Abstract
Plumbagin is a plant-based naphthoquinone with anti-cancer activity. However, its side effects have limited its pharmacological significance. This study examined the effect of treatment of vitamin E on plumbagin-induced hepatic and mitochondrial injury in mice. Mitochondrial permeability transition (mPT), mitochondrial ATPase (mATPase) activity, mitochondrial lipid peroxidation (mLPO), and DNA fragmentation were determined spectrophotometrically according to standard procedures. Histological and biochemical assays were also carried out. Treatment with plumbagin induced significant opening of the mPT pore and enhanced mATPase activity and mLPO. In addition, plumbagin-treated mice showed pathological lesions in liver sections. Conversely, the two ameliorative regimens, pre- and co-treatment vitamin E groups, significantly reversed levels of liver transaminase enzymes and improved the morphological architectures of the livers of plumbagin-treated mice. Besides, plumbagin-induced mPT pore opening, ATPase activity, and percentage DNA fragmentation were significantly reversed by vitamin E. Administration of vitamin E also significantly restored the levels of the total thiol (TSH), glutathione (GSH), and superoxide dismutase (SOD) activity while lipid peroxide generation was attenuated. Taken together, the protective effect of vitamin E on plumbagin-induced liver toxicity and cell death is due to oxidative stress attenuation, improvement in antioxidant status, and amelioration of mitochondrial dysfunction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Phytochemicals have a longstanding role in the management of several diseases (Veeresham 2012). Plumbagin (PL) (5-hydroxy-2-methyl-1, 4-naphthoquinone) is a plant-based naphthoquinone that is mostly present in the root of Plumbago zeylanica and also found in some plant families (Sumsakul et al. 2014). Over the years, plumbagin has recorded remarkable biological activities including anticancer, cardiotonic, immunosuppressive, anti-malarial, antifungal, neuroprotective, hypolipidemic, antiatherosclerosis, and antibacterial activities (Itoigawa et al. 1991; Padhye et al. 2012; Bothiraja et al. 2013; Wang et al. 2015; Giacomini et al. 2020).
Indeed, the mechanism of the anticancer role of PL in different tumor types/cancer models (including resistant phenotypes) such as liver (Wei et al. 2017), prostate (Zhou et al. 2015; Song et al. 2020), pancreas (Wang et al. 2015; Pandey et al. 2020), breast (Kuo et al. 2006; Jayanthi et al. 2020), colon (Subramaniya et al. 2011; Liang et al. 2020), ovarian (Sinha et al. 2013), lung (Liu et al. 2017; Panda et al. 2020), and cervix squamous carcinoma cells (Giacomini et al. 2020) is well established. Although, plumbagin has displayed beneficial effects in several diseases and its molecular mechanism against hepatic fibrosis has been documented (Chen et al. 2015; Wei et al. 2015), nonetheless, it is known to be extremely toxic (Castro et al. 2008; Raj et al. 2011; Mbaveng et al. 2014; Jeong et al. 2015). Plumbagin was found to be genotoxic and mutagenic (Farr et al. 1985; Demma et al. 2009). Indeed, several side effects have been attributed to its administration in rodents including diarrhea, skin rashes, leukocytosis, increase in serum phosphate and acid phosphate level, hepatic toxicity, altered cytochrome P450 profiles, and reproductive toxicity in both males and females (Bhargava 1984; Sandur et al. 2006; Sukkasem et al. 2018; Bello et al. 2021). Plumbagin has also been shown to cause hepatic injury through modulation of cellular redox status, induction of hepatic lipid peroxidation, and elevated plasma liver enzymes (Sukkasem et al. 2016). Reduced toxicity of PL as well as stronger/higher therapeutic effect is usually achieved by combination with other plants (Oyebode et al. 2012, 2017; Anuf et al. 2014). Antioxidants are effective in restoring cellular redox status through elimination of reactive oxygen species (He et al. 2017). Vitamin E is a membrane-bound lipid-soluble antioxidant vitamin that can protect the membrane from free radical attack and suppress the formation of reactive oxygen species (Traber 2007; Kurutas 2015). It has been found to be effective in the prevention, delay, treatment, and reversal of various diseases owing to its antioxidant property and immune-enhancing function (Rizvi et al. 2014). Specifically, hepatoprotective effects of vitamin E against several toxicant-induced oxidative damage and liver injury have been reported (Bansal et al. 2005; Ha et al., 2019; Chalouati et al. 2019). It is not known whether vitamin E can prevent/manage plumbagin-induced liver injury. This study aimed at investigating the role of co-administration and pre-treatment of vitamin E on plumbagin-induced hepatotoxicity in mice with the aim to put forward a theoretical basis for the prevention/treatment of hepatic impairment induced by therapeutic use of plumbagin in diseased conditions.
Materials and methods
Chemicals
All chemicals used were of analytical grade. Mannitol, sucrose, HEPES, EDTA, succinate, SDS, BSA, 1-chloro-2, 4-dinitrobenzene (CDNB), thiobarbituric acid (TBA), hydrogen peroxide (H2O2), epinephrine, glutathione (GSH), and 1-chloro 2, 4 dinitrobenzene (CDNB) and other chemicals were procured from Sigma Chemical Co. (St. Louis, MO, USA.) Plumbagin was procured from Santa Cruz Biotechnology Inc., Dallas, TX, USA (CAS No: 481–42-5), while vitamin E was provided by E. Merck (India), Pvt. OLtd.
Animals
Male Swiss mice (15–20 g) were purchased from the Experimental Animal House, Faculty of Veterinary Medicine, Ibadan, Nigeria, and were used for these experiments. The mice were housed in rodent cages and kept in a well-ventilated experimental animal house under standard conditions of temperature and 12-h dark/light cycle. The animals were provided with standard mice pellets (LadokunTM Feeds, Ibadan, Nigeria) and they had access to clean drinking water ad libitum. They were acclimatized for 2 weeks before the commencement of the experiment. Experimental animals were sufficiently cared for as detailed in the “Guide for the Care and Use of Laboratory Animals” published by the National Institute of Health and experimental procedures approved by the University of Ibadan Animal Care and Use Research Ethics Committee (ACUREC) (UI-ACUREC/2065100).
Experimental outline
A pilot study was conducted to determine the dose of PL that elicits induction of mitochondrial permeability transition (mPT) pore. Eighteen (18) male Swiss mice weighing 18–25 g were randomly divided into three (3) groups of six animals each as follows:
-
Group 1: Control (0.1% DMSO),
-
Group 2: Plumbagin (4 mg/kg) and,
-
Group 3: Plumbagin (8 mg/kg).
Plumbagin was orally administered to mice for 5 days after which they were sacrificed by cervical dislocation. Mitochondrial swelling assay, liver function tests, and histological assessments were carried out to confirm liver injury.
In the main study, fifty-six mice (18–25 g) were randomly grouped into eight treatment groups of seven mice each and were treated as follows:
-
Group 1: Control: 0.1% DMSO (5 days)
-
Group 2: Plumbagin (8 mg/kg) only (5 days)
-
Group 3: Vit E (20 mg/kg) only (5 days)
-
Group 4: Plumbagin (8 mg/kg) (5 days) + Vit E (10 mg/kg) (5 days) (co-administration)
-
Group 5: Plumbagin (8 mg/kg) (5 days) + Vit E (5 days) (20 mg/kg) (co-administration)
-
Group 6: Vit E (10 mg/kg) (5 days) + plumbagin (8 mg/kg) (5 days) (pre-treatment)
-
Group 7: Vit E (20 mg/kg) (5 days) + plumbagin (8 mg/kg) (5 days) (pre-treatment)
-
Group 8: Corn oil (10 mg/ml) only (5 days)
Mice were orally administered PL (8 mg/kg) and vitamin E (10 or 20 mg/kg). The doses of vitamin E chosen for the pilot study and that of plumbagin used were based on information in literature and as previously described from published work from our laboratory (Daniel et al. 2018; Bello et al. 2021). We chose to administer plumbagin by oral route because it is the major mode of exposure to plumbagin/plant source in humans. Subsequently, mice were sacrificed and the livers were excised, and sections stored in 10% phosphate-buffered formalin for light microscopic studies. Mitochondria were isolated from the livers of each experimental group while post-mitochondrial fraction was stored for determination of GSH content and antioxidant enzymes. Additionally, clotted blood was spurn (3000 g; 15 min), and the sera obtained were stored at − 20 °C until needed for determination of liver serum enzymes.
Biochemical assays
Protein determination
Determination of serum protein levels was performed following Lowry’s method, using bovine serum albumin (BSA) as a standard (Lowry et al. 1951). Values of protein were determined from the BSA-generated calibration curve by simple extrapolation.
Determination of superoxide dismutase activity
The activity of SOD was determined according to McCord and Fridovich (1969). The increase in absorbance was monitored at 480 nm at 30 s intervals for 150 s.
The specific activity of SOD was calculated using this formula.
and expressed in units/mg protein as 50% inhibition is equal to 1 unit of SOD.
Determination of reduced glutathione
GSH levels were determined according to the method of Jollow et al. (1974). The process is based on the development of yellow color when DTNB (5, 5’ dithiobis-(2-nitrobenzoic acid) is added to compounds containing sulfhydryl groups. The absorbance was read at 412 nm. Finally, total GSH content was expressed as nmol GSH/mg protein.
Assessment of levels of serum liver enzymes
Serum enzymatic activities of alanine aminotransferase (ALT) and aspartate aminotransferase (AST) were determined spectrophotometrically by monitoring the concentration of pyruvate hydrazone formed according to the method described by Reitman and Frankel (1957). The data are presented as IU/L.
Histological studies
Excised liver sections were fixed in formalin (10%), dehydrated in ethanol (95%), and cleared with xylene before being embedded in paraffin. Subsequently, sections of about 3–4 mm of the tissue were prepared using a microtome from the paraffin-embedded gland and stained with hematoxylin and eosin (H & E) (Bancroft and Gamble 2008). Randomly, the liver histology was observed under a light microscope, after which sections were viewed and photographed.
Isolation of mice liver mitochondria
Low ionic strength liver mitochondria were isolated according to the method described by Johnson and Lardy (1967). Mice were sacrificed and dissected and livers were immediately excised and trimmed to remove excess tissue. The liver was washed several times in isolation buffer (210 mM mannitol, 70 mM sucrose, 5 mM HEPES, and 1 mM EGTA at pH 7.4), until a clear wash was obtained. It was then weighed and minced with a pair of scissors. A 10% isolation buffer suspension was prepared by homogenizing the liver in a Teflon-glass cup homogenizer. The resulting suspension was centrifuged in a refrigerated Sigma (3e30 K, Germany) centrifuged twice at 2300 rpm for 5 min to remove the nuclear fraction and cell debris. The resulting supernatant was centrifuged at 13,000 rpm for 10 min to pellet the mitochondria. The pellet obtained (mitochondria) after the supernatant was discarded was washed twice by re-suspending in washing buffer (210 mM mannitol, 70 mM sucrose, 5 mM HEPES, and 50% BSA at pH 7.4) and centrifuged at 12,000 rpm for 10 min. The mitochondria were immediately suspended in a solution of ice-cold MSH buffer (mannitol, sucrose, HEPES–KOH, pH 7.4), then aliquoted on ice in Eppendorf tubes for immediate use. The whole process was carried out on ice to preserve the integrity of the mitochondria.
Measurement of mitochondrial swelling
Mitochondrial swelling assay was carried out according to the method of Lapidus and Sokolove (1992). Mitochondria (0.4 mg/ml) were pre-incubated in the presence of 0.8 μM rotenone and MSH buffer for 3.5 min prior to the addition of 5 mM sodium succinate. To assess Ca2+-induced swelling, mitochondria were pre-incubated in 0.8 μM rotenone and MSH buffer for 3 min. Calcium was then added to the reaction mixture while sodium succinate was added 30 s later in a total reaction volume of 2.5 ml. Spermine was used as the standard inhibitor of mitochondrial swelling and was added prior to mitochondrial pre-incubation with rotenone. Change in absorbance was estimated at 540 nm at 30-s interval for 12 min in a T70 UV–visible spectrophotometer, PG Instrument Ltd. Mitochondrial swelling was measured as decrease in absorbance at 540 nm. The mitochondrial protein content was determined by the method of Lowry et al. (1951) using bovine serum albumin as standard. Permeability transition in the mitochondria isolated from the treated groups was carried out on the same mitochondrial protein content from the control group and the absorbance monitored accordingly.
Determination of mitochondrial FoF1 ATPase activity
The mATPase activity was determined as described by Olorunsogo and Malomo (1985). The total reaction mixture contained 65 mM Tris–HCl buffer pH 7.4, 0.5 mM KCl, 1 mM ATP, and 25 mM sucrose (pH = 7.4). The reaction was started by the addition of mitochondria (1 mg/ml) and was allowed to proceed in a shaker water bath for 30 min at 27 °C after which the reaction was stopped by the addition of 10% sodium dodecyl sulfate (SDS). The zero-time tube was prepared by addition of ATP to the reaction vessel with immediate addition of SDS but for 30-s intervals for other reaction vessels. The resulting supernatant was kept for phosphate determination.
Estimation of inorganic phosphate released
The concentration of inorganic phosphate released was measured according to the procedure described by Bassir (1963) and as modified by Olorunsogo et al. (1979).
Determination of mitochondrial lipid peroxidation (in vivo)
Mitochondrial lipid peroxides were measured by estimation of thiobarbituric aid reactive substances (TBARS) present in the mitochondria, a based on the reaction between 2-thiobarbituric acid (TBA) and malondialdehyde (MDA), an end product of lipid peroxides according to the method described by Varshney and Kale (1990). Using mitochondria as a lipid-rich source, mitochondria were incubated with Tris-KCL buffer in the presence of TCA. Addition of TBA under acidic conditions produced a pink color. This was immediately cooled on ice to room temperature and centrifuged at 3000 rpm for 10 min. The absorbance of the clear supernatant was measured against a reference blank of distilled water at 532 nm. The level of TBARS was calculated using extinction coefficient of 0.156/μM/cm (Adám-Vizi and Seregi 1982).
Estimation of percentage hepatic DNA fragmentation
The method of Wu et al. (2004) was used to determine the extent of endonucleases cleavage which is an endpoint in cell death assay. Briefly, DNA was extracted from liver homogenate. The supernatant and the pellet were both subjected to diphenylamine (DPA) for color development. The optical density of diphenyamine-bound DNA was measured at 620 nm and the percentage of DNA fragmentation was calculated relative to the amount of intact DNA molecules.
Statistical analysis
Statistical analyses were performed using GraphPad Prism 6.0 (GraphPad Software, San Diego, CA, USA). Multiple comparisons were performed using one-way ANOVA analysis of variance followed by Tukey’s test. All the values were expressed in mean ± standard deviation (SD) and differences were considered significant at p < 0.05.
Results
Effect of plumbagin on certain markers of liver injury and mitochondrial health
The two representative doses of plumbagin (4 and 8 mg/kg PL) tested showed a significant dose-dependent increment (p < 0.05) of the level of hepatic ALT (Fig. 1A) and AST (Fig. 1B) when compared with the control.
Plumbagin increases levels of certain markers of liver injury. A ALT. B ALT. C Status of mPT pore. D Mitochondrial FOF1 ATPase activity. E Mitochondrial LPO. F Histological examination of liver sections at a magnification of × 400. Scale bar = 20 µm. Untreated (no pathological lesion seen), 4 mg/kgPL (mild periportal infiltration of inflammatory cells), 8 mg/kgPL (sinusoids show infiltration of inflammatory cells). Significant differences from the control are indicated by a = p < 0.05. ALT, alanine amino transferase; AST, aspartate amino transferase; PL, plumbagin; LPO, lipid peroxidation; mPT, mitochondrial permeability transition
Figure 1C represents the plot of changes in absorbance of mitochondria determined from untreated group and 4 and 8 mg/kg PL-treated groups at 540 nm for the period of 12 min. An insignificant change in absorbance in the mitochondria of the untreated mice was observed depicting intact integrity of the inner mitochondrial membrane. Large amplitude swelling of the matrix by fourfold was observed when exogenous calcium was introduced, but addition of spermine, an mPT pore desensitizer, reversed the calcium-induced swelling of the untreated mice mitochondrial matrix. Interestingly, oral administration of plumbagin caused an induction of the mPT pore opening by five- and sixfold, respectively, at 4 and 8 mg/kg PL, an inductive effect which was higher than that of calcium, a classical pore inducer.
Furthermore, mitochondrial ATPase activity was enhanced by plumbagin at physiological pH in a dose-dependent style. Significant increase of twofold at the higher dose of plumbagin administered (8 mg/kg) was observed which was comparable to that of 2, 4 dinitrophenol (2.5 folds), a standard uncoupler of oxidative phosphorylation (Fig. 1D).
Figure 1E reveals that plumbagin-treated mice gave higher levels of mitochondrial thiobarbituric acid reactive substances (TBARS) when compared with control. Significant (p < 0.05) increase in the levels of mitochondria TBARS by three- and fivefold at 4 and 8 mg/kg PL was noted.
Figure 1F reveals the histological data of liver sections. It showed that the control group had normal central venules without congestion. The morphology of the hepatocytes as well as the sinusoids also appeared normal. However, pathological lesions were seen in liver sections of plumbagin-treated mice. In this regard, moderate to severe congestions and infiltrations were observed.
Vitamin E mitigates plumbagin-induced hepatic damage in mice
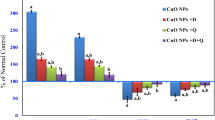
Figure 2A and B shows a significant increase (p < 0.05) of the activity of ALT and AST in the mice exposure to plumbagin respectively when compared with the control group. This effect was significantly (p < 0.05) attenuated when co-exposed and pre-treated with vit E compared with the plumbagin-treated group.
Vitamin E ameliorates plumbagin-induced liver damage in mice. A ALT. B AST. C Status of mPT pore. D Mitochondrial FOF1ATPase activity. E Percentage hepatic DNA fragmentation. Significant differences from the control are indicated by a = p < 0.05. Significant differences from plumbagin are indicated by b = p < 0.05. LPO, lipid peroxidation; PL, plumbagin; ALT, alanine aminotransferase; AST, aspartate amino transferase; mPT, mitochondrial permeability transition
The representative profile of changes in absorbance at 540 nm over period of 12 min showed in Fig. 2C showed that the untreated group retained its inner mitochondrial membrane integrity after incubated with succinate and rotenone; however, addition of calcium resulted to significant induction of mPT pore opening (4.7-fold) and reversed by 77% when incubated with spermine. The data also showed an induction fold of 3.4 in the plumbagin-treated mice, of which co-administration and pre-treatment with vit E (10 and 20 mg/kg) reversed PL-induced mPT pore opening by 61.14%, 72.54%, 74.09%, and 68.39% concomitantly.
Additionally, co-administration and pre-treatment of plumbagin with vit E (10 and 20 mg/kg) significantly ameliorated the plumbagin-induced mitochondrial ATPases activity (Fig. 2E) and percentage hepatic DNA fragmentation (Fig. 2E) when compared with the plumbagin-treated mice.
Effect of vitamin E and plumbagin on antioxidant parameters and lipid peroxidation
Administration of plumbagin induces significant depletion of the superoxide dismutase (SOD) activities when compared with the untreated group (p < 0.05). Co-administration and pre-treatment significantly abated the plumbagin-induced depletion of SOD activity, thus, enhancing the activity of the SOD even more than the control (Fig. 3A). Figure 3B and C shows that vit E significantly (p < 0.05) mitigated the depleting effect of plumbagin on the glutathione and total thiol level in the plumbagin-treated mice. More so, vit E was able to significantly (p < 0.05) inhibit the generation of mitochondrial lipid peroxide in PL-treated mice (Fig. 3D).
Vitamin E improves antioxidant status in plumbagin-induced liver toxicity in mice. A SOD. B GSH. C TSH. D LPO. Differences from the control are indicated by a = p < 0.05. Significant differences from plumbagin are indicated by b = p < 0.05. GSH, glutathione; TSH, total thiol protein; PL, plumbagin; SOD, superoxide dismutase
Vitamin E alleviates exacerbated histopathology of the liver induced by plumbagin
Administration of 8 mg/kg PL resulted to significant permeation of inflammatory cells of the periportal and sinusoid regions of the liver tissues (Fig. 4A). Co-administration and pre-treatment with vit E restored the morphology of the hepatic cell, showing mild to moderate fat infiltration and vacuolations as well as the normal morphological appearance of the sinusoids (Fig. 4 C–G).
Photomicrographs of mice liver sections stained with H and E following administration of plumbagin and treatment with vit E at a magnification of × 400. Scale bar = 20 µm. A Control: the morphology of the hepatocytes appear normal (blue arrow), no pathological lesion seen. B 8 mg/kgPL: liver parenchyma show focal areas of mild inflammatory cells. C Vit E (20 mg/kg): the sinusoids appear normal and not infiltrated (slender arrow), no pathological lesion seen. D PL + vit E (10 mg/kg): the sinusoids appear infiltrated by moderate inflammatory cells. E PL + vit E (20 mg/kg): the morphology of the hepatocytes show sparingly vesicular nuclei. F Vit E (10 mg/kg) + PL: the hepatocytes show cytoplasms with mild to moderate fat infiltration and vacuolations. G Vit E (20 mg/kg) + PL: the sinusoids appear normal and not infiltrated. H Corn oil (10 mg/ml): the liver parenchyma show focal areas of very mild inflammatory cells
Discussion
The study was conducted to examine the effect of vitamin E on plumbagin-induced hepatotoxicity in Wistar mice. Plumbagin’s LD50 has been reported to be 16 mg/kg (SivaKumar et al. 2005) with the oral bioavailability of 38.7% (Hsieh et al. 2006) for mice. Hence, a dose–response study was conducted using two doses (4 and 8 mg/kg) to examine the effect of plumbagin on the hepatic tissues as well as mitochondrial health.
Plumbagin exerted significant hepatic damage by increasing the concentration of the liver function enzymes, ALT and AST in the sera of the mice. Increase in the serum levels of ALT and AST depicts necrotic rupturing of the hepatocyte membrane (Oh et al. 2017). In addition, elevation of the plasma AST level was more prominent than that of the ALT, indicating a possibility of injury in extrahepatic organs. However, the level of ALT and AST in the sera of plumbagin-treated mice was reduced in animals pre-treated and co-administered with vitamin E.
Hepatotoxicity is well known to be associated with oxidative stress. This is a result of cellular redox status imbalance (Ramachandran et al. 2018). Thiol proteins (TSHs) and superoxide dismutase (SOD) are two cellular antioxidant that help to keep the cellular redox balance in check. Administration of plumbagin altered the hepatic redox state by significantly reducing the levels of TSH, GSH and activity of SOD when compared to the control group.
Interestingly, vitamin E significantly attenuated the plumbagin-induced oxidative stress and improves the cellular redox homeostasis of the mice via increased level of thiol proteins, glutathione, and superoxide dismutase activity.
The overwhelming effect the reactive oxygen species had on the antioxidant status resulted in oxidative stress. Studies have shown that oxidative stress can result to mitochondrial dysfunction due to alteration in mitochondrial respiratory capacity, membrane integrity, DNA stability, and calcium homeostasis (Guo et al. 2013). Hepatic dysfunction/toxicity has been correlated with the mitochondrial permeability transition pore. This is a highly evolutionarily conserved calcium-sensitive pore inside the inner membrane of the mitochondria that permits the passage of solutes smaller than 1500 Daltons in size (Mather and Rottenberg 2000; Odinokova et al. 2018). Plumbagin-treated mice showed significant induction of mPT pore opening as compared to the control. This is in consonance with the study of Giacomini et al. (2020) where plumbagin activated the opening of the transition pore in rat mitochondria. Our study showed that treatment with vitamin E significantly reversed plumbagin-induced opening of the mPT pore.
Accumulating evidence reveals that the Fo subunit of the mitochondrial ATPase is involved in the formation of the mitochondrial permeability transition pore (Giorgio et al. 2013; Bernardi and Di Lisa 2015). Therefore, to ascertain the involvement of mitochondrial ATP synthase in mPT pore formation, effects of plumbagin and varying doses of pre-treated and co-administered vitamin E in plumbagin-treated mice on mitochondrial ATPase activity were investigated. This study showed a positive correlation between mPT pore opening and mtATPase activities. The mtATPase activities were significantly enhanced in the plumbagin-treated mice, but were significantly reduced when pre-treated and co-treated with vitamin E.
Lipid serves a major player in cellular metabolic signaling such as proliferation, differentiation, inflammatory responses, energy generation, and cell death and a major component of mitochondrial membranes. Mitochondria, as a source of ROS, are particularly vulnerable to oxidative damage to lipids, DNA, and proteins (Ademowo et al. 2017). In this study, plumbagin significantly induced the generation of mitochondrial thiobarbituric acid species, which are indicators of mitochondrial lipid peroxidation. As expected, administration of vitamin E significantly reduced levels of generated lipid peroxides in the plumbagin-treated mice.
Chromatin dysfunction, such as single- and double-strand DNA fragmentation, can be caused by oxidative stress (Hernández‐Vera et al. 2010). The result showed that plumbagin showed a significant increase in percentage liver DNA fragmentation, while co-administration and pre-treatment with vitamin E significantly reduced levels of plumbagin-induced hepatic DNA fragmentation. The observed hepatotoxic effect of plumbagin and hepatoprotective effect of vitamin E was corroborated with the photomicrographs of the liver sections. These revealed severe congestions and infiltration of the liver sections in the mice treated with plumbagin and restoration of the physiological morphology of the tissue when pre-treated and co-treated with vitamin E.
Conclusion
Plumbagin caused increase in levels of oxidant species which impaired the antioxidant capacity in the mice liver. Furthermore, generation of free radicals and mitochondrial lipid peroxides activated the opening of the mPT pore and enhanced mitochondrial ATPase activity at physiological pH. These resulted in hepatic DNA fragmentation indicating that plumbagin had a detrimental and stressful effect on hepatic mitochondria. Taken together, the protective effect of vitamin E on plumbagin-induced liver toxicity is associated with oxidative stress attenuation, improvement in antioxidant status, and amelioration of mitochondrial-mediated cell death. Hence, the consumption of vitamin E can be safely used to ameliorate plumbagin-induced liver toxicity.
Data availability
Data available on request.
References
Adám-Vizi V, Seregi A (1982) Receptor independent stimulatory effect of noradrenaline on Na, K-ATPase in rat brain homogenate. Role of Lipid Peroxidation Biochem Pharmacol 31:2231–2236. https://doi.org/10.1016/0006-2952(82)90106-x
Ademowo OS, Dias HKI, Burton DGA, Griffiths HR (2017) Lipid (per) oxidation in mitochondria: an emerging target in the ageing process? Biogerontology 18:859–879
Anuf AR, Ramachandran R, Krishnasamy R et al (2014) Antiproliferative effects of Plumbago rosea and its purified constituent plumbagin on SK-MEL 28 melanoma cell lines. Pharmacognosy Res 6:312
Bancroft JD, Gamble M (2008) Theory and practice of histological techniques, 6th Edn. Churchill Livingstone, Elsevier, China.
Bansal AK, Bansal M, Soni G, Bhatnagar D (2005) Protective role of vitamin E pre-treatment on N-nitrosodiethylamine induced oxidative stress in rat liver. Chem Biol Interact 156:101–111
Bassir O (1963) Handbook of Practical Biochemistry
Bello IJ, Oyebode OT, Olanlokun JO, Omodara TO, Olorunsogo OO (2021) Plumbagin induces testicular damage via mitochondrial-dependent cell death. Chem Biol Interact 7:109–15. https://doi.org/10.1016/j.cbi.2021.109582
Bernardi P, Di Lisa F (2015) The mitochondrial permeability transition pore: molecular nature and role as a target in cardioprotection. J Mol Cell Cardiol 78:100–106
Bhargava SK (1984) Effect of plumbagin on reproductive function of male dog. Indian J Exp Biol 22:153–156
Bothiraja C, Kapare HS, Pawar AP, Shaikh KS (2013) Development of plumbagin-loaded phospholipid–Tween® 80 mixed micelles: formulation, optimization, effect on breast cancer cells and human blood/serum compatibility testing. Ther Deliv 4:1247–1259
Castro FAV, Mariani D, Panek AD et al (2008) Cytotoxicity mechanism of two naphthoquinones (menadione and plumbagin) in Saccharomyces cerevisiae. PLoS ONE 3:e3999
Chalouati H, Ben Saad MM, Payrastre L (2019) Hepatoprotective effects of vitamin E against hexachlorobenzene-induced hepatotoxicity and oxidative stress in rats: histological, biochimical and antioxidant status changes. Toxicol Mech Methods 29:18–25
Chen S, Chen Y, Chen B et al (2015) Plumbagin ameliorates CCl4-induced hepatic fibrosis in rats via the epidermal growth factor receptor signaling pathway. Evid-based Complement Altern Med 2015
Daniel OO, Adeoye AO, Ojowu J, Olorunsogo OO (2018) Inhibition of liver mitochondrial membrane permeability transition pore opening by quercetin and vitamin E in streptozotocin-induced diabetic rats. Biochem Biophys Res Commun 504(2):460–469
Demma J, Hallberg K, Hellman B (2009) Genotoxicity of plumbagin and its effects on catechol and NQNO-induced DNA damage in mouse lymphoma cells. Toxicol Vitr 23:266–271
Farr SB, Natvig DO, Kogoma T (1985) Toxicity and mutagenicity of plumbagin and the induction of a possible new DNA repair pathway in Escherichia coli. J Bacteriol 164:1309–1316
Giacomini I, Cocetta V, Carrara M et al (2020) Plumbagin induces cell cycle arrest and apoptosis in A431 cisplatin-resistant cancer cells. Nat Prod Commun 15:1934578X20921627
Giorgio V, Von Stockum S, Antoniel M et al (2013) Dimers of mitochondrial ATP synthase form the permeability transition pore. Proc Natl Acad Sci 110:5887–5892
Guo JY, Karsli-Uzunbas G, Mathew R et al (2013) Autophagy suppresses progression of K-ras-induced lung tumors to oncocytomas and maintains lipid homeostasis. Genes Dev 27:1447–1461
HA W, Bartimaeus ES, Nduka N, Nwanjo HU (2019) Effect of combination therapy of Garcinia kola seed and vitamin E in acetaminophen induced hepatotoxicity and oxidative stress in albino rats
He L, He T, Farrar S et al (2017) Antioxidants maintain cellular redox homeostasis by elimination of reactive oxygen species. Cell Physiol Biochem 44:532–553
Hernandez-Vera G, Mitrović M, Jović J et al (2010) Host-associated genetic differentiation in a seed parasitic weevil Rhinusa antirrhini (Coleptera: Curculionidae) revealed by mitochondrial and nuclear sequence data. Mol Ecol 19:2286–2300
Hsieh Y-J, Lin L-C, Tsai T-H (2006) Measurement and pharmacokinetic study of plumbagin in a conscious freely moving rat using liquid chromatography/tandem mass spectrometry. J Chromatogr B 844:1–5
Itoigawa M, Takeya K, Furukawa H (1991) Cardiotonic action of plumbagin on guinea-pig papillary muscle. Planta Med 57:317–319
Jayanthi M, Gokulanathan A, Haribalan P et al (2020) Plumbagin from two Plumbago species inhibits the growth of stomach and breast cancer cell lines. Ind Crops Prod 146:112147
Jeong SH, Choi JS, Ko YK, Kang NS (2015) The discovery of bioisoster compound for plumbagin using the knowledge-based rational method. J Mol Struct 1085:84–89
Johnson D, Lardy H (1967) [15] Isolation of liver or kidney mitochondria. Methods Enzymol 10:94–96. https://doi.org/10.1016/0076-6879(67)10018-9
Jollow DJ, Mitchell JR, Zampaglione N, Gillette JR (1974) Bromobenzene-induced liver necrosis. Protective role of glutathione and evidence for 3,4-bromobenzene oxide as the hepatotoxic metabolite. Pharmacology 11:151–169. https://doi.org/10.1159/000136485
Kuo P-L, Hsu Y-L, Cho C-Y (2006) Plumbagin induces G2-M arrest and autophagy by inhibiting the AKT/mammalian target of rapamycin pathway in breast cancer cells. Mol Cancer Ther 5:3209–3221
Kurutas EB (2015) The importance of antioxidants which play the role in cellular response against oxidative/nitrosative stress: current state. Nutr J 15:1–22
Lapidus RG, Sokolove PM (1992) Inhibition by spermine of the inner membrane permeability transition of isolated rat heart mitochondria. FEBS Lett 313:314–318. https://doi.org/10.1016/0014-5793(92)81217-A
Liang Y, Zhou R, Liang X et al (2020) Pharmacological targets and molecular mechanisms of plumbagin to treat colorectal cancer: a systematic pharmacology study. Eur J Pharmacol 881:173227
Liu Y, Cai Y, He C et al (2017) Anticancer properties and pharmaceutical applications of plumbagin: a review. Am J Chin Med 45:423–441
Lowry OH, Rosebrough NJ, Farr AL, Randal RJ (1951) Protein measurement with the Folin phenol reagent. J Biol Chem 193:265–275. https://doi.org/10.1016/0922-338X(96)89160-4
Mather M, Rottenberg H (2000) REGULAR ARTICLES-Aging enhances the activation of the permeability transition pore in mitochondria. Biochem Biophys Res Commun 273:603–608
Mbaveng AT, Zhao Q, Kuete V (2014) Harmful and protective effects of phenolic compounds from African medicinal plants. In: Toxicological Survey of African Medicinal Plants. Elsevier, pp 577–609
McCord JM, Fridovich I (1969) Superoxide dismutase: an enzymic function for erythrocuprein (hemocuprein). J Biol Chem 244:6049–6055
Odinokova IV, Baburina YL, Kruglov AG et al (2018) Operation of the permeability transition pore in rat heart mitochondria in aging. Biochem (Moscow). Suppl Ser A Membr Cell Biol 12:137–145
Oh RC, Hustead TR, Ali SM, Pantsari MW (2017) Mildly elevated liver transaminase levels: causes and evaluation. Am Fam Physician 96:709–715
Olorunsogo OO, Bababunmi EA, Bassir O (1979) Effect of glyphosate on rat liver mitochondria in vivo. Bull Environ Contam Toxicol 22:357–364. https://doi.org/10.1007/BF02026955
Olorunsogo OO, Malomo SO (1985) Sensitivity of oligomycin-inhibited respiration of isolated rat liver mitochondria to perfluidone, a fluorinated arylalkylsulfonamide. Toxicology 35:231–240. https://doi.org/10.1016/0300-483X(85)90018-6
Oyebode OT, Akinbusuyi OT, Akintimehin SE, Olorunsogo OO (2017) Modulation of cytochrome C release and opening of the mitochondrial permeability transition pore by Calliandra portoricensis (Benth) Root Bark Methanol Extract. European J Med Plants 20:1–14
Oyebode OT, Odejide TT, Kukoyi AJ et al (2012) Effects of different fractions of Calliandra portoricensis root bark on isolated rat liver mitochondrial membrane permeability transition pore. Afr J Med Med Sci 41:399–409
Padhye S, Dandawate P, Yusufi M et al (2012) Perspectives on medicinal properties of plumbagin and its analogs. Med Res Rev 32:1131–1158
Panda M, Tripathi SK, Biswal BK (2020) Plumbagin promotes mitochondrial mediated apoptosis in gefitinib sensitive and resistant A549 lung cancer cell line through enhancing reactive oxygen species generation. Mol Biol Rep 47:4155–4168
Pandey K, Tripathi SK, Panda M, Biswal BK (2020) Prooxidative activity of plumbagin induces apoptosis in human pancreatic ductal adenocarcinoma cells via intrinsic apoptotic pathway. Toxicol Vitr 65:104788
Raj G, Kurup R, Hussain AA, Baby S (2011) Distribution of naphthoquinones, plumbagin, droserone, and 5-O-methyl droserone in chitin-induced and uninduced Nepenthes khasiana: molecular events in prey capture. J Exp Bot 62:5429–5436
Ramachandran A, Visschers RGJ, Duan L et al (2018) Mitochondrial dysfunction as a mechanism of drug-induced hepatotoxicity: current understanding and future perspectives. J Clin Transl Res 4:75
Reitman S, Frankel, (1957) A colorimetric method for the determination of serum glutamic oxalacetic and glutamic pyruvic transaminases. Am J Clin Pathol 28:56–63. https://doi.org/10.1093/ajcp/28.1.56
Rizvi S, Raza ST, Faizal Ahmed AA et al (2014) The role of vitamin E in human health and some diseases. Sultan Qaboos Univ Med J 14:e157
Sandur SK, Ichikawa H, Sethi G et al (2006) Plumbagin (5-hydroxy-2-methyl-1, 4-naphthoquinone) suppresses NF-κB activation and NF-κB-regulated gene products through modulation of p65 and IκBα kinase activation, leading to potentiation of apoptosis induced by cytokine and chemotherapeutic agents. J Biol Chem 281:17023–17033
Sinha S, Pal K, Elkhanany A et al (2013) Plumbagin inhibits tumorigenesis and angiogenesis of ovarian cancer cells in vivo. Int J Cancer 132:1201–1212
SivaKumar V, Prakash R, Murali MR et al (2005) In vivo micronucleus assay and GST activity in assessing genotoxicity of plumbagin in Swiss albino mice. Drug Chem Toxicol 28:499–507
Song Y, Yuan Y, Shi X, Che Y (2020) Improved drug delivery and anti-tumor efficacy of combinatorial liposomal formulation of genistein and plumbagin by targeting Glut1 and Akt3 proteins in mice bearing prostate tumor. Colloids Surfaces B Biointerfaces 190:110966
Subramaniya BR, Srinivasan G, Mohammed Sadullah SS et al (2011) Apoptosis inducing effect of plumbagin on colonic cancer cells depends on expression of COX-2. PLoS ONE 6:e18695
Sukkasem N, Chatuphonprasert W, Jarukamjorn K (2018) Altered cytochrome P450 profiles by Plumbago indica Linn. and plumbagin after oral administration in mice. Pharmacogn Mag 14:507
Sukkasem N, Chatuphonprasert W, Tatiya-Aphiradee N, Jarukamjorn K (2016) Imbalance of the antioxidative system by plumbagin and Plumbago indica L. extract induces hepatotoxicity in mice. J Intercult Ethnopharmacol 5:137
Sumsakul W, Plengsuriyakarn T, Chaijaroenkul W et al (2014) Antimalarial activity of plumbagin in vitro and in animal models. BMC Complement Altern Med 14:1–6
Traber MG (2007) Vitamin E regulatory mechanisms. Annu Rev Nutr 27:347–362
Varshney R, Kale RK (1990) Effects of calmodulin antagonists on radiation-induced lipid peroxidation in microsomes. Int J Radiat Biol 58:733–743. https://doi.org/10.1080/09553009014552121
Veeresham C (2012) Natural products derived from plants as a source of drugs. J Adv Pharm Technol Res 3:200
Wang F, Wang Q, Zhou Z-W et al (2015) Plumbagin induces cell cycle arrest and autophagy and suppresses epithelial to mesenchymal transition involving PI3K/Akt/mTOR-mediated pathway in human pancreatic cancer cells. Drug Des Devel Ther 9:537
Wei Y, Huang M, Liu X et al (2015) Anti-fibrotic effect of plumbagin on CCl4-lesioned rats. Cell Physiol Biochem 35:1599–1608
Wei Y, Yang Q, Zhang Y et al (2017) Plumbagin restrains hepatocellular carcinoma angiogenesis by suppressing the migration and invasion of tumor-derived vascular endothelial cells. Oncotarget 8:15230
Wu LL, Chiou CC, Chang P, Wu JT (2004) Urinary 8-OHdG: a marker of oxidative stress to DNA and risk factor for cancer, atherosclerosis and diabetics. Clin Chiminca Acta 339(1–2):1–2
Zhou Z-W, Li X-X, He Z-X et al (2015) Induction of apoptosis and autophagy via sirtuin1-and PI3K/Akt/mTOR-mediated pathways by plumbagin in human prostate cancer cells. Drug Des Devel Ther 9:1511
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This research received no external funding.
Conflict of interest
The authors declare no competing interests.
Ethical approval
ARRIVE guidelines were strictly followed and all experimental procedures were conducted according to the University of Ibadan Animal Care and Use Research Ethics Committee (ACUREC) with approval number-UI-ACUREC/2065100 which conformed to that of NIH and was strictly adhered to.
Informed consent
For this type of study informed consent is not required.
Consent for publication
All authors of the paper have read, approved, and consented to the final version submitted.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Oyebode, O.T., Bello, I.J., Faleke, H. et al. Protective effect of vitamin E against plumbagin-induced liver injury and oxidative stress: biochemical, redox, and mitochondrial permeability changes. Comp Clin Pathol 32, 311–320 (2023). https://doi.org/10.1007/s00580-023-03441-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00580-023-03441-w