Abstract
The aim of this study was the genotypic characterization of methicillin resistance and virulence of Staphylococcus spp. from bovine mastitis cases. The study was designed to collect milk samples from 120 animals (90 lactating cows and 30 buffaloes) and screened using California mastitis test and somatic cell counts. Staphylococci were isolated on Baird-Parker, mannitol salt and identified based on their physiologically and species-specific biochemical tests. Antibiotic resistivity assay was performed using standard antibiotic disc diffusion technique for screening. On the basis of antibiograms, 26 strains were selected. Selective isolates were identified based on 16S rDNA gene sequencing. Virulence genes associated with Staphylococcus sp. viz. coa, ccr, sar, spa, clfA, ica complex, fnbA, and mecA were amplified on screened isolates. A total of 26 isolates, S. aureus, S. pasteuri, S. hominis, Micrococcus sp., and Macrococcus sp. were selected on the basis of all in vitro assay and their 16S rDNA sequences were submitted to NCBI, GenBank under the accession number KX821621 to KX821646. Out of 26 studied typed isolates, 19, 15, 14, 21, 6, 25, and 22 isolates give amplification for mecA, coa, spa, clfA, ccr, ica, fnbA, and sar genes, respectively. Four S. aureus possessed all virulence genes. Presence of methicillin resistance Staphylococci having virulence genes revealed that mastitis is a major concern nowadays affecting animal health, milk quality, and yield. Further genomic study of these isolates will provide broad new insights on virulence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Staphylococcus genus includes several pathogenic organisms; among which, Staphylococcus aureus is one of the most present etiological agent of mastitis (Chu et al. 2012; Lundberg et al. 2014). Emergence of coagulase-negative Staphylococcus sp. (CoNS) is also a concern nowadays (Aslantaş et al. 2014). These microorganisms’ pathogenicity against immune system of host animal affects animal health and milk yield which directly disturbs economy (Kelly et al. 2010).
The basis of pathogenicity depends on many virulence factors, including resistant to antibiotics, production of toxins, and many of surface proteins which help in attachment and colonization of the bacteria. These proteins act within the cellular and extracellular material of the host that affects the ability of the host to actively hinder infection by a specific immune response (Dhanawade et al. 2010).
Increasing ability of bacteria to survive in hostile environment is because of accumulation of resistance factors which has rendered the bacteria immune to a haphazard use of common antibiotics (Oliveira et al. 2006; Kumar et al. 2009). Other than this, the pathogenesis of Staphylococcus mastitis is attributed to a combination of extracellular factors and properties such as adherence and biofilm formation (Dhanawade et al. 2010; Chavhan et al. 2012).
Acquisition of resistance against different antibiotics mainly methicillin is due to staphylococcal cassette chromosome mec (SCCmec) integration, containing mecA gene (Paterson et al. 2013). The expression of mecA in MRSA allows cell wall synthesis to continue, despite inactivation of native PBPs by B-lactams (Shore et al. 2011). S. aureus also carries two site-specific recombinase genes, cassette chromosome recombinase A and B (ccrA and ccrB) or sometimes complex ccr (Goudarzi et al. 2016).
In Staphylococcus spp., presence of coagulase as a coa gene, clumping factor (clfA), intracellular adhesion protein (ica), and fibronectin-binding proteins (fnbA) mediate bacterial adherence states pathogenicity of a strain (Feßler et al. 2010; Nemeghaire et al. 2014). Products of icaABCD complex synthesize polysaccharide intercellular adhesion which leads organisms to form biofilms (Barakat and Nabil 2016). Staphylococcal accessory regulator (sar) helps to regulate biofilm formation and protein A (spa) gene segment encoding the immunoglobulin G binding region is one of the vital virulence factors (Hata et al. 2010).
The work was designed to study the virulence genes in Staphylococcus spp. associated with mastitis.
Materials and methods
Milk sample collection
A total of 120 animals were screened for mastitis based on California mastitis test (CMT), somatic cell counts (SCC), pH of milk were determined (Bhutto et al. 2012).
Milk samples were collected and proceeded as described in our previous study (Patel et al. 2017a, b); in brief, udder were wiped with 80% ethyl alcohol, wiped and few drops of milk was discarded initially. Afterwards, in a 50-ml falcon tube, the sample was collected and proceeded further (Bhatt et al. 2011; Patel et al. 2017a, b). Simultaneously, CMT was executed on site and on the basis of CMT score samples were collected and proceeded for somatic cell count, pH measurement, and bacteriological examination (Bhutto et al. 2012).
Isolation of staphylococci from milk samples
We used Baird-Parker agar base (Himedia, Catalog No. M043, India) for screening and mannitol salt agar (Himedia Catalog No. MH118, India) for differentiation and selection of Staphylococcus spp. as described by (Le Maréchal et al. 2011; De Oliveira et al. 2011). Confirmed isolates were cultured in Luria broth (Himedia M575, India) and cultures were preserved in 25% glycerol (Himedia, Catalog No. MB060, India) and stored at − 20 °C (Blue-star).
Determination of antibiotic susceptibility of isolates
In vitro antibiotic susceptibility of a total of 179 Staphylococcus spp. was evaluated against 20 different antibiotics (HiMedia, India) which include amoxicillin (10 mcg/disc), ampicillin (10 mcg/disc), cefotaxime (30 mcg/disc), chloramphenicol (30 mcg/disc), ciprofloxacin (5 mcg/disc), cloxacillin (10 mcg/disc), enrofloxacin (10 mcg/disc), erythromycin (15 mcg/disc), gentamicin (10 mcg/disc), kanamycin (30 mcg/disc), meropenem (10 mcg/disc), methicillin (5 mcg/disc), nalidixic acid (30 mcg/disc), ofloxacin (5 mcg/disc), oxacillin (1 mcg/disc), penicillin-G (10 mcg/disc), rifampicin (5 mcg/disc), streptomycin (10 mcg/disc), tetracycline (30 mcg/disc), and vancomycin (30 mcg/disc) using disc diffusion method according to the National Committee of Clinical Laboratory Standards (NCCLS) (Shitrit et al. 2015).
Identification of bacteria based on 16S rDNA gene sequencing and phylogenetic analysis
Isolates which showed resistance against most of the antibiotic tested were selected for further study. Genomic DNA was isolated by following the proteinase K - SDS method manually by little modification as described (Patel et al. 2016). Isolated DNA samples were checked for quality and quantity using agarose gel electrophoresis (Bio-Rad, USA) and NanoDrop spectrophotometer (ND-1000, Thermo-Scientific, USA), respectively. 16S rDNA gene was amplified using universal primer 8F and 518R (Carroll et al. 2013), followed by Sanger sequencing. The sequences obtained were submitted to NCBI GenBank. Phylogenetic analysis was conducted by MEGA 7 software using the UPGMA statistical method. Test of phylogeny was done using bootstraps method obtained from 1000 replicates.
Detection of virulence genes
We selected a total of nine genes which are prevalent and confer pathogenicity to Staphylococcus sp. The primers were designed using primer3 using MRSA252, SA RF122, and SA 8325 as a reference strain (Haran et al. 2012; Luini et al. 2015). Primers were synthesized at Eurofins Genomics India Pvt. Ltd., Bengaluru. The specific primers with sequences are shown in Table 1.
The target genes were amplified using Applied Biosystems 2720 thermal cycler. The 25 μl PCR mixture contain 1 μl of DNA template (50–70 ng), 2.5 μl PCR Taq Buffer with MgCl2 (Genei), 2.5 μl DNTP mix (2.5 mM each) (Genei, Bengaluru), 0.5 μl genomic DNA polymerase (Sigma-Aldrich, Germany), 1 μl forward primer (10 pM/μl), and 1 μl reverse primer (10 pM/μl) sterilized milli-Q water to make up the reaction volume (Chavhan et al. 2012). PCR conditions for each gene amplification was standardized by initial denaturation at 95 °C for 5 min, denaturation at 95 °C for 30 s, annealing by varying Tm, extension at 72 °C for 45 s with 25 cycles, and final extension at 72 °C for 10 min. Finalized annealing temperature is shown in Table 1 . A negative control with each of the reaction components except template DNA and positive control (Accession No: KR028445) with the genomic DNA from S. aureus and Staphylococcus sp. was taken for each gene (Darwish and Asfour 2013; Patel et al. 2016). The PCR products were visualized on 1.5% agarose gel along with the molecular markers of definite length. The gel was electrophoresed in 2 x Tris-borate buffer at 70 V for 1.5 h and documentation was done using the Gel Doc system (Bio-Rad, USA).
Results
Bacterial strains
A total of 193 Staphylococcus spp. were isolated from 180 quarters milk samples containing somatic cells higher than 500 cells/μl, pH above 6.8, and CMT score 1 or 2 (Bhutto et al. 2012). All the isolates showed black color colony on Baird-Parker medium containing rabbit plasma and out of 193 isolates; 139 yielded yellow color on mannitol salt differential media due to fermentation of mannitol and 40 with no change in color. These isolates were phenotypically confirmed to be S. aureus and Staphylococcus sp. by performing various biochemical assays as per Bergey’s manual of determinative bacteriology.
Antibiotic susceptibility of isolates
Qualitative antibiotic susceptibility test (ABST) against 179 Staphylococcus spp. comprising 139 S. aureus and 40 Staphylococcus spp. was achieved. Resistance against methicillin in 31 (22.30%) out of 139 S. aureus and in 17 (42.5%) out of 40 Staphylococcus spp. was observed. A total of 26 (14.53%) isolates were found resistant to more than 12–14 antibiotics thus used in further study.
Molecular identification and phylogenetic analysis
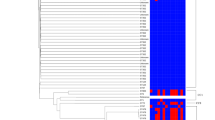
On the basis of antibiograms, 26 isolates were further selected for molecular identification using 16S rDNA gene amplification. Submitted sequences were assigned under accession number KX821628 to KX821638 for S. aureus (11), KX821621 to KX821627 for coagulase-negative Staphylococcus sp. (07), and KX821639 to KX821646 (08) for Micrococcus sp. including two Macrococcus spp. The phylogenetic tree generated from the 16S rDNA gene sequence of the Staphylococcus strains/isolates included in this study showed, as expected, that all Micrococcus spp., S. hominis and S. pasteuri were clustered in individual clade, whereas S. aureus were clustered individual and also found closely related with Macrococcus sp. in some strains (Fig. 1).
Virulence gene detection
Nine eminent virulence genes were amplified using gene-specific primers. Results revealed that all the resistant genes were present in the isolates, but not all nine in each isolate. Amplification of genomic DNA of all 26 typed isolates with antibiotic resistivity gave positive amplification for mecA gene resulted in the amplification of a fragment of approx. 1900 bp in 19 isolates; no amplification was observed in the rest of the isolates. Among the 26 isolates, 15 showed amplification of 850 bp fragment for coa gene which includes all S. aureus and four Micrococcus spp., 14 isolates to carry spa gene having size of 920 bp and 21 isolates were found positive for clfA gene having 980 bp size. Amplification of ccr gene with 425 bp amplicon size was found in 04 coagulase-negative Staphylococcus spp. (CNS) and 2 MRSA. Biofilm associated virulence gene amplification was observed in most of the isolates. Twenty-five isolates were found ica (icaA of approx. 550 bp and icaD of approx. 330 bp) and fnbA (520 bp) positive, while 22 isolates were found positive for sar gene of 250 bp amplified product (Fig. 2a–i).
Though the amplification of all nine genes was observed but not consistently in all of the isolates, different genes were existing in different isolates. However, four of the 11 S. aureus possessed all virulence genes.
Discussion
Virulence factors of S. aureus and coagulase-negative Staphylococcus sp. (CoNS) enable the bacteria to attach, colonize, invade, survive, and infect the host which directly intrudes immunity. In this study, we investigated virulence determinants in methicillin resistance Staphylococcal strains isolated from the milk having higher SCC (> 500 cells/μl) and CMT positive. Methicillin-resistant S. aureus are considered resistant against β-lactams antibiotics which are widely used to treat and prevent mastitis in dairy cows. Emergence of this resistant is due to irrational use of antibiotics for treatment (Chavhan et al. 2012).
Phenotypic resistance by ABST against methicillin was found in 31 (22.30%) out of 139 S. aureus, which is in accordance with detailed study of past 13 years on clinical S. aureus isolates by authors where around 22% MRSA was observed among studied isolates in UK, Slovenia, Belgium, Finland, and France (Denis et al. 2014). A study from India revealed 30% MRSA from their studied 323 strains by in vitro ABST assay, which is 8% higher than our study (Debnath and Chikkaswamy 2015).
coa gene was found to be present in all the isolates of S. aureus and Micrococcus sp. and absent in remained strains; which is confirmatory of phenotypically performed biochemical assay to distinguish coagulase-positive and negative strains. Coagulase-negative Staphylococcus spp. (CoNS) are also becoming more prevailing with mastitis in the population of mixed animals. Two different sized coa amplified product is observed in few isolates, which states that S. aureus is having two different regions for coa. However, two bands of coa gene amplicons have also been reported by various authors (Al-Ashmawy et al. 2016; Nagaraju and Raju 2017).
Presence of mecA gene in S. aureus is the only known way to spread the gene by horizontal gene transfer mechanism. In this study, mecA gene encoding PBP2a (penicillin-binding protein 2a) was detected in 11 S. aureus can be confirmatory termed as MRSA and 07 in coagulase-negative Staphylococcus sp. termed as CNS. Emergence of such methicillin-resistant CNS is due to excessive use of antibiotics in treatment of Staphylococcus spp. A group of scientists from Brazil also observed mecA-positive CNS strains which were classified as methicillin-resistant by both the MIC and disc diffusion method (Fernandes Dos Santos et al. 2015). Resistance against this antibiotic is due to changes in penicillin-binding proteins (PBPs) other than PBP2 thus giving no activity against methicillin. In our study, the mecA gene was not detected in seven strains containing six Micrococcus spp., which did not show phenotypic methicillin resistance.
A genetic element that encoded methicillin resistance and carried unique site-specific recombinase designated as cassette chromosome recombinase (ccr) was identified in six of the 26 studied isolates containing 4 CNS and 2 MRSA having mecA and can be designated as the staphylococcal cassette chromosome mec (SCCmec) on the basis of studies (Chongtrakool et al. 2006; Aslantaş et al. 2014; Harrison et al. 2014; McManus et al. 2015).
Biofilm forming ability of a pathogenic strain against stress and inapt environment is considered to be one of the important virulence factors. S. aureus adhere to the extracellular matrix and cell components that are internalized into the mammary gland epithelial cells (Li et al. 2012). Like fibrinogen-binding proteins (fnbpA), clumping factor A (clfA) and clumping factor B (clfB) are important S. aureus bacterial adhesins: they contribute to initiate infection. Clumping factor A (clfA) is the major virulence factor responsible for clumping of S. aureus and all S. aureus clinical strains carry the clfA gene.
The ability of S. aureus to adhere to extracellular matrix proteins is essential for the colonization and establishment of infections and S. aureus possesses various adhesion genes. In one of the study on virulence factors, researchers found clfA (77.1%) and fnbpA (94.3%) (Wang et al. 2016). Similarly, we observed in this study too that clfA (80.76%) and fnbpA (96.15%) were found to be prevalent (Wang et al. 2016). Similarly, intracellular adhesion representing genes, icaA and icaD were also present in 96.15% of the isolates which is in accordance with a Brazilian study (Marques et al. 2017).
Staphylococcal accessory regulator (sar) protein is responsible for growth of strain during exponential phase that leaves it to form a layer to defend against stress condition so called as biofilm. Few studies also suggest that sar may also incidentally regulate Staphylococcal protein A (spa) production (Bar-Gal et al. 2015). In our study, 53.8 and 84.61% isolates were found positive for spa and sar genes, respectively which states that in some cases spa is not regulated by sar gene (Morrison et al. 2012; Brackman et al. 2016).
Use of β-lactams, lincosamide, and macrolides as a therapeutic purpose is not eternally effective, as the prevalence of antibiotic resistance in various CoNS causing mastitis in cattle. Therefore, it is essential to evaluate the susceptibility of individual CoNS species against antimicrobials before applying for therapeutic application to treat mastitis. Few trials have been also applied by adding citric acid in lesser amount with beta lactum antibiotics against MRSA (Chandak et al. 2014). Moreover, the PCR technique to amplify the particular gene is not sufficient to confirm the antimicrobial resistivity of MRSA and CoNS but it is an insight into bacteria causing mastitis. Further genomic level study can help to understand the biological and functional processes of virulence gene and its mode of actions.
Conclusion
Presence of virulence factors including antibiotic resistivity in mastitis causing Staphylococcus spp. is an alarming spot for veterinarians, as several sources are there for spreading of microorganisms including human activities. Judicious use of antimicrobials for treatment of mastitis by eliminating the effect of pathogenic microbes is essential to control the emergence and spread of resistance against antibiotics. Antibiotic resistance and spreading of virulence have emerged in the last two decades shows alarming status in the field of medicine. Detailed genomic evaluation of particular resistant strain having virulent factors may possess a great scope for future development by targeting treatment purpose.
References
Al-Ashmawy MA, Sallam KI, Abd-Elghany SM et al (2016) Prevalence, molecular characterization, and antimicrobial susceptibility of methicillin-resistant Staphylococcus aureus isolated from milk and dairy products. Foodborne Pathog Dis 13:156–162. https://doi.org/10.1089/fpd.2015.2038
Aslantaş Ö, Yılmaz MA, Yılmaz EŞ, Kurekci C (2014) Antimicrobial susceptibility pattern and SCCmec types of methicillin-resistant coagulase-negative staphylococci from subclinical bovine mastitis in Hatay. Turkey Bull Vet Inst Pulawy. https://doi.org/10.2478/bvip-2014-0087
Barakat GI, Nabil YM (2016) Correlation of mupirocin resistance with biofilm production in methicillin-resistant Staphylococcus aureus from surgical site infections in a tertiary centre, Egypt. J Glob Antimicrob Resist 4:16–20. https://doi.org/10.1016/j.jgar.2015.11.010
Bar-Gal GK, Blum SE, Hadas L et al (2015) Host-specificity of Staphylococcus aureus causing intramammary infections in dairy animals assessed by genotyping and virulence genes. Vet Microbiol 176:143–154. https://doi.org/10.1016/j.vetmic.2015.01.007
Bhatt VD, Patel MS, Joshi CG, Kunjadia A (2011) Identification and antibiogram of microbes associated with bovine mastitis. Anim Biotechnol 22:163–169. https://doi.org/10.1080/10495398.2011.570132
Bhutto AL, Murray RD, Woldehiwet Z (2012) California mastitis test scores as indicators of subclinical intra-mammary infections at the end of lactation in dairy cows. Res Vet Sci 92:13–17. https://doi.org/10.1016/j.rvsc.2010.10.006
Brackman G, Breyne K, De Rycke R et al (2016) The quorum sensing inhibitor hamamelitannin increases antibiotic susceptibility of Staphylococcus aureus biofilms by affecting peptidoglycan biosynthesis and eDNA release. Sci Rep 6:20321. https://doi.org/10.1038/srep20321
Carroll IM, Ringel-Kulka T, Ferrier L et al (2013) Fecal protease activity is associated with compositional alterations in the intestinal microbiota. PLoS One 8:1–10. https://doi.org/10.1371/journal.pone.0078017
Chandak NA, Deshmukh SR, Wadher B (2014) J. drug prescribing pattern of antibiotics for treatment of methicillin resistant staphylococcus aureus. Indian Medical Gazette 148(12):463–468
Chavhan SK, Kalorey DR, Nagdive AA et al (2012) Molecular characterization of intercellular adhesion gene in Staphylococcus aureus isolated from bovine mastitic milk. Trop Anim Health Prod 44:247–252. https://doi.org/10.1007/s11250-011-0009-9
Chongtrakool P, Ito T, Ma XX et al (2006) Staphylococcal cassette chromosome mec ( SCCmec ) typing of methicillin-resistant Staphylococcus aureus strains isolated in 11 Asian countries: a proposal for a new nomenclature for SCCmec elements. Antimicrob Agents Chemother 50:1001–1012. https://doi.org/10.1128/AAC.50.3.1001
Chu C, Yu C, Lee Y, Su Y (2012) Genetically divergent methicillin-resistant Staphylococcus aureus and sec-dependent mastitis of dairy goats in Taiwan. BMC Vet Res 8:39. https://doi.org/10.1186/1746-6148-8-39
Darwish SF, Asfour HAE (2013) Investigation of biofilm forming ability in staphylococci causing bovine mastitis using phenotypic and genotypic assays. Sci World J. https://doi.org/10.1155/2013/378492
De Oliveira LP, Santana L, Silva VC, Cirqueira MG (2011) Study of Staphylococcus aureus in raw and pasteurized milk consumed in the Reconcavo area of the state of Bahia, Brazil. J Food Process Technology. 2:128. https://doi.org/10.4172/2157-7110.1000128
Debnath A, Chikkaswamy BK (2015) Antibiogram and susceptibility pattern of methicillin-resistant Staphylococcus aureus collected from various clinical samples in Bengaluru. Asian J Pharm Clin Res 8:260–264
Denis O, Nonhoff C, Dowzicky MJ (2014) Antimicrobial susceptibility among gram-positive and gram-negative isolates collected in Europe between 2004 and 2010. J Glob Antimicrob Resist 2:155–161. https://doi.org/10.1016/j.jgar.2014.05.001
Dhanawade NB, Kalorey DR, Srinivasan R et al (2010) Detection of intercellular adhesion genes and biofilm production in Staphylococcus aureus isolated from bovine subclinical mastitis. Vet Res Commun 34:81–89. https://doi.org/10.1007/s11259-009-9326-0
Fernandes Dos Santos F, Mendonca LC, Reis DR et al (2015) Presence of mecA-positive multidrug-resistant Staphylococcus epidermidis in bovine milk samples in Brazil. J Dairy Sci 99:1374–1382. https://doi.org/10.3168/jds.2015-9931
Feßler A, Scott C, Kadlec K et al (2010) Characterization of methicillin-resistant Staphylococcus aureus ST398 from cases of bovine mastitis. J Antimicrob Chemother 65:619–625. https://doi.org/10.1093/jac/dkq021
Goudarzi M, Goudarzi H, Marie A, et al (2016) Molecular characterization of methicillin resistant Staphylococcus aureus strains isolated from intensive care units in Iran: ST22-SCC mec IV/t790 emerges as the major clone. Plos One 969:1–13. https://doi.org/10.1371/journal.pone.0155529
Haran KP, Godden SM, Boxrud D et al (2012) Prevalence and characterization of Staphylococcus aureus, including methicillin-resistant Staphylococcus aureus, isolated from bulk tank milk from Minnesota dairy farms. J Clin Microbiol 50:688–695. https://doi.org/10.1128/JCM.05214-11
Harrison EM, Paterson GK, Holden MTG et al (2014) A novel hybrid SCCmec-mecC region in Staphylococcus sciuri. J Antimicrob Chemother 69:911–918. https://doi.org/10.1093/jac/dkt452
Hata E, Katsuda K, Kobayashi H et al (2010) Genetic variation among Staphylococcus aureus strains from bovine milk and their relevance to methicillin-resistant isolates from humans. J Clin Microbiol 48:2130–2139. https://doi.org/10.1128/JCM.01940-09
Kelly WJ, Leahy SC, Altermann E et al (2010) The glycobiome of the rumen bacterium butyrivibrio proteoclasticus B316T highlights adaptation to a polysaccharide-rich environment. PLoS One. https://doi.org/10.1371/journal.pone.0011942
Kumar JD, Negi YK, Gaur A, Khanna D (2009) Detection of virulence genes in Staphylococcus aureus isolated from paper currency. Int J Infect Dis 13:450–455. https://doi.org/10.1016/j.ijid.2009.02.020
Le Maréchal C, Jardin J, Jan G et al (2011) Staphylococcus aureus seroproteomes discriminate ruminant isolates causing mild or severe mastitis. Vet Res 42:35. https://doi.org/10.1186/1297-9716-42-35
Li L, Yang H, Liu D, et al (2012) Analysis of biofilm formation and associated gene detection in Staphylococcus isolates from bovine mastitis. 11:2113–2118. doi: https://doi.org/10.5897/AJB11.081
Luini M, Cremonesi P, Magro G et al (2015) Methicillin-resistant Staphylococcus aureus (MRSA) is associated with low within-herd prevalence of intra-mammary infections in dairy cows: genotyping of isolates. Vet Microbiol 178:270–274. https://doi.org/10.1016/j.vetmic.2015.05.010
Lundberg Å, Aspán A, Nyman A, Helle EU, Karin PW (2014) Associations between bacterial genotype and outcome of bovine clinical Staphylococcus aureus mastitis. Acta Veterinaria Scandinavica 56(2):1–8
Marques VF, da Motta CC, da Silva Soares B et al (2017) Biofilm production and beta-lactamic resistance in Brazilian Staphylococcus aureus isolates from bovine mastitis. Brazilian J Microbiol 48:118–124. https://doi.org/10.1016/j.bjm.2016.10.001
McManus BA, Coleman DC, Deasy EC et al (2015) Comparative genotypes, staphylococcal cassette chromosome mec (SCCmec) genes and antimicrobial resistance amongst Staphylococcus epidermidis and Staphylococcus haemolyticus isolates from infections in humans and companion animals. PLoS One 10:e0138079. https://doi.org/10.1371/journal.pone.0138079
Morrison JM, Anderson KL, Beenken KE et al (2012) The staphylococcal accessory regulator, SarA, is an RNA-binding protein that modulates the mRNA turnover properties of late-exponential and stationary phase Staphylococcus aureus cells. Front Cell Infect Microbiol 2:26. https://doi.org/10.3389/fcimb.2012.00026
Nagaraju U, Raju B (2017) Methicillin-resistant Staphylococcus aureus in community-acquired pyoderma in children in South India. Indian J Paediatr Dermatol 18:14. https://doi.org/10.4103/2319-7250.188425
Nemeghaire S, Argudín MA, Haesebrouck F, Butaye P (2014) Epidemiology and molecular characterization of methicillin-resistant Staphylococcus aureus nasal carriage isolates from bovines. BMC Vet Res 10:153. https://doi.org/10.1186/1746-6148-10-153
Oliveira M, Bexiga R, Nunes SF, et al (2006) Biofilm-forming ability profiling of Staphylococcus aureus and Staphylococcus epidermidis mastitis isolates Vet Microbiol 118:133–140. https://doi.org/10.1016/j.vetmic.2006.07.008
Patel S, Vaidya Y, Joshi C, Kunjadia A (2016) Culture-dependent assessment of bacterial diversity from human milk with lactational mastitis. Comp Clin Path 25:437–443. https://doi.org/10.1007/s00580-015-2205-x
Patel K, Joshi C, Kunjadiya A (2017a) Isolation and molecular identification of Staphylococcus spp. from bovine mastitis milk samples. Int J Adv Res 5:2320–5407. https://doi.org/10.21474/IJAR01/4818
Patel RJ, Pandit RJ, Bhatt VD et al (2017b) Metagenomic approach to study the bacterial community in clinical and subclinical mastitis in buffalo. Meta Gene 12:4–12. https://doi.org/10.1016/j.mgene.2016.12.014
Paterson GK, Harrison EM, Craven EF et al (2013) Incidence and characterisation of methicillin-resistant Staphylococcus aureus (MRSA) from nasal colonisation in participants attending a cattle veterinary conference in the UK. PLoS One 8:e68463. https://doi.org/10.1371/journal.pone.0068463
Shitrit P, Openhaim M, Reisfeld S et al (2015) Characteristics of SCCmec IV and V methicillin-resistant Staphylococcus aureus ( MRSA ) in Israel. Isr Med Assoc J 17:470–475
Shore AC, Deasy EC, Slickers P et al (2011) Detection of staphylococcal cassette chromosome mec type XI carrying highly divergent mecA, mecI, mecR1, blaZ, and ccr genes in human clinical isolates of clonal complex 130 methicillin-resistant Staphylococcus aureus. Antimicrob Agents Chemother 55:3765–3773. https://doi.org/10.1128/AAC.00187-11
Wang D, Zhang L, Zhou X et al (2016) Antimicrobial susceptibility, virulence genes, and randomly amplified polymorphic DNA analysis of Staphylococcus aureus recovered from bovine mastitis in Ningxia, China. J Dairy Sci 99:9560–9569. https://doi.org/10.3168/jds.2016-11625
Acknowledgements
Authors are gratefully thanking the substantial support of dairy farmers of Kheda and Anand districts and acknowledge SICART, Charutar Vidya Mandal for providing support and Animal Biotechnology department, Veterinary College of Science and A.H. for providing platform to conduct experiments.
Funding
The authors received no financial support for the research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
No need of ethical approval.
Conflict of interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Patel, K., Joshi, C., Nauriyal, D. et al. Genotypic identification of methicillin resistance and virulence factors in Staphylococcus spp. from bovine mastitis milk. Comp Clin Pathol 26, 1355–1361 (2017). https://doi.org/10.1007/s00580-017-2540-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00580-017-2540-1