Abstract
This study analyses the radiological and clinical results according to the two techniques of unilateral and bilateral balloon kyphoplasty in osteoporotic vertebral compression fractures. Fifty-two patients with osteoporotic vertebral compression fractures occurring at the thoracolumbar junction were enrolled in this study. All patients were classified into two groups; group I was treated with a unilateral approach and group II with a bilateral approach. The Cobb angle was measured each time to evaluate the kyphotic angle during the pre- and post-operative periods and at last follow-up, and a 10-point visual analog scale for pain was recorded at the same time. We found that the bilateral approach had a greater advantage in the reduction of kyphosis and the loss of reduction was less than the unilateral approach for the treatment of osteoporotic vertebral compression fractures.
Résumé
Cette étude analyse les résultats cliniques et radiologiques de deux techniques de kyphoplastie après fracture vertébrale ostéoporotique avec tassement. 52 patients ont été inclus dans l’étude. Tous les patients ont été classés en deux groupes. Le groupe 1 traité par abord unilatéral et le groupe 2 par un abord bilatéral. L’angle de Cobb a permis d’évaluer l’angle de cyphose pré et post-opératoire et au dernier recul. De même, une analyse de la douleur en 10 points a été utilisée sur la même période. En conclusion, nous pouvons indiquer que la kyphoplastie bilatérale permet une meilleure réduction vertébrale et diminue le tassement secondaire que l’on observe dans les abords unilatéraux.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporotic vertebral compression fractures (VCFs) are not uncommon and thus many patients may suffer from acute pain due to the fracture and also its chronic symptoms and resultant osteoporotic spinal deformities. Osteoporotic VCFs reduce mobility, worsen the quality of life and even reduce life expectancy. The adverse effect on activities of daily living is almost as great as that seen with hip fractures [9]. The primary treatment of osteoporotic VCFs consists in conservative measures including bed rest, analgesics and early ambulation with a brace after symptomatic relief. As is well known, a few patients may still complain of severe pain not responding to these conservative treatments and even show progressive collapse of the vertebral body and kyphosis with or without neurological deficit. Even though more aggressive treatment may be needed in these cases, the majority of patients with osteoporotic VCFs are not ideal candidates for surgical treatment, especially under general anaesthesia. Over the past decades, vertebroplasty (VP) was adopted as an optimal treatment of osteoporotic VCFs, having the advantage of rapid pain relief and long-lasting effect, but it could not restore the decreased height of the vertebral body. With the introduction of a newly designed, minimally invasive technique, balloon kyphoplasty (BK), the collapsed vertebral body was restored by an inflatable bone tamp and then more viscous polymethylmethacrylate (PMMA) was safely put into the hollow cavity made by the inflatable bone tamp with low pressure. To our knowledge, there have been no reports comparing the two techniques of unilateral and bilateral approaches of balloon kyphoplasty to treating osteoporotic vertebral compression fractures.
Material and methods
Patients
Fifty-two patients with confirmed osteoporotic vertebral compression fractures occurring at the thoracolumbar junction (T11–L2) were enrolled in this study. All patients were randomly allocated into two groups; group I (n = 24) was treated with a unilateral approach and group II (n = 28) with a bilateral approach. Mean age was 66.8 years (57–80) in group I and 68.9 years (57–83) in group II . Only three patients were male (two in group I and one in group II). The results of bone densitometry in both groups were not statistically different (T-score: −3.55, –3.64). Balloon kyphoplasty was performed in both groups within 2 months after injury. Mean time from injury was 3.44 and 3.68 weeks. The Cobb angle to evaluate kyphosis and a 10-point visual analog scale for pain were measured pre- and post-operatively. The minimum follow-up period was 12 months and mean follow-up was 17.8 months (12–24) in group I and 16.6 months (13–27) in group II. There were no significant differences between the groups regarding demographic data, which are shown in Table 1.
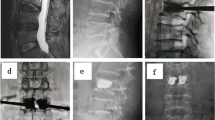
Technique
The indication for unilateral and bilateral balloon kyphoplasty was the same. The entire procedures of balloon kyphoplasty were performed under local anaesthesia. Patients were positioned prone on a radiolucent operating table. When using a unilateral approach, in contrast to a bilateral approach, the bone tamp was advanced more to the midline on the anteroposterior view. Also to prevent great vessel injury, the entry site of the bone tamp was selected at the same side of the great vessels. The remainder of the procedure was identical to the bilateral approach.
Statistical method
Pre-operative kyphotic angle, post-operative reduction and loss of reduction between both groups were evaluated with Student’s t-test. A value of p < 0.05 was considered statistically significant (MedCalc Software, version 8.1.1, Mariakerke, Belgium). Multiple regression analysis was also conducted to determine the relative importance of the possible independent factors (sex, age, treatment method, amount of PMMA) as predictors of kyphosis correction at the last follow-up.
Results
Demographic data and pre-operative index of vertebral fractures did not show any significant statistical differences. The pre-operative kyphotic angle was 17.6 ± 2.8° (13–25) in group I and 18.5 ± 3.5° (12–27) in group II (p = 0.369). The post-operative reduction rate was 41.3 ± 8.9% (22–63) and 67.8 ± 8.6% (52–83) (p < 0.001) and loss of reduction was 4.7 ± 2.9% (0–14) and 1.6 ± 1.1% (0–4.9) (p = 0.0001), respectively. The average amount of PMMA introduced was 3.44 ml (2.8–4.1) in group I and 6.43 ml in group II (p < 0.001). The results of the visual analog scale for pain were not statistically different from the pre-operative period through the immediate post-operative period to the final follow-up. In group I, the pain score on the visual analog scale was 8.1 prior to surgery, decreased to 2.1 in the immediate post-operative period and remained at 1.9 at the final follow-up. The respective scores for group II were 7.9, 1.7 and 1.8 at each measurement (p = 0.54, 0.14, 0.46). Stepwise multiple regression resulted in the following formula: LKC=−13.162 + 0.191A + 1.542S−0.7PMMA + 6.262 T, r 2 = 0.516, p < 0.001. LKC is the corrected kyphotic angle at last follow-up, A is the patient’s age, S is sex and T is treatment method. Age (p = 0.002) and treatment method (p = 0.025) were significant predictors, but sex (p = 0.302) and PMMA (p = 0.427) were not important predictors. There were two complications of PMMA leakage within the spinal canal only in group I, but they did not cause any neurological deficit.
Discussion
Osteoporosis is a very prevalent skeletal disorder, which is characterised by loss of bone density and increased risks of fractures. Osteoporosis is defined as diminished bone density measuring 2.5 standard deviations below the average bone density of healthy 25-year-old same sex members of the population. Following the criteria, 25% of post-menopausal women and 35% of women over 65 years of age in the US suffer from osteoporosis (1994) [1]. The incidence of osteoporotic spine fractures in the US is about 700,000 per year of which more than one third become chronically painful and 85% of these cases are due to primary osteoporosis [18]. Osteoporotic VCFs occurs most commonly at the thoracolumbar junction, especially L1 [12, 13]. The pain from acute osteoporotic vertebral compression fractures resolves over 6–8 weeks with conservative measures including medical and orthotic treatments. However, a few patients continue to complain of severe back pain especially on motion of the trunk and resultant kyphotic deformity. These patients who are unresponsive to nonoperative treatments may be candidates for surgical treatment. In the late 1980s, vertebroplasty was developed and Lapras first introduced this technique to treat fractured vertebral bodies [11]. Since then, this technique has been gaining so much in popularity and has been used for osteoporotic vertebral compression fractures. In 2001, the first clinical results of balloon kyphoplasty were reported by Lieberman et al. Balloon kyphoplasty has several advantages over vertebroplasty [14]. It offers immediate pain relief, stability and also restoration of local kyphosis by reducing the fractured vertebra with the inflatable bone tamp. In addition more viscous PMMA was introduced under low pressure into the cavity made by the inflatable bone tamp so that the rate of complications associated with this procedure such as thromboembolism and neurological deficit due to extravertebral PMMA leakage was low. For that reason, balloon kyphoplasty has been substituted for vertebroplasty. Nowadays the indication for balloon kyphoplasty has been expanded to include pathological fractures and even revision cases [7, 18]. Several authors reported the results of balloon kyphoplasty performed under general anaesthesia [5, 6, 12], but we performed both techniques under local anaesthesia in all cases. Many authors have reported the results using a bilateral approach [2, 8, 10]. Garfin et al. [8] described that two balloons are usually used to provide en masse reduction. Although Brugieres et al. [4] reported on a transcostovertebral technique known as the extrapedicular or parapedicular approach [17], it was applied only to thoracic vertebrae. There has been just one study reporting on the clinical result using unilateral kyphoplasty by Boszczyk et al. in the area of the mid and high thoracic spine. In this report [3], the reduction of the kyphotic angle was not sufficient. We found that it is difficult to obtain en masse reduction with a unilateral approach and consider that a unilateral approach achieves less vertebral fracture reduction with greater loss of reduction. However, it has been reported that the clinical results of balloon kyphoplasty were not always positively correlated with the restoration of height and amount of PMMA introduced [2]. That the incidence of complications in kyphoplasty was lower than in vertebroplasty has been well known, but PMMA leakage, pulmonary oedema, rib fractures and adjacent vertebral fractures have been reported in kyphoplasty [14–16]. In our study, two cases of PMMA leakage occurred in group I. We suspect that the effort of placing the bone tamp more centrally within the vertebral body violated the medial wall of the pedicle and PMMA was introduced into the spinal canal through this breakage. The limitations of our study are the small number of patients and fractures as well as the short follow-up period.
In conclusion, although the pain score for the two techniques was not so different, the bilateral approach of balloon kyphoplasty can achieve reduction of the kyphotic deformity due to an osteoporotic vertebral compression fracture to achieve good sagittal alignment.
References
World Health Organization (1994) Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. World Health Organ Tech Rep Ser 843:1–129
Berlemann U, Franz T, Orler R, Heini PF (2004) Kyphoplasty for treatment of osteoporotic vertebral fractures: a prospective non-randomized study. Eur Spine J 13:496–501
Boszczyk BM, Bierscneider M, Hauck S, Beisse R, Potulski M, Jaksche H (2005) Transcostovertebral kyphoplasty of the mid and high thoracic spine. Eur Spine J 14:992–999
Brugieres P, Gaston A, Heran F, Voisin MC, Marsault C (1990) Percutaneous biopsied of the thoracic spine under CT guidance: transcostaovertebral approach. J Comput Assist Tomogr 14:446–448
Coumans JV, Reinhardt MK, Lieberman IH (2003) Kyphoplasty for vertebral compression fractures: 1-year clinical outcomes from a prospective study. J Neurosurg Spine 99:44–50
Crandall D, Slaughter D, Hankins PJ, Moore C, Jerman J (2004) Acute versus chronic vertebral fractures treated with kyphoplasty: early results. Spine J 4:418–424
Gaitanis IN, Hadjipavlou AG, Katonis PG, Tzermiadianos MN, Pasku DS, Patwardhan AG (2005) Balloon kyphoplasty for the treatment of pathological vertebral compressive fractures. Eur Spine J 14:250–260
Garfin SR, Yuan HA, Reiley MA (2001) New technologies in spine: kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures. Spine 26:1511–1515
Greendale GA, Barrett-Connor E, Ingles S, Haile R (1995). Late physical and functional effects of osteoporotic fractures in women: the Rancho Bernado Study. J Am Geriatr Soc 43:955–961
Grohs JG, Matzner M, Trieb K, Krepler P (2005) Minimal invasive stabilization of osteoporotic vertebral fractures: a prospective nonrandomized comparison of vertebroplasty and balloon kyphoplasty. J Spinal Disord Tech 18:238–242
Lapras C, Mottolese C, Deruty R, Lapras C Jr, Remond J, Duquesnel J (1989) Percutaneous injection of methyl-methacrylate in osteoporosis and severe vertebral osteolysis (Galibert’s technic) (in French). Ann Chir 43:371–376
Ledlie JT, Renfro M (2003) Balloon kyphoplasty: one-year outcomes in vertebral body height restoration, chronic pain and activity levels. J Neurosurg Spine 98:36–42
Lee YL, Yip KM (1996) The osteoporotic spine. Clin Orthop Relat Res 323:91–97
Lieberman IH, Dudeney S, Reinhardt MK, Bell G (2001) Initial outcome and efficacy of “kyphoplasty” in the treatment of painful osteoporotic vertebral compression fractures. Spine 26:1631–1638
Phillips FM, Ho E, Campbell-Hupp M, McNally T, Todd Wetzel F, Gupta P (2003) Early radiographic and clinical results of balloon kyphoplasty for the treatment of osteoporotic vertebral compression fractures. Spine 28:2260–2267
Weisskopf M, Herlein S, Birnbaum K, Sibert C, Stanzel S, Wirtz DC (2003) Kyphoplasty-a new minimally invasive treatment for repositioning and stabilising vertebral bodies (in German). Z Orthop Ihre Grenzgeb 141:406–411
Wong W, Reiley M, Garfin S (2000) Vertebroplasty/kyphoplasty. J Womens Imaging 2:117–124
Yoon ST, Qureshi AA, Heller JG, Nordt JC 3rd (2005) Kyphoplasty for salvage of a failed vertebroplasty in osteoporotic vertebral compression fractures: case report and surgical technique. J Spinal Disord Tech 18(Suppl):S129–S134
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chung, H.J., Chung, K.J., Yoon, H.S. et al. Comparative study of balloon kyphoplasty with unilateral versus bilateral approach in osteoporotic vertebral compression fractures. International Orthopaedics (SICO 32, 817–820 (2008). https://doi.org/10.1007/s00264-007-0439-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-007-0439-1