Abstract
Purpose of Review
Sacroiliac dysfunction is an important cause of low back pain with significant impact on quality of life and daily activities. Minimally invasive sacroiliac joint fusion (MIS SI fusion) is an effective treatment for patients who failed non-surgical strategies. The purpose of this article is to review the clinical outcomes and complications of this surgical technique.
Recent Findings
For patients with SI joint dysfunction, MIS SI fusion reduced pain and disability as measured by Visual Analog Scale and Oswestry Index and improved quality of life as measured by Short-Form 36 and EuroQol-5D questionnaires. Satisfaction rates were higher in the SI fusion group when compared to the conservative management. In recent clinical trials, adverse events occurred with a similar rate in the first 6 months for patients assigned in the conservative management versus patients assigned to MIS SI fusion.
Summary
MIS SI fusion is an effective and safe procedure for patients with sacroiliac dysfunction who failed non-surgical strategies. This procedure provides rapid as well as sustained pain relief, improvement in back function, high patient satisfaction, with low rate of complications.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Low back pain (LBP) is estimated to afflict more than 74 million adults in the USA, with an estimate in a 2002 National Health Interview survey showing that 10% of the US population likely suffers from chronic LBP and that 2.3% of visits to physicians are due to LBP [1]. The effective treatment of LBP is complicated by the vast differential diagnosis, including degenerative disk disease, muscular instability, ligamentous disease, and sacroiliac (SI) joint dysfunction. The SI joint is involved in 15–30% of patients with back pain, with varying numbers between prevalence studies due to the often nebulous definitions used for diagnosis [2]. Schwarzer et al. found that 16% of a 43 patient series had SI joint pain that fulfilled three diagnostic criteria: response to local anesthetics, abnormalities on CT imaging, and pain provocation during joint manipulation [3]. Another study by Maigne et al. found that 18.5% of patients responded to both lidocaine blocking and confirmatory bupivacaine block and thus were considered to have true SI joint pain [4].
Etiology
SI joint dysfunction has a broad range of etiological factors, including many pathologies implicated in degeneration of other joints and spinal segments [5]. Trauma, including falls and motor vehicle accidents (MVAs), can injure either the bony elements of the SI joint or affect the ligamentous connections between bony elements, resulting in subsequent destabilization [6]. In addition, microtrauma, often from repeated physical activity such as lifting and bending, can cause SI joint in the absence of overt trauma [7]. Sacroiliitis is a broad term used for inflammatory processes affecting the SI joint and includes various forms of spondylarthritis such as ankylosing spondylitis, which is often associated with SI joint widening or narrowing, subchondral erosion, sclerosis, and proliferation as an early hallmark. In the subset of patients with reactive arthritis, this inflammatory process follows infection. In addition, sacroiliitis has been associated with other systemic inflammatory conditions, such as inflammatory bowel disease, Crohn’s disease, gout, tuberculosis, and osteoarthritis [8]. Lastly, iatrogenic causes of SI joint dysfunction have been explored, with Liliang et al. finding that 40.4% of 52 patients who underwent lumbar or lumbosacral fusion were considered to have SI joint pain on the basis of two positive responses to diagnostic blocks [9]. Ha et al. performed a prospective cohort study investigating SI joint pain and found that 75% of 32 patients who underwent posterolateral fusion had SI joint degeneration, compared to 38.2% of the control group [10].
Diagnosis
Diagnosis of SI joint dysfunction is made most commonly through history and physical examination including provocative maneuvers to elicit pain from SI dysfunction and confirmed with targeted (fluoroscopic) intra-articular injections of local anesthetic. The role of radiography is predominantly to exclude alternative pathology. Patients often complain of increased pain with sitting and are often standing or sitting in a way to avoid pressure on the affected side in the exam room. A history of trauma, pain after vaginal delivery, and prior lumbar or lumbosacral procedures is often present. On physical examination, pain inferior to the posterior superior iliac spine and lateral to the gluteal fold (Fortin Finger test) is sensitive for SI joint dysfunction [11]. SI pain will often radiate into the lower extremity, hip, and groin and can often be confused for sciatica or disc pathology [2]. In addition, pain in this region on loading activities such as walking, lifting, and standing can point toward SI joint dysfunction. Provocative maneuvers for testing the SI joint include compression test, thigh thrust test, FABER (flexion, abduction, external rotation) test, distraction test, and Gaenslen’s test have varying degrees of sensitivity and specificity for determining SI joint pathology; however, negative results across a broad range of provocations are a general rule-out criteria for SI joint dysfunction [12]. According to Van Der Wurff et al. three or more positive provocation tests resulted in a 65–93% probability that pain was related to the SI joint [13].
Diagnostic imaging of the SI joint is used to evaluate for other causes of LBP such as osteoarthritis or spondylosis or other more serious pathologies such as neoplasia. Plain radiographs can be helpful in evaluating for lumbosacral spondylosis and presence of instability. X-rays can show sclerosis or widening of the SI joint, but absence of changes does not exclude SI pathology. Additionally, due to its ligamentous anatomy and oblique position, the evaluation of the SI joint directly on AP radiographs can be challenging. CT scans can show joint changes and subchondral sclerosis, but one study showed only 57.5% sensitivity and 69% specificity in findings [14]. MRI, in addition to being used to rule out other lumbosacral or pelvic pathologies, is also helpful for detecting inflammatory processes in the SI joint. If an inflammatory source of SI joint pain is suspected, a rheumatologic workup including laboratory studies should be initiated.
Fluoroscopic SI joint injections serve both a diagnostic and therapeutic purpose and consist of injections of the anesthetic agent or corticosteroids into the SI joint and evaluation of pain after the procedure. Criteria have been established by the North American Spine Society, consisting of ≥ 75% pain relief on 2 diagnostic intra-articular injections, and by the International Society for Advancement of Spine Surgery, consisting of ≥ 50% acute decrease in pain upon fluoroscopically guided diagnostic intra-articular SIJ block using local anesthetic [15, 16].
Sacroiliac Joint Anatomy
The SI joint is the largest articular joint in the body with an average surface area of approximately 17.5 cm2. It consists of a synovial joint that connects the axial skeleton with the lower extremities. It is surrounded by a fibrous capsule and innervated by the dorsal rami of the L4-S3 nerve roots. The anterior third of the sacroiliac junction is a true synovial joint while the posterior section is composed of intricate ligamentous connections. The articular surfaces of the SI joint are uniquely roughened to decrease mobility and increase stability.
Therapeutic Options
Non-surgical options for management of SI joint dysfunction include physical interventions, medication, intra-articular injection, and radiofrequency ablation. Physical interventions, such as physical therapy aimed at strengthening the surrounding musculature and thus providing stability to the joint capsule as well as bracing treatment (SI belts) to decrease SI joint mobility, are popular first-line treatments alongside medical management for pain such as non-steroid anti-inflammatories (NSAIDs), local lidocaine patches, or opiate medication. Intra-articular injections with anesthetic and corticosteroid are the non-surgical modalities that have the strongest evidence in support, but are often short-term solutions requiring repeated visits to the healthcare provider [17, 18]. Radiofrequency ablation is a therapeutic option utilizing radiofrequency lesioning to target pain-generating neural structures. A randomized study by Cohen et al. reported 79%, 64%, and 57% radiofrequency-treated patients experienced pain relief of 50% or greater and significant functional improvement at 1, 3, and 6 months after the procedure [19]. However, only 14% of patients reported pain relief 1 year after treatment, suggesting that like intra-articular injection, radiofrequency ablation is a poor choice for long-term pain control.
Sacroiliac Joint Fusion
SI joint arthrodesis or fusion is an option for patients who have failed non-surgical strategies. Minimally invasive sacroiliac joint fusion (MIS SI fusion) is an effective treatment for patients who failed non-surgical strategies. The purpose of this article is to review the clinical outcomes and complications of this surgical technique. The first report of non-instrumented SI joint arthrodesis was published in 1921 by Smith-Petersen [20]. Studies describing an open approach with internal fixation using metal plates and screws became available in the 80 s; however, the perioperative morbidity was still quite significant [21]. In the late 2000s, although minimally invasive surgical (MIS) techniques began to appear, the procedure was still limited to threaded screws and cages implanted with a posterior approach [22]. Most recently, a different MIS technique using a lateral approach to place triangular titanium implants across the SI joint gained popularity [23,24,25]. The major goal of this technique is to provide immediate and long-term stabilization of the SI joint. The implantation of multiple triangular implants prevents micromovements and joint rotation, allowing bone binding to the implant surface on both sides of the joint and consequently promoting intra-articular fusion [26].
Open SI Joint Fusion
There are several techniques for open SI joint fusion including anterior, posterior, and lateral approaches reported in the literature [22, 27, 28]. Typically, the open SI joint fusion is performed under general anesthesia using a posterior approach with the patient in the prone position. Usually, neuromonitoring with electromyography is utilized to ensure safe placement of instrumentation. A longitudinal incision is made over the posterior superior iliac spine (PSIS), and the bone is exposed with a Bovie cautery. Then, part of the PSIS is removed using an osteotome and curettes, and rongeurs are used to remove cartilage and ligament from the joint. Then, two holes are drilled with a reamer so that the cages (packed with morselized bone) can be implanted into the SI joint. Additionally, different types of screws can be implanted, including iliosacral lag screws, pedicle screws into S1 pedicle or between the inner and outer tables of the ilium, connected by a spinal rod. Alternatively, recon plating across the SI joint with cancellous screws placed in the sacral ala and the ilium, as well as one long cannulated screw across the SI join, can be used for fixation. Finally, the tissue layers are closed in a standard way with the use of a drain [25].
MIS SI Fusion
MIS SI fusions are performed with the patient positioned prone on a radiolucent table to allow the use of image guidance, either with intraoperative fluoroscopy or with O-arm (Medtronic, Minneapolis, Minnesota, USA) and neuronavigation. The procedure is done either through a lateral or posterior approach.
Posterior Approach
The Rialto SI Fusion System (Medtronic, Minneapolis, Minnesota, USA) is an example of system implanted through a posterior approach and consists of cylindrical threaded devices that can be filled with bone graft. In brief, the patient is positioned prone, and a small incision was made over the contralateral PSIS, followed by the insertion of the tracker pin. A three-dimensional O-arm spin is performed with the images transferred to the navigation system. The trajectories for placing the implants are planned in a posterior-to-anterior and medial-to-lateral direction across the SI joint. Through a small incision, the trajectory is drilled and then tapped across the SI joint, followed by the placement of the cylindrical threaded implants filled with allograft. Finally, an additional O- arm spin is acquired to confirm the final position of the implants. The wounds were closed in standard fashion [29].
Lateral Approach — Guided by Fluoroscopy
The procedure is performed under general anesthesia, typically with patient in the prone position. Useful landmarks to localize the lateral incision are the sacral ala, the posterior and the anterior walls of the sacrum, and the sciatic notch. A line is drawn over the posterior wall of the sacrum and over the sacral ala. A ~ 3-cm incision is planned along the posterior sacral line 1 cm posteriorly to where it intersects the alar line (Fig. 1). After incision is made in the lateral buttock, the fascia is dissected bluntly, and the outer table of the ilium is reached. Through fluoroscopy, lateral, inlet, and outlet views are used to monitor the position of pins and implants [30]. The lateral view is used to localize the starting point 1 cm inferior to the sacral ala and 1 cm anterior to the posterior wall of the sacrum. Using the outlet view, the pin is positioned in such a way that it stays parallel to the S1 endplate and that it does not violate the S1 foramen. The inlet view allows verifying if the trajectory is not too anterior or posterior (Fig. 2). A sharp Steidman pin is passed through the ilium across the SI joint, and a blunt dissector is rotated around the pin, followed by the insertion of the soft tissue protector parallel to the ala. A hand drill creates a pathway across ilium, SI joint, and sacrum. A triangular broach is used to decorticate and prepare the bone for the implant and the implants are then placed.
Lateral Approach — Guided by Neuronavigation
The procedure is typically performed with the patient in the prone position although the lateral position has also been described [31]. The procedure starts with the insertion of the tracker pin into the contralateral PSIS. Three-dimensional imaging is acquired using the O-arm and transferred to the navigation system. Sacral ala and the posterior wall of the sacrum are used again to plan the incision. After incision is made in the lateral buttock, the fascia is dissected bluntly, and the outer table of the ilium is reached. Neuronavigation allows the surgeon to plan and to verify the trajectory and position of the implants in axial, coronal, and sagittal planes, as well as a three-dimensional reconstruction denominated synthetic lateral view (Fig. 3). A reverse threaded pin is passed through the ilium across the SI joint, and a blunt dissector is rotated around the pin, followed by the insertion of the soft tissue protector parallel to the ala. A hand drill creates a pathway across ilium, SI joint, and sacrum and then a triangular broach is used to decorticate and prepare the bone for the implant. The implants are most frequently placed in a triangular fashion, but positioning the implants forming a straight line used to be a common approach in the past. The most rostral implant should be directed into the S1 Segment, the second implant is directed into the S2 segment, and the third implant is placed in a position ventral to the first implant directed into the S1 segment. Interoperative CT is used to confirm implant position following implantation. Long-acting local anesthetic is injected into the soft tissue. A deep dermal closure of 2–0 Vicryl suture, followed by Subcuticular 4–0 Monocryl and skin glue is applied. The postoperative course includes partial weight bearing with the assistance of a walker or crutches for 3 weeks. Physical therapy is initiated at 6 weeks postoperative if needed [25, 32•].
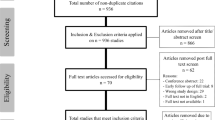
Methods
In this review, we analyzed the most recent literature regarding MIS SI fusion for SI joint dysfunction. A PubMed search focusing on articles published in the last 5 years was performed using the terms “minimally invasive sacroiliac joint fusion,” “minimally invasive sacral-iliac joint fusion,” “minimally invasive sacral iliac joint fusion,” and “MIS SI fusion.” The search was also tailored for only articles published in English only, with available abstract, resulting in a total of 75 articles. These articles were screened and included in this review accordingly. In order to review outcomes from articles with the best evidence level, the initial search was further filtered for article type including “Clinical Trial,” “Meta-analysis,” and “Randomized Controlled Trial,” which yielded 7 articles. Furthermore, articles that were not published in the past 5 years but that were considered relevant by the authors were also included in this review.
Results
Types of Implants
Several devices have been approved for MIS SI fusion including iFuse Implant System (SI-BONE, Inc., Santa Clara, California, USA), iFuse-3D Implant System ((SI-BONE, Inc., Santa Clara, CA, USA), Rialto SI Fusion System (Medtronic, Minneapolis, MN, USA), SI-LOK Sacroiliac Joint Fixation System (Globus Medical, Inc., Audubon, PA, USA), SambaScrew SI Fixation System (Orthofix, Lewisville, TX, USA), Silex Sacroiliac Joint Fusion System (Xtant Medical, Belgrade, MT, USA), and Simmetry Sacroiliac Joint Fusion System (Zyga Technology, Inc., Minnetonka, MN, USA) [29]. A meta-analysis demonstrated that the majority of articles published with strong evidence level utilized the iFuse systems [33], and therefore, this review will focus on those studies. The original iFuse system manufactured through a titanium plasma spray (TPS) coating process and consists of solid implants with porous surfaces that provide a scaffold for osteoconduction and osteointegration. Porous surfaces promote bony ingrowth and ongrowth, which decreases the incidence of migration, subsidence, and consequently pseudoarthrosis [34•]. The iFuse-3D system for SI fusions consists of a titanium 3D-printed implant which has an optimized and consisted microstructure that resembles the characteristics of the cancellous bone. In comparison to TPS implants, 3D-printed implants support the growth of human osteoblasts, with higher calcium production and have higher bony ingrowth and ongrowth [35, 36].
Clinical Outcomes
The first studies in the literature demonstrating the effectiveness and safety of triangular, porous plasma spray-coated titanium implants placed across the SI joint were published in 2012 [23, 30]. However, the first prospective, multicenter, postmarket (on-label) single-arm interventional clinical trial was the SIFI study, published online in 2015 by Duhon et al. [24]. This study reported the outcomes of the 1-year follow up, and the 2-year follow up article was published in the following year [37•]. In summary, this prospective study included 172 patients from 26 centers who underwent MIS SI fusion with porous triangular titanium implants. The majority of the patients were females, with 5 years of pain in average, and about 44% of the subjects had had a prior lumbar fusion. Pain was evaluated by a 100-mm visual analog scale (VAS) and decreased from 79.8 at baseline to 30.4 at 12 months and remained low at 26.0 at 24 months. Disability was measured by the Oswestry Disability Index (ODI) and decreased from 55.2 at baseline to 31.5 at 12 months and remained low at 30.9 at 24 months. Quality of life was accessed by Short-Form 36 (SF-36) and EuroQoL-5D (EQ-5D), and again, improvements seen at 12 months were sustained at 24 months. Furthermore, the use of opioids for SI joint or low back pain decreased from 76.2% at baseline to 55.0% at 24 months (Table 1).
A Level 1 multicenter prospective randomized controlled trial, the INSITE study by Polly et al. compared 148 patients from 19 centers, who were randomized to undergo non-surgical management (NSM) (n = 49) or SI fusion (n = 109) with triangular, porous plasma spray–coated titanium implants for SI dysfunction using [32•]. NSM included physical therapy, steroid injections, radiofrequency ablation, and oral pain medications. Subjects assigned to the NSM group were allowed to cross over to the SI fusion group at any time after the 6-month follow up visit. A total of 39 patients crossed over, and therefore, comparisons were done between 6-month and baseline scores. An average pain reduction of 12.2 (100 mm VAS) was found for the NSM, whereas the SI fusion group had an average reduction of 55.4. At 6 months, the NSM group had an improvement of 4.6 points, while the SF fusion group had an improvement of 27.3 points in relation to baseline. Quality of life (SF-36) scores were also significantly better in the surgical group. Moreover, opioid use increased in the NSM group (63% to 70.5%), whereas a decrease was demonstrated in the SF fusion group (68.6 to 58.4%). At the 2-year follow up, 82% of the patients in the SI fusion group reported improvement ≥ 25 points in the VAS score, while only 10% of the patients remaining in the NSM group reported the same. Similarly, 65.9% of the patients in the SI fusion group reported improvement ≥ 25 points in the ODI score, while only 10% of the patients remaining in the NSM group were found to have the same improvement (Table 1). Satisfaction rates were higher in the SI fusion group when compared to the NSM group at the 6-month follow-up (77.2% versus 27.3%, p < 0.0001), and satisfaction with the surgery remained high at the 12- and 24-month follow ups (78% and 73% respectively). Another important article described the results from the iMIA study, a prospective, open-label, multicenter, randomized trial that included 103 patients from 9 centers [38•]. Similarly to Dengler et al. this study randomized patient with SI dysfunction to NSM or MIS SI fusion, allowing for cross over after the 6-month follow up. The impact of cross over from NSM to surgical treatment was assessed using a last-observation-carried-forward approach, substituting the last observation prior to crossover for subsequent values [38•]. Once again, improvements on pain level (VAS), pain related disability (ODI), and quality of life (EQ-5D) were significantly better in the SI fusion group (Table 1).
A pooled patient-level analysis combining data from the 3 trials described above (SIFI, INSITE, and iMIA) (n = 423) used random effects models with multivariate regression analysis to identify predictors for treatment outcome separately. In brief, once again, improvement of pain (VAS) and ODI was larger for the SI fusion group. In the NSM group, no predictors of outcome could be identified, whereas in the SI fusion group, reduced improvement in outcome could be predicted by smoking, opioid use, lower patient age, and lower duration of SI joint pain [39]. Furthermore, Darr and Cher demonstrated that SI fusion promotes long-term improvement in patients with pain caused by SI dysfunction. At 4 years, 93 patients from the INSITE and SIFI studies still exhibited improvement in pain (reduction of 54 points from baseline in the VAS), disability (reduction of 26 points in the ODI), and quality of life (improvement of 0.3 points in the EQ-5D) [40]. Another prospective, multicenter trial, the SALLY study, published recently, demonstrated the effectiveness SI fusion with 3D-printed triangular titanium implants [26, 34]. Similarly to the TPS triangular implants, there was significant improvement at 24 months when compared to baseline in pain (mean VAS reduction from 78.5 to 21.5) and disability (mean ODI reduction from 52.8 to 28.3). In addition, the percentage of patients using opioids preoperatively decreased from 59 to 18% at the 24-month follow up (Table 1). This trial also demonstrated a 77% rate of bone bridging on CT scans.
Open Surgery, Minimally Invasive, Fluoroscopy, and Neuronavigation
There is no prospective, randomized trial, comparing open versus MIS SI fusions. However, Smith et al. conducted a retrospective multicenter comparing both methods with regard to operative measures safety and effectiveness [25]. A total of 263 patients (149 patients treated with open SI fusion) were included in the study. Operative measures, including estimated blood loss, operating time, and length of hospitalization, were significantly lower for the MIS SI fusion patients. Moreover, pain relief improved significantly for both groups; however, when the patients were matched for age, gender, history of prior lumbar spinal, and pain scores were on average 3 points lower for the MIS SI fusion group. There were no intraoperative complications. Postoperative complications occurred in 21% of the patients who underwent open surgery and in 18% of the patients who underwent MIS procedure. The most common complications were postoperative neuropathy and transient trochanteric bursitis, leg pain, wound-related issues, facet pain, and falls. As most of MIS procedures, an MIS SI fusion requires image guidance. Typically, image guidance can be performed using 2D images (i.e., fluoroscopy) or 3D images (i.e., neuronavigation). Montenegro et al. showed no significant difference between complications and mean pain improvement 3 months after surgery between fluoroscopic and navigation groups for MIS SI fusion [41]. In addition, a prospective study by Bessar et al. comparing the use fluoroscopy and the use of CT for SI joint injections suggests that the total radiation dose for the patient is similar between both imaging modalities [42].
Adverse Events and Revisions
A retrospective study included 406 patients (305 females) who underwent MIS SI fusion from 2007 to 2014 and reported an overall complication rate of 13.2% at 90 days postoperatively and 16.4% at months [43]. The most common complications found in this study were wound infections; neurologic symptoms, including pain and neuropathy; and urinary tract infection. However, this study has several limitations due to its design consisting of a retrospective review using billing records for data mining. The major prospective trials published in the past years provide data with a higher level of evidence. Overall, the rate of complications in these trials was lower than the retrospective study by Schoell et al. [24, 32•, 34•, 38•, 43]. Adverse events occurred with a similar rate in the first 6 months for patients assigned in the conservative management (NSM) versus patients assigned in the SI fusion group [32•, 38•]. The most common adverse events were neuropathy related to implant malposition, wound issues (including drainage, hematoma, infection, delayed wound healing), increased SI joint pain, and postoperative complications (urinary retention, nausea/vomiting, anemia, atrial fibrillation, pneumonitis). Table 2 summarizes the most common complications and respective incidences.
Conclusions
MIS SI fusion is an effective and safe procedure for patients with sacroiliac dysfunction who failed non-surgical strategies. This procedure provides rapid as well as sustained pain relief, improvement in back function, and high patient satisfaction, with low rate of complications.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Deyo RA, Mirza SK, Martin BI. Back pain prevalence and visit rates: estimates from U.S. national surveys, 2002. Spine (Phila Pa 1976). 2006;31:2724–7.
Barros G, McGrath L, Gelfenbeyn M. Sacroiliac joint dysfunction in patients with low back pain. Fed Pract. Frontline Medical Communications. 2019;36:370.
Schwarzer AC, Aprill CN, Bogduk N. The sacroiliac joint in chronic low back pain. Spine (Phila Pa 1976). 1995.
Maigne JY, Aivaliklis A, Pfefer F. Results of sacroiliac joint double block and value of sacroiliac pain provocation tests in 54 patients with low back pain. Spine (Phila Pa 1976). 1996;1889:92.
Thawrani DP, Agabegi SS, Asghar F. Diagnosing sacroiliac joint pain. J Am Acad Orthop Surg NLM (Medline). 2019;27:85–93.
Harrison DE, Harrison DD, Troyanovich SJ. The sacroiliac joint: a review of anatomy and biomechanics with clinical implications. J Manipulative Physiol Ther United States. 1997;20:607–17.
Chou LH, Slipman CW, Bhagia SM, Tsaur L, Bhat AL, Isaac Z, et al. Inciting events initiating injection-proven sacroiliac joint syndrome. Pain Med Pain Med. 2004;5:26–32.
Baronio M, Sadia H, Paolacci S, Prestamburgo D, Miotti D, Guardamagna VA, et al. Etiopathogenesis of sacroiliitis: Implications for assessment and management. Korean J Pain. 2020;294–304.
Liliang PC, Lu K, Liang CL, Tsai YD, Wang KW, Chen HJ. Sacroiliac joint pain after lumbar and lumbosacral fusion: findings using dual sacroiliac joint blocks. Pain Med Pain Med. 2011;12:565–70.
Ha KY, Lee JS, Kim KW. Degeneration of sacroiliac joint after instrumented lumbar or lumbosacral fusion: a prospective cohort study over five-year follow-up. Spine (Phila Pa 1976). 2008;33:1192–8.
Fortin JD, Falco FJ. The Fortin finger test: an indicator of sacroiliac pain. Am J Orthop (Belle Mead NJ). United States. 1997;26:477–80.
Nejati P, Sartaj E, Imani F, Moeineddin R, Nejati L, Safavi M. Accuracy of the diagnostic tests of sacroiliac joint dysfunction. J Chiropr Med. Elsevier Inc. 2020;19:28–37.
Van Der Wurff P, Buijs EJ, Groen GJ. A multitest regimen of pain provocation tests as an aid to reduce unnecessary minimally invasive sacroiliac joint procedures. Arch Phys Med Rehabil. 2006.
Elgafy H, Semaan HB, Ebraheim NA, Coombs RJ. Computed tomography findings in patients with sacroiliac pain. Clin Orthop Relat Res. Lippincott Williams and Wilkins. 2001;112–8.
Kreiner DS, Matz P, Bono CM, Cho CH, Easa JE, Ghiselli G, et al. Guideline summary review: an evidence-based clinical guideline for the diagnosis and treatment of low back pain. Spine J. 2020.
Lorio MP. ISASS Policy 2016 update – minimally invasive sacroiliac joint fusion. Int J Spine Surg. International Society for the Advancement of Spine Surgery. 2016;10.
Schmidt GL, Bhandutia AK, Altman DT. Management of sacroiliac joint pain. J Am Acad Orthop Surg. Lippincott Williams and Wilkins. 2018;26:610–6.
Vanelderen P, Szadek K, Cohen SP, De Witte J, Lataster A, Patijn J, et al. 13. Sacroiliac joint pain. Pain Pract. Pain Pract. 2010;10:470–8.
Cohen SP, Hurley RW, Buckenmaier CC, Kurihara C, Morlando B, Dragovich A. Randomized placebo-controlled study evaluating lateral branch radiofrequency denervation for sacroiliac joint pain. Anesthesiology Anesthesiology. 2008;109:279–88.
Smith-Petersen MN. Arthrodesis of the sacroiliac joint. A new method of approach. J Orthop Surg. 1921;3:400–5.
Waisbrod H, Krainick JU, Gerbershagen HU. Sacroiliac joint arthrodesis for chronic lower back pain. Arch Orthop Trauma surgery Arch fur orthopadische und Unfall-Chirurgie. Germany. 1987;106:238–40.
Wise CL, Dall BE. Minimally invasive sacroiliac arthrodesis: outcomes of a new technique. J Spinal Disord Tech. 2008.
Sachs D, Capobianco R. One year successful outcomes for novel sacroiliac joint arthrodesis system. Ann Surg Innov Res. 2012.
Duhon BS, Cher DJ, Wine KD, Kovalsky DA, Lockstadt H. Triangular titanium implants for minimally invasive sacroiliac joint fusion: a prospective study. Glob Spine J. 2016.
Smith AG, Capobianco R, Cher D, Rudolf L, Sachs D, Gundanna M, et al. Open versus minimally invasive sacroiliac joint fusion: a multi-center comparison of perioperative measures and clinical outcomes. Ann Surg Innov Res. 2013.
Patel V, Kovalsky D, Meyer SC, Chowdhary A, LaCombe J, Lockstadt H, et al. Prospective trial of sacroiliac joint fusion using 3D-printed triangular titanium implants: 24-month follow-up. Med Devices (Auckl) [Internet]. Dove. 2021;14:211–6. Available from: https://pubmed.ncbi.nlm.nih.gov/34234582
Slinkard N, Agel J, Swiontkowski MF. Documentation of outcomes for sacroiliac joint fusion: does prior spinal fusion influence the outcome? Eur Spine J. 2013.
Buchowski JM, Kebaish KM, Sinkov V, Cohen DB, Sieber AN, Kostuik JP. Functional and radiographic outcome of sacroiliac arthrodesis for the disorders of the sacroiliac joint. Spine J. 2005.
Rajpal S, Burneikiene S. Minimally invasive sacroiliac joint fusion with cylindrical threaded implants using intraoperative stereotactic navigation. World Neurosurg. 2019.
Rudolf L. Sacroiliac joint arthrodesis-MIS technique with titanium implants: report of the first 50 patients and outcomes. Open Orthop J. 2012.
Kazemi N, Abu-Rmaileh M, Dalal S, Helton M, Walters J. Novel lateral approach for MIS sacroiliac joint arthrodesis: an assessment of feasibility and outcomes. World Neurosurg. 2021.
• Polly DW, Swofford J, Whang PG, Frank CJ, Glaser JA, Limoni RP, et al. Two-year outcomes from a randomized controlled trial of minimally invasive sacroiliac joint fusion vs. non-surgical management for sacroiliac joint dysfunction. Int J Spine Surg. 2016. This randomized controlled trial demonstrated that minimally invasive SI fusion with triangular titanium implants provided larger improvements in pain, disability, and quality of life compared to non-surgical management.
Tran ZV, Ivashchenko A, Brooks L. Sacroiliac joint fusion methodology - minimally invasive compared to screw-type surgeries: a systematic review and meta-analysis. Pain Physician. 2019.
• Patel V, Kovalsky D, Craig Meyer S, Chowdhary A, Lockstadt H, Techy F, et al. Prospective trial of sacroiliac joint fusion using 3D-printed triangular titanium implants. Med Devices Evid Res. 2020. This prospective, multicenter, single-arm study demonstrated that MIS SI fusions using 3D-printed triangular titanium implants resulted in persistent improvements in pain and quality of life, with a low rate of late device-related adverse events.
MacBarb RF, Lindsey DP, Bahney CS, Woods SA, Wolfe ML, Yerby SA. Fortifying the bone-implant interface part 1: an in vitro evaluation of 3D-printed and TPS porous surfaces. Int J Spine Surg. 2017.
MacBarb RF, Lindsey DP, Woods SA, Lalor PA, Gundanna MI, Yerby SA. Fortifying the bone-implant interface part 2: an in vivo evaluation of 3D-printed and TPS-coated triangular implants. Int J Spine Surg. 2017.
• Duhon BS, Bitan F, Lockstadt H, Kovalsky D, Cher D, Hillen T, et al. Triangular titanium implants for minimally invasive sacroiliac joint fusion: 2-year follow-up from a prospective multicenter trial. Int J Spine Surg. 2015. This prospective, multicenter single-arm study demonstrated sustained clinical improvement after 2 years.
• Dengler J, Kools D, Pflugmacher R, Gasbarrini A, Prestamburgo D, Gaetani P, et al. Randomized trial of sacroiliac joint arthrodesis compared with conservative management for chronic low back pain attributed to the sacroiliac joint. J Bone Jt Surg - Am Vol. 2019. This randomized controlled trial demonstrated that MIS SI fusion with triangular titanium implants was safe and effective at 2 years for the treatment of chronic sacroiliac joint pain when compared to conservative management.
Dengler J, Duhon B, Whang P, Frank C, Glaser J, Sturesson B, et al. Predictors of outcome in conservative and minimally invasive surgical management of pain originating from the sacroiliac joint. Spine (Phila Pa 1976). 2017.
Darr E, Cher D. Four-year outcomes after minimally invasive transiliac sacroiliac joint fusion with triangular titanium implants. Med Devices Evid Res. 2018.
Montenegro TS, Hoelscher C, Hines K, Thalheimer S, Matias C, Wilent B, et al. The impact of intraoperative image-guidance modalities and neurophysiologic monitoring in the safety of sacroiliac fusions. Glob Spine J. Global Spine J. 2021.
Bessar AAA, Arnaout MM, Basha MAA, Shaker SE, Elsayed AE, Bessar MA. Computed tomography versus fluoroscopic guided-sacroiliac joint injection: a prospective comparative study. Insights Imaging. 2021.
Schoell K, Buser Z, Jakoi A, Pham M, Patel NN, Hsieh PC, et al. Postoperative complications in patients undergoing minimally invasive sacroiliac fusion. Spine J. 2016.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Caio M. Matias, Lohit Velapagapudi, and Thiago S. Montenegro declare no conflict of interest. Joshua E. Heller is a consultant for SI-BONE participating in surgeon education.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Anesthetic Techniques in Pain Management
Rights and permissions
About this article
Cite this article
Matias, C.M., Velagapudi, L., Montenegro, T.S. et al. Minimally Invasive Sacroiliac Fusion—a Review. Curr Pain Headache Rep 26, 173–182 (2022). https://doi.org/10.1007/s11916-022-01016-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11916-022-01016-y