Abstract
Purpose
Limited hip flexion may lead to a poor lumbopelvic motion during seated active hip flexion in people with low-back pain (LBP). The purpose of this study was to compare lumbopelvic motion during seated hip flexion between subjects with and without LBP accompanying limited hip flexion.
Methods
Fifteen patients with LBP accompanying limited hip flexion and 16 healthy subjects were recruited. The subjects performed seated hip flexion with the dominant leg three times. A three-dimensional motion-analysis system was used to measure lumbopelvic motion during seated hip flexion.
Results
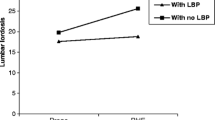
During seated active hip flexion, the angle of hip flexion was significantly lower in patients with LBP accompanying limited hip flexion (17.4 ± 4.4 in the LBP group, 20.8 ± 2.6 in the healthy group; t = 2.63, p = 0.014). The angle of the lumbar flexion (4.8 ± 2.2 in the LBP group, 2.6 ± 2.0 in the healthy group; t = −2.96, p = 0.006) and posterior pelvic tilting (5.0 ± 2.6 in the LBP group, 2.9 ± 2.0 in the healthy group; t = 2.48 p = 0.019), however, were significantly greater in patients with this condition.
Conclusions
The results of this study suggest that limited hip flexion in LBP can contribute to excessive lumbar flexion and posterior pelvic tilting during hip flexion in the sitting position. Further studies are required to confirm whether improving the hip flexion range of motion can reduce excessive lumbar flexion in patients with LBP accompanying limited hip flexion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The majority of the population experience non-specific low-back pain (LBP) at least once in a lifetime [1, 2]. Non-specific LBP comprises a large proportion of LBP cases, and the cost of treating LBP is high [3–5]. Several studies have demonstrated factors contributing to the development of LBP, and LBP patients present with various symptoms or behaviors [6–8]. For this reason, clinicians and investigators have sought to determine sources and/or causes of LBP based on posture and movement tests, and to provide guidelines for the management of LBP [9–12].
Sahrmann [11] and Harris-Hayes et al. [12] suggested that LBP occurred as a result of repetitive movement in specific sites in the lumbar region, and movement impairment can be explained by a direction-based mechanism of provocation or relief of symptoms and/or pain. Comerford and Mottram [13] reported that movement dysfunction is often present at the site and in the direction of uncontrolled motion of the lumbar region. Previous reports proposed that altered strategies for postural and movement control should be identified through movement tests and the abnormal movement pattern should be modified because altered movement patterns of the lumbar spine might contribute to the development of LBP [11–13].
The normal angle of hip flexion is 120° in healthy people performing functional activities [14, 15], and hip flexion flexibility is required to perform many daily activities, such as squatting, putting on shoes and socks, and riding a bicycle [16–19]. Since the hip joint and lumbar spine are both adjacent to the pelvis, the hip joint moves in cooperation with the lumbar spine to provide functional movement [20–22]. However, limited hip flexion range can be a risk factor contributing to musculoskeletal pain syndromes, changing mechanical forces, and potentially leading to excessive stress in the lumbopelvic region [1, 2, 23, 24]. In previous studies, it has been demonstrated that insufficient hip mobility contributes to excessive lumbar motion during forward bending, resulting in LBP [24]. Seated hip flexion is involved in daily living activities such as a cyclist, driving, putting socks and crossed leg posture. In addition, hip flexion motion in sitting is frequently used for strengthening and manual muscle testing of the hip flexor muscle. Although the association between LBP and hip flexibility is considered important, effects on the lumbopelvic region have not been assessed sufficiently during seated hip flexion in patients with LBP [1, 2, 23, 24]. Thus, clinicians and researchers must focus on examining hip motion to consider the effects of limited hip flexion in sitting in terms of kinematic changes in lumbopelvic motion.
To date, studies of lumbopelvic motion have been conducted through kinematic investigation into LBP; however, no reported study has examined the effects of limited hip flexion on lumbopelvic motion in LBP during hip flexion in sitting [2, 4, 7, 19]. A kinematic study of lumbopelvic motion may be helpful in understanding altered movement strategies in subjects with LBP accompanying limited hip flexion during seated hip flexion. Thus, the aim of this study was to investigate lumbopelvic motion during seated hip flexion in subjects with LBP accompanying limited hip flexion. Through this study, we aimed to provide clinical information to support the assessment of movement impairment and propose treatment strategies for LBP. It was hypothesized that subjects with LBP accompanying limited hip flexion would (1) display a decreased range of the hip flexion and (2) demonstrate increased lumbopelvic motion in the sagittal plane during seated active hip flexion.
Methods
Target population
In total, 77 subjects were screened by a physical therapist skilled in the evaluation and management of LBP and 46 subjects who were unsuitable for the study were excluded (Fig. 1). Fifteen subjects with LBP accompanying limited hip flexion (11 males, four females) and 16 age-matched subjects without LBP or limited hip flexion (10 males, six females) participated (Table 1). All subjects with LBP were considered to have experienced LBP on at least half of the days in the past 12 weeks with a limited range of passive hip flexion (90–110°). Subjects were excluded if they reported (1) hip or knee injuries in the previous 6 months, (2) a history of a spinal fracture or surgery, (3) spinal deformity, as defined by a physician, or (4) any systemic inflammatory condition or other serious medical condition that could affect the ability to move. The subjects without LBP displayed no history of LBP and had a range of passive hip flexion >110°. All subjects possessed strength in the hip flexors above the “fair plus” grade on manual muscle testing [25].
All participants signed an informed consent statement and were supplied with information sheets prior to participation. This study was approved by the Yonsei University Wonju Campus Human Studies Committee. No subjects with LBP showed any acute symptom or pain during the test.
Outcome measures
The severity and perception of the LBP experience were measured using the visual analog scale (VAS) [6]. The VAS was a 10-cm line anchored at the two ends with “no pain” at 0 and “worst pain” at 10. Subjects with LBP accompanying limited hip flexion were asked to mark their pain level on the line. The modified Oswestry Disability Index (ODI) was used to measure pain and disability in LBP patients [6, 26]. The modified ODI consists of 10 items with six answers per item, and items are scored from 0 to 5. The total score for each subject was presented as a relative value (total possible score/total score × 100).
Subjects were asked to sit on a stool with no back or armrests, with the hips and knees flexed at 90°. Before testing, all subjects were provided with an explanation of the test procedure by the examiner and were allowed to practice ten times to become familiarized with the test. Since the starting posture could affect the lumbar or pelvic angle during the test, it was standardized using a plumb line hung from the ceiling. The plumb line, which was perpendicular to the floor, was aligned with the external auditory meatus, acromion, and greater trochanter. The target bar was placed at a position requiring 20° hip flexion from the starting position; the 20° hip flexion angle was set using a universal goniometer. Subjects were asked to cross their arms and look straight ahead. Then, they were instructed to raise the dominant leg at a preferred speed until the midpoint of the distal femur between the medial and lateral epicondyle touched the target bar located at a level of 110° of hip flexion (Fig. 2). Kinematic data were collected from the starting position until the distal femur touched the target bar. Subjects performed the trial three times, and 3-min rest periods were allowed between trials.
A three-dimensional motion-analysis system (Vicon MX system, Oxford Metrics, Oxford, UK) was used to measure the angles of hip flexion, lumbar flexion, lumbar lateral bending, lumbar rotation, and posterior pelvic tilting during seated hip flexion. Kinematic data were collected using six cameras and processed using Nexus 1.4 software. The sampling rate was 60 Hz. The reflective markers (14-mm circles) were placed on specific anatomical landmarks of the lumbar spine, pelvis, and both lower limbs. Four markers were placed on the lower back: on the spinous processes of T12 and L1, and on the left and right sides of the spinous process of L1. The center-to-center distance between the markers was 3 cm. Sixteen markers were placed bilaterally on the subject’s anterior superior iliac spine, posterior superior iliac spine, lateral aspect of the thigh, lateral epicondyle of the femur, lateral surface of the shank, lateral malleolus, second metatarsal head, and the posterior midpoint of the calcaneus. The pelvic angle was defined as the angle between the pelvis and the transverse plane. The angle of the hip joint and the lumbar spine was derived from the relative orientation of each segment and the pelvic segment.
The kinematic data obtained by Nexus were imported into Polygon software (Oxford Metrics, Ltd., Oxford, UK). To obtain the angular displacement of the hip, lumbar spine, and pelvis during seated hip flexion, the start and end points were determined by the movement of knee markers. The angular data for hip flexion were then normalized to 100 % of the total phase duration. Subsequently, kinematic variables were calculated by the difference in angles between the end and start position of hip flexion. The kinematic data were averaged across the three trials for each subject.
Statistical analyses
PASW 18.0 for Windows (SPSS, Inc., Chicago, IL, USA) was used to perform all statistical analysis. The Shapiro–Wilk test was conducted to ensure a normal distribution of the variables (kinematic data of the hip, lumbar, and pelvis). All variables were confirmed to be normally distributed; thus, parametric statistics were used. An independent t test was used to compare the angles of the hip, lumbar spine, and pelvis during seated hip flexion between two groups. The level of statistical significance was set at p < 0.05.
Results
Description of samples
No significant differences were observed in age, height, weight, and body mass index between the subjects with and without LBP accompanying limited hip flexion (p > 0.05). The pain duration, VAS, and modified ODI scores for LBP in subjects with accompanying limited hip flexion are shown in Table 1. The passive hip flexion angles differed significantly between the two groups (p < 0.01).
Kinematic data
Data on angular displacements of hip flexion, lumbar flexion, lumbar lateral bending, lumbar rotation, and posterior pelvic tilting during seated hip flexion (0–100 %) are summarized in Table 2. Significant differences were evident in the angles of hip flexion, lumbar flexion, and posterior pelvic tilting. The angle of hip flexion was significantly lower in subjects with LBP accompanying limited hip flexion (p = 0.014). The angle of lumbar flexion, however, was significantly greater in subjects with LBP accompanying limited hip flexion (p = 0.006). The angle of posterior pelvic tilting in subjects with LBP accompanying limited hip flexion also significantly increased compared with that in subjects without LBP accompanying limited hip flexion (p = 0.019). No significant difference was observed in lumbar lateral bending or lumbar rotation between the groups (p > 0.05).
Discussion
The purpose of this study was to compare lumbopelvic motion during seated hip flexion in subjects with and without LBP accompanying limited hip flexion. Consistent with our hypotheses, the results of this study showed significant differences in the angle of hip flexion and lumbopelvic motion during seated hip flexion in subjects with and without LBP accompanying limited hip flexion. When asked to raise the leg to a point 20° of hip flexion from the starting position, subjects with LBP accompanying limited hip flexion demonstrated significantly lower active ranges of hip flexion and greater lumbar flexion and posterior pelvic tilting compared with those without LBP accompanying limited hip flexion.
In our study, we selected a target bar height of 20° of hip flexion from a sitting position. Although the possible range of motion of flexion in the supine position has been stated to be 120° [14, 15], there is no reported study of the hip flexion range in a sitting posture for performing functional activities. Previous kinematic studies have demonstrated that high hip flexion, i.e., 95–114°, occurs in daily activities such as sitting with legs crossed, squatting, and putting on socks, in asymptomatic subjects [16, 27, 28]. Thus, we selected a target bar position of 20° hip flexion from a sitting posture.
In the present study, although the angle of hip flexion was lower, posterior pelvic tilting and lumbar flexion significantly increased in subjects with LBP accompanying limited hip flexion during seated hip flexion. When hip flexion was performed in the seated position, the flexed knee could remove the effects of the shortened or stiff hamstring. However, other muscles of the hip joint, including the gluteus maximus, posterior capsule, and ligament, could not be excluded in this study [11, 21]. It is possible to increase the tension of the hip extensors, posterior capsule, and ligament in subjects with limited hip flexion. In the present study, although the angle of hip flexion was lower, posterior pelvic tilting significantly increased in subjects with LBP accompanying limited hip flexion during seated hip flexion. Thus, the subjects with limited hip flexion could not perform “true” hip flexion, but compensated by posterior pelvic tilting and lumbar flexion, due to an insufficient length or increased tension of the posterior muscle, capsule, and ligament of the hip.
Mechanical stability of the lumbar spine is essential to prevent disc degeneration and facet joint osteoarthritis [29, 30]. Previous studies have demonstrated that repetitive and excessive lumbar flexion motion can increase compressive forces in the lumbar spine and affect disc degeneration during daily activities [29–32]. Kuo et al. [33] reported that interdiscal pressure was 0.9 MPa at level L1/L2 in lumbar flexion, which is a greater value when compared with extension, rotation, and standing postures. In addition, intervertebral discs and ligaments are highly vulnerable to injury in combined spine action of the forward bending and compression, such as when lifting objects [32]. Thus, in our study, the increased lumbar flexion motion during seated hip flexion in people with LBP accompanying limited hip flexion may contribute to increase interdiscal pressure and LBP.
In LBP, a limited range of hip motion could lead to compensation in the lumbopelvic area during lower limb movement. Repetitive increased lumbopelvic motion leads to progressively excessive stress, microtrauma, and pain in the lumbar spine region [7, 34, 35]. Scholtes et al. [7] found that movement patterns of the hip and lumbopelvic area in athletes with a history of LBP displayed greater lumbopelvic rotation compared with those in healthy athletes while performing hip lateral rotation and knee flexion. It was suggested that a greater lumbopelvic rotation angle may induce increased mechanical stress in the lumbopelvic region, resulting in LBP. In the present study, the angle of lumbar flexion and posterior pelvic tilting was increased by approximately 2.2° and 2.0°, respectively, in subjects with LBP accompanying limited hip flexion compared with subjects without them. Increasing flexion over the whole lumbar spine from a neutral posture could cause damage to the low back, and greater changes may occur in common movements such as walking, riding a bike, putting on socks, and running. Furthermore, such compensation in the pelvic and lumbar region should be considered a standard part of LBP rehabilitation during core strengthening exercises in a sitting position.
An altered movement strategy is another possible explanation for the greater angle of lumbar flexion and posterior pelvic tilting in subjects with LBP accompanying limited hip flexion. A previous study suggested that excessive lumbopelvic movements during limb movement were due to both biomechanical restriction and learned movement strategies [7]. If the onset of lumbar flexion and posterior pelvic tilting occurs in the early phase, prior to reaching the targeted end range of hip flexion, a changed movement strategy could be a plausible reason. Therefore, both exercises to improve the flexibility of the hip joint and motor-control training for lumbopelvic stabilization should be considered when performing seated hip flexion exercises in patients with LBP accompanying limited hip flexion.
This study has several limitations. First, these findings cannot be generalized to other age groups because the subjects were all in their early twenties. Spine posture and range of motion depend on age [36]. Thus, it is necessary to conduct the experiments in other age groups. Second, although we selected a target motion of 20° hip flexion, the overall combination of hip flexion and pelvic tilt exceeded the target motion of 20° by 2.4° and 3.7° in the LBP and control groups, respectively. These greater motions could have occurred because of differences between measurements by the goniometer and by the Vicon motion-analysis system. We set the 20° target angle using a universal goniometer, and the placement of the goniometer axis and the center of the Vicon reflective marker over the hip joint may have differed. Third, it was difficult to demonstrate a cause-effect relationship between excessive lumbopelvic motion and limited hip flexion, as this study was a cross-sectional study. It was unclear whether the increased lumbopelvic motion and limited hip flexion led to pain in the lumbar region or whether LBP induced the limited hip and excessive lumbopelvic motion. Despite this limitation, the findings are important, as they demonstrate that increased lumbopelvic motion may contribute to LBP and lead to aggravation or a reproduction of pain in the lumbar region.
Conclusions
The purpose of this study was to investigate lumbopelvic motion during seated hip flexion in subjects with LBP accompanying limited hip flexion. The results of this study showed that subjects with LBP accompanying limited hip flexion demonstrated a significantly decreased angle of hip flexion and increased lumbar flexion and posterior pelvic tilting, compared with controls without the condition during seated hip flexion. Clinically, it is important to assess relative lumbopelvic motions during hip flexion in a sitting position, and these finding may help to prevent and treat LBP accompanying limited hip flexion.
References
Harris-Hayes M, Sahrmann SA, Van Dillen LR (2009) Relationship between the hip and low back pain in athletes who participate in rotation-related sports. J Sport Rehabil 18:60–75
Shum GL, Crosbie J, Lee RY (2007) Three-dimensional kinetics of the lumbar spine and hips in low back pain patients during sit-to-stand and stand-to-sit. Spine 32:211–219
Lin CW, Haas M, Maher CG et al (2011) Cost-effectiveness of guideline-endorsed treatments for low back pain: a systematic review. Eur Spine J 20:1024–1038
Porter JL, Wilkinson A (1997) Lumbar-hip flexion motion. A comparative study between asymptomatic and chronic low back pain in 18- to 36-year-old men. Spine 22:1508–1513
Wand BM, Hunter R, O’Connell NE et al (2009) The self-reported aggravating activities of people with chronic non-specific low back pain do not involve consistent directions of spinal movement: an observational study. Aust J Physiother 55:47–51
Marshall P, Murphy B (2010) Delayed abdominal muscle onsets and self-report measures of pain and disability in chronic low back pain. J Electromyogr Kinesiol 20:833–839
Scholtes SA, Gombatto SP, Van Dillen LR (2009) Differences in lumbopelvic motion between people with and people without low back pain during two lower limb movement tests. Clin Biomech 24:7–12
van Deursen LL, Patijn J, Durinck JR et al (1999) Sitting and low back pain: the positive effect of rotary dynamic stimuli during prolonged sitting. Eur Spine J 8:187–193
Fritz JM, Brennan GP, Clifford SN et al (2006) An examination of the reliability of a classification algorithm for subgrouping patients with low back pain. Spine 31:77–82
O’Sullivan P (2005) Diagnosis and classification of chronic low back pain disorders: maladaptive movement and motor control impairments as underlying mechanism. Man Ther 10:242–255
Sahrmann S (2002) Diagnosis and treatment of movement impairment syndromes. Mosby, New York
Harris-Hayes M, Van Dillen LR, Sahrmann SA (2005) Classification, treatment and outcomes of a patient with lumbar extension syndrome. Physiother Theory Pract 21:181–196
Comerford M, Mottram S (2012) Kinetic control: the management of uncontrolled movement. Churchill Livingstone, Australia
Nussbaumer S, Leunig M, Glatthorn JF et al (2010) Validity and test-retest reliability of manual goniometers for measuring passive hip range of motion in femoroacetabular impingement patients. BMC Musculoskelet Disord 11:194
Roach KE, Miles TP (1991) Normal hip and knee active range of motion: the relationship to age. Phys Ther 71:656–665
Hemmerich A, Brown H, Smith S et al (2006) Hip, knee, and ankle kinematics of high range of motion activities of daily living. J Orthop Res 24:770–781
Burnett AF, Cornelius MW, Dankaerts W et al (2004) Spinal kinematics and trunk muscle activity in cyclists: a comparison between healthy controls and non-specific chronic low back pain subjects-a pilot investigation. Man Ther 9:211–219
McHardy A, Pollard H, Fernandez M (2006) Triathlon injuries: a review of the literature and discussion of potential injury mechanisms. Clinical Chiropractic 9:129–138
Shum GL, Crosbie J, Lee RY (2005) Symptomatic and asymptomatic movement coordination of the lumbar spine and hip during an everyday activity. Spine 30:697–702
Jo HJ, Song AY, Lee KJ et al (2011) A kinematic analysis of relative stability of the lower extremities between subjects with and without chronic low back pain. Eur Spine J 20:1297–1303
Kuo YL, Tully EA, Galea MP (2010) Lumbofemoral rhythm during active hip flexion in standing in healthy older adults. Man Ther 15:88–92
Tully EA, Wagh P, Galea MP (2002) Lumbofemoral rhythm during hip flexion in young adults and children. Spine 27:432–440
Ellison JB, Rose SJ, Sahrmann SA (1990) Patterns of hip rotation range of motion: a comparison between healthy subjects and patients with low back pain. Phys Ther 70:537–541
Wong TK, Lee RY (2004) Effects of low back pain on the relationship between the movements of the lumbar spine and hip. Hum Mov Sci 23:21–34
Kendall FP, McCreary EK, Provance PG (2005) Muscles: Testing and function, 5th edn. Williams & Wilkins, Baltimore
Maughan EF, Lewis JS (2010) Outcome measures in chronic low back pain. Eur Spine J 19:1484–1494
Kapoor A, Mishra SK, Dewangan SK et al (2008) Range of movements of lower limb joints in cross-legged sitting posture. J Arthroplasty 23:451–453
Shum GL, Crosbie J, Lee RY (2005) Symptomatic and asymptomatic movement coordination of the lumbar spine and hip during an everyday activity. Spine 30:697–702
Adams M, Dolan P (1995) Recent advances in lumbar spinal mechanics and their clinical significance. Clin Biomech 10:3–19
Fujiwara A, Tamai K, An HS et al (2000) The relationship between disc degeneration, facet joint osteoarthritis, and stability of the degenerative lumbar spine. J Spinal Disord 13:444–450
Adams MA, Dolan P (1991) A technique for quantifying the bending moment acting on the lumbar spine in vivo. J Biomech 24:117–126
Dolan P, Earley M, Adams MA (1994) Bending and compressive stresses acting on the lumbar spine during lifting activities. J Biomech 27:1237–1248
Kuo CS, Hu HT, Lin RM et al (2010) Biomechanical analysis of the lumbar spine on facet joint force and intradiscal pressure–a finite element study. BMC Musculoskelet Disord 5(11):151
Scholtes SA, Norton BJ, Lang CE et al (2010) The effect of within-session instruction on lumbopelvic motion during a lower limb movement in people with and people without low back pain. Man Ther 15:496–501
McGill SM (1997) The biomechanics of low back injury: implications on current practice in industry and the clinic. J Biomech 30:465–475
Consmüller T, Rohlmann A, Weinland D et al (2012) Comparative evaluation of a novel measurement tool to assess lumbar spine posture and range of motion. Eur Spine J 21:2170–2180
Acknowledgments
The authors thank the subjects for participating in the study and for their helpful assistance in the preparation of this paper.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Study information
The protocol for this study was approved by the Yonsei University Wonju Campus Human Studies Committee.
Rights and permissions
About this article
Cite this article
Kim, Sh., Kwon, Oy., Yi, Ch. et al. Lumbopelvic motion during seated hip flexion in subjects with low-back pain accompanying limited hip flexion. Eur Spine J 23, 142–148 (2014). https://doi.org/10.1007/s00586-013-2973-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-013-2973-4