Abstract
Purpose
Our aim was to compare the safety and efficacy of anterior cervical discectomy and fusion (ACDF) using the Zero-P spacer versus the plate method in patients with cervical spine spondylosis.
Methods
Clinical and radiologic data from 69 patients undergoing two-level ACDF from January 2009 to May 2011 were collected prospectively. The Zero-P spacer was implanted in 37 patients (group A) and the anterior cervical plate and interbody cage in 32 (group B). Patients were followed for at least 3 years after surgery. Clinical outcomes were analyzed using the Neck Disability Index and Japanese Orthopaedic Association (JOA) scoring. The thickness of the prevertebral soft tissue at the fused levels was measured on the lateral cervical spine radiographs and dysphagia was assessed using the Bazaz score. Fusion rate, change in cervical lordosis, and adjacent segment degeneration were analyzed.
Results
Neurologic outcomes were statistically equivalent between the two groups. The incidence of postoperative dysphagia was significantly lower in group A than in group B at 2 and 6 months (p < 0.05). At the final follow-up, there were no significant differences in the C2–C7 Cobb angles between the two groups (p > 0.05). Also, degenerative changes in adjacent segments occurred in five group A patients and seven group B patients (p = 0.361). There were no differences in fusion rate during the radiologic follow-up.
Conclusions
Clinical results with the Zero-P spacer used for two-level ACDF were satisfactory. The device is superior to the traditional plate for preventing postoperative dysphagia and avoiding possible complications associated with a plate. Prospective trials with more patients and longer follow-ups are required to confirm these observations.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Degenerative conditions of the cervical spine (e.g., degenerative disc disease, cervical spondylotic myelopathy) are major causes of arm pain with or without neurologic deficits. When nonoperative treatment fails, surgery may be considered. Since the 1950s, anterior cervical discectomy and fusion (ACDF) has been widely applied in patients with cervical disc degenerative diseases [1, 2]. During this period, anterior cervical plates [3–6] and intervertebral cages [7–11] have been adopted as well. Many surgeons add an anterior plate during fusion procedures to enhance stabilization based on the fact that several studies have suggested that it leads to higher fusion rates and a lower incidence of failure [6]. Plate-associated complications, however, such as postoperative dysphagia [8, 12, 13], tracheoesophageal lesions [14], and plate shift, have raised increasing concern.
The Zero-P spacer, which can accomplish immediate stability of a treated segment as compared with the stand-alone concept, has been developed and used during the past few years. The objective of this study was to compare clinical and radiologic results of cervical spine procedures using the Zero-P spacer with those using a traditional plate method.
Materials and methods
A total of 69 patients (41 men, 28 women) were enrolled in this study from January 2009 to May 2011. Conservative therapy had been ineffective in all these patients. The decision to perform surgery was based on a clinical picture that correlated with recent magnetic resonance imaging (MRI) evidence of root or spinal cord compression. Patients with symptomatic findings at two levels of the cervical spine were included in this study. The causative diseases were radiculopathy and/or myelopathy unresponsive to conservative treatment. All patients underwent two-level ACDF from C3 to C7. The patients themselves were asked to choose which device (Zero-P spacer or anterior plate and cage) they wished to have implanted. The Zero-P spacer was implanted in 37 patients (group A) and the traditional plate and intervertebral cages in 32 patients (group B). Japanese Orthopaedic Association (JOA) score and Neck Disability Index (NDI) questionnaires were administered for functional evaluation. The incidence of dysphagia was assessed using the Bazaz system [12] at 48 h postoperatively and at the 2-, and 6-month follow-up visits (Table 1). The thickness of the prevertebral soft tissue at the fused levels was measured on the lateral cervical spine radiographs, and at plated levels, the thickness of the prevertebral soft tissue was measured from the front of the plate [15]. The mean follow-up was 41.9 months (range 36–60 months). The Specialty Committee on Ethics of Biomedicine Research at our institution approved the study.
One senior spinal surgeon from our team performed all the surgical procedures using a standard, Smith–Robinson technique. In brief, after thorough decompression and scraping off the cartilaginous endplate, the right Zero-P spacer (Synthes GmbH, Oberdorf, Switzerland) was implanted in the group A patients. In group B patients, a suitable intervertebral cage was implanted, after which a pre-bent locking plate (Slim-Loc; Depuy Spine, Johnson & Johnson, NJ, USA) of suitable curvature and length was placed. Screws were then implanted and locked. Both the intervertebral cage and the Zero-P spacer were packed with demineralized bone matrix (DBM). The correct position of the implants was identified by lateral fluoroscopy.
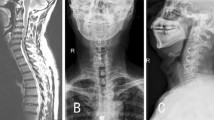
All patients wore a soft collar for the first 2 weeks after surgery. Patients underwent regular follow-up in the outpatient clinic at 2 and 6 months postoperatively and then yearly. Fusion was evaluated by computed tomography (CT) and radiograph was performed at all regular follow-ups. The sagittal profile of the cervical spine was assessed from the lateral radiographs using the Cobb angle measured between the lower endplate of the second cervical vertebra and the lower endplate of the seventh cervical vertebra. If the seventh cervical vertebra was invisible, the lower endplate of the most caudal visible cervical vertebra was chosen. The measurements were conducted in the same way for each patient [16]. The Cobb angle of the fused segments was measured by drawing two lines between the upper endplate of the cranial vertebra and the lower endplate of the caudal vertebra (Fig. 1).
Two surgeons independently performed functional and radiologic evaluations preoperatively, postoperatively, and at each follow-up visit. Statistical analysis was performed using SPSS software (version 18.0, 2010; SPSS, Chicago, IL, USA). Student’s t test and the χ 2 test were used to analyze differences between the two groups. Any value of p < 0.05 was considered to indicate statistical significance.
Results
The average operative time was 97.7 ± 4.9 min with an average blood loss of 88.9 ± 8.1 ml in group A. Group B had an average operative time of 100.3 ± 6.8 min with a mean blood loss of 92.6 ± 10.9 ml. The differences between the operative time and intraoperative blood loss for the two groups were not statistically significant (Table 2). Symptoms were alleviated in all patients after the surgery. The NDI significantly improved postoperatively in both groups. There were no significant intergroup differences pre- or postoperatively. The mean JOA score improved from 9.1 ± 0.7 points before surgery to 13.1 ± 1.7 points at the final follow-up in group A and from 8.9 ± 1.6 points to 12.9 ± 0.8 points in group B. Neurologic gain showed no significant difference between the two groups.
The mean preoperative C2–C7 Cobb angles for the fused segments were similar in the two groups. The mean C2–C7 Cobb angle was +15.2° ± 2.3° in group A and +16.3° ± 3.3° in group B at the final follow-up (p = 0.126). The mean Cobb angle for the fused segments was +7.8° ± 1.9° in group A and +8.3° ± 1.1° in group B at the final follow-up (p = 0.063). The mean C2–C7 and fused segments Cobb angles showed evident increases in both groups right after the operation. These values, however, gradually decreased throughout the follow-up visits (Figs. 2, 3). The fusion rate at 6 months postoperatively was 91.9 % (34/37) in group A and 93.8 % (30/32) in group B (p = 1.00). At the final follow-up, all patients had solid fusion.
At 48 h postoperatively, eight group A patients complained of mild dysphagia and ten group B patients (p = 0.364) complained of mild (n = 4) or moderate (n = 6) dysphagia. At the 2-month follow-up, two patients in group A still had mild dysphagia, but by 6 months it had resolved completely. In group B at 2 months, five patients still had mild and three had moderate dysphagia. Among these eight group B patients, five still complained of mild dysphagia at the 6-month follow-up (Table 3). There were significant differences between the two groups regarding the incidence of dysphagia 2 and 6 months after the surgery (p < 0.05). The thickness of the prevertebral soft tissue at the fused levels was measured (Table 4). The results suggested a significant difference of the soft tissue-swollen severity between the plate-and-cage group and the Zero-P group. The p value was significant at 48-h and 2-month postoperatively between the two groups (p < 0.05). Degenerative changes in the adjacent segments were apparent in five group A patients and seven group B patients at the final follow-up (p = 0.361). None of the patients, however, required revision surgery for any reason.
Discussion
The role of ACDF in patients with cervical spine disc disease has long been established. With increasing experience, numerous reports have documented the effective use of additional plating to treat degenerative spine conditions [4, 6, 17]. Compared to autografts and allografts, plating has the advantages of immediate postoperative stability, higher fusion rate, and a lower incidence of pseudarthrosis. It also prevents interbody graft/cage dislocation or subsidence, especially after multilevel procedures [18].
Use of an additional anterior plate, however, is associated with various intraoperative and postoperative complications. Dysphagia and tracheoesophageal lesions are reported most frequently [13, 19]. Direct contact with the esophagus is a possible cause of postoperative dysphagia, whose incidence is reported to be as high as 30 % during the first 3 months after surgery [13]. Although the stand-alone interbody cage technique was devised to avoid this problem [11, 20], unanchored cage subsidence and segmental kyphosis sometimes develop in the treated segment. Jagannathan et al. [21] reported a relatively lower incidence of dysphagia in their series of ACDF without a plate: only 9 % of their patients had dysphagia during the postoperative period, with only 3 % of patients complaining of dysphagia at the 3-month follow-up.
The Zero-P spacer ensures less contact with the anterior soft tissue, especially the esophagus, which may avoid mechanical irritation [22]. In our study, the Zero-P group had a lower incidence of dysphagia (5.4 %) at the 2-month follow-up, whereas the incidence was higher (25.0 %) in the plate-and-cage group (p = 0.037). At the 6-month follow-up, none of the Zero-P group patients complained of dysphagia, whereas five patients in the traditional plate group continued to suffer from mild dysphagia (p = 0.018). Based on this study, the Zero-P spacer is associated with a lower incidence of dysphagia than the plate-and-cage group, a finding also reported by others [16, 23].
At the mean time, the average thickness of prevertebral soft tissue in both groups increased significantly at 48 h postoperatively. We consider it is probably the prevertebral soft tissue edema and inflammation due intraoperative manipulation (e.g., retraction of the esophagus) that lead to the symptom, so the rate of dysphagia between the two groups was comparable at this time point. As time goes by, the swollen condition of the prevertebral soft tissue gradually improved. The rate of dysphagia in both groups decreased at 2 months and 6 months compared to 48 h postoperatively. However, in addition to having a higher rate of postoperative dysphagia at 2 months, five patients (15.6 %) in the plate group still complained of mild dysphagia at the 6-month follow-up. We consider that with the swollen condition improved, the direct contact with the esophagus would cause the mechanical irritation. So, we may conclude that a plate of certain thickness combined with soft tissue-swollen condition would be the possible cause of postoperative dysphagia. The direct contact with the esophagus would cause the mechanical irritation which may contribute to dysphagia after 2 months postoperatively.
The Zero-P spacer implant can avoid the possible irritation [24] against the adjacent segment caused by a plate, which is regarded as a predisposing factor [25] of adjacent segment degeneration (ASDeg). Goffin et al. [26] suggested that the shortest plate possible be used to avoid intrusion into the adjacent segments. Others [27] have asserted that a surgeon performing anterior cervical discectomy and fusion should try to achieve a plate-to-disc distance of ≥5 mm. In the present study, seven patients in the traditional plate group developed ASDeg, and we assumed that ASDeg in one patient was associated with mechanical irritation by the plate. New anterior osteophytes had formed from the tip of the plate to the adjacent level, and MRI revealed disc degeneration (Figs. 4, 5). Compared to traditional plates, the Zero-P spacer is contained within the disc space, thereby fundamentally avoiding the possible complications associated with plate insertion. At the last follow-up, none of our patients required surgical intervention. In future, we will continue to investigate and further assess whether the Zero-P device contributes to lowering the incidence of ASDeg and the need for revision surgery.
Conclusions
The primary clinical and radiographic efficacies of the Zero-P spacer used for two-level ACDF proved satisfactory. Its use avoids the possible complications caused by plate insertion and is associated with a lower incidence of postoperative dysphagia. Prospective randomized trials with more patients and longer follow-up are needed to confirm these observations.
References
Smith GW, Robinson RA (1958) The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am 40-A:607–624
Cloward RB (1958) The anterior approach for removal of ruptured cervical disks. J Neurosurg 15:602–617. doi:10.3171/jns.1958.15.6.0602
Bohler J, Gaudernak T (1980) Anterior plate stabilization for fracture-dislocations of the lower cervical spine. J Trauma 20:203–205
Fraser JF, Hartl R (2007) Anterior approaches to fusion of the cervical spine: a metaanalysis of fusion rates. J NeurosurgSpine 6:298–303. doi:10.3171/spi.2007.6.4.2
Kaiser MG, Haid RW, Jr., Subach BR, Barnes B, Rodts GE, Jr. (2002) Anterior cervical plating enhances arthrodesis after discectomy and fusion with cortical allograft. Neurosurgery 50:229–236; discussion 236–228
Song KJ, Taghavi CE, Lee KB, Song JH, Eun JP (2009) The efficacy of plate construct augmentation versus cage alone in anterior cervical fusion. Spine 34:2886–2892. doi:10.1097/BRS.0b013e3181b64f2c (Phila Pa 1976)
Agrillo U, Mastronardi L, Puzzilli F (2002) Anterior cervical fusion with carbon fiber cage containing coralline hydroxyapatite: preliminary observations in 45 consecutive cases of soft-disc herniation. J Neurosurg 96:273–276
Hwang SL, Lin CL, Lieu AS, Lee KS, Kuo TH, Hwang YF, Su YF, Howng SL (2004) Three-level and four-level anterior cervical discectomies and titanium cage-augmented fusion with and without plate fixation. J Neurosurg Spine 1:160–167. doi:10.3171/spi.2004.1.2.0160
Niu CC, Liao JC, Chen WJ, Chen LH (2010) Outcomes of interbody fusion cages used in 1 and 2-levels anterior cervical discectomy and fusion: titanium cages versus polyetheretherketone (PEEK) cages. J Spinal Disord Tech 23:310–316. doi:10.1097/BSD.0b013e3181af3a84
Tortolani PJ, Cunningham BW, Vigna F, Hu N, Zorn CM, McAfee PC (2006) A comparison of retraction pressure during anterior cervical plate surgery and cervical disc replacement: a cadaveric study. J Spinal Disord Tech 19:312–317. doi:10.1097/01.bsd.0000210117.01897.ca. 00024720-200607000-00002 [pii]
Vavruch L, Hedlund R, Javid D, Leszniewski W, Shalabi A (2002) A prospective randomized comparison between the cloward procedure and a carbon fiber cage in the cervical spine: a clinical and radiologic study. Spine (Phila Pa 1976) 27:1694–1701. doi:00007632-200208150-00003 [pii]
Bazaz R, Lee MJ, Yoo JU (2002) Incidence of dysphagia after anterior cervical spine surgery: a prospective study. Spine 27:2453–2458. doi:10.1097/01.BRS.0000031407.52778.4B (Phila Pa 1976)
Riley LH, 3rd, Skolasky RL, Albert TJ, Vaccaro AR, Heller JG (2005) Dysphagia after anterior cervical decompression and fusion: prevalence and risk factors from a longitudinal cohort study. Spine (Phila Pa 1976) 30:2564–2569. doi:00007632-200511150-00015 [pii]
Sahjpaul RL (2007) Esophageal perforation from anterior cervical screw migration. Surg Neurol 68:205–209; discussion 209–210. doi:10.1016/j.surneu.2006.09.032
Yang L, Gu Y, Liang L, Gao R, Shi S, Shi J, Yuan W (2012) Stand-alone anchored spacer versus anterior plate for multilevel anterior cervical diskectomy and fusion. Orthopedics 35:e1503–e1510. doi:10.3928/01477447-20120919-20
Vanek P, Bradac O, Delacy P, Lacman J, Benes V (2013) Anterior interbody fusion of the cervical spine with Zero-P spacer: prospective comparative study-clinical and radiological results at a minimum 2 years after surgery. Spine 38:E792–E797. doi:10.1097/BRS.0b013e3182913400 (Phila Pa 1976)
Troyanovich SJ, Stroink AR, Kattner KA, Dornan WA, Gubina I (2002) Does anterior plating maintain cervical lordosis versus conventional fusion techniques? A retrospective analysis of patients receiving single-level fusions. J Spinal Disord Tech 15:69–74
Pitzen TR, Chrobok J, Stulik J, Ruffing S, Drumm J, Sova L, Kucera R, Vyskocil T, Steudel WI (2009) Implant complications, fusion, loss of lordosis, and outcome after anterior cervical plating with dynamic or rigid plates: two-year results of a multi-centric, randomized, controlled study. Spine 34:641–646. doi:10.1097/BRS.0b013e318198ce10 (Phila Pa 1976)
Yue WM, Brodner W, Highland TR (2005) Persistent swallowing and voice problems after anterior cervical discectomy and fusion with allograft and plating: a 5- to 11-year follow-up study. Eur Spine J 14:677–682. doi:10.1007/s00586-004-0849-3
Peolsson A, Vavruch L, Hedlund R (2007) Long-term randomised comparison between a carbon fibre cage and the Cloward procedure in the cervical spine. Eur Spine J 16:173–178. doi:10.1007/s00586-006-0067-2
Jagannathan J, Shaffrey CI, Oskouian RJ, Dumont AS, Herrold C, Sansur CA, Jane JA (2008) Radiographic and clinical outcomes following single-level anterior cervical discectomy and allograft fusion without plate placement or cervical collar. J Neurosurg Spine 8:420–428. doi:10.3171/SPI/2008/8/5/420
Lee MJ, Bazaz R, Furey CG, Yoo J (2005) Influence of anterior cervical plate design on Dysphagia: a 2-year prospective longitudinal follow-up study. J Spinal Disord Tech 18:406–409. doi:00024720-200510000-00005 [pii]
Chin KR, Eiszner JR, Adams SB, Jr. (2007) Role of plate thickness as a cause of dysphagia after anterior cervical fusion. Spine (Phila Pa 1976) 32:2585–2590. doi:10.1097/BRS.0b013e318158dec8 00007632-200711010-00012 [pii]
Scholz M, Schnake KJ, Pingel A, Hoffmann R, Kandziora F (2011) A new zero-profile implant for stand-alone anterior cervical interbody fusion. Clin Orthop 469:666–673. doi:10.1007/s11999-010-1597-9
Chung JY, Kim SK, Jung ST, Lee KB (2014) Clinical adjacent-segment pathology after anterior cervical discectomy and fusion: results after a minimum of 10-year follow-up. Spine J. doi:10.1016/j.spinee.2014.01.027
Goffin J, van Loon J, Van Calenbergh F, Plets C (1995) Long-term results after anterior cervical fusion and osteosynthetic stabilization for fractures and/or dislocations of the cervical spine. J Spinal Disord 8:500–508; discussion 499
Park JB, Cho YS, Riew KD (2005) Development of adjacent-level ossification in patients with an anterior cervical plate. J Bone Joint Surg Am 87:558-563. doi:10.2106/JBJS.C.01555
Conflict of interest
No conflict of interest exits in the submission of this manuscript, and manuscript is approved by all authors for publication. I would like to declare on behalf of my co-authors that the work described was original research that has not been published previously, and not under consideration for publication elsewhere, in whole or in part. All the authors listed have approved the manuscript that is enclosed.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors (H. Chen and P. Cao) contributed equally to this article.
Rights and permissions
About this article
Cite this article
Chen, Y., Chen, H., Cao, P. et al. Anterior cervical interbody fusion with the Zero-P spacer: mid-term results of two-level fusion. Eur Spine J 24, 1666–1672 (2015). https://doi.org/10.1007/s00586-015-3919-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-015-3919-9