Abstract
Purpose and methods
For the treatment of degenerative disc diseases of the cervical spine, anterior cervical discectomy and fusion (ACDF) still represents the standard procedure. However, long term clinical studies have shown a higher incidence of pathologies in the adjacent segments. As an alternative to spinal fusion, cervical total disc replacement (cTDR) or dynamically implants were increasingly used. This in vitro study analyzed the kinematics and intradiscal pressures in seven multi-segmental human cervical spine using hybrid multidirectional test method. The aim of our study was to compare the intact condition with a single-level dynamic stabilization with DCI®, with cTDR (activC®) and with simulated ACDF (CeSPACE® cage and CASPAR plate).
Results
No significant changes in the kinematics and pressures were observed in all segments after arthroplasty. The DCI® significantly decreased the motion of the treated segment in flexion/extension and lateral bending with some remaining residual mobility. Thereby the motion of the upper segment was increased significantly in flexion/extension. No significant changes of the intradiscal pressures were observed. With simulated fusion the motion of the indexed level was significantly decreased in flexion/extension and axial rotation with the greatest changes in the adjacent levels and the highest pressures.
Conclusion
Based on our biomechanical study the DCI® can pose an alternative to fusion, which has a lesser effect on adjacent levels. This might reduce the risk of long-term degeneration in those levels. In particular, the facet joint arthritis and kyphotic deformity, as a contraindication to the arthroplasty, could be a clinical application of the dynamic implant.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anterior cervical discectomy and fusion (ACDF) and cervical total disc replacement (cTDR) are two concurrent options in treatment of degenerative disc disease. Biomechanical studies have shown that arthrodesis of the cervical spine leads to an increase in the segmental range of motion (ROM) and the intradiscal pressure (IDP) in the levels proximal and distal to a simulated mono- or bisegmental fusion [1–3]. In contrast, when treated by arthroplasty, the kinematics in the target segment as well as in the neighboring segments reach near to physiologic state, indicating an almost physiologic restoration of the affected motion segments [1, 2, 4].
From a clinical point of view, patients with a history of cervical arthrodesis have a higher incidence of adjacent segment degeneration [5, 6]. Controlled clinical trials with a prospective and randomized study design have published the results after 4- to 5-year follow-up. They show at least comparable or even better findings after cTDR in contrast to ACDF with a lower reoperation rate after arthroplasty [7, 8].
Accepted contraindications for cTDR are osteoporotic bone and cervical instability [9]. Furthermore, segmental kyphosis and symptomatic facet joint arthrosis are reported as contraindications for arthroplasty, because first disc prosthesis are not able to restore a pathologic kyphotic sagittal profile and second the facet joints are expected to be overstressed mainly in extension due to preservation of normal ROM with cTDR [9].
Another treatment option, so called dynamical implants, has been proposed by several manufactures. The aim of these devices is to provide stability but at the same time reduce adjacent segment degeneration by providing some motion in the stabilized segment. One such device is the dynamic cervical implant (DCI®, Paradigm Spine, Germany), which is a single-piece design of titanium alloy. The DCI® was developed to bridge the gap between fusion and disc arthroplasty by addressing the potential downsides of fusion and by offering the advantages of motion preservation.
The aim of our experimental study was to analyze the kinematics and intradiscal pressures in a multi-segmental human cervical spine model after single-level dynamic stabilization with DCI® in comparison to the intact condition and after simulated ACDF and cTDR. We hypothesized that the stabilizing capabilities of the dynamical cervical implant put the DCI® between fusion and prosthesis regarding motion in the treated segment and adjacent level effect on motion and pressure.
Materials and methods
Specimen preparation
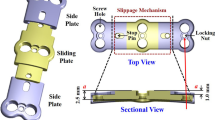
The study was conducted on seven, five female and two male, multi-segmental human cervical spine specimens [C4–C7; median age 59.5 years (27–73 years), median weight 54.4 kg (38.5–104.3 kg), median bone mineral density 0.62 g/cm2 (0.47–0.89 g/cm2)]. The specimens were radiologically screened before testing and an experienced surgeon (DD) evaluated the state of the disc to exclude specimens with degenerated intervertebral discs. All extraneous soft tissue was dissected, leaving the ligamentous structures including the intervertebral discs intact. The proximal (C4) and distal (C7) ends of the vertebrae were embedded in casting resin (Rencast FC52/53, gössl&pfaff, Germany). Optical markers for the tracking system (Polaris P4, NDI, Canada) were rigidly attached to the vertebral bodies (Fig. 1). To apply a compressive preload the follower load technique was used, with loading frames attached to C4, C5 and C6 [10]. The follower load was applied bilaterally at C4 by two steel cables, which passed freely through guides of the lower two loading frames. The path of the follower load was adjusted to the contour of the spinal column and to the rotation center of each motion segment in the sagittal plane. Pressure sensors (Type FMSPEZ10, MIPM GmbH, Germany) were placed in the nucleus pulposus of C4/5 and C6/7 under fluoroscopic control to measure intradiscal pressure.
Test setup
The specimens were loaded with the hybrid multidirectional test method [11]. Hereby, the specimens subjected to a constant follower load of 120 N were loaded in the intact state with pure moment loadings sequentially in flexion and extension (x-axis), lateral bending (z-axis), and axial rotation (y-axis). The resulting total range of motion (tROM), total neutral zone (tNZ) in all motion segments, as well as the IDP in C4/5 and C6/7 were measured. The testing device consisted of a sensor-guided robotic system (robot system: KR15/1, KUKA, Germany; sensor: KMS 60, IpeA GmbH, Germany, Fig. 1) and a servo-hydraulic system with force controlled actuators (Type 8417-6005, Burster, Germany) [12]. The robot is used as a manipulator and capable of applying unconstrained rotational moments about three axes according to the standard flexibility test protocol [13]. The rotational velocity of the robot was 0.2 deg/s for all tested directions. The cranial vertebra C4 was fixed to the sensor of the robotic system and the caudal vertebra was mounted on a rigid base. The kinematic and kinetic of the whole specimen were recorded by the robotic system. The intersegmental range of motion (iROM) and intersegmental neutral zone (iNZ) were measured by the optical tracking system. Local coordinate systems were defined with a digitizing probe for each vertebra according to the recommendation of Crawford et al. [14]. The kinematic data were collected together with the values for the low-pass filtered IDP using a custom-made program (LabView 2010, NI, USA). As the range of the pressure sensor is limited (measuring range up to 1 MPa), an offset was performed in situ in neutral position under follower load. Thus reported pressure values represent change in intradiscal pressure.
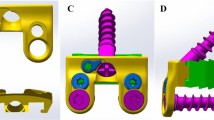
Reconstructive conditions and test protocol
The specimens were first tested in an intact state with ±2.0 Nm of pure moment loading about the respective testing axis. After (1) a complete discectomy at C5/6, the specimen was subsequently tested with (2) dynamical cervical implant DI (DCI®, Paradigm Spine, Germany), (3) arthroplasty cTDR (activC® artificial disc, Aesculap AG, Germany) and (4) fusion ACDF (cervical cage CeSPACE® and an anterior CASPAR plate stabilization, both Aesculap AG, Germany). Thereby the posterior longitudinal ligament was kept intact to preserve the stability. All surgeries were performed by an experienced spine surgeon (DD) and according to manufacturer’s instructions. The three treated conditions had ap and lateral radiographs to check their correct position in the intervertebral space (Fig. 2). In the treated states, the specimens were tested until the tROM of the treated spinal construct was equal to the total range of motion of the intact state. Thus the applied moments were different depending on the treatment. The percentage changes of the iROM were calculated using the hybrid test method to evaluate the effects on the adjacent and indexed levels when comparing the treated to the intact state (\({\text{iROM}}_{\text{change}} = \left( {{\text{iROM}}_{\text{treated}} - {\text{iROM}}_{\text{intact}} } \right)/{\text{iROM}}_{\text{intact}}\)) [11].
Data and statistical analysis
According to the recommended standard protocol three test cycles were carried out for each condition and the third cycle was used for the analysis [13]. The Wilcoxon matched-pairs signed rank test was performed using SPSS (SPSS Statistics 20, IBM, USA) to determine the significant changes of the three treated conditions (cTDR, dynamic cervical implant, fusion) to the intact state. A significance level of alpha = 0.05 was applied. Due to the limited sample size no Bonferroni correction was used.
Results
All the seven tested specimens could be fully tested in all conditions.
Flexion/extension
Mean tROM in all tested conditions was 38.7 ± 9.4° (Fig. 3), whereby the largest contribution of movement was observed in the most cranial segment C4/5.
The implantation of the DI leads to a significant 25 % increase of required moment (p = 0.016) to achieve intact tROM in flexion, while iROM of C4/5 was significantly increased (p = 0.016) and of C5/6 was significantly decreased (p = 0.016). The tNZ and iNZ of the indexed level C5/6 were not significantly affected and IDP increased only slightly. With implantation of the cTDR, no significant changes in iROM, tNZ, iNZ, required moment and IDP occur. The application of the ACDF resulted in a significant 66 % increase in required moment (p = 0.016) and a significant increase of iROM in C4/5 (p = 0.016) and C6/7 (p = 0.031) and a decrease in C5/6 (p = 0.016). IDP in C6/7 also increases significantly (p = 0.047) (Tables 1, 2, 3).
Lateral bending
Mean tROM in all tested conditions was 12.5 ± 6.7° (Fig. 3).
The implantation of the DI leads to a significant 20 % increase of required moment (p = 0.031) to achieve intact ROM on the right side, while iROM of C5/6 is significantly decreased (p = 0.031). The tNZ and iNZ are not significantly affected and IDP increases slightly. With implantation of the cTDR, no significant changes in iROM, tNZ, iNZ, required moment and IDP occur. The application of the ACDF resulted in no significant changes in iROM, tNZ, iNZ, required moment and IDP (Tables 1, 2, 3).
Axial rotation
Mean tROM in all tested conditions was 12.2 ± 6.2° (Fig. 3).
With implantation of the DI or cTDR prosthesis, no significant changes in iROM, tNZ, iNZ, required moment and IDP occur. The application of the ACDF resulted in a significant decrease of iROM in C5/6 (p = 0.047) and a significant increase in C6/7 (p = 0.016). The tNZ, iNZ, required moment and IDP did not change significantly (Tables 1, 2, 3).
Discussion
The aim of the presented in vitro study was to determine and to compare the effects of different stabilization treatments on the biomechanics of the affected and adjacent spinal motion segments. The tests were conducted on human multi-segmental specimens using the hybrid test method [11] to analyze the biomechanical behavior of a cTDR, dynamical cervical implant and spinal fusion on the adjacent motion segments. As it is a motion preserving technology, we found that the artificial disc (cTDR) had no significant effect on the kinematics and intradiscal pressures in all motion directions tested. The dynamical implant (DI) stabilized the treated segment in flexion/extension and lateral bending. The iROM in treated segment C5/6 was significantly reduced by the DI while allowing residual mobility. The spinal fusion (ACDF) showed the greatest effects on the tested kinematics and intradiscal pressures in the upper and lower adjacent levels.
Anterior cervical discectomy and fusion is currently the standard procedure for the treatment of most degenerative disc disease in the cervical spine. However, clinical long-term studies have shown evidence of an increased incidence of pathologies in the motion segments adjacent the fused segment [5, 6]. Our testing protocol showed that the reduced iROM in the ACDF treated C5/6 was compensated by increased motion in the adjacent levels. In our study, the cranial segment (C4/5) compensated motion in flexion/extension and lateral bending slightly more than the caudal segment C6/7. Due to the postoperative state in the in vitro setup some residual motion is still remaining in the treated segment. This is a common limitation of in vitro studies in which the stabilizing bony ingrowth could not be simulated. Next to the greatest changes in the kinematics of the adjacent levels, the highest values for the intradiscal pressures were observed after spinal fusion for all treated conditions except for IDP in C6/7 in lateral bending and axial rotation. The stiffness of the whole specimens increased after ACDF in all three tested directions, as reflected by the increase in the applied moment required to reach the tROM of the intact state (up to 66 % in flexion). This is due to the fact that motion segment stiffness increases non-linearly with increasing flexion angle. As the adjacent segments are forced to compensate for the motion lost in the treated segment, the required moment to reach physiologic tROM is increased. Nonetheless, although iROM of the adjacent levels increases, it is still within physiological range reported in the literature [15].
The arthroplasty had the smallest effect on the intersegmental range of motion of the treated segment in all tested directions. In lateral bending the iROM even decreased, which is in accordance to a similar study by Patwardhan et al. [16]. Although investigating a slightly different prosthesis design, they found a significant increase of adjacent level iROM in flexion–extension and axial rotation. We observed no hypermobility in any direction, which is in contrast to a study by Chang et al., who found an increased iROM in two different prosthesis designs (ProDisc-C and Prestige) [17]. This hypermobility may partly be caused by the loss of the anterior longitudinal ligament due to the surgical approach. In our case, this may be partly stabilized by the follower load. On the other hand, McAfee et al. found no significant differences in iROM of a motion preserving implant with intact or resected posterior longitudinal ligament [18]. In a clinical study, the same cervical disc prosthesis as used in our study did show a decrease in flexion/extension from 9.8° post-op to 6.4° after 2 years [19].
The DI implant had the most homogenous effects of all treatments in all directions. The affected segment was stabilized as indicated by a significant decrease of iROM in flexion–extension and lateral bending. The moments required to reach intact tROM in flexion and lateral bending were between moments for the prosthesis and fusion. The IDP of the C4/5 segment, however, was the lowest of all treated conditions. It might be due to a load transfer to the facet joints with an anterior shift of the center of rotation, as shown computer simulation by Mo et al. [20]. Their study also revealed a constant IDP in C4/5 during different conditions. Clinically, Wang et al. found a slight increase in flexion–extension iROM of the DI from 12.2° post-op to 13.6° at 2 years follow-up [21]. Additionally, Matgé et al. found a satisfying motion preservation at 2 years follow-up with only −5.5 % change of iROM in the indexed level [22].
The intersegmental neutral zone, as a parameter for instability, showed a stabilizing effect for the DI and ACDF in the treated segment. Due to the immediate post-operative condition the authors expect the stabilizing effect of the ACDF to further increase in the clinical situation a few weeks post-operative because of the bony ingrowth. The cTDR does not show a stabilizing effect in the iNZ.
There are several limitations to this study that must be acknowledged. As common with biomechanical in vitro test, only the immediate post-operative condition is represented. Thus, the bony ingrowth of implants is not considered. Especially in the case of the DI in axial rotation a relative motion between implant and bone cannot be ruled out. In the case of fusion, the uncommon configuration of plate and cage had to be chosen to assure additional stiffness in all directions. The hybrid test method used is one of many published methods for in vitro multi-segment spine testing. Other accepted standards are the flexibility test method [23], the pure moment method or the multi-directional test method of Panjabi [11]. We used the hybrid method to investigate the effect on the indexed and adjacent levels, but this is discussed controversially [24, 25]. The authors decided to use the hybrid method as the most suited protocol to determine the adjacent level effects. As the bending stiffness of the multisegmental specimen is nonlinearly distributed along the cranio-caudal axis it is not predictable how the motion change of the affected level will be compensated by the upper and lower level. The utilized follower load used in all directions represents a static model of compressive axial forces, but the line of action of the follower load needs to be precisely adjusted as we have done to avoid additional bending moment artefacts that would confound the results [26]. Furthermore the applied loading rate of 0.2 deg/s was below recommended threshold of 0.5 deg/s to keep shear forces from robot control to a minimum [13].
In summary, our study is the first biomechanical in vitro study on the dynamical stabilization implant DI. In clinical cases where a cTDR is contraindicated because of kyphotic deformities or facet joint arthritis, the novel dynamical cervical implant can pose an alternative to fusion, which has a lesser effect on adjacent levels. This might reduce the risk of long-term degeneration in those levels. First clinical studies have been promising, but long-term observations need to confirm these findings [22, 27, 28].
References
Chang U-K, Kim DH, Lee MC et al (2007) Changes in adjacent-level disc pressure and facet joint force after cervical arthroplasty compared with cervical discectomy and fusion. J Neurosurg Spine 7:33–39. doi:10.3171/SPI-07/07/033
DiAngelo DJ, Foley KT, Morrow BR et al (2004) In vitro biomechanics of cervical disc arthroplasty with the ProDisc-C total disc implant. Neurosurg Focus 17:E7
Ragab AA, Escarcega AJ, Zdeblick TA (2006) A quantitative analysis of strain at adjacent segments after segmental immobilization of the cervical spine. J Spinal Disord Tech 19:407–410
Galbusera F, Bellini CM, Raimondi MT et al (2008) Cervical spine biomechanics following implantation of a disc prosthesis. Med Eng Phys 30:1127–1133. doi:10.1016/j.medengphy.2008.02.002
Goffin J, Geusens E, Vantomme N et al (2004) Long-term follow-up after interbody fusion of the cervical spine. J Spinal Disord Tech 17:79–85
Hilibrand AS, Carlson GD, Palumbo MA et al (1999) Radiculopathy and myelopathy at segments adjacent to site of a previous anterior cervical arthrodesis. J Bone Jt Surg Br 81-A:519–528
Delamarter RB, Zigler J (2013) Five-year reoperation rates, cervical total disc replacement versus fusion, results of a prospective randomized clinical trial. Spine 38:711–717. doi:10.1097/BRS.0b013e3182797592 (Phila Pa 1976)
Blumenthal SL, Ohnmeiss DD, Guyer RD, Zigler JE (2013) Reoperations in cervical total disc replacement compared with anterior cervical fusion: results compiled from multiple prospective food and drug administration investigational device exemption trials conducted at a single site. Spine 38:1177–1182. doi:10.1097/BRS.0b013e31828ce774 (Phila Pa 1976)
Auerbach JD, Jones KJ, Fras CI et al (2008) The prevalence of indications and contraindications to cervical total disc replacement. Spine J 8:711–716. doi:10.1016/j.spinee.2007.06.018
Patwardhan AG, Havey RM, Ghanayem AJ et al (2000) Load-carrying capacity of the human cervical spine in compression is increased under a follower load. Spine 25:1548–1554 (Phila Pa 1976)
Panjabi MM (2007) Hybrid multidirectional test method to evaluate spinal adjacent-level effects. Clin Biomech 22:257–265. doi:10.1016/j.clinbiomech.2006.08.006
Hurschler C, Pott LS, Gossé F, Wirth C (2005) Sensor-guided robot. Spine motion-segment. Biomech. Test. Valid. against pure moment Appar. In: Transactions of the 51st annual meeting of the Orthopedic Research Society
Wilke H, Wenger K, Claes L (1998) Testing criteria for spinal implants: recommendations for the standardization of in vitro stability testing of spinal implants. Eur Spine J 7:148–154
Crawford N, Dickman C (1997) Construction of local vertebral coordinate systems using a digitizing probe: technical note. Spine 22:559–563 (Phila Pa 1976)
White AA III, Panjabi M (1990) Clinical biomechanics of the spine, 2nd edn. J.B. Lippincott Comp, Philadelphia
Patwardhan AG, Tzermiadianos MN, Tsitsopoulos PP et al (2012) Primary and coupled motions after cervical total disc replacement using a compressible six-degree-of-freedom prosthesis. Eur Spine J 21:618–629. doi:10.1007/s00586-010-1575-7
Chang U-K, Kim DH, Lee MC et al (2007) Range of motion change after cervical arthroplasty with ProDisc-C and prestige artificial discs compared with anterior cervical discectomy and fusion. J Neurosurg Spine 7:40–46. doi:10.3171/SPI-07/07/040
McAfee PC, Cunningham B, Dmitriev A et al (2003) Cervical disc replacement-porous coated motion prosthesis: a comparative biomechanical analysis showing the key role of the posterior longitudinal ligament. Spine 28:S176–S185. doi:10.1097/01.BRS.0000092219.28382.0C (Phila Pa 1976)
Suchomel P, Jurák L, Antinheimo J et al (2014) Does sagittal position of the CTDR-related centre of rotation influence functional outcome? Prospective 2-year follow-up analysis. Eur Spine J 23:1124–1134. doi:10.1007/s00586-014-3223-0
Mo ZJ, Bin Zhao Y, Wang LZ et al (2014) Biomechanical effects of cervical arthroplasty with U-shaped disc implant on segmental range of motion and loading of surrounding soft tissue. Eur Spine J 23:613–621. doi:10.1007/s00586-013-3070-4
Wang L, Song YM, Liu LM et al (2014) Clinical and radiographic outcomes of dynamic cervical implant replacement for treatment of single-level degenerative cervical disc disease: a 24-month follow-up. Eur Spine J 23:1680–1687. doi:10.1007/s00586-014-3180-7
Matgé G, Berthold C, Gunness VRN et al (2015) Stabilization with the dynamic cervical implant: a novel treatment approach following cervical discectomy and decompression. J Neurosurg Spine 22:237–245. doi:10.3171/2014.10.SPINE131089
Panjabi MM (1988) Biomechanical evaluation of spinal fixation devices: I. A conceptual framework. Spine 13:1129–1134 (Phila Pa 1976)
Crawford NR (2007) Does the “hybrid multidirectional test method” generate quality data or paradoxical data? Clin Biomech (Bristol, Avon) 22:861–2; author reply 863–4. doi: 10.1016/j.clinbiomech.2007.04.005
Panjabi M (2007) Reply. Clin Biomech 22:863–864. doi:10.1016/j.clinbiomech.2007.04.001
Dreischarf M, Zander T, Bergmann G, Rohlmann A (2010) A non-optimized follower load path may cause considerable intervertebral rotations. J Biomech 43:2625–2628. doi:10.1016/j.jbiomech.2010.05.033
Herdmann J, Buddenberg P, Pilz A et al (2011) Life quality after cervical reconstruction with dynamic cervical implant. Eur Spine J, Springer, p 2026
Li Z, Yu S, Zhao Y et al (2014) Clinical and radiologic comparison of dynamic cervical implant arthroplasty versus anterior cervical discectomy and fusion for the treatment of cervical degenerative disc disease. J Clin Neurosci 21:942–948. doi:10.1016/j.jocn.2013.09.007
Acknowledgments
This study was funded by the Paradigm Spine GmbH and in parts by grants of the HiLF program of the Hannover Medical School. Aesculap AG provided the implants for the cTDR and ACDF.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The corresponding author BW received honoraria for lectures during two workshops of the Paradigm Spine GmbH.
Rights and permissions
About this article
Cite this article
Welke, B., Schwarze, M., Hurschler, C. et al. In vitro investigation of a new dynamic cervical implant: comparison to spinal fusion and total disc replacement. Eur Spine J 25, 2247–2254 (2016). https://doi.org/10.1007/s00586-015-4361-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-015-4361-8