in comparison to lumbar fusion in their study. These inconsistent findings have resulted in uncertainty for decision makers regarding the surgical treatments of LDDD.
In recent years, systematic reviews of overlapping meta-analyses have been widely published in many medical fields [20–23]. These studies help to select the highest quality level of evidence for decision-making by evaluating meta-analyses with the discordant results on certain topic [20–23]. However, to the best of our knowledge, there is no systematic review of overlapping meta-analyses investigating the relative effects between TDR and fusion for LDDD. The objective of this study was to perform a systematic review of overlapping meta-analyses regarding TDR versus lumbar fusion for the treatment of LDDD, to assist decision makers in selection among conflicting meta-analyses, and to provide treatment recommendations based on the best available evidence.
Materials and methods
This study was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) statement [24]. The design of this study was based on previous similar publications [20–23].
Literature search
On July 10, 2015, the literature databases, including PubMed, EMBASE, and Cochrane Library, were systematically retrieved. The following keywords were used, including lumbar, arthroplasty, prosthesis, replacement, arthrodesis, fusion, low back pain, intervertebral disc degeneration, degenerative disc disease, systematic review, and meta-analysis. The search was independently performed by two authors, with the limitation of English language. The references of the included studies were also checked to find potential meta-analyses. The titles and abstracts were first reviewed, and the full texts were acquired if the information was not enough. Disagreements were settled by discussion, and a third author was consulted when necessary.
Eligibility criteria
The inclusion criteria of this systematic review were: (1) comparing TDR with fusion for treating LDDD; (2) meta-analysis exclusively including RCTs; (3) at least 1 outcomes (e.g., functional scores and complications). The narrative review, meetings abstract, correspondence, meta-analysis comprising non-RCTs, and systematic review without meta-analysis conducted were excluded.
Data extraction
Two authors independently extracted the following data from the included studies: first author, year of publications, databases for search, primary study design, the number of RCTs included, heterogeneity or subgroup analyses of primary study, and meta-analysis results. When disagreements occurred between the two authors, a third author was consulted.
Quality assessment
The methodological quality was evaluated by the Oxford Levels of Evidence [25] and the Assessment of Multiple Systematic Reviews (AMSTAR) instrument [26]. AMSTAR has been proved as a methodological assessment tool with good reliability, validity, and responsibility [27, 28]. It is widely used to assess the quality of systematic reviews [20–23]. Two authors independently evaluated the quality of the included meta-analyses. Disagreements between authors were settled by discussion, and a third author was consulted if necessary.
Application of Jadad decision algorithm
The Jadad decision algorithm was applied to investigate the source of inconsistence among systematic reviews, comprising differences in clinical question, inclusion and exclusion criteria, data extraction, quality assessment, data pooling, and statistical analysis [29]. It had been widely conducted to provide treatment recommendations among meta-analyses with discordant results [20–23, 29]. This algorithm was independently applied by three authors, who reached a consensus regarding which meta-analysis provided the best available evidence.
Results
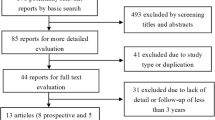
Literature search
A flow chart of the study selection is shown in Fig. 1. A total of 502 titles were found from the literature source. Five meta-analyses met the inclusion criteria [15–19]. The characteristics of these included studies are listed in Table 1. These studies were published between 2010 and 2015. The primary studies of included meta-analyses were published between 2005 and 2011, and the number of primary trials ranged from 5 to 7 (Table 2).
Search methodology
Three of the included meta-analyses only included English literature [15–17], and the other two studies had no language restriction [18, 19]. The databases of Embase and Medline (PubMed) were searched in all included meta-analyses, whether Cochrane Library, OVID, and BIOSIS were included in search strategy that was inconsistent among the studies. Search methodology used in the included meta-analyses is shown in Table 3.
Methodological quality
All meta-analyses included only RCTs, and were determined as Level-II evidence according to Oxford Levels of Evidence (Table 4). Only one meta-analysis showed that the GRADE was conducted in their study [19]. The results of AMSTAR scores for the included meta-analyses are listed in Table 5, ranging from 6 to 9 (median 7). A Cochrane review with 9 scores of AMSTAR was the highest quality study [19].
Heterogeneity assessment
The I 2 statistic value, as a measurement tool for investigating the interstudy variability, was used to evaluate the heterogeneity of study in each meta-analysis (Table 6) [15–19]. A total of three studies performed sensitivity analyses according to methodological quality [16, 18, 19] (Table 4). One meta-analysis did not conduct sensitivity or subgroup analysis [15] (Table 6).
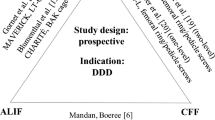
Results of Jadad decision algorithm
Which meta-analysis represented the best available evidence among the five included meta-analyses was investigated following the Jadad decision algorithm [29]. The meta-analysis results of the included studies are show in Fig. 2. Based on that the included studies investigated the same study question did not comprise the same trials, and the selection criteria were discordant, the Jadad decision algorithm indicated that the best available evidence should be chosen according to the publication status and the methodological quality of primary trials, language restrictions, and analysis of data on individual patients. Hence, a high-quality Cochrane review was selected (Fig. 3) [19]. This study concluded that statistical significances were observed between TDR and fusion for LDDD regarding disability, pain relief, and pain in the short term, but it was not over clinically important differences. The preventative effects on adjacent segment disease and facet joint degeneration, as the primary goal of adopting TDR stated by the manufacturers, were not appropriately evaluated [19].
Discussion
To the best of our knowledge, this is the first systematic review of overlapping analyses regarding TDR versus fusion for LDDD. This study may help the surgeons to understand the current best evidence on this topic, and assist decision makers in selection among conflicting meta-analyses. In this study, five meta-analyses [15–19] were included in terms of a comprehensive literature search. This study found that most of meta-analysis identified by the literature search was published within similar period, but they did not comprise the same primary trials, and not provide the same conclusions for the treatment of LDDD [15–19]. According to the Jadad decision algorithm, Jacobs et al. [19] was selected as the current best available evidence on this topic. This systematic review of overlapping meta-analyses suggests that TDR may be an effective intervention to treat the selected LDDD, and is at least equal to fusion in the short term. However, given that disadvantages may appear after years, spine surgeons should be serious about performing TDR on a large scale.
Our study demonstrated that there were discordant results among the included meta-analyses. Some meta-analyses [18, 19] showed that TDR did not show significant superiority for the treatment of LDDD compared with fusion. Therefore, the benefits of motion preservation are still unable to be concluded. However, the other meta-analyses [15–17] concluded that TDR showed significant safety and efficacy comparable to lumbar fusion. The possible sources of inconsistence among meta-analyses have been analysed and reported by Jadad et al. [29], including the clinical question, study selection and inclusion, data extraction, assessment of study quality, assessment of the ability to combine studies, and statistical methods for data synthesis. Moreover, a decision algorithm was also designed to choose the highest quality level of evidence from currently discordant systematic reviews [29]. This decision tool adopted in this study was widely used to find the best available evidence among overlapping systematic reviews [20–23].
Jacobs et al. [19] was the current best available evidence on the comparison of TDR and fusion for LDDD. It demonstrated that TDR was superior to lumbar fusion in Oswestry disability index, visual analogue scale, back pain, patient satisfaction, implant motion, and subsidence [19]. There were no differences between TDR and lumbar fusion in leg pain, proportion of full-time and part-time work, reoperation rate, blood loss, radiographic loosening, and adjacent segment and facet joint degeneration. However, Jacobs et al. [19] believed that the current meta-analyses did not properly evaluate adjacent segment and facet joint degeneration, which is a defect as this is the reason that the disc prosthesis was manufactured. Thus, Jacobs et al. [19] concluded that because disadvantages may appear after years, spine surgeons should be serious about applying TDR on a large scale, despite TDR may be an effective technique for treating selected patients with LDDD and is at least equal to fusion in the short term.
Although Jacobs et al. [19] provided the best evidence, however, it should be recognised that this study had several factors that influenced their findings. First, most of their results were pooled by less than four primary RCTs, although six studies were included in their study. This may be mainly because different studies adopt different outcome measures. The results could not be pooled using all the data in the included studies. Therefore, more RCTs with similar outcome assessments should be performed in the future. Second, many new techniques, such as minimally invasive spine surgery [30, 31], have been increasingly used in treating LDDD in recent years. These procedures may further improve the outcomes of spine surgery for the treatment of LDDD [31, 32]. However, these new techniques could not be well discussed in their study, due to a few RCTs was included. Third, their study was published in 2012 and the latest included RCTs was published in 2011. Their study could not include newer RCTs published in recent years, which may strengthen or weaken the conclusions. Therefore, the meta-analysis regarding TDR versus fusion for the treatment of LDDD should be updated in the futher.
The included meta-analyses were published in five journals, including three orthopaedic journals, European Spine Journal, International Orthopaedics, and Archives of Orthopaedic and Trauma Surgery. The study from Jacobs et al. [19] was chosen according to the Jadad decision algorithm, which was published in Cochrane Database of Systematic Reviews. This journal is a professional journal in the field of evidence-based medicine, and has the highest impact factor among the included journals. It indicates that some high-level study in the evidence-based orthopaedics may not definitely published in the professional orthopaedic journals.
There are several limitations in this study. First, the literature search was limited in articles published using English language. Non-English literature could not included in this systematic review, despite multiple databases were searched. Second, to get the highest level of evidence, meta-analyses only comprising RCTs were included in this study. However, all the included studies were Level II of evidence. Therefore, this systematic review could not provide treatment recommendations based on Level-I evidence. Third, this study could not assess the long-term results, because almost all of the primary studies only have data for 2 years, and the long-term complications, such as adjacent segment diseases, may be well assessed in more than 10 years follow-up.
Conclusion
This is the first systematic review of overlapping meta-analyses on comparing TDR with fusion for the treatment of LDDD. This systematic review showed that there are conflicting results among these overlapping meta-analyses. Based on this systematic review of overlapping meta-analyses, the best available evidence indicated that TDR compared with fusion for LDDD had statistically, but not clinically, significant superiority regarding disability, pain relief, and quality of life in a selected group of patients in the short term. The prevention of adjacent segment and facet joint degeneration, as the primary reason for adopting TDR noted by the manufactures, was not appropriately evaluated. Hence, considering that disadvantages may appear after years, spine surgeons should be serious about applying TDR on a large scale, despite TDR may be an effective technique for treating selected patients with LDDD and is at least equal to lumbar fusion in the short term.
Change history
08 September 2018
The authors declare that when writing their article [1] they referenced two previously published papers [2, 3]. Several sentences on pages 807, 808, and 813 were similar to sentences from these two previously published articles.
References
van Tulder MW, Koes BW, Bouter LM (1995) A cost-of-illness study of back pain in The Netherlands. Pain 62(2):233–240
Walker BF, Muller R, Grant WD (2003) Low back pain in Australian adults: the economic burden. Asia Pac J Public Health 15(2):79–87
Frelinghuysen P, Huang RC, Girardi FP, Cammisa FP Jr (2005) Lumbar total disc replacement part I: rationale, biomechanics, and implant types. Orthop Clin N Am 36(3):293–299
Kalanithi PS, Patil CG, Boakye M (2009) National complication rates and disposition after posterior lumbar fusion for acquired spondylolisthesis. Spine (Phila Pa 1976) 34(18):1963–1969
Gamradt SC, Wang JC (2005) Lumbar disc arthroplasty. Spine J 5(1):95–103
Auerbach JD, Jones KJ, Milby AH, Anakwenze OA, Balderston RA (2009) Segmental contribution toward total lumbar range of motion in disc replacement and fusions: a comparison of operative and adjacent levels. Spine (Phila Pa 1976) 34(23):2510–2517
Delamarter RB, Bae HW, Pradhan BB (2005) Clinical results of ProDisc-II lumbar total disc replacement: report from the United States clinical trial. Orthop Clin N Am 36(3):301–313
Moreno P, Boulot J (2008) Comparative study of short-term results between total artificial disc prosthesis and anterior lumbar interbody fusion. Rev Chir Orthop Reparatrice Appar Mot 94(3):282–288
Gornet MF, Burkus JK, Dryer RF, Peloza JH (2011) Lumbar disc arthroplasty with Maverick disc versus stand-alone interbody fusion: a prospective, randomized, controlled, multicenter investigational device exemption trial. Spine (Phila Pa 1976) 36(25):E1600–E1611
Sasso RC, Foulk DM, Hahn M (2008) Prospective, randomized trial of metal-on-metal artificial lumbar disc replacement: initial results for treatment of discogenic pain. Spine (Phila Pa 1976) 33(2):123–131
Delamarter R, Zigler JE, Balderston RA, Cammisa FP, Goldstein JA, Spivak JM (2011) Prospective, randomized, multicenter Food and Drug Administration investigational device exemption study of the ProDisc-L total disc replacement compared with circumferential arthrodesis for the treatment of two-level lumbar degenerative disc disease: results at twenty-four months. J Bone Joint Surg Am 93(8):705–715
Blumenthal S, McAfee PC, Guyer RD, Hochschuler SH, Geisler FH, Holt RT, Garcia R Jr, Regan JJ, Ohnmeiss DD (2005) A prospective, randomized, multicenter Food and Drug Administration investigational device exemptions study of lumbar total disc replacement with the CHARITE artificial disc versus lumbar fusion: part I: evaluation of clinical outcomes. Spine (Phila Pa 1976) 30(14):1565–1575 (discussion E1387–E1591)
Zigler J, Delamarter R, Spivak JM, Linovitz RJ, Danielson GO 3rd, Haider TT, Cammisa F, Zuchermann J, Balderston R, Kitchel S, Foley K, Watkins R, Bradford D, Yue J, Yuan H, Herkowitz H, Geiger D, Bendo J, Peppers T, Sachs B, Girardi F, Kropf M, Goldstein J (2007) Results of the prospective, randomized, multicenter Food and Drug Administration investigational device exemption study of the ProDisc-L total disc replacement versus circumferential fusion for the treatment of 1-level degenerative disc disease. Spine (Phila Pa 1976) 32(11):1155–1162 (discussion 1163)
Berg S, Tullberg T, Branth B, Olerud C, Tropp H (2009) Total disc replacement compared to lumbar fusion: a randomised controlled trial with 2-year follow-up. Eur Spine J 18(10):1512–1519
Rao MJ, Cao SS (2014) Artificial total disc replacement versus fusion for lumbar degenerative disc disease: a meta-analysis of randomized controlled trials. Arch Orthop Trauma Surg 134(2):149–158
Wei J, Song Y, Sun L, Lv C (2013) Comparison of artificial total disc replacement versus fusion for lumbar degenerative disc disease: a meta-analysis of randomized controlled trials. Int Orthop 37(7):1315–1325
Nie H, Chen G, Wang X, Zeng J (2015) Comparison of total disc replacement with lumbar fusion: a meta-analysis of randomized controlled trials. J Coll Physicians Surg Pak 25(1):60–67
Yajun W, Yue Z, Xiuxin H, Cui C (2010) A meta-analysis of artificial total disc replacement versus fusion for lumbar degenerative disc disease. Eur Spine J 19(8):1250–1261
Jacobs W, Van der Gaag NA, Tuschel A, de Kleuver M, Peul W, Verbout AJ, Oner FC (2012) Total disc replacement for chronic back pain in the presence of disc degeneration. Cochrane Database Syst Rev 9:CD008326
Mascarenhas R, Cvetanovich GL, Sayegh ET, Verma NN, Cole BJ, Bush-Joseph C, Bach BR Jr (2015) Does double-bundle anterior cruciate ligament reconstruction improve postoperative knee stability compared with single-bundle techniques? A systematic review of overlapping meta-analyses. Arthroscopy 31(6):1185–1196
Zhao JG, Wang J, Wang C, Kan SL (2015) Intramedullary nail versus plate fixation for humeral shaft fractures: a systematic review of overlapping meta-analyses. Medicine (Baltimore) 94(11):e599
Mascarenhas R, Chalmers PN, Sayegh ET, Bhandari M, Verma NN, Cole BJ, Romeo AA (2014) Is double-row rotator cuff repair clinically superior to single-row rotator cuff repair: a systematic review of overlapping meta-analyses. Arthroscopy 30(9):1156–1165
Zhao JG, Wang J, Long L (2015) Surgical versus conservative treatments for displaced midshaft clavicular fractures: a systematic review of overlapping meta-analyses. Medicine (Baltimore) 94(26):e1057
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6(7):e1000100
Wright JG, Swiontkowski MF, Heckman JD (2003) Introducing levels of evidence to the journal. J Bone Joint Surg Am 85-A(1):1–3
Shea BJ, Grimshaw JM, Wells GA, Boers M, Andersson N, Hamel C, Porter AC, Tugwell P, Moher D, Bouter LM (2007) Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol 7:10
Shea BJ, Hamel C, Wells GA, Bouter LM, Kristjansson E, Grimshaw J, Henry DA, Boers M (2009) AMSTAR is a reliable and valid measurement tool to assess the methodological quality of systematic reviews. J Clin Epidemiol 62(10):1013–1020
Shea BJ, Bouter LM, Peterson J, Boers M, Andersson N, Ortiz Z, Ramsay T, Bai A, Shukla VK, Grimshaw JM (2007) External validation of a measurement tool to assess systematic reviews (AMSTAR). PLoS One 2(12):e1350
Jadad AR, Cook DJ, Browman GP (1997) A guide to interpreting discordant systematic reviews. CMAJ 156(10):1411–1416
Phan K, Rao PJ, Kam AC, Mobbs RJ (2015) Minimally invasive versus open transforaminal lumbar interbody fusion for treatment of degenerative lumbar disease: systematic review and meta-analysis. Eur Spine J 24(5):1017–1030
Hoff EK, Strube P, Pumberger M, Zahn RK, Putzier M (2016) ALIF and total disc replacement versus 2-level circumferential fusion with TLIF: a prospective, randomized, clinical and radiological trial. Eur Spine J 25(5):1558–1566
Noshchenko A, Hoffecker L, Lindley EM, Burger EL, Cain CM, Patel VV (2015) Long-term treatment effects of lumbar arthrodeses in degenerative disk disease: systematic review with meta-analysis. J Spinal Disord Tech 28(9):E493–E521
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has any potential conflict of interest.
Funding
This study was supported by the Funding of Health and Family Planning Commission of Wuhan Municipality (No. WX15B11).
Additional information
F. Ding and Z. Jia contributed equally to this work.
Rights and permissions
About this article
Cite this article
Ding, F., Jia, Z., Zhao, Z. et al. Total disc replacement versus fusion for lumbar degenerative disc disease: a systematic review of overlapping meta-analyses. Eur Spine J 26, 806–815 (2017). https://doi.org/10.1007/s00586-016-4714-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-016-4714-y