Abstract
Background context
Although pain is generally regarded as originating in the lumbar spine, it has been estimated that in 15–30 % of patients, LBP originates from the sacroiliac joint (SIJ).
Purpose
To determine whether sacroiliac joint fusion (SIJF) for LBP is effective in reducing pain when the SIJ is known to be the pain generator.
Study design/setting
Systematic review and meta-analysis.
Methods
A systematic literature review and meta-analysis was performed of observational studies describing outcome of SIJF in patients with LBP. Outcome measures were VAS pain, ODI, SF-36 PCS/MCS and Majeed score. The following databases were searched: PubMed, Web of Science, Embase, Medline and Google scholar. The methodological quality of selected studies was assessed using the National Heart Lung and Blood Institute case series quality assessment tool. Meta-analysis was used to combine the studies for each outcome and forest plots were prepared. Outcomes were expressed as mean difference (MD).
Results
Six studies were included in the meta-analysis with a mean follow-up of 17.6 months. All outcomes showed statistical and clinical improvement (VAS pain MD: 54.8; 95 % CI 48.6, 61.0; n = 380; p < 0.001, ODI MD: 14.5; 95 % CI 8.4, 20.6; n = 102; p < 0.001, SF-36 PCS MD: -19.5; 95 % CI -24.7, -14.2; n = 140; p < 0.001, SF-36 MCS MD: −8.5; 95 % CI −12.9, −4.1; n = 198; p < 0.001 and Majeed score MD: −35.4; 95 % CI −48.5, −22.2; n = 140; p < 0.001).
Conclusions
SIJF appears to be a satisfactory procedure for alleviating pelvic girdle pain.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Low back pain (LBP) is a major public health problem and the cause of much misery and disability. Although pain is generally regarded as originating in the lumbar spine, it has been estimated that in 15–30 % of patients LBP originates from the sacroiliac joint (SIJ) [1]. Pelvic girdle pain (PGP) is defined as pain experienced between the posterior iliac crest and gluteal fold [2]. Poor outcome after spinal fusion for LBP may be due to incorrect diagnosis of the spine as the pain source. Once non-operative treatments have been exhausted and the SIJ has been determined as the source of the PGP by physical exam and SIJ injection, and once the extra-articular ligaments and nerves have been excluded as the pain source, surgical intervention may be considered. Sacroiliac joint fusion (SIJF) can be performed using a variety of approaches and techniques, both open and minimally invasive.
There have been a number of reports that have studied SIJF surgery outcome in patients with LBP. Schutz et al. [3] in a series of 17 patients found unfavourable outcome for bilateral SIJF using bone graft and internal fixation. Eighty-two percent of patients had poor outcome at mean follow-up of 39 months. In contrast, other reports have contradicted these findings showing a statistically and clinically significant improvement. Kibsgard et al. [4] in a series of eight patients found the majority had good outcome at 12 months follow-up. Sachs et al. [5] in a series of 40 patients found all but one had a clinically and statistically significant improvement in outcome at 1 year. Similarly, a recent systematic review by Zaidi et al. [6] concluded that SIJF is beneficial in a carefully selected subset of patients where the pain source has been accurately diagnosed as originating from the SIJ.
Meta-analysis has become an accepted research methodology for quantitatively integrating the results of a collection of studies, some of which may be contradictory, in an unbiased way. Because there have been no meta-analyses of outcome of SIJF in patients with PGP, our aim was to determine whether SIJF, is on the whole, a satisfactory procedure for PGP when the pain source originates from the SIJ.
Materials and methods
A detailed protocol was prepared in accordance with the guidelines described in the Cochrane handbook for systematic reviews of interventions [7]. The review team consisted of two spinal surgeons (KL, SA) and an epidemiologist (RP).
Study selection criteria
Types of studies
Prospective and retrospective observational studies of adults over 16 years suffering from LBP attributed to the SIJ.
Types of interventions
Any type of SIJF. Both standard and minimally invasive surgery (MIS) procedures were included.
Types of outcomes
The primary outcome measure was pain. The secondary outcome measures were Oswestry Disability Index (ODI), Majeed score [8] and SF-36 Physical (PCS) and Mental (MCS) component scores. Data on complications was also extracted.
Exclusion criteria were general discussion papers not presenting original data, fusion for fracture and animal studies.
Literature search
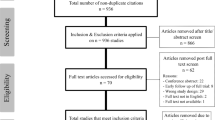
Academic and grey literature was searched with no language restrictions. Electronic searches of on-line databases used the search terms listed below. Any articles that were unsuitable were excluded in the early stages on the basis of their title and abstract whilst the decision to exclude or include articles was made from a review of the full paper. RefWorks 2.0 on-line reference management software [9] was used to store relevant papers as their titles and abstracts. The number of articles included and excluded was noted in a flow chart (Fig. 1).
In addition articles in-press and published ahead of print, where available on the internet, were searched for in the following journals: Spine, The Spine Journal, European Spine Journal, The Bone and Joint Journal (Br & Am), Journal of Spinal Disorders and Techniques, Joint Bone Spine. These articles may not yet have been entered into the searchable databases.
The following databases were searched:
-
Embase 1974 to 10/12/2014
-
Medline 1946 to present 10/12/2014
-
Web of Science to 10/12/2014
-
PubMed to 10/12/2104
-
Cochrane Library to 10/12/2014
-
Google Scholar on 10/12/2014
Synonyms and boolean logic of search: sacroiliac joint AND (fusion OR arthrodesis) AND back pain.
Manual searches of reference lists in relevant papers were also carried out to identify any additional studies missed during the electronic searches.
Study selection
Two authors (KL and RP) applied the search strategy independently and after removing irrelevant studies and duplicates there were 21 studies for possible inclusion. Because of the small number of studies, all were obtained as full text versions and independently reviewed. The remit was to determine whether there was outcome data that could be extracted for SIJF for LBP. Three of the studies were from the same authoring group describing their increasingly large cohort of patients. In this case only the most recent report was included. Finally six studies were deemed eligible for inclusion (Fig. 1).
Methodological quality assessment
The National Heart Lung and Blood Institute (NIH) quality assessment tool for case series studies [10] was used to assess the methodological quality of the selected studies (Table 1). This categorises studies as either good, fair or poor. Identified studies were assessed by two reviewers (KL & RP) independently and any disagreement over scoring was resolved by consensus.
Data extraction
Data extraction forms were designed and for each outcome the following were extracted: study design, type of SIJF surgery and whether MIS or open, number of patients and mean and standard deviation (SD) for the outcomes. Two authors (KL, RP) extracted the data independently which was subsequently reviewed jointly to produce accurate data.
Statistical analysis
Meta-analysis performed using RevMan review manager software [11] was used to combine the studies for each outcome to provide an overall estimate of the effect in the form of a forest plot. Missing SD’s, needed for combining the outcomes, were calculated from the range of values (where given) using the formulae of Hozo [12] or from the confidence interval (CI) [7]. Data were expressed as mean and SD and the treatment effect as mean difference and associated CI. Where it was necessary to combine means and SD’s in an individual study (as in the cases where data were given separately for open and MIS procedures to get an overall mean and SD), the formula of Headrick [13] was used.
Statistical heterogeneity was assessed from the I 2 statistic using a fixed effects model. An I 2 value ≥50 % was considered suggestive of statistical heterogeneity. Where heterogeneity was present, efforts were made to explore possible causes such as patient selection, data outliers etc. for each included study. A “leave-one-out” sensitivity analysis was performed by iteratively removing one study at a time to confirm the source of the heterogeneity. Analysis was then performed without the study to determine if heterogeneity was still present and if so, random effects modelling was used.
Results
Two hundred and seventy-six studies were identified using the search strategy. Duplicates and irrelevant studies amounted to 255 leaving 21 studies for detailed evaluation. All were case series. Thirteen were excluded after review leaving 8 papers for data extraction. Reasons for exclusion were no baseline data, only qualitative data on outcome and studies that were from the same author describing cumulative patient data over time i.e. including previously reported historical data. Of the eight studies, two could not be included due to missing SD’s leaving six studies for the meta-analysis (Fig. 1). Included studies all had complete data in at least one of the outcomes (Table 3).
The methodological quality as measured by the NIH quality assessment tool was high with all studies assessed as good (Table 1). Two were retrospective, utilising patient database/hospital registers to get their data and the remainder prospective (Table 2). Two of the studies were small with 17 patients or less.
Participants were adults who underwent SIJF surgery with LBP attributed to the SIJ. A variety of surgical approaches were used (Table 2). Three of the studies used MIS techniques, another used both and the other two used open procedures. Table 3 lists the outcomes reported in each study.
In total 407 patients underwent SIJF with mean age of 53 years (range 30–89). There was a slight excess of females (n = 211, 52 %). All but five patients had unilateral fusions.
Meta-analysis
VAS pain
Pain intensity on a 0–100 scale was reported in four studies [14–17]. Follow-up ranged from 6–60 months. The meta-analysis for pain shows a statistically significant improvement in pain after surgery using a fixed effects model (weighted mean difference: 48.57; 95 % CI 43.46, 53.69; n = 490; p < 0.001). Because of significant heterogeneity (I 2 = 80 %), a sensitivity analysis was performed. All the studies apart from the Mason2013 [14] study used MIS procedures. Removing this study from the analysis reduced the heterogeneity to 39 % using a fixed effects model (weighted mean difference: 54.79; 95 % CI 48.56, 61.03; n = 380; p < 0.001) (Fig. 2).
Forest plot of VAS pain (Mason2013 excluded from analysis). The forest plot consists of a vertical line which denotes no change in the outcome after SIJ fusion The position of the black diamond denotes whether there is any change and if so in which direction it lies i.e. improvement or deterioration The squares denote the individual studies with their size proportional to the weightings given to each study
ODI
This was reported in three studies [14, 16, 18]. The study by Rudolf and Capobianco [16] only had follow-up data so could not be included in the meta-analysis. The follow-up ranged from 6–17 months. The fixed effects forest plot (Fig. 3) shows a significant improvement in ODI after surgery (weighted mean difference: 14.53; 95 % CI 8.42–20.64; n = 102; p < 0.001). Heterogeneity was 0 %.
SF-36 PCS
Three studies [14, 15, 18] reported this outcome. The follow-up ranged from 6–36 months. The fixed effects forest plot (Fig. 4) shows a significant improvement after surgery (weighted mean difference: −13.02; 95 % CI −16.4, −9.67; n = 198; p < 0.001). Because of significant heterogeneity (I 2 = 82 %) a sensitivity analysis was performed. All the studies apart from the Duhon2013 [14] study used open procedures. Removing this study from the analysis reduced the heterogeneity to 34 % using a fixed effects model (weighted mean difference: −19.46; 95 % CI −24.68, −14.24; n = 140; p < 0.001) (Fig. 4).
SF-36 MCS
Three studies [14, 15, 18] reported this outcome. The follow-up ranged from 6–36 months. The fixed effects forest plot (Fig. 5) shows a significant improvement after surgery (weighted mean difference: −8.50; 95 % CI −12.9, −4.1; n = 198; p < 0.001). Heterogeneity was 0 %.
Majeed Score
Two studies [15, 18] reported this outcome. The follow-up ranged from 17–36.2 months. The forest plot (Fig. 6) shows a significant improvement after surgery (weighted mean difference: −35.36; 95 % CI −48.49, −22.23; n = 140; p < 0.001). A random effects model was used because of the significant heterogeneity (I 2 = 88 %). Both studies used open procedures and there was no apparent cause for the high heterogeneity.
Complications were reported in all six studies [14–19]. Sixteen patients out of 307 experienced complications (5.21 %) These were due to implant misplacement, implant failure, PE, infection, hematoma and neuralgia.
Discussion
In contrast to the lumbar spine, the SIJ is not widely recognised as a pain generator for LBP. Pain can originate from a number of areas both spinal and non-spinal. Spinal generators include nerves, discs, facet joints, muscles and ligaments. Non-spinal sources include the SIJ and hip. Failure to alleviate pain after surgical treatment of the spine may be due to incorrect identification of the pain source.
In common with the intervertebral disc as a source of pain, pathology in the SIJ does not necessarily correlate with symptoms making radiological diagnosis difficult. Physical tests have been shown to have poor sensitivity and specificity [20, 21]. The best available reference standard for diagnosing the SIJ as a pain source is intra-articular steroid injection under fluoroscopic guidance although there is some doubt about its diagnostic validity [20, 21]. More recently, single-photon emission computed tomography (SPECT/CT) has been used to diagnose SIJ dysfunction [22]. Results from SPECT/CT have been shown to correlate well with those from intra-articular steroid injections. Therefore, SPECT/CT could be useful as a supplementary diagnostic procedure to intra-articular steroid injections.
Sembrano and Polly Jr. [23] found, in a series of 200 patients with LBP, that using diagnostic injections, the pain source originated in the SIJ in 15 % of patients. In two other studies, Schwarzer et al. [1] reported the SIJ as the source of pain in 30 % of LBP patients and Maigne et al. [24] in 19 %.
Conservative therapies for SIJ pain include medication, physiotherapy and external orthotics such as pelvic belts. Intra-articular steroid injection has been shown to give short term pain relief and additionally, pain relief confirms the SIJ as the pain generator. Failure of pain relief using conservative therapies may require SIJF. A variety of techniques and approaches have been described both open and MIS.
Schutz et al. [3] found almost universal poor outcome in a series of 17 patients who underwent open bilateral fusion for PGP, with 82 % of patients reporting unsatisfactory pain relief as measured by VAS. This poor outcome was accounted for by the novel surgical procedure used which resulted in poor quality fusion with 42 % achieving no fusion at all. The technique used internal fixation and decortication of the SIJ with local bone grafting. This study was not included in the meta-analysis because of the poor fusion rate with only 35 % showing a definite fusion.
Wise et al. [25] in a series of 13 patients, using a MIS posterior approach with percutaneously inserted fusion cages and morphogenic protein, found significant pain reduction as measured on a VAS and 89 % fusion rate. Patient satisfaction with the procedure was high with 77 % of patients satisfied with the result. This study was not included in the analysis because only VAS improvement scores were given—there was no baseline and follow-up data.
Similarly Slinkard et al. [26] found significant improvement in functional ability (ODI) using an open technique in a series of 19 patients. Furthermore they found those patients who had previous spinal fusion surgery showed less improvement than those that did not. They used an anterior ilioinguinal approach with autograft and plates across the SIJ. This study was also excluded from the analysis as only improvement scores were given.
Kibsgard et al. [4] in a case series of eight patients at 12 months follow-up found satisfactory pain reduction (VAS), decrease in disability as measured by the ODI and improvement in health related quality of life (SF-36), after fusion using an open anterior approach with autologous bone and plates, in 78 % of patients. Unfortunately they did find three major and three minor complications in six of the eight patients operated on. This study was not included in the meta-analysis due to missing SD’s.
In another study by Kibsgard et al. [27], 50 patients who underwent SIJ fusion for PGP were followed-up at 1 and 23 years after surgery. Those patients (48 %) with successful 1 year outcomes had retained their decrease in pain and disability as measured by VAS and ODI, respectively. This study was not included in the meta-analysis due to missing baseline data.
Cummings Jr.et al. [28] in a study of 18 patients using a MIS technique, found favourable outcome for pain (VAS) and functional ability (ODI) with only one complication due to implant malposition. Patent satisfaction with the procedure was 95 %. They used a posterior approach and tubular implants without bone. This study was excluded from the meta-analysis because it included data that was subsequently included in another report from this centre [5].
In this meta-analysis of the six studies that included usable data, which excluded the foregoing studies, three reported results using MIS, two used open methods, and one study used both. The analysis has found that patients undergoing SIJF for PGP had a statistically and clinically significant improvement in pain relief, ODI, SF-36 and Majeed score. The minimally clinically important difference (MCID) for VAS back pain is around 20 points [29, 30]. The meta-analysis shows a mean improvement of 55 points. Similarly, MCID for ODI is considered to be 10 points [31]. The meta-analysis for SIJF was 14.5 points. For SF-36 PCS, 5 points is considered to be a MCID [32]. The analysis gave 19.5 points. SF-36 MCS summary score was 8.5 which is within the range of the MCID of 7.0–15.9 [31]. There have been no studies on what is the MCID for the Majeed score but it showed an improvement of 36 points. Both studies included in the meta-analysis for the Majeed score showed a mean improvement from poor (37 and 36.2, respectively) to good (64.8) [18] and excellent (79) [15].
Complications due to the surgery were low and occurred in 16 patients out of 307 (5.2 %). For the open surgery the rate was 5.44 and 3.49 % for the MIS methods.
The strength of our meta-analysis is that it is the first to consider outcomes for SIJF for PGP and has been carried out according to Cochrane guidelines. In addition, the follow-up periods for the included studies varied from 6 to 60 months with the majority over 13 months.
Our meta-analysis has some limitations. It pools the results of observational studies but these were the only studies available on the topic. All the included studies were case series. Furthermore, the number of studies available for meta-analysis was only six. The ODI and Majeed scores only pooled the results of two studies.
Although this meta-analysis has shown functional and pain outcomes to be statistically and clinically significant, the conclusion is based upon very limited data and therefore its validity may be low. Providing the SIJ is unequivocally identified as the source of pain by means of provocative SIJ injections, SIJF appears to be a satisfactory procedure for alleviating PGP. Further high quality studies are needed to verify this finding.
References
Schwarzer AC, Aprill CN, Bogduck M (1995) The sacroiliac joint in chronic low back pain. Spine 20:31–37
Vleeming A, Albert HB, Ostgaard HC et al (2008) European guidelines for the diagnosis and treatment of pelvic girdle pain. Eur Spine J 17(6):794–819
Schutz A, Grob D (2006) Poor outcome following bilateral sacroiliac joint fusion for degenerative sacroiliac joint syndrome. Acta Orthop Belg 72:296–308
Kibsgard TJ, Roise O, Stug B (2014) Pelvic joint fusions in patients with severe pelvic girdle pain—a prospective single-subject research design study. BMC Musculoskelet Disord 15:85
Sachs D, Capobianco R (2013) Minimally invasive sacroiliac joint fusion: one year outcomes in 40 patients. Adv Orthop 2013:536128
Zaidi HA, Montoure AJ, Dickman CA (2015) Surgical and clinical efficacy of sacroiliac joint fusion: a systematic review of the literature. J Neurosurg Spine 23:59–66
Higgins JPT, Green S (eds) (2009) Cochrane handbook for systematic reviews of interventions. Wiley-Blackwell, Chichester
Majeed SA (1989) Grading the outcome of pelvic fractures. J Bone Joint Surg [Br] 71:304–306
RefWorks [computer program]. Version 2. http://www.refworks.com
The National Heart Lung and Blood Institute. Quality assessment tool for case series studies. Available at http://www.nhlbi.nih.gov/health-pro/guidelines/in-develop/cardiovascular-risk-reduction/tools/case_series. Accessed Oct 2014
RevMan [computer program]. Version 5.2.11, Nordic Cochrane Center, Copenhagen, 2013
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range and the size of the sample. BMC Med Res Methodol 5(1):13–20
Headrick TC (2010) Statistical simulation: power method polynomials and other transformations. Chapman & Hall/CRC, Boca Raton, p 137
Duhon BS, Cher DJ, Wine KD et al (2013) Safety and 6-month effectiveness of minimally invasive sacroiliac joint fusion: a prospective study. Med Dev Evid Res 6:219–229
Mason LW, Chopra I (2013) The percutaneous stabilisation of the sacroiliac joint with hollow modular anchorage screws: a prospective outcome study. Euro Spine J 22:2325–2331
Rudolf L, Capobianco R (2014) Five year clinical and radiographic outcomes after minimally invasive sacroiliac joint fusion using triangular implants. Open Orthop J 8:375–383
Sachs D, Capobianco R, Cher D et al (2014) One year outcomes after minimally invasive sacroiliac joint fusion with a series of triangular implants: a multicenter patient level analysis. Med Dev Evid Res 7:299–304
Khurana A, Guha AR, Mohanty K et al (2009) Percutaneous fusion of the sacroiliac joint with hollow modular anchorage screws. J Bone Joint Surg 91:627–631
Ledonio CGT, Polly DW Jr, Swiontkowski MF (2014) Minimally invasive versus open sacroiliac joint fusion. Clin Orthop Relat Res 472:1831–1838
Stuber KJ (2007) Specificity, sensitivity and predictive values of clinical tests of the sacroiliac joint; a systematic review of the literature. J Can Chiropr Assoc 51(1):30–41
Berthelot JM, Labat JJ, Le Goff B et al (2006) Provocative sacroiliac joint maneuvers and sacroiliac joint block are unreliable for diagnosing sacroiliac joint pain. Joint Bone Spine 73(1):7–23
Tofuku K, Koga H, Komiya S (2015) The diagnostic value of single-photon emission computed tomography/computed tomography for severe joint dysfunction. Euro Spine J 24:859–863
Sembrano JN, Polly DW Jr (2009) How often is low back pain not coming form the back? Spine 34:E27–E32
Maigne JY, Planchon CA (2005) Sacroiliac joint pain after lumbar fusion. A study with anesthetic blocks. Eur Spine J 14:654–658
Wise CL, Dall BE (2008) Minimally invasive sacroiliac arthrodesis: outcomes of a new technique. J Spinal Disord Tech 21:579–584
Slinkard N, Agel J, Swiontkowski MF (2013) Documenation of outcomes for sacroiliac joint fusion: does prior spinal fusion influence outcome? Eur Spine J 22:2318–2324
Kibsgard TJ, Roise O, Sudmann E (2013) Pelvic joint fusions in patients with chronic pelvic girdle pain: a 23-year follow-up. Eur Spine J 22:871–877
Cummings J Jr, Capobianco RA (2013) Minimally invasive sacroiliac joint fusion: one year outcomes in 18 patients. Ann Surg Innov Res 7:12
Hägg O, Fritzell P, Nordwall A (2003) The clinical importance of changes in outcome scores after treatment for chronic low back pain. Eur Spine J 12:12–20
Ostelo RW, de Vet HC (2005) Clinically important outcomes in low back pain. Best Pract Res Clin Rheumatol 19:593–607
Vianin M (2008) Psychometric properties and clinical usefulness of the Oswestry Disabiity Index. J Chiropr Med 7:161–163
Copay AG, Glassman SD, Subach BR (2008) Minimum clinically important difference in lumbar spine surgery patients: a choice of methods using the Oswestry Disability Index, Medical Outcomes Study questionnaire Short Form 36, and pain scales. Spine J 8:968–974
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Lingutla, K.K., Pollock, R. & Ahuja, S. Sacroiliac joint fusion for low back pain: a systematic review and meta-analysis. Eur Spine J 25, 1924–1931 (2016). https://doi.org/10.1007/s00586-016-4490-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-016-4490-8