Abstract
Plumbagin (PL) is a natural naphthoquinone compound, isolated from Plumbago zeylanica that has cytotoxic and antimigratory potential in many cancer. However, the cytotoxic mechanism of plumbagin in drug resistant lung cancer is poorly understood. To reveal the mechanism, we studied the anticancer effect of plumbagin in both gefitinib-sensitive and resistant A549 lung cancer cells. The anticancer potential of PL was demonstrated by MTT assay and the result suggested that PL showed cytotoxicity in both gefitinib-sensitive (A549) and gefitinib-resistant (A549GR) lung cancer cells. IC50 values of PL in A549 and A549GR were 3.2 μM and 4.5 μM, respectively. Morphological changes were also observed after treatment with PL. Furthermore, PL decreased cell survival by inhibiting colony formation ability, and inhibited cell migration at very low concentrations. From Annexin V-FITC/PI, AO/EtBr, and DAPI staining, we found that increasing concentration of PL leads to increase in apoptosis of lung cancer cells. Furthermore, western blotting results suggested that Bax and Caspase 3 levels were upregulated after PL treatment. In addition, treatment of PL caused DNA damage in a dose-dependent manner. PL arrested the cell cycle at S-G2/M phase, and enhanced reactive oxygen species (ROS) generation. Excess ROS generated by PL disrupted mitochondrial membrane resulted in depletion of mitochondrial membrane potential (MMP). These results conclude that PL decreases lung cancer cell viability by arresting cells at S-G2/M phase, and induces apoptosis by activation of mitochondrial-mediated apoptotic pathway through excess ROS generation. Overall findings suggest that plumbagin shows cytotoxic and therapeutic potential against both A549 and A549GR cell lines.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
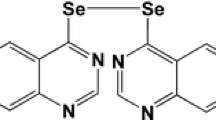
Lung cancer continues to be the most leading cause of cancer-related death worldwide. Identification and analysis of lung cancer in the earlier stage is troublesome due to the lack of any visible symptoms. Current therapeutic options, such as chemo- and radio-therapy have limited success in lung cancer especially in non-small cell lung carcinoma (NSCLC). Therefore, better therapeutic choices that could possibly counteract the underlying phases of lung carcinogenesis are massively advantageous. Natural compounds possess anticancer properties; therefore these naturally derived compounds are preferentially used in the in vivo and clinical studies. Recently, use of natural products in the targeted therapy is extensively studied [1]. Plumbagin (5-hydroxy-2-methyl-1, 4-naphthoquinone) is a natural compound confined from the root of the plant, Plumbago zeylanica. Plumbagin has many medicinal properties such as antiatherogenic, antiatherosclerotic, antimicrobial, cardiotonic, hepatoprotective, and neuroprotective impacts. In addition, the compound shows potent anticancer activity due to its promising antiproliferative and apoptotic activity in various cancer cell. Due to pleiotropic nature of plumbagin (PL), it may categorize as a more suitable therapeutic drug for the treatment of cancer over conventional anticancer drugs in near future [2,3,4,5]. Interstingly, studies suggest that plumbagin shows cytotoxicity in different types of cancer cells (such as breast cancer, cervical cancer, and lung cancer); however lack of toxicity in normal human cells ( such as normal BJ cells, HepG2 cells, and lung fibroblast cells WI-38) [6, 7]. In short, PL can be used as a potent therapeutic agent in various diseases, including cancer [8,9,10,11,12,13]. Plumbagin also acts as a chemosensitizer in some cancers, such as breast cancer [14]. Moreover, it has been observed that PL induces anti-lung cancer activity via enhancing intracellular reactive oxygen species (ROS) levels [15, 16]. However, molecular insights underlying the reversal of drug resistance by PL in gefitinib resistant A549 lung cancer cell line (A549GR) are still unraveled.
The study of Gomathinayagam et al. suggested that plumbagin decreases cell viability and induces apoptosis by activating caspase 3 protein in lung cancer [17]. Previous studies have shown that anticancer activity of plumbagin is associated with ROS generation in many cancers, such as breast, osteosarcoma, prostate, pancreatic etc.[9, 18,19,20]. It has been also shown that plumbagin induced excess ROS generation, leads to disruption of mitochondrial membrane potential of cancer cells, thereby cancer cell death [21]. Molecular docking analysis suggests that plumbagin has well binding ability with TRAIL–DR5 receptor ligand complex, which induces apoptosis in breast cancer cells [21]. Moreover, it has also been reported that intracellular ROS level is positively correlated with DNA damage [22]. These findings give the idea to investigate further cytotoxic and pro-apoptotic role of plumbagin in lung cancer cell A549 and gefitinib-resistant cell A549GR. This is the first study to elucidate the effect of PL on intracellular ROS levels and mitochondrial dysfunction in A59 and A549GR cells. The present study aimed to explore the role of plumbagin in cytotoxicity, changes in morphology, DNA damage, and cellular apoptosis via increase in intracellular ROS level and decrease in mitochondrial membrane potential (MMP) in A549 and A549GR cells.
Materials and methods
Chemical reagents
Carbonyl cyanide m-chlorophenylhydrazone (CCCP), Plumbagin, Dichloro-dihydro-fluorescein diacetate (DCF‐DA), Rhodamine-123 (RHO-123) were purchased from Sigma-Aldrich, USA. Acridine orange (AO), Ethidium bromide (EtBr), 4′,6-diamidino-2-phenylindole (DAPI), N-Acetyl Cysteine (NAC), 3-(4, 5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT), Ribonuclease-A, and Triton X-100 were supplied by HI Media Laboratories Pvt. Ltd., India. AnnexinV-FITC/PI staining kit, and primary antibodies Bax, Caspase 3, and secondary antibodies were brought from ABGENEX Private Limited, India. Primers (GAPDH, Beta-actin, GSTP1, SOD2, and PARK7) were brought from Integrated DNA Technologies (IDT). Gefitinib was purchased from Santa Cruz Biotechnology, USA.
Cell culture
The lung cancer cell line A549 was purchased from National Centre for Cell Science (NCCS) Pune, India. A549 cell line was cultured in Dulbecco’s Modified Eagle Medium (DMEM) containing 2 mM glutamine, 1% antibiotic–antimycotic, and 10% fetal bovine serum (FBS). The cell lines were maintained at 37 ˚C in a 5% CO2 incubator. DMEM, glutamine, antibiotic–antimycotic, and FBS were brought from Gibco/Invitrogen, USA.
Generation of gefitinib resistance in A549 cell line (A549GR)
Gefitinib resistance in A549 cell line was developed from the parental A549 cell line. Parental A549 cell line was treated with gefitinib having starting concentration 10 nM. Gefitinib concentration was increased when the cells were adapted to new drug concentration, and the cells were fixed at the final concentration of 25 μM.
MTT assay
To study the cytotoxic potential of PL in the A549 cell line and A549GR cell line, 5000 cells per well were seeded in 96-well culture plate. After 15 h of incubation, seeded cells were treated with various doses of PL ranging from 0 to 10 μM. After 24 h of PL drug treatment, 100 μL of MTT solution (5 mg/ml) was added to each well and kept in the incubator for 4 h at 37 ˚C. Then, 100 μL DMSO was added to dissolve the crystals, and cell viability was measured by taking absorbance at a wavelength of 570 nM in ELISA Plate Reader (Synergy-H1microplatereader, Biotek, USA).
Colony-forming assay
To measure the antiproliferative potential of PL in both A549 and A549GR cell lines, 500 cells were seeded in each well of 6-well plate. After 24 h of incubation, PL treatment was done at 3 μM and 5 μM concentrations for 24 h, and cells were grown for 10–14 days to form colonies. Then, cells were fixed with 100% methanol for 20 min. After that, fixed cells were stained with 150 μl crystal violet for 5 min. Total numbers of colonies were calculated.
Morphological observation
To study the effect of PL in morphological changes, cells from both the cell lines were seeded at a density of 1 × 105 cells/well in 12-well plate, and PL treatment was done. Images were taken at 24 h and 48 h and alternations in the cellular morphology were observed under a bright-field microscope (Olympus, Japan).
In vitro scratch assay
Inhibitory effect of PL on A549 and A549GR cell migration was demonstrated by performing wound healing assay. In brief, 3 × 105 cells per well were seeded in 6-well plate and incubated till a confluency monolayer formed. Then, serum-free media was added, and kept for 24 h. Scratch was created with the help of a 1 ml tip. Then, PL drug treatment was done and images were taken at 0 h and 24 h under an inverted microscope (Magnus, India).
where Ai is area of wound scratch at the initial time, Af is area of wound healing at the final time.
Acridine orange/Ethidium bromide (AO/EtBr) staining
Apoptosis-inducing effect of PL was examined by staining with AO/EtBr. AO stains both healthy and dead cells whereas EtBr stains only dead cells. Cells at a density of 3 × 105 per well were seeded in 6-well plate. After adhesion, seeded cells were exposed to PL for 24 h. Then, cells were trypsinized and 25 μL of cell suspensions were incubated with 1 μL of AO/EtBr solution. The stained cells were observed under a fluorescence microscope (Olympus, Japan).
4′,6-Diamidino-2-phenylindole (DAPI) staining
Nuclear morphology changes were detected through DAPI staining. Cells at a density of 3 × 105 per well were plated in 6-well plate and exposed to PL for 24 h. Then, cells were washed with PBS and fixed with 2% paraformaldehyde for 15 min. Then, cells were suspended in PBS containing 0.2% Triton-X for 15 min at room temperature. The stained cells were observed under a fluorescence microscope (Olympus, Japan).
Annexin V-FITC/PI staining assay
Apoptotic inducing effect of PL was confirmed by performing Annexin V-FITC/PI staining assay and % of apoptosis was quantified by flow cytometry. In brief, 1 × 105 cells were seeded in 12-well cell culture plate. PL was given to seeded cells and incubated for 24 h. Then, cells were pelleted down, and pellet was suspended in 100 μL binding buffer containing 5 μL Annexin V and 5 μL PI and incubated them for 20–25 min in the darkroom. After incubation, 400 μL binding buffer was added, and % of apoptosis was measured by using flow cytometer (BD AccuriTMC6, USA).
Comet assay
Comet assay was performed as described by Dhawan et al. [22]. Control and PL-treated cells were centrifuged and resuspended the pelleted cells in 0.5% low melting agarose at 37 °C. Then, 50 μL of agarose containing cells laid down on pre-coated glass slide (coated with 0.5% normal melting agarose), and covered with a coverslip. Then, the slides were kept at 4 °C for 5 min to solidify. After solidification, the coverslip was removed, and slides were placed in lysis solution (2.5 M NaCl, 100 mM EDTA, 10 mM Tris, 1% Triton X-100, and 10% dimethyl sulfoxide) for 1 h at 4° C. Then, the slides were electrophoresed for 30 min at 25 V. After electrophoresis, cells were washed with 0.4 M Tris and stained with ethidium bromide and observed under a fluorescence microscope (Olympus, Japan).
Cell cycle analysis
To check cell cycle distribution, cells were seeded for 15 h in 12 well plate and then treated with 3 μM and 5 μM of PL for 24 h. After treatment, cells were pelleted down. Then, cells were suspended in ice-cold 70% ethanol overnight. After incubation, cells were pelleted down and suspended the cells in 0.5 ml cold PBS solution having Ribonuclease-A (1000 μg/ml), and Triton X-100 (1%) for 30 min at room temperature. Then, cells were stained with PI (50 μg/ml) for 30 min, and stained cells (10,000 cells) were analyzed using flow cytometer (BD AccuriTMC6, USA).
Measurement of reactive oxygen species
To measure the intracellular ROS level, 1 × 105 cells per well were seeded in 12-well plate. Seeded cells were treated with PL alone or in combination with NAC for 24 h. Then, staining was done with 20 μM DCFH-DA for 45 min. Flow cytometer was used to monitor the fluorescent-oxidized DCF, and qualitative images were examined under a fluorescence microscope (Olympus, Japan).
Measurement of mitochondrial membrane potential
To evaluate the effect of PL in mitochondrial membrane potential, 1 × 105 cells/well were plated in 12-well plate. After 15 h of seeding, 3 μM and 5 μM concentrations of PL were given, and 50 μM CCCP was used as a positive control. Next, cells were pelleted down, and incubated with Rhodamine123 (10 μg/ml) for 30 min at room temperature. Quantitative measurement was taken by measuring the intensity of the stained cell using flow cytometer (BD AccuriTMC6, USA), and qualitative images were examined under a fluorescence microscope (Olympus, Japan).
Quantitative Real-time PCR
To measure the antioxidant gene expression, total RNA was extracted using the Trizol (Molecular Research Centre, USA) method. cDNA was synthesized using cDNA synthesis kit (Applied Biosystems,Thermofisher Scientific USA), and Real-time PCR was performed using Invitrogen protocol. β-actin was used as a housekeeping gene for qRT-PCR. All primer sequences are enlisted in Table 1.
Western blotting analysis
Proteins were extracted by RIPA buffer and quantified using the Pierce™ BCA Protein Assay kit. Then, proteins were separated by SDS-PAGE gel and transferred to the nitrocellulose membrane (HI Media Laboratories Pvt. Ltd.). Then, the blot was blocked for 1 h using blocking buffer containing 5% skimmed milk in Rockymax. After blocking, the blot was incubated with primary antibodies (dilution 1:250) such as- Bax, and Caspase-3 (Abgenex, Pvt. Ltd.) for 9 h at 4 °C. After that, blot was incubated with their respective secondary antibodies for 2 h in room temperature. β-actin was used as a loading control.
Statistical analysis
Results were exhibited as the mean ± standard deviation of three independent experiments. Statistical differences between the control and treatment tests were controlled by paired t-test. **P < 0.05 and ***P < 0.001 were considered to suggest statistically significant differences.
Results
Cytotoxic potential of plumbagin
Cytotoxic potential of PL in both A549 and A549GR cell lines was evaluated by performing MTT assay. Treatment with various doses of PL (0–10 μM) for 24 h, inhibited cell growth in a dose-dependent manner in both the cell lines. Also, a decrease in the rate of cell proliferation of A549 was found to be more as compared to A549GR in presence of PL. IC50 values of PL in A549 and A549GR cells were 3.2 μM and 4.5 μM respectively (Fig. 1a). Since PL inhibited cell proliferation significantly at very low doses, we further investigated the effect of PL on colonogenic potential in both A549 and A549GR cell lines. Exposure of cells with 3 μM and 5 μM concentration of PL strongly inhibited clonal expansion as compared to non-treated control cell (Fig. 1b, c). This experiment also confirmed that PL decreased cell survival in a dose-dependent manner. Furthermore, we also found that treatment of PL induced morphological changes in both A549 and A549GR cells. In comparision to control cells, morphology of PL-treated cells was changed dramatically, and number of PL treated cells was also reduced. Additionally at 5 μM concentration, most of the cells were detached from the plate and floated on medium while untreated control cells exhibited a normal morphology (Fig. 1d). Together all the results concluded that PL shows cytotoxicity against both A549 and A549GR cell lines.
Effect of PL on cell viability and morphology in A549 and A549GR cell lines. a cell viability was determined by MTT assay. Both the cell lines were treated with various doses of PL (0–10 μM) for 24 h and IC50 values were calculated by GraphPad Prism 5.0 (GraphPad, USA). Experiments were done in quadruplex (n = 4), b represents qualitative images of clonogenic assay, c influence of PL on no. of colony-forming cells, quantified from clonogenic assay images, d morphological differences between A549 and A549GR cells were observed under a phase-contrast microscope; scale bar = 10 μm
Antimigratory potential of plumbagin
To evaluate the antimigratory effect of PL, cells were treated with 3 μM and 5 μM concentrations of PL. Cell migration was evaluated using in vitro scratch assay. The results from in vitro scratch assay of A549 cells demonstrated that PL treatment for 24 h resulted in wound closure by 56.5%, 20.66% and 7.33% in control, 3 μM and 5 μM PL respectively. But in A549GR, wound closure occurred by 52.33%, 24.82% and 17.33% in control, 3 μM and 5 μM PL respectively (Fig. 2a, b). These results determined that PL significantly reduced the invasiveness and rapid proliferation of A549 and A549GR in a dose-dependent manner.
Effect of PL on cell invasion in both A549, and A549GR cell lines. Wound healing assay of lung cancer cell was performed; treatment of cells was done at 3 μM and 5 μM concentrations of PL. a Images were captured at 0, 24 h under a phase-contrast inverted microscope, b represents quantitative data obtained from images of in vitro scratch assay. Experiments were done in three independent experiments. Bars, s.e.m, **P < 0.05
Apoptotic potential of plumbagin
To explore the apoptotic effect of PL, we performed AO/EtBr, DAPI, and Annexin V-FITC/PI staining. AO can enter to an intact cell, and stained live cell shows green but EtBr can penetrate only to the damaged cell such as late apoptotic cell and necrotic cell. AO/EtBr staining data suggested that live cells had normal cellular morphology, and uniformly stained with AO forming green nuclei. Contrast to control, plumbagin treated A549 and A549GR cells showed changes in morphology like membrane shrinkage and membrane damage. Early apoptotic cells stained green and contained small dots of bright green color in nuclei whereas, late apoptotic cells showed more number of orange to red nuclei because of incorporation of EtBr due to membrane damage (Fig. 3a). Further, we evaluated the apoptotic effect of PL on nuclear morphology of both A549 and A549GR cell lines. DAPI staining suggested that both A549 and A549GR control cells possessed normal intact nuclei. However, PL-treated cells were found to be increased in nuclear condensation and fragmentations at 3 μM and 5 μM concentrations of PL (Fig. 3b). To figure out the alternation of phosphatidylserine from inner to outer membrane after PL treatment, Annexin V-FITC/PI staining was performed. The results showed that the percentage of the apoptotic cells increased significantly at 3 μM and 5 μM concentration of PL as compared to control. In addition, ROS scavenger NAC was also used to confirm the PL-induced ROS based mitochondrial-mediated apoptosis. Results showed that NAC reversed the apoptotic effect of PL in both the cell lines. While treatment of NAC, the percentage of apoptotic cells decreased significantly at NAC + 3 μM PL as compared to 3 μM PL alone in both A549 and A549GR cell lines (Fig. 3c).
Effect of PL on nuclear morphology and apoptosis in lung cancer cells. A549 and A549GR cells were treated with 3 μM and 5 μM concentrations of PL for 24 h. a apoptosis induced phenotypic changes, b nuclear morphology changes during apoptosis of both the cancer cells were viewed under a fluorescence microscope, c represents apoptotic cell in terms of percentage obtained from Annexin V-FITC/PI double-staining, d, e influence of PL on apoptotic proteins
To cross-confirm the apoptosis-inducing potential of PL, we further examined the apoptotic potential at the protein level. 3 μM and 5 μM of PL were given to A549 and A549GR cells for 24 h. Result suggested that pro-apoptotic protein; Bax was upregulated in PL-treated cells in both the A549 and A549GR cell lines. Caspase activation is a hallmark of apoptosis such as- DNA condensation and DNA fragmentation. Therefore, we also studied the Caspase expression at the protein level. Figure 3d showed that Caspase 3 expression was upregulated in both A549 and A549GR cell lines. These results suggested that increase in the concentration of PL also increased pro-apoptotic protein, Bax and Caspase 3 levels.
DNA damaging potential of plumbagin
Since PL enhanced ROS level in both A549 and A549GR cell lines, therefore we hypothesized that ROS might induce breaks in the DNA strand. That's why we evaluated the DNA damaging potential of PL by performing the comet assay. This is a very sensitive technique used to detect DNA strand breaks. In the presence of the electric field, broken DNA migrates from the nucleus and form a tail of the comet. In addition, comet tail length represents the extent of DNA damage. Results showed that 5 μM PL treated cells were having more damaged DNA as compared to 3 μM PL treated cells. However, control cells showed no DNA damage (Fig. 4).
PL induced DNA fragmentation as indicated by comet assay. A549 cells were treated with 3 μM and 5 μM PL. Cells were stained with ethidium bromide and observed under fluorescence microscope. a influence of PL on DNA damage which was obtained from fluorescence microscopy, b, c represents tail DNA %, and tail moment data obtained from fluorescence microscopy. Experiments were done in triplicates, and **P < 0.05 and ***P < 0.001
Induction of cell cycle arrest at S-G2/M by plumbagin
PL has been reported to induce cell cycle arrest in various cancers such as- pancreatic, cervical, breast cancer, etc. [23,24,25]. In both A549 and A549GR cell lines, most of the control cells were at G1 and S phases. However, after 24 h of PL treatment, most of the cells were at S and G2/M phases along with reducing the percentage of cells at the G1 phase. This indicated that PL induced cell cycle arrest at S-G2/M phases. Moreover, NAC treatment reversed the cell cycle arrest in both the cell lines. These results suggested that PL induced cell cycle arrest by increasing ROS levels (Fig. 5a, b).
Elevation of reactive oxygen species generation by plumbagin
There are many reports suggested that ROS plays a vital role in inducing apoptosis in various cancers [26, 27]. In our study, treatment of PL at 3 μM and 5 μM concentrations, ROS related fluorescent intensity increased as compared to control. PL induced ROS generation, which was confirmed by treatment with NAC alone or in combination with PL (Fig. 6a). The results showed that the combined treatment of PL with NAC reduced cytotoxicity of PL. In addition, flow cytometry data suggested that the peak of PL treated cells was shifted towards right side compared to the control. However, treatment with NAC alone or combined with PL; peak was reverted towards control side (Fig. 6b). Collectively, these data showed that PL increased ROS levels, which in turn induced apoptosis in A549 and A549GR lung cancer cells.
PL induced ROS generation in lung cancer. a cells from both the cell lines A549 and A549GR were treated with various doses of PL alone, and combination of NAC with PL, and observed under a fluorescence microscope, b represents flow cytometry data of ROS measurement, c measurement of relative mRNA expression levels of antioxidant genes through Q-PCR
As excess ROS creates damages to DNA, lipid, and protein, so to counteract these effects, cells adopt the ROS stress mechanism by activating various antioxidant ROS scavengers such as superoxide dismutase (SOD), catalase (CAT), glutathione peroxidase (GPx), and thioredoxin (Trx). If ROS levels further increases, then the cells undergo apoptosis [28,29,30]. To confirm this, we evaluated the transcript levels of specific antioxidant genes such as SOD2, GSTP1, and PARK7. Our results suggested that PL upregulated these antioxidant genes in a dose-dependent manner (Fig. 6c).
Alleviation of mitochondrial membrane potential by plumbagin
Many reports suggested that in increase in the level of ROS damages the mitochondrial membrane resulting in a decrease of mitochondrial membrane potential (MMP) [31, 32]. Therefore, we hypothesized that PL might deplete MMP by increasing ROS levels. In our study, 3 μM and 5 μM concentration of PL treatment decreased MMP related fluorescent intensity as compared to control (Fig. 7a). In addition, flow cytometry data suggested that peak of PL treated cells was shifted towards the left side compared to control. Here, CCCP was used as a positive control. Also, in peak of CCCP-treated cell was shifted towards the left side (Fig. 7b). Together with all these results, we concluded that PL depletes mitochondrial membrane potential in both A549 and A549GR lung cancer cell lines.
PL depletes mitochondrial membrane potential in both A549, and A549GR cell lines. a represents fluorescence images of both the cell lines after Rhodamine-123 staining, b shows flow cytometry data in which peaks shifted towards the left side in PL-treated cells as compared to control. CCCP was used as a positive control
Discussion
Nowadays, development of a novel therapeutic drug for cancer is a promising approach for all researchers. Plumbagin (PL), a yellow pigment isolated from the root of Plumbago zeylenica, which shows anticancer activities in many cancer cell lines. Together all the previous experimental reports suggested that PL triggers apoptosis by acting as a pro-oxidant [3, 24, 33, 34]. In our study, we evaluated the molecular mechanism behind anticancer potential of PL in both A549 and A549GR cell lines. Many reports have shown that PL exhibits anticancer properties by inhibiting cell migration, and inducing apoptosis [35, 36]. Firstly, we found that PL inhibited their cell growth at very low concentrations ranges from 0–10 μM. However, A549 cells showed more sensitive to PL as compared to A549GR. In addition, the colonogenic assay also suggested that PL inhibited cell growth, and also decreased cell survival. PL also affected the morphology of lung cancer cells. Treatment with 5 μM concentration of PL for 24 h, more number of floated cells were found whereas, treatment for 48 h, all cells were detached from plate surface and floated on media. From these results, it confirmed that PL possessed cytotoxic potential against both A549 and A549GR cell lines.Tumor cell migration is an important parameter to assess cancer invasion and metastasis. Therefore, in vitro scratch assay was performed to evaluate cancer cell migration. Our result showed that PL treatment significantly inhibited wound healing as compared to non-treated control cells. This data strongly evidenced that PL inhibited cell migration in both A549 and A549GR cell lines.
Induction of apoptosis is a hallmark for cancer therapy. We found that PL induced apoptosis in both A549 and A549GR cell lines in a dose-dependent manner. In PL-treated cells, maximum cells were shown in red color. But in control, all live cells were green color. In addition, nuclear staining was performed by DAPI. At 3 μM and 5 μM concentration of PL, nuclear condensation, and nuclear fragmentation appeared. Moreover, Annexin-V/PI staining data showed that after PL treatment, apoptosis was found to be increased whereas after NAC alone or in combination with PL treatment, PL-induced apoptosis was reduced. These data suggested that PL induced apoptosis in both A549 and A549GR cells through ROS generation. Furthermore, the comet assay confirmed that PL induced apoptosis by damaging DNA.
Aberrant cell proliferation in cancer is correlated with cell cycle progression [37]. Thus, effect of PL on phase distribution of the cell cycle was determined by flow cytometry study. Our study showed that PL treatment decreased the percentage of cells at G1 phase and increased the percentage of cells at S and G2/M phases. This indicated that PL induced S-G2/M arrest in both A549 and A549GR cancer cells. Furthermore, PL induced cell cycle arrest by enhancing ROS level. Result showed that PL with NAC treatment abolished the cell cycle arrest at S-G2/M phases.
Previous reports suggested that PL enhances ROS level in many cancers [18, 33, 38]. Our fluorescence microscopic and flow cytometry data also suggested that PL enhanced ROS level in both A549 and A549GR cells. In fluorescence microscopy, fluorescent intensity increased with increased concentration of PL. Moreover, flow cytometry study showed that the peak of treated cells was shifted towards right compared to control. However, NAC treatment reduced the ROS levels produced by PL in both the cell lines. It is also reported that ROS is positively correlated with DNA damage and induction of apoptosis [39]. Our results also suggested that treatment of PL with NAC reduced the apoptotic effect of PL. This confirms that excess ROS levels induces apoptosis.
Generally, there are two types of apoptotic pathways such as death receptor-dependent extrinsic pathway, and mitochondrial-dependent intrinsic pathway [40]. The mitochondrial-mediated apoptotic pathway is characterized by disruption in mitochondrial membrane results in loss of mitochondrial membrane potential, and discharge of cytochrome C from mitochondria to the cytosol. This activates Caspase 9/Caspase 3 pathway which in turn induces condensation of chromatin, and fragmentation of DNA [41]. In our study, loss of mitochondrial membrane potential (MMP) was observed after PL treatment, which is confirmed from fluorescence microscopy, and flow cytometry data. In addition, western blotting data suggested that PL enhanced the Bax and Caspase 3 levels. Together all results suggest that PL induces apoptosis by upregulating Caspase 3 levels via generating excess ROS (Fig. 8).
Diagrammatic illustration of Caspase 3 pathway activation by plumbagin. Plumbagin enhances ROS level which in turn depletes mitochondrial membrane potential and finally activates Caspase 3, consequently results in DNA fragmentation leads to cell death. However, treatment of plumbagin with NAC reduces apoptotic cell death
Conclusion
In summary, our study suggested that plumbagin showed significant inhibitory effect on the proliferation, and migration of both A549 and A549GR cell lines by arresting cell cycle at S and G2/M phases. However, PL induced cell death due to induction of mitochondrial-mediated apoptosis via ROS generation, which was reduced with NAC treatment. Therefore, more investigations are needed to explore the mechanism associated with ROS generation. Our findings suggest that PL is a best candidate for the development of novel therapeutic drug for the treatment of lung cancer.
References
Atanasov AG, Yeung AWK, Banach M (2018) Natural products for targeted therapy in precision medicine. Biotechnol Adv 36(6):1559
Mossa JS, El-Feraly FS, Muhammad I (2004) Antimycobacterial constituents from Juniperus procera, Ferula communis and Plumbago zeylanica and their in vitro synergistic activity with isonicotinic acid hydrazide. Phytother Res 18(11):934–937
Srinivas P, Gopinath G, Banerji A, Dinakar A, Srinivas G (2004) Plumbagin induces reactive oxygen species, which mediate apoptosis in human cervical cancer cells. Mol Carcin 40(4):201–211
Tilak JC, Adhikari S, Devasagayam TP (2004) Antioxidant properties of Plumbago zeylanica, an Indian medicinal plant and its active ingredient, plumbagin. Redox Rep 9(4):219–227
Ding Y, Chen ZJ, Liu S, Che D, Vetter M, Chang CH (2005) Inhibition of Nox-4 activity by plumbagin, a plant-derived bioactive naphthoquinone. J Pharm Pharmacol 57(1):111–116
Sagar S, Esau L, Moosa B, Khashab NM, Bajic VB, Kaur M (2014) Cytotoxicity and apoptosis induced by a plumbagin derivative in estrogen positive MCF-7 breast cancer cells. Anti-Cancer Agents Med Chem (Formerly Current Medicinal Chemistry-Anti-Cancer Agents) 14(1):170–180
Binoy A, Nedungadi D, Katiyar N, Bose C, Shankarappa SA, Nair BG, Mishra N (2019) Plumbagin induces paraptosis in cancer cells by disrupting the sulfhydryl homeostasis and proteasomal function. Chem Biol Interact 310:108733
Li Y-C, He S-M, He Z-X, Li M, Yang Y, Pang J-X, Zhang X, Chow K, Zhou Q, Duan W (2014) Plumbagin induces apoptotic and autophagic cell death through inhibition of the PI3K/Akt/mTOR pathway in human non-small cell lung cancer cells. Cancer Lett 344(2):239–259
Huang H, Xie H, Pan Y, Zheng K, Xia Y, Chen W (2018) Plumbagin triggers ER stress-mediated apoptosis in prostate cancer cells via induction of ROS. Cell Physiol Biochem 45(1):267–280
Cao Y-Y, Yu J, Liu T-T, Yang K-X, Yang L-Y, Chen Q, Shi F, Hao J-J, Cai Y, Wang M-R (2018) Plumbagin inhibits the proliferation and survival of esophageal cancer cells by blocking STAT3-PLK1-AKT signaling. Cell Death Dis 9(2):17
Lin Y, Chen Y, Wang S, Ma J, Peng Y, Yuan X, Lv B, Chen W, Wei Y (2018) Plumbagin induces autophagy and apoptosis of SMMC-7721 cells in vitro and in vivo. J Cell Biochem 120(6):9820–9830
Niu M, Cai W, Liu H, Chong Y, Hu W, Gao S, Shi Q, Zhou X, Liu X, Yu R (2015) Plumbagin inhibits growth of gliomas in vivo via suppression of FOXM1 expression. J Pharmacol Sci 128(3):131–136
Tripathi SK, Panda M, Biswal BK (2019) Emerging role of plumbagin: cytotoxic potential and pharmaceutical relevance towards cancer therapy. Food Chem Toxicol 125:566–582
Sakunrangsit N, Kalpongnukul N, Pisitkun T, Ketchart W (2016) Plumbagin enhances tamoxifen sensitivity and inhibits tumor invasion in endocrine resistant breast cancer through EMT regulation. Phytother Res 30(12):1968–1977
Xu T-P, Shen H, Liu L-X, Shu Y-Q (2013) Plumbagin from Plumbago Zeylanica L induces apoptosis in human non-small cell lung cancer cell lines through NF-κB inactivation. Asian Pac J Cancer Prev 14(4):2325–2331
Tripathi SK, Rengasamy KR, Biswal BK (2020) Plumbagin engenders apoptosis in lung cancer cells via caspase-9 activation and targeting mitochondrial-mediated ROS induction. Arch Pharmacal Res 43(2):242–256
Gomathinayagam R, Sowmyalakshmi S, Mardhatillah F, Kumar R, Akbarsha MA, Damodaran C (2008) Anticancer mechanism of plumbagin, a natural compound, on non-small cell lung cancer cells. Anticancer Res 28(2A):785–792
Tian L, Yin D, Ren Y, Gong C, Chen A, Guo F-J (2012) Plumbagin induces apoptosis via the p53 pathway and generation of reactive oxygen species in human osteosarcoma cells. Mol Med Rep 5(1):126–132
Lee J-H, Yeon J-H, Kim H, Roh W, Chae J, Park H-O, Kim D-M (2012) The natural anticancer agent plumbagin induces potent cytotoxicity in MCF-7 human breast cancer cells by inhibiting a PI-5 kinase for ROS generation. PLoS ONE 7(9):e45023
Pandey K, Tripathi SK, Panda M, Biswal BK (2020) Prooxidative activity of plumbagin induces apoptosis in human pancreatic ductal adenocarcinoma cells via intrinsic apoptotic pathway. Toxicol In Vitro 65:104788
Ka T, Kc S, Nair RS, Banerji A, Somasundaram V, Srinivas P (2013) Structure activity relationship of plumbagin in BRCA1 related cancer cells. Mol Carcinog 52(5):392–403
Dhawan A, Bajpayee M, Parmar D (2009) Comet assay: a reliable tool for the assessment of DNA damage in different models. Cell Biol Toxicol 25(1):5–32
Wang F, Wang Q, Zhou Z-W, Yu S-N, Pan S-T, He Z-X, Zhang X, Wang D, Yang Y-X, Yang T (2015) Plumbagin induces cell cycle arrest and autophagy and suppresses epithelial to mesenchymal transition involving PI3K/Akt/mTOR-mediated pathway in human pancreatic cancer cells. Drug Des Dev Ther 9:537
Jaiswal A, Sabarwal A, Mishra JPN, Singh RP (2018) Plumbagin induces ROS-mediated apoptosis and cell cycle arrest and inhibits EMT in human cervical carcinoma cells. RSC Adv 8(56):32022–32037
De U, Son JY, Jeon Y, Ha S-Y, Park YJ, Yoon S, Ha K-T, Choi WS, Lee BM, Kim IS (2019) Plumbagin from a tropical pitcher plant (Nepenthes alata Blanco) induces apoptotic cell death via a p53-dependent pathway in MCF-7 human breast cancer cells. Food Chem Toxicol 123:492–500
Simon H-U, Haj-Yehia A, Levi-Schaffer F (2000) Role of reactive oxygen species (ROS) in apoptosis induction. Apoptosis 5(5):415–418
Circu ML, Aw TY (2010) Reactive oxygen species, cellular redox systems, and apoptosis. Free Radical Biol Med 48(6):749–762
Gorrini C, Harris IS, Mak TW (2013) Modulation of oxidative stress as an anticancer strategy. Nat Rev Drug Discovery 12(12):931
Leone A, Roca MS, Ciardiello C, Terranova-Barberio M, Vitagliano C, Ciliberto G, Mancini R, Di Gennaro E, Bruzzese F, Budillon A (2015) Vorinostat synergizes with EGFR inhibitors in NSCLC cells by increasing ROS via up-regulation of the major mitochondrial porin VDAC1 and modulation of the c-Myc-NRF2-KEAP1 pathway. Free Radical Biol Med 89:287–299
Leone A, Roca MS, Ciardiello C, Costantini S, Budillon A (2017) Oxidative stress gene expression profile correlates with cancer patient poor prognosis: Identification of crucial pathways might select novel therapeutic approaches. Oxid Med Cell Longev. https://doi.org/10.1155/2017/2597581
Jing X-B, Cai X-B, Hu H, Chen S-Z, Chen B-M, Cai J-Y (2007) Reactive oxygen species and mitochondrial membrane potential are modulated during CDDP-induced apoptosis in EC-109 cells. Biochem Cell Biol 85(2):265–271
Marchi S, Giorgi C, Suski JM, Agnoletto C, Bononi A, Bonora M, De Marchi E, Missiroli S, Patergnani S, Poletti F (2012) Mitochondria-ros crosstalk in the control of cell death and aging. J Signal Transduct. https://doi.org/10.1155/2012/329635
Powolny AA, Singh SV (2008) Plumbagin-induced apoptosis in human prostate cancer cells is associated with modulation of cellular redox status and generation of reactive oxygen species. Pharm Res 25(9):2171–2180
Hwang GH, Ryu JM, Jeon YJ, Choi J, Han HJ, Lee Y-M, Lee S, Bae J-S, Jung J-W, Chang W (2015) The role of thioredoxin reductase and glutathione reductase in plumbagin-induced, reactive oxygen species-mediated apoptosis in cancer cell lines. Eur J Pharmacol 765:384–393
Panrit L, Plengsuriyakarn T, Martviset P, Na-Bangchang K (2018) Inhibitory activities of plumbagin on cell migration and invasion and inducing activity on cholangiocarcinoma cell apoptosis. Asian Pacific Journal of Tropical Medicine 11(7):430
Subramaniya BR, Srinivasan G, Sadullah SSM, Davis N, Subhadara LBR, Halagowder D, Sivasitambaram ND (2011) Apoptosis inducing effect of plumbagin on colonic cancer cells depends on expression of COX-2. PLoS ONE. https://doi.org/10.1371/journal.pone.0018695
Richardson JSM, Aminudin N, Malek SNA (2017) Chalepin: A compound from Ruta angustifolia L. pers exhibits cell cycle arrest at S phase, suppresses nuclear factor-kappa B (NF-κB) pathway, signal transducer and activation of transcription 3 (STAT3) phosphorylation and extrinsic apoptotic pathway in non-small cell lung cancer carcinoma (A549). Pharmacogn Mag 13(3):489
Xu K-H, Lu D-P (2010) Plumbagin induces ROS-mediated apoptosis in human promyelocytic leukemia cells in vivo. Leuk Res 34(5):658–665
Matés JM, Sánchez-Jiménez FM (2000) Role of reactive oxygen species in apoptosis: implications for cancer therapy. Int J Biochem Cell Biol 32(2):157–170
Winter E, Chiaradia LD, Silva AH, Nunes RJ, Yunes RA, Creczynski-Pasa TB (2014) Involvement of extrinsic and intrinsic apoptotic pathways together with endoplasmic reticulum stress in cell death induced by naphthylchalcones in a leukemic cell line: advantages of multi-target action. Toxicol In Vitro 28(5):769–777
Madesh M, Gr H (2001) VDAC-dependent permeabilization of the outer mitochondrial membrane by superoxide induces rapid and massive cytochrome c release. J Cell Biol 155(6):1003–1016
Funding
The work done was supported by a grant from the Department of Scienceand Technology, Science and Engineering Research Board (DST, SERB), New Delhi, India (Grant Number: ECR/2016/000792) and Department of Science and Technology, Odisha, India (Grant no-1201).
Author information
Authors and Affiliations
Contributions
MP and BKB designed the research work. MP and SKT performed the experiments. MP wrote the manuscript under the guidance of BKB and edited by all the authors.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Panda, M., Tripathi, S.K. & Biswal, B.K. Plumbagin promotes mitochondrial mediated apoptosis in gefitinib sensitive and resistant A549 lung cancer cell line through enhancing reactive oxygen species generation. Mol Biol Rep 47, 4155–4168 (2020). https://doi.org/10.1007/s11033-020-05464-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-020-05464-w