Abstract
Purpose
To compare the short- and long-term clinical outcomes, operation times, restoration rate, dosage of polymethylmeth-acrylate (PMMA) injected, complications and X-rays exposure frequency between unilateral and bilateral kyphoplasty approaches for the treatment of OVCF.
Study design
Systematic review and meta-analysis.
Methods
Randomized or non-randomized controlled trials published up to April 2015 that compared the unilateral and bilateral PKP for the treatment of OVCF were acquired by a comprehensive search in the Cochrane Controlled Trial Register, PubMed, MEDLINE, EMBASE, Web of Science, OVID. Exclusion criteria were patients with neoplastic etiology (metastasis or myeloma), infection, neural compression syndrome, invasive and degenerative disease, traumatic fracture, re-operation, neurological deficits, significant scoliosis and spinal stenosis. The main end points included: operation times, the short- and long-term postoperative Visual Analogue Scale (VAS) scores, the short-term postoperative Oswestry Disability Index (ODI), restoration rate, dosage of PMMA injected, cement leakage, X-ray exposure frequency and postoperative adjacent-level fractures.
Results
A total of 8 studies involving 428 patients were included in the meta-analysis. The mean operative time was shorter in the unilateral groups compared with the bilateral groups [P < 0.05, weighted mean difference (WMD) −19.74 (−30.56, −8.92)]. There was no significant difference in the short-term postoperative VAS scores [P > 0.05, WMD 0.03 (−0.34, 0.40)], the long-term postoperative VAS scores between them [P > 0.05, WMD 0.01 (−0.42, 0.45)] and the short-term postoperative ODI [P > 0.05, WMD −0.33 (−2.36, 1.69)] between the two groups. The unilateral approaches required significantly less dosage of PMMA than the bipedicular approaches did [P < 0.05, WMD −1.56 (−1.59, −1.16)]. The restoration rate in the bilateral groups was higher than the unilateral groups [P < 0.05, WMD −7.82 (−12.23, −3.41)]. There was no significant difference in the risk ratio of cement leakage [P > 0.05, RR 0.86 (0.36, 2.06)] and postoperative adjacent-level fractures [P > 0.05, RR 0.91 (0.25, 3.26)] between the two methods. The mean X-ray exposure frequency in the unilateral groups was greater than the bilateral groups [P < 0.05, WMD −5.69 (−10.67, −0.70)].
Conclusions
A definitive verdict could not be reached regarding which approach is better for the treatment of OVCF. Although unilateral PKP was associated with shorter operative time, less X- ray exposure frequency and dosage of PMMA than bilateral PKP. There was no apparent difference in the short- and long-term clinical outcomes and complications between them. However, bilateral PKP approaches were higher than unilateral PKP in term of the restoration rate. But on account of lack of some high-quality evidence, we hold that amounts of high-quality randomized controlled trials should be required and more complications should be analysed to resolve which surgical approach is better for the treatment of OVCF in the future.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The traditional treatment for OVCF consists of conservative management, including bed rest, analgesia, and brace and physical therapy after symptomatic relief. Unfortunately, due to long-term in bed, it is easier result in patients with bone demineralization and worsening the condition. Except for that, for patients who are unable to tolerate progressive deformity and debilitating pain of some fractures, procedures such as percutaneous kyphoplasty (PKP) should be considered. PKP was first performed in 1999, and has been widely regarded as a minimally invasive technique for OVCF that uses a balloon tamp inserted into the vertebral body by a transpedicular approach, followed by fixation of the fracture fragments with PMMA bone cement [1, 2]. PKP can increase bone strength and reduce the pain caused by OVCF and restore the height of the vertebral bodies. Many literatures have reported that PKP can reduce immediate pain compared with conservative treatments and that can improve function, disability and quality of life more effectively than nonsurgical therapy without increasing the risk of additional vertebral fractures [3–6]. In addition, PKP for OVCF can be divided into unilateral and bilateral PKP approaches. Traditional bilateral PKP approaches were regarded as safe and effective. Nevertheless, unilateral PKP approaches were accepted attribute to surgical time, safety, and less expense [7, 8].
A recent systematic review indicated that the unilateral approach should be considered, because unilateral required less cement to be injected and had a lower risk of cement leakage than bilateral approach did [2]. However, some studies have reported that no clinically important differences were found between the unilateral and bilateral PKP [9, 10]. At present, no standards or guidelines exist for the treatment of OVCF. Therefore, an evidence base was needed to help surgeons make clinical decisions and choose optimal treatments. Generally, bilateral PKP is thought to be more stable as more cement is injected in our clinical work. We performed the meta-analysis to compare the unilateral and bilateral PKP for patients with OVCF in terms of the short- and long-term clinical outcomes, operation times, restoration rate, dosage of PMMA injected, complications and X-rays exposure frequency.
Materials and methods
Search strategy and study selection
We searched for studies published up to April 2015 that compared the unilateral and bilateral PKP approaches for OVCF. The databases included the Cochrane Controlled Trial Register, PubMed, MEDLINE, EMBASE, Web of Science, OVID with no language restriction. The following search terms were used: osteoporosis, osteoporosis vertebral compression fractures, OVCF, unilateral kyphoplasty, unipedicular approach, single-balloon kyphoplasty, one-ballon kyphoplasty, double-balloon kyphoplasty, bilateral kyphoplasty, bipedicular approach, two-ballon kyphoplasty. Searches were performed by at least 2 authors independently in an unblinded standardized manner. Accuracy was confirmed by a statistician. All searches were combined to obtain an unified search strategy. A third author and consensus resolved any disagreements between reviewers. Reference lists of all included studies were scanned to identify additional potentially relevant studies. Two reviewers independently screened the titles and abstracts of identified papers, and full text copies of all potentially relevant studies were obtained.
Inclusion criteria
Studies were included in the analysis if the following inclusion criteria were met: (1) study design: randomized or non-randomized controlled study; (2) study population: participants were patients with OVCFs; (3) purpose of interventions: to compare clinical outcome differences between unilateral and bilateral kyphoplasties; (4) outcome measurements: the study reported at least one of the following outcomes: operation time, cement dosage, VAS, ODI, restoration rate, cement leakage, X-ray exposure frequency and postoperative adjacent-level fractures. Studies that did not meet the above criteria were excluded from selection.
Data extraction
Data were extracted independently by two authors, without blinding to the title and author affiliation. Relevant information was extracted from studies, included: (1) the title; (2) authors; (3) year of publication; (4) sample size; (5) gender; (6) type of intervention; (7) surgical approach; (8) duration of the follow-up; (9) the short- and long-term clinical outcomes as reflected in the VAS scores and Oswestry Disability Index; (10) cement dosage; (11) operation times; (12) X-rays exposure frequency; (13) incidence of adjacent vertebral fracture and (14) bone cement leakage; (15) restoration rate. “Short-term” was defined as within 4 weeks; “long-term” was defined as at least 6 months. The outcomes between 4 weeks and 6 months were not analyzed in our meta-analysis.
Data analysis
All the meta-analyses were performed with the Review Manager software (RevMan Version 5.3 Cochrane Collaboration). Heterogeneity was tested using Chi square test and quantified by calculating I 2 statistic, for which P < 0.1 and I 2 > 50 % was considered to be statistically significant. For the pooled effects, weighted mean difference (WMD) or standard mean difference (SMD) was calculated for continuous variables according to the consistency of measurement units, and relative ratio (RR) was calculated for dichotomous variables. Continuous outcomes are presented as mean differences and 95 % confidence intervals (CI), whereas dichotomous outcomes are presented as relative risk and 95 % CI. P < 0.05 was considered statistically significant. Random-effects or fixed-effects models were used depending on the heterogeneity of the studies included.
Results
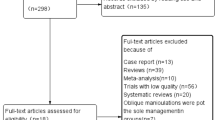
The selection process of relevant studies is summarized in Fig. 1. From the included databases, 1015 references were obtained. Because of duplicates, irrelevant studies, case reports, not comparative studies and review, 985 references were excluded by screening the titles and abstracts. The remaining 30 reports underwent a detailed and comprehensive evaluation. Finally, eight studies were included in this meta-analysis [11–18]. Table 1 summarizes the basic characteristics of included studies.
Quality and risk of bias assessment of the studies
The major baseline characteristics of participants in each study were similar. Cochrane review criteria [19] was used to assess the quality of each article included in the analysis (Table 2). Two authors independently using an unblinded standardized method to evaluate the quality and risk of bias of included studies. A third author was required if a consensus was not reached. Studies achieving a Cochrane score of 9 or higher were considered as high quality, 6–8 were considered as moderate quality, and studies scoring less than 6 were rated as having a “a high risk of bias”. In the studies, two studies scored 8 points, four studies scored 7 points and one study scored 6 points. ALL of them were of a moderate quality. However, one study scored 5 points and has a high risk of bias (Table 3). Disagreement was resolved by discussion among the authors.
Clinical outcome
Operative time
Operative time obtained in six studies involving 331 patients (166 in the unilateral surgery groups and 165 in the bilateral surgery groups) was analyzed. The mean operative time in the unilateral surgery groups was shorter than the bilateral surgery groups [P < 0.05, WMD −19.74 (−30.56, −8.92); Fig. 2].
VAS and Oswestry disability index
The short-term postoperative VAS scores obtained in six studies with a total of 334 patients (155 in the unilateral surgery groups and 179 in the bilateral surgery groups) was analyzed. There was no significant difference in the short-term postoperative VAS scores between the two groups [P > 0.05, WMD 0.03 (−0.34, 0.40); Fig. 3]. The short-term postoperative VAS scores obtained in six studies involving 325 patients (157 in the unilateral surgery approaches and 168 in the bilateral surgery approaches) was analyzed. There was no significant difference in the long-term postoperative VAS scores between them [P > 0.05, WMD 0.01 (−0.42, 0.45); Fig. 4]. The short-term postoperative ODI obtained in two studies embracing 103 patients (48 in the unilateral PKP groups and 55 in the bilateral PKP groups) was analyzed. There was also no significant difference in the short-term postoperative ODI between the unilateral surgery groups and the bilateral surgery groups [P > 0.05, WMD −0.33 (−2.36, 1.69); Fig. 5].
Restoration rate
Restoration rate obtained in two studies with a total of 108 patients (60 in the unilateral surgery groups and 48 in the bilateral surgery groups) was analyzed. In the included studies, Chen et al. [11] reported that the average percentage of RR was 25.84 ± 13.79 % in unilateral groups, and 32.32 ± 10.33 % in bilateral groups. From the research of Chen et al. [13], the RR in unilateral method and in bilateral approach was 24.97 ± 13.97 and 34.16 ± 8.31 % 24 months after surgery. The restoration rate in the bilateral surgery groups was higher than the unilateral surgery groups [P < 0.05, WMD −7.82 (−12.23, −3.41); Fig. 6]. The restoration rate (RR) was calculated after surgery: (restored vertebral height-initial fracture height)/adjacent normal vertebral height.
Cement dosage
Cement dosage obtained in six studies involving 325 patients (157 in the unilateral surgery groups and 168 in the bilateral surgery groups) was analyzed. The unilateral approach required significantly less dosage of PMMA than the bipedicular approach did [P < 0.05, WMD −1.56 (−1.59, −1.16); Fig. 7].
Cement leakage
The risk ratio for cement leakage obtained in five studies embracing 284 patients (139 in the unilateral surgery groups and 145 in the bilateral surgery groups) was analyzed. There was no statistically significant difference in the risk ratio of cement leakage between the unilateral approaches and the bilateral approaches [P > 0.05, RR 0.86 (0.36, 2.06); Fig. 8].
Postoperative adjacent-level fractures
The risk ratio for postoperative adjacent-level fractures obtained in two studies with a total of 99 patients (51 in the unilateral surgery groups and 48 in the bilateral surgery groups) was analyzed. There was no statistically significant difference in the risk ratio of postoperative adjacent-level fractures between the two approaches [P > 0.05, RR 0.91 (0.25, 3.26); Fig. 9].
X-ray exposure frequency
X-ray exposure frequency obtained in two studies involving 130 patients (59 in the unilateral surgery groups and 71 in the bilateral surgery groups) was analyzed. Patients were exposed to X-rays 37 ± 12 times in the unilateral PKP group and 65 ± 19 times in the bilateral PKP group in study of Wang et al. [15]. However, Wang et al. [16] indicated that the X-ray exposure frequency was 64 ± 11 times in unilateral surgery groups, and 55 ± 16 times in bilateral surgery groups. The mean X-ray exposure frequency in the unilateral PKP approaches was greater than the bilateral PKP approaches [P < 0.05, WMD −5.69 (−10.67, −0.70); Fig. 10].
Discussion
Unilateral and bilateral kyphoplasties have been reported for the treatment of OVCF. However, due to lack of comprehensive studies comparing the clinical outcomes of both surgical kyphoplasty approaches, the optimum of surgical strategy for OVCF remains controversial. Recently, Chen et al. [2] reported that the unilateral kyphoplasty approach should be considered as an option for the treatment of osteoporosis vertebral compression fractures, based on the unilateral kyphoplasty approach required less cement to be injected and had a lower risk of cement leakage than bilateral kyphoplasty did. In addition, incorporative analysis revealed that the unilateral approach had no advantage over the bipedicular approach in pain relief at postoperative and the difference in ODI scores was still not significant between the two approaches. However, some included studies of the meta-analysis have a high risk of bias, and the relevant literature was only searched up to April 2013. Over the last 2 years, a series of comparative studies on unilateral or bilateral surgical approaches for the treatment of OVCF have been published. Therefore, it remains necessity to verify the above conclusion based on the latest studies for strong evidence. The purpose of our meta-analysis is to systematically compare surgical approaches (unilateral PKP or bilateral PKP) for the treatment of OVCF.
Eight articles from the literature search up to April 2015 were considered to be of adequate methodological quality and were included in this meta-analysis. Our meta-analysis results showed that no statistically significant differences were found in the short- and long-term postoperative VAS scores, the short-term postoperative ODI and the risk ratio of postoperative adjacent-level fractures between the two groups. Compared with the bilateral PKP surgery, the mean operation time, cement dosage and X-ray exposure frequency were significantly greater. These are similar to the results reported by others [2]. However, we also suggested that there was no statistically significant difference in the risk ratio of cement leakage between them, whereas the restoration rate in the unilateral PKP groups was lower than the bilateral PKP groups.
Cement volumes used clinically are 2–3 mL for thoracic and 3–5 mL for lumbar vertebrae or 2–10 mL for all levels [20]. Percent of cement dose (4 %, 1.2 mL on average; 12 %, 3.5 mL on average; and 24 %, 7 mL on average) were chosen to represent the low, medium, and high ranges of cement volumes at any levels injected. Graham et al. [20] found that only the highest cement dose used (24 % fill, 7 mL on average) had an effect on mechanical stiffness or strength and these improvements in stiffness and strength depended significantly on bone density. Fehlings MG [21] suggested that it is better to use a higher viscosity and a smaller dosage of bone cement. But Chen et al. [22] reported that both unipedicular PKP and bipedicular PKP can significantly increase the stiffness of compression fractured vertebral bodies. In our meta-analysis, we also obtained that the unilateral approach required significantly less dosage of PMMA than the bipedicular approach did, whereas there was no statistically significant difference in the risk ratio of postoperative adjacent-level fractures between the unilateral and bilateral surgery groups. These results fall in line with Chen [22]. In addition, Lin et al. [23] also reported that unilateral balloon KP needs less surgery time and PMMA consumption compared to bilateral balloon KP. For X-ray exposure frequency, Feng et al. [24] considered that the mean X-ray exposure frequency in the unilateral PKP approaches was greater than the bilateral PKP approaches, if only one fracture vertebral body. In addition, there was no statistically significant difference in X-ray exposure frequency between them (two doctors participate in the surgery and inject the bone cement at the same time) for participators. And for patients, the mean X-ray exposure frequency in the improved bilateral surgery groups was even less. To compare with our results, it was shown that the advantage for unilateral kyphoplasty surgery appears to be more obvious than bilateral kyphoplasty surgery in operation times, cement dosage and X-ray exposure frequency. However, we believe that both of cement dosage and X-ray exposure frequency can be controlled in the unilateral and bilateral kyphoplasty surgery procedures, such as Feng et al. [24] did. Moreover, we found that the restoration rate in the bipedicular PKP surgery groups was higher than the unipedicular PKP surgery groups. The restoration rate is an important measure of radiographic outcomes after percutaneous kyphoplasty. Doo et al. [25] reported that the decrease of vertebral body height damages the surrounding zygapophyseal joint and narrows the intervertebral foramen leading to the symptoms of paravertebral. Therefore, the restoration rate should be considered as an important evidence to compare the advantage of which surgical approach is more prominent for the treatment of OVCF.
To evaluate the short- and long-term clinical outcomes, the short-term and long-term postoperative VAS, the short-term postoperative ODI was selected for our meta-analysis, which revealed that there were no significant difference between the two groups. Similarly, Chen et al. [2] also suggested that the differences in postoperative VAS and ODI scores were not significant between the two surgical approaches. The risk ratio of cement leakage and postoperative adjacent-level fractures was analysed to assess the complications in the article. In spite of Ren et al. [26] reported that the incidence of new symptomatic VCFs after PVP was higher in osteoporotic patients with initial multiple-level fractures. We found that there were no significant difference in the risk ratio of cement leakage and postoperative adjacent-level fractures between the unilateral surgery groups and the bilateral surgery groups. Lin et al. [23] considered that both unilateral and bilateral balloon KP can provide rapid, significant, and sustained pain relief for patients with osteoporotic VCFs. And there was no evidence to prove that unilateral balloon KP results in higher incidence of PMMA leakage than bilateral balloon KP. It seems that both unilateral and bilateral PKP were safe and effective for curing OVCF. However, based on literature review, there have been many cases of pulmonary cement embolism and intercostal neuralgia reported [27–29]. Thus, these important complications should be included.
We consider that our result of meta-analysis is influenced by the following reasons: first, the description of randomization process is not sufficient in most of the studies. Although aggregate data had larger statistical power, the included studies still had various types of bias. Eight of studies have moderate quality and one has a high risk of bias. It is necessary that amounts of high-quality randomized controlled trials should be required. Second, there were only cement leakage and postoperative adjacent-level fractures in our analysis. More important complications should also be considered, such as intraoperative pulmonary cement embolism, intercostal neuralgia and cerebrospinal fluid leakage. And these complications might affect the preponderance of the two approaches and could be included by long-term follow-up. Third, the clinical outcomes of the included studies were limited, although data pooling. Thus, our meta-analysis might be limited to answer some important clinical questions. Studies contained large outcomes are required.
In summary, our meta-analysis confirmed that the bilateral approach was associated with higher restoration rate than the unilateral approach in the treatment of OVCF. There were no significant difference in the short- and long-term postoperative VAS, the short-term postoperative ODI, the risk ratio of cement leakage and postoperative adjacent-level fractures. The mean operation time, cement dosage and X-ray exposure frequency were significantly greater in the unilateral approach compared with the bilateral kyphoplasty approach.
Conclusions
In conclusion, our meta-analysis suggested that a definitive verdict could not be reached regarding which surgical approach is better for OVCF. Although unilateral PKP was associated with shorter operative time, less X-ray exposure frequency and dosage of PMMA than bilateral PKP in the treatment of OVCF. There was no apparent difference in the short- and long-term clinical outcomes and complications between the two approaches. However, bilateral PKP approaches were higher than unilateral PKP approaches in terms of the restoration rate. But on account of lack of some high-quality evidence, we consider that more high-quality randomized controlled trials are required and more complications should be analysed to resolve which surgical approach is better for OVCF treatment in the future.
References
Garfin SR, Yuan HA, Reiley MA (2001) New technologies in spine: kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures. Spine (Phila Pa 1976) 26:1511–1525
Chen H, Tang P, Zhao Y, Gao Y, Wang Y (2014) Unilateral versus bilateral balloon kyphoplasty in the treatment of osteoporotic vertebral compression fractures. Orthopedics 37:e828–e835
Klazen CA, Lohle PN, de Vries J, Jansen FH, Tielbeek AV, Blonk MC, Venmans A, van Rooij WJ, Schoemaker MC, Juttmann JR, Lo TH, Verhaar HJ, van der Graaf Y, van Everdingen KJ, Muller AF, Elgersma OE, Halkema DR, Fransen H, Janssens X, Buskens E, Mali WP (2010) Vertebroplasty versus conservative treatment in acute osteoporotic vertebral compression fractures (Vertos II): an open-label randomised trial. Lancet 376:1085–1092
Wardlaw D, Cummings SR, Van Meirhaeghe J, Bastian L, Tillman JB, Ranstam J, Eastell R, Shabe P, Talmadge K, Boonen S (2009) Efficacy and safety of balloon kyphoplasty compared with non-surgical care for vertebral compression fracture (FREE): a randomised controlled trial. Lancet 373:1016–1024
Boonen S, Van Meirhaeghe J, Bastian L, Cummings SR, Ranstam J, Tillman JB, Eastell R, Talmadge K, Wardlaw D (2011) Balloon kyphoplasty for the treatment of acute vertebral compression fractures: 2-year results from a randomized trial. J Bone Miner Res 26:1627–1637
Ma XL, Xing D, Ma JX, Xu WG, Wang J, Chen Y (2012) Balloon kyphoplasty versus percutaneous vertebroplasty in treating osteoporotic vertebral compression fracture: grading the evidence through a systematic review and meta-analysis. Eur Spine J 21:1844–1859
Korovessis P, Hadjipavlou A, Repantis T (2008) Minimal invasive short posterior instrumentation plus balloon kyphoplasty with calcium phosphate for burst and severe compression lumbar fractures. Spine (Phila Pa 1976) 33:658–667
Rhyne A, Banit D, Laxer E, Odum S, Nussman D (2004) Kyphoplasty: report of eighty-two thoracolumbar osteoporotic vertebral fractures. J Orthop Trauma 18:294–299
Huang Z, Wan S, Ning L, Han S (2014) Is unilateral kyphoplasty as effective and safe as bilateral kyphoplasties for osteoporotic vertebral compression fractures? A meta-analysis. Clin Orthop Relat Res 472:2833–2842. doi:10.1007/s11999-014-3745-0
Steinmann J, Tingey CT, Cruz G, Dai Q (2005) Biomechanical comparison of unipedicular versus bipedicular kyphoplasty. Spine 30:201–205. doi:10.1097/01.brs.0000150831.46856.87
Chen C, Chen L, Gu Y, Xu Y, Liu Y, Bai X, Zhu X, Yang H (2010) Kyphoplasty for chronic painful osteoporotic vertebral compression fractures via unipedicular versus bipedicular approachment: a comparative study in early stage. Injury 41:356–359. doi:10.1016/j.injury.2009.09.021
Song BK, Eun JP, Oh YM (2009) Clinical and radiological comparison of unipedicular versus bipedicular balloon kyphoplasty for the treatment of vertebral compression fractures. Osteoporos Int 20:1717–1723. doi:10.1007/s00198-009-0872-7
Chen CM, Wei HF, Zhang WJ, Gu Y, Tang GL, Dong RB, Xu Y, Chen L (2011) Comparative study of kyphoplasty for chronic painful osteoporotic vertebral compression fractures via unipedicular versus bipedicular approach. J Spinal Disord Tech 24:E62–E65
Chung HJ, Chung KJ, Yoon HS, Kwon IH (2008) Comparative study of balloon kyphoplasty with unilateral versus bilateral approach in osteoporotic vertebral compression fractures. Int Orthop 32:817–820. doi:10.1007/s00264-007-0439-1
Wang Z, Wang G, Yang H (2012) Comparison of unilateral versus bilateral balloon kyphoplasty for the treatment of osteoporotic vertebral compression fractures. J Clin Neurosci 19:723–726. doi:10.1016/j.jocn.2011.08.023
Wang H, Sun Z, Wang Z, Jiang W (2015) Single-balloon versus double-balloon bipedicular kyphoplasty for osteoporotic vertebral compression fractures. J Clin Neurosci 22:680–684. doi:10.1016/j.jocn.2014.10.014
Chen L, Yang H, Tang T (2011) Unilateral versus bilateral balloon kyphoplasty for multilevel osteoporotic vertebral compression fractures: a prospective study. Spine (Phila Pa 1976) 36:534–540. doi:10.1097/BRS.0b013e3181f99d70
Rebolledo BJ, Gladnick BP, Unnanuntana A, Nguyen JT, Kepler CK, Lane JM (2013) Comparison of unipedicular and bipedicular balloon kyphoplasty for the treatment of osteoporotic vertebral compression fractures: a prospective randomised study. Bone Joint J 95-B:401–406
Yang LY, Wang XL, Zhou L, Fu Q (2013) A systematic review and meta-analysis of randomized controlled trials of unilateral versus bilateral kyphoplasty for osteoporotic vertebral compression fractures. Pain Phys 16:277–290
Graham J, Ahn C, Hai N, Buch BD (2007) Effect of bone density on vertebral strength and stiffness after percutaneous vertebroplasty. Spine (Phila Pa 1976) 32:E505–E511
Fehlings MG (2009) The safety of percutaneous vertebroplasty and kyphoplasty. J Neurosurg Spine 11:605–606
Chen B, Li Y, Xie D, Yang X, Zheng Z (2011) Comparison of unipedicular and bipedicular kyphoplasty on the stiffness and biomechanical balance of compression fractured vertebrae. Eur Spine J 20:1272–1280
Lin J, Zhang L, Yang HL (2013) Unilateral versus bilateral balloon kyphoplasty for osteoporotic vertebral compression fractures. Pain physsician 16:447–453
Feng JZQ, Xiao SX, Xia P (2012) Clinical comparison of unilateral and bilateral percutaneous kyphoplasty for treating osteoporotic vertebral compression fracture. Chinese J Trad Med Traum Orthop 20:26–29
Doo TH, Shin DA, Kim HI, Shin DG, Kim HJ, Chung JH, Lee JO (2008) Clinical relevance of pain patterns in osteoporotic vertebral compression fractures. J Korean Med Sci 23:1005–1010
Ren HL, Jiang JM, Chen JT, Wang JX (2015) Risk factors of new symptomatic vertebral compression fractures in osteoporotic patients undergone percutaneous vertebroplasty. Eur Spine J 24:750–758
Chong T, Lieu J, Alamin T, Mitra R (2011) Pulmonary cement embolism after kyphoplasty. Pain Pract 11:570–573
Krueger A, Bliemel C, Zettl R, Ruchholtz S (2009) Management of pulmonary cement embolism after percutaneous vertebroplasty and kyphoplasty: a systematic review of the literature. Eur Spine J 18:1257–1265
Wang E, Yi H, Wang M, Huang C (2013) Treatment of osteoporotic vertebral compression fractures with percutaneous kyphoplasty: a report of 196 cases. Eur J Orthop Surg Tr 23:S71–S75
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest concerning this article.
Rights and permissions
About this article
Cite this article
Cheng, X., Long, HQ., Xu, JH. et al. Comparison of unilateral versus bilateral percutaneous kyphoplasty for the treatment of patients with osteoporosis vertebral compression fracture (OVCF): a systematic review and meta-analysis. Eur Spine J 25, 3439–3449 (2016). https://doi.org/10.1007/s00586-016-4395-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-016-4395-6