Abstract
Purpose
The purpose of this study was to evaluate the surgical management of an osteoblastoma involving the entire C2 vertebra.
Materials and methods
A 14-year-old girl presented with unbearable neck pain. Her medical history was unremarkable. Computed tomography and magnetic resonance imaging revealed lytic and osteoblastic bone lesions involving the entire C2 vertebra. The tumor was resected in two stages with vertebral artery mobilization. Histological examination confirmed the diagnosis of osteoblastoma. The pain resolved postoperatively, and the patient had no further complaints. Sufficient fusion formation and no tumor recurrence with no complaints were seen in postoperatively 4 years.
Conclusion
Marginal resection remains the best treatment for osteoblastoma of the spine. If tumor tissue surrounds the vertebral artery, the vertebral artery should be mobilized and the surrounding tumor mass excised.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoblastomas constitute less than 1 % of all bone tumors and generally develop from the long bones and posterior vertebral elements [1]. Unlike those in other regions, cervical osteoblastomas often occur in the vertebral body. Osteoblastoma of the cervical region is uncommon, and there are few reports of its treatment. The most common symptom is pain. However, they can cause neurological deficits and deformities depending on the location in the spine [2].
Osteoblastomas of C2 may envelop the vertebral artery. Removal of the entire tumor with preventing VA is difficult [2]. We report a successful outcome following resection of a C2 osteoblastoma with vertebral artery liberation and the restoration of spinal stability.
Case
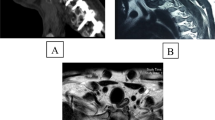
A 14-year-old girl presented with constant pain in the neck for 6 months. She had no history of trauma or other disease. The neurological examination was normal. Cervical computed tomography (CT) and magnetic resonance imaging (MRI) showed lytic and osteoblastic bone lesions that involved in the entire C2 vertebra, but they had not invaded the surrounding tissues (Figs. 1, 2).
Surgery was planned. First, laminectomy of C2 with removal of intervertebral joints was performed, and the posterior portion of the mass to the vertebral artery was excised totally with a posterior approach, and the vertebral arteries were freed. After stabilizing the spine with screws in the occiput and lateral mass of C3–C4, posterior fusion was performed using two autologous rib grafts. The posterior grafts were fixed to the occiput by insert under the occipital plate, atlas by connecting rope and C3–C4 laminae by compressing under rods. Before performing the anterior resection, we waited for 1.5 months to allow better integration of the bone screws and posterior grafts. Some relief of the neck pain in the period between the two stages was observed. Then, the odontoid and the mass located anterior to the vertebral artery were excised totally via the anterolateral/retropharyngeal approach to the high cervical spine. An autologous rib graft was placed between C1 anterior arch and C3 corpus under compression. The graft attached to C1 anterior arch with fish-mouth shaped and stabilized to C3 body with miniplates after decortications of C1 anterior arch and C3 corpus. Bone Wax (Aesculap Implant Systems) and FLOSEAL Hemostatic Matrix (Baxter) were used for control of bleeding. In addition, meticulous homeostasis was performed. Excessive bleeding was not observed in both approaches.
The patient had no postoperative problems. Histopathology of the tumor specimen was in keeping with a diagnosis of osteoblastoma. No adjuvant therapy was applied postoperatively. A cervical collar with chin support was recommended for 3 months. At the 4-year follow-up, the patient had no additional complaints, and fusion was detected in the cervical spine radiographs (Fig. 3). No recurrence was observed on cervical MRI (Fig. 4).
Discussion
Osteoblastomas are rare, benign, primary bone tumors that arise from osteoblasts [3]. They constitute 1 % of all bone tumors and 5 % of spinal tumors and occur mostly in individuals younger than 30 years old [4]. Most involve the long bones and spine, but they can also occur in the mandible and hand bones. They typically originate from the spinous processes and lamina in the spine [4, 5].
Although osteoblastomas are similar to osteoid osteomas from a histological perspective, they are less sclerotic and more aggressive than are osteoid osteomas [1]. Some osteoblastomas can recur locally and metastasize. Furthermore, in the spine, osteoblastomas are more frequent than osteoid osteomas [6].
Clinically, the most frequent symptom of an osteoblastoma is pain, whereas other findings depend on the location of the tumor in the spine. Unlike osteoid osteomas, the pain of osteoblastomas does not increase at night. The pain is not relieved with acetylsalicylic acid. The pain is nonspecific, which can delay the diagnosis [7]. With growth, spinal osteoblastomas may lead to scoliosis, radiculopathy, or myelopathy [7]. In our case, the interval between the onset of pain and the diagnosis was 6 months.
To diagnose the disease, CT and MRI are used. CT can show lytic bone lesions and expansive masses, whereas MRI can show soft tissue invasion [3]. If the diagnosis is not made using CT and MRI, a technetium bone scan can be performed [3].
The spinal tumors were staged according to the Enneking system: st.2 for active lesions and st.3 for benign aggressive lesions [8]. St.2 lesions were defined as mostly combined lytic and osteosclerotic image, with well defined borders. Frequently the lytic area is found surrounding an ossified core, strongly resembling the appearance of an osteoid osteoma. Diameter, by definition, must be superior to two cm. The clinical course is slowly progressive with pain and possible deformity related to muscle spasm. The lesion does not infiltrate the soft tissues. St.3 lesions were defined as fully lytic images, eroding the cortex and invading the canal and/or the surrounding soft tissues. The margins are not well defined, confirming the aggressiveness of the tumor. Some spot of pathologic bone can be found inside the lesion. The clinical course is faster with early possible neurologic symptoms.
Intralesional excision proved to be effective in st.2 lesions and en bloc resection in st.3 [9]. In our case, the osteoblastoma is st 2. So marginal resection is enough.
The goal of treating spinal osteoblastomas is to remove the tumor entirely and ensure the stability of body structures. The vertebral artery is located just anterolateral to the C2 pedicle and enters the transverse foramen [10]. A tumor at this level may envelop the vertebral artery. In this situation, as in our case, tumor resection should be performed after mobilization of the vertebral artery.
The anterolateral/retropharyngeal approach provides relatively easy access to the anterior arch of C1 and to the vertebral bodies of C2–C4 and can be applied to a variety of different conditions. In addition, this approach may be a viable alternative to the transoral route and its associated morbidities. In our case, the mass located anterior to the vertebral artery was excised totally via the anterolateral/retropharyngeal approach with no morbidities.
Radiotherapy can be applied to any residual mass, although malignant transformation has been reported following radiotherapy [11]. In our case, no adjuvant therapy was applied postoperatively because of the known risk for malignant transformation and also marginal resection was applied. The complete resection of the lesion can prevent recurrence and malignant transformation [3]. The only treatment in osteoblastomas is the radical excision.
Conclusion
The best treatment for osteoblastomas in the spine is resection with a wide margin, instrumentation in unstable cases, and autologous grafting with fusion. If tumor tissue surrounds the vertebral artery, the vertebral artery should be mobilized and the surrounding tumor mass excised.
References
Lucas DR, Unni KK, McLeod RA, O’Connor MI, Sim FH (1994) Osteoblastoma: clinicopathologic study of 306 cases. Hum Pathol 25:117–134
Tripathy P, Sarkar S, Maiti B (1999) Osteoblastoma of dorsal spine: a case report. Neurol India 47:330–331
Amirjamshidi A, Abbassioun K (2010) Osteoblastoma of the third cervical vertebra in a 16-year-old boy: case report and review of the literature. Pediatr Neurosurg 46:396–401
Saifuddin A, White J, Sherazi Z, Shaikh MI, Natali C, Ransford AO (1998) Osteoid osteoma and osteoblastoma of the spine. Factors associated with the presence of scoliosis. Spine 23:47–53
Haller JM, Iwanik M, Shen FH (2011) Clinical relevant anatomy of high anterior cervical approach. Spine 36:2116–2121
Stavridis SI, Pingel A, Schnake KJ, Kandziora F (2013) Diagnosis and treatment of a C2-osteoblastoma encompassing the vertebral artery. Eur Spine J 22:2504–2512
Jiang L, Liu XG, Wang C, Yang SM, Liu C, Wei F, Wu FL, Zhou H, Dang L, Liu ZJ (2015) Surgical treatment options for aggressive osteoblastoma in the mobile spine. Eur Spine 24:1778–1785
Enneking WF (1986) A system of staging musculoskeletal neoplasms. Clin Orthop Relat Res 204:9–24
Boriani S, Amendola L, Bandiera S, Simoes CE, Alberghini M, Di Fiore M, Gasbarrini A (2012) Staging and treatment of osteoblastoma in the mobile spine: a review of 51 cases. Eur Spine J 21:2003–2010
Saetia K, Phankhongsab A (2015) C2 anatomy for translaminar screw placement based on computerized tomographic measurements. Asian Spine J 9:205–209
Singh DK, Das KK, Mehrotra A, Srivastava AK, Jaiswal AK, Gupta P, Behari S, Kumar R (2013) Aggressive osteoblastoma involving the craniovertebral junction: a case report and review of literature. J Craniovertebr Junction Spine 4:69–72
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has any potential conflict of interest.
Rights and permissions
About this article
Cite this article
Koc, K., Ilik, M.K. Surgical management of an osteoblastoma involving the entire C2 vertebra and a review of literature. Eur Spine J 25 (Suppl 1), 220–223 (2016). https://doi.org/10.1007/s00586-016-4445-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-016-4445-0