Abstract
Purpose
We aimed to analyze the clinical efficacy of the zero-profile anchored spacers in the treatment of one-level or two-level cervical degenerative disc disease.
Methods
From April 2011 to April 2013, a total of 63 consecutive patients with cervical degenerative disc disease who underwent one- or two-level ACDF using either the zero-profile anchored spacer or the stand-alone cages and a titanium plate fixation were reviewed for the radiological and clinical outcomes and complications. The zero-profile anchored spacers were used in 30 patients (anchored group) and stand-alone cages with an anterior cervical plate were implanted in 33 cases (non-anchored group). Operative time, intraoperative blood loss, clinical and radiological results were compared between the anchored group and the non-anchored group.
Results
All patients were followed up for at least 12 months. There were not bolt loosening or rupture of anchoring clips, screws or titanium plates observed in two groups during follow-up period. There were no significant difference in neck disability index scores, Japanese Orthopedic Association scores, fusion rate, and cervical lordosis during follow-up between two groups (P > 0.05), but significant difference in the operation time, blood loss and the presence of dysphagia were found (P < 0.05). There were no adjacent disc degeneration and instability observed in two groups.
Conclusions
The zero-profile anchored spacer achieved similar clinical outcomes compared to ACDF with anterior plating for the treatment of the cervical degenerative disc disease. However, zero-profile anchored spacer was associated with a lower risk of postoperative dysphagia, shorter operation time, less blood loss, and relatively greater simplicity than the stand-alone cage with a titanium plate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since the anterior cervical discectomy and fusion (ACDF) was first described by Smith and Robinson [1], ACDF has yielded good results for the treatment of cervical degenerative disc disease and is accepted as the standard operative procedure. Meanwhile, the requirement to increase the immediate postoperative stability after bone grafting between vertebral bodies led to the development of the anterior plating system. Titanium plate fixation may decrease the micro-movement of the cervical spine, enhance the fusion rate, and correct the spinal curve to physiological lordosis [2]. However, plate implantation in the anterior cervical spine poses a substantial risk of hardware-related complications such as screws or plate dislodgement, soft-tissue injury, esophagus perforation, spinal cord or nerve injury and dysphagia [3–7]. To avoid irritation of the esophagus, in recent years, a zero-profile anchored spacer (ROI-C, LDR, Troyes, France) of the cervical spine has attracted attention as a possible treatment for cervical degenerative disc disease. The zero-profile anchored spacer is a radiolucent cervical integrated intervertebral fusion device constructed of polyether-ether-ketone (PEEK) cage with two integrated self-locking clips designed to provide lag compression between the adjacent vertebral bodies and confer anterior column fixation, bridging the index levels. This design avoids the need for any additional internal fixation devices and theoretically circumvents the aforementioned morbidities associated with anterior plating while providing the segmental rigidity necessary for cervical spinal fusion. Thus, we perform this retrospective study to compare the clinical results of the zero-profile anchored spacer and the stand-alone cages with a titanium plate for treating single-level or two-level cervical degenerative disc disease.
Materials and methods
Patient demographics
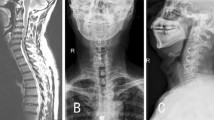
A total of 63 consecutive patients with cervical degenerative disc disease who underwent ACDF using either the zero-profile anchored spacer or the stand-alone cages and a titanium plate fixation between April 2011 and April 2013 were enrolled in this retrospective study. They were divided into two groups based on surgical procedure. 30 patients who underwent fusion using zero-profile anchored spacer (ROI-C, LDR, Troyes, France) implants were classified as anchored group (Fig. 1), and 33 patients underwent fusion using stand-alone cages and an anterior plate (Medtronic, Minneapolis, American) served as the non-anchored group (Fig. 2). The average age was 56.8 ± 11.0 years (range 37–77 years) in the anchored group and 54.0 ± 10.0 years (range 34–72 years) in the non-anchored group. The inclusion criteria were: (1) myelopathy or radiculopathy on the physical examination; (2) spinal cord or root compression visible on recent magnetic resonance imaging (MRI) at one disc level or two disc levels; and (3) no response to at least 6 weeks of conservative treatment. Exclusion criteria were: (1) significant segmental instability and developmental stenosis; (2) a history of cervical spine surgery and other cervical diseases, including ossification of the posterior longitudinal ligament, fracture, tumor, infection, or severe osteoporosis; and (3) a requirement for simultaneous anterior and posterior surgery. The patients’ preoperative data and number of treated segments are shown in Table 1. There were no statistically significant differences for patient age, sex, number of treated segments, follow-up time, or hospital stay between the anchored group and the non-anchored group (P > 0.05, Table 1). This study was approved by the Institutional Ethics Committee of Soochow University.
Surgical procedure
Operations were performed by the same surgeon from our team. After successful general anesthesia, the basic techniques for exposure, discectomy and decompression were performed using a right-sided skin incision and a standard Smith–Robinson approach [1]. Then, using a surgical microscope and a microdrill, the intervertebral disc and herniated nucleus pulposus were extirpated. Extensive decompression was performed, including removal of the osteophytes. The posterior longitudinal ligament was opened transversely and dorsal osteophytes possibly compressing the nerve root were removed with rongeurs or a drill. The dura mater and nerve root origins were exposed and decompressed. The endplates were abraded before fusion and the bony endplate was preserved as much as possible to prevent cage subsidence.
The anchored group: the appropriate size of the anchored intervertebral fusion cage was determined by both preoperative templating and intraoperative evaluation using a trial cage to confirm initial stability. 0.25 mg of recombinant human bone morphogenetic protein (rhBMP-2, pharmaceutical group investment limited corporation, Hangzhou, China) was exclusively placed in the center of a PEEK cage and the two ends of the cage were packed with excised local osteophytes for containing the rhBMP-2. Then the cage was inserted into the disc space using an impactor. After implantation of the cage, two cervical anchoring clips were placed into the lower and upper vertebra through the anterior part of the cage to ensure primary stabilization by self-locking function of anchoring clips. The non-anchored group: the appropriate size for stand-alone cage was determined by both preoperative templating and intraoperative evaluation using a trial cage to confirm optimal implant size. A PEEK cage was packed with 0.25 mg of rhBMP-2 and excised local osteophytes and inserted into the disc space as described above. After removal of the Caspar distracter, the self-tapping screws were used cranially and caudally to fix the anterior cervical plating.
After surgery, patients were allowed to sit up on the first postoperative day and walk on the second postoperative day with a soft cervical collar, which was removed the same day after these radiographs were deemed satisfactory. Patients were discharged home on the fourth or tenth postoperative day. The patient demographics and operative details for the two groups were recorded. All data were collected and reviewed by an independent observer.
Outcome assessment
All outpatients visit at postoperative 2 weeks, 1 month, 3 months, 6 months, and every 6 months thereafter. Follow-up clinical examinations were obtained by a physician unrelated to the surgical procedures. Operative time and intraoperative blood loss were compared between the anchored group and the non-anchored group. At before surgery and each follow-up, the patients were asked to complete the neck disability index (NDI) scores questionnaire [10] and Japanese Orthopedic Association (JOA) scores questionnaire [11]. The JOA recovery rate, which indicates the degree of normalization postoperatively, was calculated using Hirabayashi’s [12] formula: (postoperative score − preoperative score) × 100/[17 (full score) − preoperative score]. The incidence of dysphagia was recorded using the system defined by Bazaz [8, 9]. Severity of dysphagia was graded as none, mild, moderate, or severe (Table 2). The presence of dysphagia was evaluated at 2 weeks postoperatively and at 3 months postoperatively. The cervical spine static and dynamic X-ray were obtained at each follow-up. Cervical lordosis was defined as the angle between the lower endplate of C2 and the upper endplate of C7 using Cobb’s method. The fusion rate was assessed on cervical spine static and dynamic X-ray Fusion was considered according to the following accepted criteria [13]: (1) absence of motion between the spinous processes at dynamic lateral radiographs, (2) absence of a radiolucent gap between the graft and endplates, (3) presence of continuous bridging bony trabeculae at the graft-endplate interface. When the radiographic fusion is controversial, two-dimensional computed tomography (CT) scan reconstructions were performed and considered as a more accurate means to assess for radiographic fusion. New anterior osteophyte formation or enlargement, increased narrowing of the interspace, new disc degeneration disease, or calcification of the anterior longitudinal ligament were radiological findings indicating adjacent segment degeneration.
Statistical analysis
Continuous variables are shown as mean ± standard deviation. Differences between the two treatment groups were assessed utilizing the Student t test. An independent-samples t test was used for the unpaired data. The paired data were compared with a paired sample t test. Categorical variables of interest are depicted as total numbers and percentages (in parentheses). Differences of categorical variables were assessed using the Chi square test. The two-tailed test results were considered significant when P was less than 0.05. All the analyses were performed using the Statistical Package for the Social Sciences (version 16.0 SPSS, Chicago, IL, USA).
Results
All patients were followed up for at least 12 months with the mean follow-up period of 24.0 ± 7.9 (range 12–36) months. All devices were implanted successfully, and there were no hematoma, deep infection, bolt loosening or rupture of anchoring clips, screws or titanium plates observed in two groups during follow-up period. The zero-profile anchored spacers were implanted in 31 patients (46 segments). The non-anchored group consisted of 43 patients (48 segments) treated with stand-alone cages and a titanium plate. Surgical procedures covered the whole extent of the subaxial cervical spine from C3 to C7. Patient characteristics were very similar among the two treatment groups (Fig. 3). Anchored group had a mean intraoperative blood loss of 56.8 ± 19.0 ml in single-level and 78.8 ± 22.5 ml in two-level while the average operative time was 80.4 ± 12.1 min in single-level and 124.3 ± 19.3 min in two-level. Non-anchored group had a mean intraoperative blood loss of 89.4 ± 29.7 ml in single-level and 102.3 ± 36.6 ml in two-level while the average operative time was 108.7 ± 22.8 min in single-level and 143.3 ± 22.4 min in two-level. The differences between the operative time and intraoperative blood loss for the anchored group and non-anchored group were statistically significant (P < 0.05, Table 3). There were no statistically significant differences for postoperative JOA scores, NDI scores and cervical lordosis between the anchored group and the non-anchored group (P > 0.05). None of patient complained about dysphagia before operation. The postoperative JOA scores and NDI scores in both groups differed significantly from their respective preoperative JOA scores and NDI scores (P < 0.001, Table 4). The JOA recovery rate was 61.3 ± 11.4 % in the anchored group and 59.7 ± 15.6 % in the non-anchored group. There were no significant differences in the JOA recovery rate between two groups. Six (20.0 %) patients complained about mild dysphagia at postoperative 2 weeks in the anchored group; the dysphasia disappeared at postoperative 3 months. There were 14 (42.4 %) patients who complained of dysphagia in the non-anchored group. Eight patients complained about mild dysphagia and six patients complained of moderate dysphagia at postoperative 2 weeks. After conservative treatment, five patients had recovered at postoperative 3 months, but nine patients had no apparent relief at the last follow-up. There were no significant difference in the presence of dysphagia between the two groups at postoperative 2 weeks, but significant difference in incidence of dysphagia at postoperative 3 months was found (P < 0.001, Table 5). The postoperative cervical lordosis in both groups differed significantly from their respective preoperative cervical lordosis (P < 0.001, Table 4). But no significant difference was found between the two groups at each time point (P > 0.05). Solid fusion was achieved in all patients of two groups at 3–6 months postoperatively (Fig. 4). There were no adjacent disc degeneration and instability observed in two groups.
Discussion
Anterior cervical discectomy and fusion has been demonstrated to be effective in the treatment of cervical disc degenerative disorders in many reports. The surgical outcome depends on decompression of spinal cord and nerve roots, stabilization of fused segments and avoidance of complications [14]. The requirement to increase the immediate postoperative stability after bone grafting between vertebral bodies led to the development of an anterior plating system. However, there are increased risks of hardware failure [15]. The presence of a plate itself in the anterior cervical spine and its contact with the esophagus is considered to be a possible cause of postoperative dysphagia. The application of anterior plating is a time-consuming procedure that can compromise vital structures on the anterior aspect of the cervical spine such as the trachea, carotid arteries, and esophagus [16]. In our study, the zero-profile anchored spacer was found to be superior to the titanium plate group in terms of operation times and bleeding amounts.
Anterior plating is associated with higher rates of postoperative dysphagia. The reported rate of postoperative transient dysphagia following ACDF ranges from 2 to 67 % [8, 17, 18]. In the majority of cases dysphagia resolves within the first 3 months, however, in 12.5–35.1 % of patients dysphagia persists for more than 3 months [8]. The similar results were observed in titanium plate group in our study. We did not find significant difference in the incidence of dysphagia 2 weeks after surgery, but the significant difference was found at 3 months follow-up. Furthermore, Lee et al. [19] has demonstrated that design and thickness of anterior locking plates correlate with postoperative dysphagia. Although the exact pathophysiologic mechanism of dysphagia remains unknown, it is considered to be a possible cause of postoperative dysphagia that the anterior cervical locking plate is placed directly posterior to the esophagus and may impinge or irritate the esophagus [8, 19, 20]. The zero-profile anchored spacer is not placed across the anterior vertebral body, and can be completely contained in the decompressed intervertebral space, avoiding the mechanical stimulus to the esophagus and other pre-vertebral soft tissues, preserving as many normal anatomical tissues as possible which resulting in the lower postoperative dysphagia incidence in the anchored group. Although the safety profile of rhBMP-2 in the anterior lumbar spine has been well documented, that for off-label usage in the anterior cervical spine has not been fully determined. There have been serious complications reported with off-label use of rhBMP-2 including dysphagia. However, we have not observed that with use of rhBMP-2 in all patients in our study. It is possible that the discrepancy in swelling complications between this study and other published studies could be due to differences in dosage or placement of rhBMP-2. Two facts should be noted. First, the rhBMP-2 is used off-label in the anterior cervical spine, the conditions for its usage are borrowed from those appropriate to the lumbar spine in previously reported. We use much smaller doses of rhBMP-2 in our cervical spine patients. We have used a dose of 0.25 mg of rhBMP-2 in our study. Second, the rhBMP-2 is prevented from leaking into surrounding tissue with use of a PEEK cage and the local decompression osteophytes. Another potential reason for the discrepancy may be differences in sample size, as the current series is smaller than the other published series. A proper dose and containment of rhBMP-2 are capable of providing the benefits with respect to achieving fusion while avoiding relative complications [21].
An integral part of the zero-profile anchored spacer is a cage and two anchoring clips, eliminating the basic disadvantage of stand-alone cages. The zero-profile anchored spacer combines interbody support and supplemental fixation into a single device. These unique structures offer a fixation mechanism that is similar to the function of a plate and screws. Scholz et al. [20] found that the anchored spacer provided a similar biomechanical stability to that of the established anterior fusion technique using an anterior plate and cage. In our study, we also found an excellent fusion rate with good stability. The self-locking devices ensure excellent primary stability of the implant and promote early fusion. Furthermore, the elastic modulus of the anchored cage is similar to that of bone, which theoretically helps to decrease stress shielding and increase bony fusion. The anatomical shape of the anchored cage (with its upper convex part in the frontal and sagittal planes) allows a wide grafting space and close contact between the endplate bone and the implant. Besides, this satisfactory fusion rate may be related to surgical techniques that include optimal preparation of the fusion bed and proper disc space distraction.
The exact pathophysiologic mechanism of adjacent segment degeneration remains unknown. Anterior interbody fusion can easily cause adjacent segment degeneration [22]. The presence of a plate is also likely to accelerate degenerative changes in adjacent segments [23]. A number of authors have suggested that ACDF may alter the natural history of cervical spondylosis and hasten the development of degenerative changes at levels immediately above and below fused regions [24]. Schwab et al. [25] found that cervical fusion reduced the number of vertebrae with active function and caused biomechanical changes. To maintain the scope of activities of the whole cervical spine, the body increases the activity of the adjacent fused vertebral segments to compensate, causing adjacent segment degeneration. During the follow-up period, no pseudarthrosis, internal fixation loosening, detachment, fractures, adjacent segment degeneration, and instability occurred postoperatively in our study. However, there are some limitations in our study. First, the design of the study is a retrospective cohort study and we were not able to perform a randomized control trial study. In addition, only 63 consecutive patients were included in current study. The patient’s number is small. Thus, a long-term study, with a larger number of patients, should be performed to further investigate the efficacy of the zero-profile anchored spacer spacers for the treatment of cervical degenerative disc diseases.
In conclusion, the results of this study do not show significant differences between the zero-profile anchored spacer and the stand-alone cages with a titanium plate for cervical degenerative disc disease in terms of improvement in NDI scores, JOA scores, fusion rate, and restoration of cervical lordosis, but the zero-profile anchored spacer was associated with a lower risk of postoperative dysphagia, shorter operation time, less blood loss, and relatively greater simplicity than the stand-alone cage with a titanium plate.
References
Smith GW, Robinson RA (1958) The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am 40(3):607–624
Silber JS, Anderson DG, Daffner SD, Brislin BT, Hilibrand AS, Albert TJ (2003) Donor site morbidity after anterior iliac crest bone harvest for single-level anterior cervical discectomy and fusion. Spine (Phila Pa 1976) 28(2):134–139
Fujibayashi S, Shikata J, Kamiya N, Tanaka C (2000) Missing anterior cervical plate and screws: a case report. Spine (Phila Pa 1976) 25(17):2258–2261
Lowery GL, McDonough RF (1998) The significance of hardware failure in anterior cervical plate fixation. Patients with 2- to 7-year follow-up. Spine (Phila Pa 1976) 23(2):181–186 (discussion 186–187)
Fountas KN, Kapsalaki EZ, Nikolakakos LG, Smisson HF, Johnston KW, Grigorian AA, Robinson JS (2007) Anterior cervical discectomy and fusion associated complications. Spine Phila Pa (1976) 32(21):2310–2317
Jung A, Schramm J, Lehnerdt K, Herberhold C (2005) Recurrent laryngeal nerve palsy during anterior cervical spine surgery: a prospective study. J Neurosurg Spine 2(2):123–127
Orlando ER, Caroli E, Ferrante L (2003) Management of the cervical esophagus and hypofarinx perforations complicating anterior cervical spine surgery. Spine 28(15):E290–E295
Bazaz R, Lee MJ, Yoo JU (2002) Incidence of dysphagia after anterior cervical spine surgery: a prospective study. Spine Phila Pa (1976) 27(22):2453–2458
Yue WM, Brodner W, Highland TR (2005) Persistent swallowing and voice problems after anterior cervical discectomy and fusion with allograft and plating: a 5-to 11-year follow-up study. Eur Spine J 14(7):677–682
Vernon H, Mior S (1991) The Neck Disability Index: a study of reliability and validity. J Manipulative Physiol Ther 14(7):409–415
Yonenobu K, Okada K, Fuji T, Fujiwara K, Yamashita K, Ono K (1986) Causes of neurologic deterioration following surgical treatment of cervical myelopathy. Spine Phila Pa (1976) 11(8):818–823
Hirabayashi K, Miyakawa J, Satomi K, Maruyama T, Wakano K (1981) Operative results and postoperative progression of ossification among patients with ossification of cervical posterior longitudinal ligament. Spine Phila Pa (1976) 6(4):354–364
Hacker RJ, Cauthen JC, Gilbert TJ, Griffith SL (2000) A prospective randomized multicenter clinical evaluation of an anterior cervical fusion cage. Spine Phila Pa (1976) 25(20):2646–2655
Rao RD, Gourab K, David KS (2006) Operative treatment of cervical spondylotic myelopathy. J Bone Joint Surg Am 88(7):1619–1640
Vaccaro AR, Falatyn SP, Scuderi GJ, Eismont FJ, McGuire RA, Singh K, Garfin SR (1998) Early failure of long segment anterior cervical plate fixation. J Spinal Disord 11(5):410–415
Sahjpaul RL (2007) Esophageal perforation from anterior cervical screw migration. Surg Neurol 68(2):205–209
Smith-Hammond CA, New KC, Pietrobon R, Curtis DJ, Scharver CH, Turner DA (2004) Prospective analysis of incidence and risk factors of dysphagia in spine surgery patients: comparison of anterior cervical, posterior cervical, and lumbar procedures. Spine 29(13):1441–1446
Frempong-Boadu A, Houten JK, Osborn B, Opulencia J, Kells L, Guida DD, Roux PD (2002) Swallowing and speech dysfunction in patients undergoing anterior cervical discectomy and fusion: a prospective, objective preoperative and postoperative assessment. J Spinal Disord Tech 15(5):362–368
Lee MJ, Bazaz R, Furey CG, Yoo J (2005) Influence of anterior cervical plate design on dysphagia: a 2-year prospective longitudinal follow-up study. J Spinal Disord Tech 18(5):406–409
Scholz M, Schnake KJ, Pingel A, Hoffmann R, Kandziora F (2011) A new zero-profile implant for stand-alone anterior cervical interbody fusion. Clin Orthop Relat Res 469(3):666–673
Dickerman RD, Reynolds AS, Morgan BC, Tompkins J, Cattorini J (2007) Bennett Mrh-BMP-2 can be used safely in the cervical spine: dose and containment are the keys! Spine J 7(4):508–509
Maldonado CV, Paz RD, Martin CB (2011) Adjacent-level degeneration after cervical disc arthroplasty versus fusion. Eur Spine J 20(3):403–407
Kao FC, Niu CC, Chen LH, Lai PL, Chen WJ (2005) Maintenance of interbody space in one-and two-level anterior cervical interbody fusion: comparison of the effectiveness of autograft, allograft, and cage. Clin Orthop Relat Res 430:108–116
Baba H, Furusawa N, Imura S, Kawahara N, Tsuchiya H, Tomita K (1993) Late radiographic findings after anterior cervical fusion for spondylotic myeloradiculopathy. Spine (Phila Pa 1976) 18(15):2167–2173
Schwab JS, Diangelo DJ, Foley KT (2006) Motion compensation associated with single-level cervical fusion: where does the lost motion go? Spine Phila Pa (1976) 31(21):2439–2448
Conflict of interest
None of the authors has any potential conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wang, Z., Jiang, W., Li, X. et al. The application of zero-profile anchored spacer in anterior cervical discectomy and fusion. Eur Spine J 24, 148–154 (2015). https://doi.org/10.1007/s00586-014-3628-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-014-3628-9