Abstract
Bone is a complex, constantly changing organ comprised of mineralized hard tissue. This important structural component of vertebrate’s body serves a variety of functions. Healthy bone system is essential for lifelong execution of these functions. Millions of people worldwide suffer from bone defects due to various reasons, including trauma, tumor, bone diseases, congenital defects, and aging. These defects are increasingly becoming the majority of the clinical cases in orthopedics. For all the aforementioned cases in which the normal process of bone regeneration is either impaired or simply insufficient, there are currently a number of treatment methods available which can be used either alone or in combination for the enhancement of bone healing and regeneration. Accordingly, bone repair has been the focus of many research activities related to clinical therapies. The traditional bone repair procedure widely used in current era involves the use of bone-grafting methods such as autografts, allografts, and xenografts; however, these methods are associated with number of limitations. Therefore, to overcome these problems, tissue engineering as a new and developing option had been introduced recently. In order to provide ideal bone substitutes, a wide range of biomaterials and synthetic bone substitutes are available depending on the goal, each has advantages and disadvantages. The combined use of different bone substitutes together with healing promotive factors, stem cells, gene therapy, and more recently, three-dimensional printing of tissue-engineered constructs may open new insights in bone regeneration in near future. In this review, we describe developments and recognized properties of some of the most utilized materials in bone regenerative medicine heretofore. It may be concluded that presently strong requirements are still to be met in the repair and regeneration of bone defects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
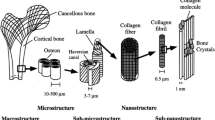
The skeleton forms the basic frame that supports the locomotory apparatus and forms a mechanical point of view consists largely of a series of lever arms designed to contract the force of gravity and to constrain and direct the forces of muscular contraction (Sarkar and Lee 2015). Bone has several functions which include protection of vital organs, regulation of calcium and phosphorus metabolism, and hematopoiesis (Liao et al. 2011; Clarke 2008; De Baat et al. 2005; McMahon et al. 2013). It also serves as a reservoir of cytokines and growth factors (Liao et al. 2011; Clarke 2008; De Baat et al. 2005; McMahon et al. 2013). Healthy bone system is essential for lifelong execution of these functions (Liao et al. 2011). According to Wolff’s law, long bones change shape to accommodate stresses placed on them; this is called “modeling” (Clarke 2008; De Baat et al. 2005). Bone goes through remodeling concurrently, the process by which bone is renewed to maintain bone strength and mineral homeostasis (Clarke 2008; De Baat et al. 2005). In this process, osteoclasts resorb old bone and osteoblasts replace it with new bone (Liao et al. 2011; Clarke 2008; Buckwalter and Cooper 1987; Zigdon-Giladi et al. 2015). Dynamic balance between these two processes maintains bone structure; therefore, impairment of any of these processes results in bone abnormalities such as fracture, osteoporosis, and osteoarthritis (Liao et al. 2011; Clarke 2008; Buckwalter and Cooper 1987; Zigdon-Giladi et al. 2015). In USA, bone injury occurs to seven million people every year (Wang et al. 2013). Among these, fracture is one of the most important bone injuries that may be defined as a disruption in the continuity and integrity of a bone due to various reasons such as car accidents and falls (Denny and Butterworth 2000). Fracture is classified as complete and incomplete (Denny and Butterworth 2000). A complete fracture is one in which there is total disruption of the continuity of the bone and usually marked displacement of the fragments (Denny and Butterworth 2000). An incomplete fracture is one in which partial continuity of the bone is maintained as in the greenstick fractures of young animals or fissure fractures in mature animals (Denny and Butterworth 2000). Following a fracture, the healing process is initiated (Sarkar and Lee 2015; Kovach et al. 2015; Marsell and Einhorn 2011; Dimitriou et al. 2011). Healing of bone defects in adults closely resembles bone formation during organogenesis (Sarkar and Lee 2015; Marsell and Einhorn 2011; Dimitriou et al. 2011). Fractured bone heals through direct and indirect pathways. Direct pathway is achieved via intramembranous ossification, whereas indirect (secondary) fracture healing consists of both endochondral and intramembranous ossification and is the most common form of fracture healing (Sarkar and Lee 2015; Marsell and Einhorn 2011; Dimitriou et al. 2011). Soon after the bone injury, an acute inflammatory response initiates locally including the production and release of important chemical mediators leading to clot formation (Sarkar and Lee 2015; Kovach et al. 2015; Marsell and Einhorn 2011). The combination of collagen fibers and mineralized osteoids forms the primary soft cartilaginous callus later; gradually, vascularization and calcification lead to ossification of this primary structure and finally remodeling occurs to restore normal bone structure (Sarkar and Lee 2015; Kovach et al. 2015; Marsell and Einhorn 2011). Unlike other tissues, the bone can regenerate and repair itself, this inherent potential causes bone injuries and fractures to heal without scar formation (Sarkar and Lee 2015; Marsell and Einhorn 2011; Dimitriou et al. 2011; Oryan et al. 2014a). Nevertheless, pathological fractures, arthritis, and massive bone defects due to trauma and bone tumor resections may lead to larger bone defects that may have a compromised healing. This biologic process fails or may be insufficient leading to delayed union or non-union of the fracture (Wang et al. 2013; Kovach et al. 2015; Oryan et al. 2014a; Hannouche et al. 2001; Balmayor and van Griensven 2015). It is estimated that, of the 7.9 million fractures sustained in the USA each year, 5 to 20% result in delayed or impaired healing requiring therapeutic intervention (Kovach et al. 2015). However, there are complex clinical conditions in which bone regeneration is required in large quantity, such as for skeletal reconstruction of large bone defects created by trauma, infection, tumor resection, and skeletal abnormalities (Clarke 2008; De Baat et al. 2005; Zigdon-Giladi et al. 2015; Wang et al. 2013; Kovach et al. 2015; Marsell and Einhorn 2011; Dimitriou et al. 2011; Oryan et al. 2014a; Navarro et al. 2008). In these cases, surgery is essential in order to fill the defect with bone grafts or synthetic biomaterials (Clarke 2008; De Baat et al. 2005; Zigdon-Giladi et al. 2015; Wang et al. 2013; Kovach et al. 2015; Marsell and Einhorn 2011; Dimitriou et al. 2011; Oryan et al. 2014a; Navarro et al. 2008). Bone-grafting frequency is indeed the second most frequent tissue transplantation worldwide, coming right after blood transfusion (Oryan et al. 2014a; Campana et al. 2014). Over two million bone-grafting procedures are performed every year, with more than 500,000 implanted in the USA alone (Oryan et al. 2014a; Campana et al. 2014). A bone graft is defined as an implanted material that promotes bone healing alone or in combination with other materials (Oryan et al. 2014a). The selection of an ideal bone graft relies on several factors such as tissue viability, defect size, graft size, shape and volume, biomechanical characteristics, graft handling cost, ethical issues, biological characteristics, and associated complications (Oryan et al. 2014a).
An ideal bone graft material should induce osteogenesis, osteoinduction, osteoconduction, and osseointegration (Oryan et al. 2014a). The materials used in bone grafting can be divided into several major categories, including autografts, allografts, and xenografts (Oryan et al. 2014a). Using natural and synthetic biomaterials is another choice to repair a bone defect (Oryan et al. 2014a; Campana et al. 2014). Repair of bone defects using implanted material commenced millennia ago; ancient Peruvian and Egyptian societies used implants to heal bone defects (Sarkar and Lee 2015). The modern era of bone substitutes commenced with the attempt of the Dutch surgeon Job van Meekeren to repair a soldier’s broken skull using a skull fragment from a dog (Sarkar and Lee 2015). Generally, a bone substitute can be defined as “a synthetic, inorganic, or biologically organic combination which can be inserted for the treatment of a bone defect instead of autogenous or allogenous bone” (Campana et al. 2014). A wide variety of bone substitutes have been employed over the past 50 years (Campana et al. 2014). Bone substitutes must meet stringent requirements; they must be non-toxic, mechanically sound, biocompatible, and not evoke any adverse inflammatory response. They should be osteoconductive and osteoinductive, have a three-dimensional (3D) porous structure, and exhibit optimum biodegradation. They should be easily molded into the bone defect within a short-setting time and allow easy fabrication into the final preforms. The ideal bone substitute should be possibly traceable in vivo; to this aim, radiolucency is ideal to allow optimal radiographic assessment. Also, they should be thermally non-conductive, sterilizable, and readily available at a reasonable cost (Sarkar and Lee 2015; Campana et al. 2014). In this report, we will review some of the available options in bone repair and regeneration including different types of bone grafts and some of the most used biomaterials, their characteristics, advantages, and disadvantages. Moreover, we will highlight the application of tissue engineering techniques to overcome the limitations of the grafts and to enhance bone regeneration.
Grafts
Bone grafting was introduced into general surgical practice early in the twentieth century, and the principles of grafting have been well established for more than 75 years (Piermattei et al. 2006). Bone grafts may be used to bridge major defects or to establish the continuity of a long bone, to aid in fusion of joints, to fill cavities or defects, and to promote bone union in delayed union or non-union fractures (Millis and Martinez 2003). Bone grafting is now a well-established, commonly performed procedure to augment bone regeneration in a variety of veterinary orthopedic surgeries, with autologous bone being considered as the “gold standard” bone-grafting material (Dimitriou et al. 2011; Millis and Martinez 2003). Autograft refers to the transfer of tissue from one site to another in the same animal (Denny and Butterworth 2000). It is the safest and most effective grafting procedure since it contains patient’s own bone-growing cells and proteins to enhance osteogenesis and osteoinduction, respectively (Gomez-Barrena et al. 2015). Bone can be harvested from non-essential bones, such as the iliac crest or the fibula, scapula, radius, the chin, the ribs, the mandible, and even parts of the skull. Autogenous bone possesses all the properties essential for bone formation: it is osteoconductive and osteoinductive, and it houses growth factors and osteogenic cells with no associated immune- or infective-related risks; therefore, this method has been suggested as the gold standard (Sarkar and Lee 2015; Zigdon-Giladi et al. 2015; Dimitriou et al. 2011; Oryan et al. 2014a; Campana et al. 2014). Nevertheless, this method also has some limitations such as limited availability, difficulties in harvesting of adequate quantities of bone, the need for general sedation or anesthesia, need for further surgery, longer operative time, postoperative pain and complications, likelihood of blood loss or hematomas, infection, fracture, neurovascular injury, and cosmetic deformity (Sarkar and Lee 2015; Liao et al. 2011; McMahon et al. 2013; Dimitriou et al. 2011; Oryan et al. 2014a; Campana et al. 2014). According to Barnes et al. investigation in 2015, the combination of autogenous cancellous bone graft and extracorporeal shock wave therapy may lead to increased radiographic density of the osteotomy gap in the first 4 weeks after surgery (Barnes et al. 2015). The next solution is allograft. Allograft refers to the transfer of tissue taken from one animal and transplanted to another animal of the same species (Denny and Butterworth 2000). Allografts have lower donor-associated problems, but some of the most important limitations of such transplants are potential antigenic response and disease transmission, lack of osteogenic properties, variable osteoinductivity, limited supply, laborious procedure (tissue processing, harvesting) and loss of biologic and mechanical properties due to its processing (sterilization by gamma irradiation), non-availability worldwide due to religious and financial concerns, and increased cost (Oryan et al. 2014a; Campana et al. 2014). Shafiei et al. compared fresh cortical autograft and fresh cortical allograft, and they reported that autograft was radiographically but not biomechanically and histopathologically superior to allograft (Shafiei et al. 2009). Xenograft refers to the transfer of tissues taken from one animal and transplanted to another of a different species such as bovine, porcine, and ostrich bone which can be freeze-dried, demineralized, and deproteinized or decellularized (Campana et al. 2014). Bovine bone was first introduced by Maatz and Bauermeister in 1957 (Campana et al. 2014). In spite of availability, good physical characteristics, and low cost, xenografts carry the risks of transmission of zoonotic diseases such as BSE (bovine spongiform encephalopathy) or PERV (porcine endogenous retroviruses), and rejection of the graft is more likely and aggressive (Oryan et al. 2014a; Campana et al. 2014). Recently researchers have devised different methods to decrease the disadvantages of xenografts including decellularization. Decellularization of soft and hard connective tissues such as tendons, ligaments, and bones reduces or even eliminates the immunogenicity associated with allografts and xenografts and, therefore, may be effective in enhancing incorporation of these grafts (Oryan et al. 2014a). Multiple physical, chemical, and enzymatic methods have been used to remove cytoplasmic and nuclear antigens with preservation of the extracellular matrix structure and maintenance of mechanical and functional characteristics (Oryan et al. 2014a).
Ceramics
A ceramic is an inorganic solid that is produced by sintering (a heat-treating process) of non-metallic salts to form crystalline structures. In some cases, the surface characteristics become biologically compatible and support bone ingrowth; hence, these ceramics are termed bioceramics (Kraus 2012). Ceramics can be characterized as bioinert, bioactive, and bioresorbable. Alumina and zirconia were the first ceramics to be introduced to orthopedics, mainly as femoral heads of total hip replacements (McMahon et al. 2013; Navarro et al. 2008).
One of the earliest and though oldest bone substitutes firstly implanted in humans by Dreesman in 1892 is gypsum or calcium sulfate familiar as plaster of Paris (Campana et al. 2014; Millis and Martinez 2003; Kraus 2012; Dewi et al. 2015). This ceramic considered to be a fast degradable material that allows complete resorption before the bone defect area is completely filled by new bone and therefore is not suitable for structural support or for long-term presence as an osteoconductive material (Kraus 2012; Dewi et al. 2015). In a study in 2015, the incorporation of CaCO3 hydrogel into plaster of Paris (POP) in different compositions was assessed by Dewi et al., assuming that it may enhance the bone biological activity of POP and decrease its degradability. Histological analysis of the retrieved specimens indicated that the addition of CaCO3 hydrogel into POP increased bone formation, angiogenesis, and collagen density and resulted into faster bone formation and maturation. It was also confirmed that the degradation rate of the POP decreased by the addition of CaCO3 hydrogel (Dewi et al. 2015). In addition, in a retrospectively review by Yongkun et al. on 50 patients in 2014, calcium sulfate grafts (study group) were compared with bone allografts (control group) for the treatment of benign bone tumors. They investigated bone-healing response, complications, and factors affecting bone healing and reported that calcium sulfate bone substitute healing outcome and safety profile is satisfactory in reconstruction of bone defects after benign bone tumor curettage, especially in smaller cavities. Commercial forms of calcium sulfate (Osteoset and MIIG) supplied as cylindrical pellets and injectable formulations are available as bone graft substitutes that could function as bone void fillers (Millis and Martinez 2003; Kraus 2012). Some of the ceramics, such as hydroxyapatite (HA) and tricalcium phosphate (TCP), possess high compressive strength and hardness along with good biocompatibility; therefore, these materials are appropriate as bone substitutes (McMahon et al. 2013). HA is a naturally occurring mineral form of calcium apatite, considered as the material of choice for preparation of bone graft substitutes because the structure of HA resembles the minerals found in natural bone resulting in osteoconductive properties and formation of tight bonds with surrounding native tissues (McMahon et al. 2013; Oryan et al. 2014a). Although HA accounts for nearly 70% of the mineral content of teeth and bone, the occurring HA in the human body exists in a substituted form. Calcium phosphates have been chemically modified in an effort to produce HA that more closely resembles the mineral content of native bone by incorporating Si, Sr, Zn, Mg, alginate, and carbonate as a replacement for hydroxyl or phosphate groups of the apatite structure (Sarkar and Lee 2015; Campana et al. 2014). These chemical modifications enhanced bioactivity and osteoconduction, osteoblastic proliferation and material performance, dissolution rate, densification behavior, mechanical strength, and biocompatibility. For instance, Hawakawa and collaborators experimental study in 2013 revealed that with the increase in the silicon content in the HA lattice, the in vitro degradation rate of the silicon-containing HA increased, while their crystallite size stayed nearly unchanged (Hayakawa et al. 2013). In another study, Zhao et al. demonstrated that electrochemically deposited magnesium-substituted HA promotes osteogenic differentiation of preosteoblasts in vitro and may improve implant osteointegration during the early stages of bone healing compared with electrochemically deposited pure HA-coated surfaces (Zhao et al. 2013). Another widely used strategy is the combined use of HA and TCP as granules that exhibit interconnected pores, each measuring 100–400 μm (Gomez-Barrena et al. 2015). Since it has been proved that high porosity (more than 80%) and a pore diameter distribution in the range of 200–400 μm are optimal for new bone tissue regeneration, porous calcium phosphate ceramic could be ideal as a bone substitute (Liao et al. 2011). For instance, Hu et al. reported in their study in 2015 that mesenchymal stem cells (MSCs) seeded into porous biphasic calcium phosphate ceramics coated with nano-HA may be an effective bone substitute to reconstruct bone defects (Hu et al. 2015). Newer fabrication techniques have been proposed which allow greater control of pore size, porosity, scaffold shape, ease of fabrication, and reliability of physico-mechanical properties. These various techniques include salt leaching, sponge replica and gas foaming, porogen-based method, and 3D printing (Sarkar and Lee 2015).
Healing promotive factors
Growth factors are a large class of cytokines that have been extensively used to treat bony defects. Growth factors are present in the healthy bone matrix and can be provided by clot or the injured bone itself during different phases of tissue healing as well; therefore, they play a significant role in promoting bone regeneration (Oryan et al. 2014a; Hannouche et al. 2001; Roffi et al. 2013). Platelet-derived growth factor (PDGF) and TGF-β are regulatory molecules released by platelets during clot formation; also BMPs, TGF-β, PDGF, IGF-I, IGF-II, and basic and acidic fibroblast growth factors originate from the bone at the site of injury (Oryan et al. 2014a; Hannouche et al. 2001). The mechanisms of growth factor influences are usually cell surface receptor-mediated, which, in turn, results in expression of one or more gene of the target cell (Kraus 2012). Single growth factors may exhibit more than one type of influence (Kraus 2012). Several advantages have been mentioned for healing promotive factors. For instance, these factors induce migration, growth, proliferation and differentiation of an appropriate subset of cells, as well as vascularization regulation in the site of injury; however, growth factors are expensive, instable in vivo, and needed in high supraphysiological doses due to their susceptibility to burst in the body and their short half-life (Balmayor and van Griensven 2015; Moeinzadeh and Jabbari 2015; Zhao et al. 2015; Civinini et al. 2011). These imperfections lead to a number of undesirable side effects which include bone overgrowth, tumor formation, and immune reactions (Balmayor and van Griensven 2015; Moeinzadeh and Jabbari 2015). Recently, researchers have introduced novel methods to overcome aforementioned disadvantages such as providing controlled-release systems to enhance sustained release of growth factors in vivo and to protect the recombinant growth factors from enzymatic degradation at the injury site (Zhao et al. 2015).
For instance in Santo and colleagues study in 2012, the tridimensional (3D) structure of chitosan-chondroitin sulfate nanoparticles loaded with platelet lysate included in a poly(D,L-lactic acid) foam was seeded with human adipose-derived stem cells (hASCs) and cultured in vitro under osteogenic stimulus, and the synergistic effect of this combination was suggested (Santo et al. 2012).
Platelet-rich plasma
Orthobiologics such as platelet-rich plasma (PRP) are innovative biological sources which offer exciting new possibilities to promote and accelerate bone and soft tissue healing. Recently PRP has become a field of research interest and has had a wide clinical application (Civinini et al. 2011; Dhillon et al. 2012; Alsousou et al. 2009).
PRP is a volume of fractionated plasma from the patient’s own blood (autologous blood) having platelet concentrations above baseline, so that the number of platelets is five times higher than that of the blood (Roffi et al. 2013; Civinini et al. 2011; Dhillon et al. 2012; Alsousou et al. 2009). PRP is an easily obtainable, cost-effective, and valuable source of growth factors with possible beneficial outcomes including reduction of bleeding and pain after surgery, possibility of infection, and rapid tissue healing that might favor the regenerative process (Oryan et al. 2014a; Campana et al. 2014; Roffi et al. 2013; Civinini et al. 2011; Alsousou et al. 2009). In addition, autologous nature of PRP eliminates concerns about immunogenic reactions and disease transmission (Alsousou et al. 2009). When activated by thrombin and calcium, the platelet α granules containing more than 30 bioactive proteins release their contents which play an essential role in bone healing; these include transforming growth factor β, vascular endothelial growth factor (VEGF), insulin-like growth factor, platelet-derived growth factor, epidermal growth factor, hepatocyte growth factor, and basic fibroblast growth factor (Campana et al. 2014; Civinini et al. 2011; Alsousou et al. 2009; Salamanna et al. 2015). Bioactive proteins such as fibrin, fibronectin, vitronectin, and thrombospondin are responsible for osteoblast, fibroblast, and endothelial cell migration (Civinini et al. 2011; Alsousou et al. 2009). For PRP preparation, blood is withdrawn from a patient’s peripheral vein and centrifuged to achieve a high concentration of platelets within a small volume of plasma; after that, PRP is reinjected at a site of injury or inserted as a gel or in combination with other biomaterials during surgery (Salamanna et al. 2015). The first evidence of the clinical benefits of PRP in bone reconstruction therapy was reported by Marx et al. in 1998 (Civinini et al. 2011). Heretofore, PRP has been utilized in combination with autograft, allograft, and xenograft to promote bone regeneration; furthermore, many studies have focused on concurrent use of PRP and different natural or synthetic bone substitutes such as HA and β-TCP (Roffi et al. 2013; Civinini et al. 2011; Alsousou et al. 2009; Salamanna et al. 2015; Hakimi et al. 2010; EL Backly et al. 2014; DurmuŞlar et al. 2014). Many studies evaluated the in vitro effects of PRP and confirmed its strong inductive properties; for example, Parson et al. assessed PRP influences on human MSC proliferation, bone morphogenetic protein-2 messenger RNA expression, alkaline phosphatase activity, and bone formation in vitro and reported that PRP can promote bone regeneration (Parsons et al. 2008). In addition, Simson and collaborators detected that the combination of an injectable chondroitin sulfate tissue adhesive and PRP with human MSC could support bone growth. In a newer study in 2015, Fang-Tian et al. showed that different concentrations of PRP have obvious stimulatory effects on proliferation and osteogenic differentiation of human adipose-derived stem cells in vitro (Xu et al. 2015).
Furthermore, numerous studies highlighted PRP effects on bone healing in vivo. For instance, Hakimi et al. in 2010 demonstrated that PRP combined with autologous cancellous graft leads to a significantly better bone regeneration compared to isolated application of autologous cancellous graft in an in vivo critical size defect on load-bearing long bones of mini-pigs (Hakimi et al. 2010). Shafiei-Sarvestani et al. in 2012 reported promising results from combined use of HA and Persian Gulf coral by macroscopic, histologic, radiologic, and biochemical evaluations in an experimental study on rabbit bone (Oryan et al. 2014a). In a similar study in 2014, EL Backly et al. proved that PRP can enhance osteoconductivity of HA and β-TCP composite (EL Backly et al. 2014). Also, Neves et al. subjected rabbits to a total osteotomy of the proximal portion of the right fibula with or without hyperbaric oxygen therapy and autologous platelet concentrations in 2013 and revealed that hyperbaric oxygen therapy and autologous platelet concentrates combined increased the rate of bone healing in this experimental model (Neves et al. 2013).
Although PRP has been used pervasively, clinical effectiveness and its mechanism of action have not been fully recognized, and enhancement of tissue healing by PRP remains largely anecdotal and controversial (Civinini et al. 2011; Alsousou et al. 2009; Salamanna et al. 2015; Hakimi et al. 2010).
Bone morphogenetic proteins
Bone morphogenetic proteins (BMPs) are a wide and heterogeneous family of secreted proteins within the transforming growth factor beta superfamily introduced by Urist in the 1960s, which can induce ectopic bone formation (Zigdon-Giladi et al. 2015; Dimitriou et al. 2011; Campana et al. 2014; Kraus 2012; Miyazaki et al. 2009; Harwood and Giannoudis 2005). They comprise only 0.1% by weight of all bone proteins and are not accessible until the bone matrix has been demineralized; therefore, they remain rare and very expensive (Miyazaki et al. 2009). Intracellular cascades which resemble endochondral ossification are activated subsequent to adhesion of BMPs to specific receptors on the surface of the osteogenic progenitors, which leads to mitogenesis of MSCs and other osteoprogenitors and their differentiation toward osteoblasts (Dimitriou et al. 2011; Miyazaki et al. 2009; Poth et al. 2015). Most highly studied members of this family are BMP-2, BMP-4, and BMP-7 (Oryan et al. 2014a; Kraus 2012; Miyazaki et al. 2009). Bone morphogenetic proteins are soluble and are rapidly cleared from a local environment easily and become inactivated in vivo if not in a carrier matrix that attenuates clearance and releases them consistently over time (Kraus 2012; Miyazaki et al. 2009). Additionally, carrier matrices may also possess osteoconductive capacities or structural strength (Miyazaki et al. 2009). Several carriers have been utilized; some of them had distinct problems such as technical difficulties, inflammatory reactions, and formation of bony voids within the healed bone (Kraus 2012; Harwood and Giannoudis 2005).
For instance, Cha and colleagues evaluated the efficacy of a bovine HA/collagen carrier loaded with Escherichia coli-derived bone morphogenetic protein 2 (BMP-2) at 0.1, 0.5, and 1.5 mg/ml to augment bone formation in a mongrel dogs nasal sinus in 2014, and they reported that bone morphogenetic protein in this carrier even at low concentrations induces osteogenic activity, enhancing local bone formation in a canine sinus model (Cha et al. 2014). In a similar study in 2015, Taniyama et al. utilized a porous HA-collagen composite as a drug delivery carrier of recombinant human BMP-2 by impregnating of the composite with different amounts of BMP-2, and they concluded that this implant is effective for the repair of osteochondral defects generated in the patellar groove of Japanese white rabbits (Taniyama et al. 2015). Furthermore, Poth et al. in 2015 reported the potential of biodegradable chitosan-tripolyphosphate nanoparticles for a fast release of unmodified BMP-2 at the titanium implant surface in order to enhance the osseointegration of endoprosthesis after revision operations (Poth et al. 2015).
Although many reports confirmed the beneficial effects of BMP on bone regeneration and quality, some others showed their ineffectiveness on regeneration of non-weight-bearing bone healing (Oryan et al. 2014b). For instance, the efficacy of commercially available rhBMP-2-based system to regenerate canine calvarial defect was assessed, and in their result defects treated with rhBMP-2 were significantly less protective against trauma than native bone at 6 months (Cray et al. 2014). It has also been shown in an animal model that artificially administered BMP can cross the placenta and subsequently be detected in the growing embryo. As this area has been little investigated, use in pregnancy is currently contraindicated (Harwood and Giannoudis 2005). In addition, BMPs showed adverse effect in cervical spine and are hence contraindicated in this application (Campana et al. 2014). Finally, the comparison of bone morphogenetic protein-7 and platelet-rich plasma was done by Calori et al. for treating 29 cases of long-bone non-unions. The results indicated that BMP-7 is more efficacious that PRP as there was a significant failure rate of 6.2 versus 38.5% between BMP-7 and PRP, respectively (Civinini et al. 2011; Calori et al. 2006).
Gene therapy
Another promising method in bone repair is the application of gene therapy. The first idea related with a gene therapy approach evolved as early as 1966 and was mentioned by Edward Tatum when he speculated that viruses could be used effectively to introduce new genes into defective cells of particular organs (Balmayor and van Griensven 2015). In 1969, the first isolation of a gene was succeeded by Beckwith, promising a brilliant future to the so-called human genetic engineering (Balmayor and van Griensven 2015). Gene therapy consists of transfer of genetic information into the genome of the target cell, allowing expression of bioactive factors from the cells themselves for a prolonged time where the bone is intended to be regenerated, though it is a safe and effective strategy to induce bone healing (Sarkar and Lee 2015; Dimitriou et al. 2011; Oryan et al. 2014a).
Genetic material can be introduced directly into a distinct area and then can be translocated into the nucleus of the cells by physical mechanisms such as electric-pulsed or ultrasonic waves (Kraus 2012). Alternatively, gene delivery can be performed by viral (transfection) vectors or non-viral (transduction) vectors such as liposomes, cationic polymers, lipids, peptides, and even calcium phosphate (Dimitriou et al. 2011; Oryan et al. 2014a; Balmayor and van Griensven 2015; Kraus 2012; Heyde et al. 2007). Also recently, sonoporation seems to be a promising means (Balmayor and van Griensven 2015). With the in vivo method, viral vectors (adenovirus, retrovirus, and adeno-associated virus) containing the desired genetic material transfer genes directly into the host, and the virus is used to transport the gene into the cell and facilitate its expression (Dimitriou et al. 2011; Oryan et al. 2014a; Kraus 2012). This technique is relatively easier; however, a number of safety issues currently limit using this procedure (Dimitriou et al. 2011). Another method is the indirect ex vivo technique which is performed by harvesting cells from tissues, their genetic modification in vitro, and then re-implantation (Dimitriou et al. 2011). Although this method is technically more demanding, it is a safer method, allowing testing of the cells for any abnormal behavior before re-implantation and selection of those with the highest gene expression (Dimitriou et al. 2011). Adenovirus vectors encoding for bone morphogenetic protein genes have been used (Balmayor and van Griensven 2015; Kraus 2012). In a study by Schwabe et al. in 2012, a COPROG-coated implant and hBMP-2 plasmid, a newly developed non-viral vector, was used to stabilize rat tibial fracture, and a positive effect on fracture healing was shown (Balmayor and van Griensven 2015). Gene therapy has many advantages such as flexibility to express the protein locally and focally, or in a disseminated fashion, as needed and reducing the amounts of therapeutic molecules (Balmayor and van Griensven 2015). Indeed, there are several advantages of gene therapy; this approach has a series of limitations including transinfection of the target cells with the foreign genes and hardship of targeting the right gene at the right location in the right cells. Additionally, another unresolved issue of gene therapy is to express it for sufficiently long time, while minimizing adverse reactions (Oryan et al. 2014a).
Tissue engineering
Tissue engineering, an important therapeutic strategy to be used in regenerative medicine in the present and in the future, can be defined as “a complex and dynamic process that affects the structure and architecture of any viable and non-viable tissue with the aim to increase the effectiveness of the construct to restore, regenerate, maintain, or improve function in defective tissue or lost tissue caused by different pathologic situations” (Oryan et al. 2014a; Gong et al. 2015; Rodriguez-Vazquez et al. 2015). The fundamental concept of tissue engineering, first defined in 1988, is to combine different biocomponents, such as living cells, biomaterials, and biologically active factors, to form tissue engineered constructs to promote the repair and regeneration of tissues; therefore, the triad formed by stem-cells, signaling molecules, and scaffolds or extracellular matrix is considered as the principle of tissue engineering (Rai et al. 2015; Jeong and Atala 2015). Tissue engineering is possible by using different strategies such as introducing isolated MSCs from different origins into defect site, application of growth factors as tissue inducers, and arranging the cells on biologic or synthetic constructs to develop a structural scaffold or matrix to promote bone regeneration (Oryan et al. 2014a; Kraus 2012; Rodriguez-Vazquez et al. 2015).
Isolated stem cells
A stem cell is defined as an unspecialized cell that can renew and maintain itself for a longer period of time with the potential to commit to a cell or tissue lineage with specialized functions (Rai et al. 2015). Multipotent MSCs are non-hematopoietic clonogenic cells of mesodermal derivation residing in several postnatal organs and connective tissues (Barba et al. 2013; Gomez-Barrena et al. 2011). They were first described in the early 1960s, as an adherent, fibroblastoid cell population with inherent osteogenic properties and isolated for the first time from bone marrow by Friedenstein et al. in 1976 (Barba et al. 2013; Gomez-Barrena et al. 2011). These are the most popular stem cells used in bone tissue engineering because of their relatively decreased morbidity during isolation and potential for expansion, proliferation, production of necessary cytokines, differentiation into a variety of cell types such as adipocytes, chondrocytes, and osteocytes, invoking a vascular response, and produce matrix and new bone (Kovach et al. 2015; Campana et al. 2014; Kraus 2012; Rai et al. 2015; Barba et al. 2013). MSCs that contribute to healing are primarily derived from the periosteum, endosteum, and marrow cavity (Marcucio et al. 2015; Knight and Hankenson 2013). MSC harvest, however, requires aspiration from the iliac crest which only yields 10–40 ml of marrow or from bone marrow biopsies, both of which can be painful and yield low numbers; so as an alternative, these cells can be isolated from many other types of tissues and organs such as the adipose tissue, brain, thymus, lung, liver, spleen, kidney, dental pulp, and also embryonic tissues, such as Wharton’s jelly and umbilical cord blood (Kovach et al. 2015; Barba et al. 2013; Marcucio et al. 2015; Aurrekoetxea et al. 2015; Levi and Longaker 2011). An example of stem cell application is Schimming and collaborators study in 2004 which revealed that periosteum-derived osteoblasts can form lamellar bone within 3 months after transplantation (Liao et al. 2011). Another study by Kim et al. in 2009 demonstrated promising results from injection of autologous cultured bone marrow osteoblasts for treating large bone defects (Kim et al. 2009). In a more recent study by Kisiel et al. in 2012, proliferative capacities of bone marrow, adipose tissue, muscle, and periosteum-derived MSCs were compared, and periosteum was reported as a superior tissue source for MSCs (Kisiel et al. 2012). Restrictive factors in clinical use of stem cells are immune rejection of cells that are not of autologous origin, donor-related differences (e.g., age and systemic conditions) that affect cell function, absence of potency test that can predict the in vivo function of cells before transplantation, and the necessity to perform safety and regulation of these procedures before clinical trials (Zigdon-Giladi et al. 2015; Gomez-Barrena et al. 2011).
Scaffolds
Since cell therapy alone is not sufficient to regenerate large tissue defects and replace whole organs, the approach of combining stem cells and biocompatible scaffolds is a more promising strategy. To achieve this, after harvesting stem cells from selected tissues and organs they will be introduced into a natural or synthetic scaffold to assemble a structure similar to desired injured tissue. Scaffolds as the most important issue in this field can be defined as a permanently or temporarily placed three-dimensional porous and permeable natural or synthetic biomaterial that is biocompatible (Oryan et al. 2014a; Rai et al. 2015). Scaffolds act as a matrix for cell adhesion, migration, and proliferation and differentiation, and though properties of scaffolds such as biodegradability, resorbability, hydrophilicity, and hydrophobicity, porosity, suitable pore size and shape, internal and external architecture, stiffness, and strength are responsible for osteoinduction (Oryan et al. 2014a; Rai et al. 2015). In addition, scaffolds for osteogenesis should mimic bone morphology and structure in order to optimize integration into the surrounding tissue and to provide a suitable microenvironment for MSC adhesion, proliferation, and differentiation (Barba et al. 2013). Several major technical advances have been achieved in this field during the past decade. For instance, in the study of Parrilla et al. in 2011, suitability of a synthetic scaffold seeded with adipose tissue-derived stem cells for mandibular defect healing was reported in comparison with the same scaffold seeded with differentiated human dermal fibroblasts and naked scaffold by histologic and computerized tomographic analysis (Parrilla et al. 2011). In a similar study performed by Liao and colleagues in 2013, the osteogenic potential of porcine adipose-derived stem cells was compared among three-dimensional fabricated polycaprolactone, polycaprolactone, and β-TCP and collagen-coated polycaprolactone and β-TCP scaffolds (Liao et al. 2013). The results showed no significant difference in porosity of aforementioned scaffolds; but collagen-coated scaffold was superior in hydrophilicity and swelling ratios and also osteogenic differentiation in vitro (Liao et al. 2013). In addition, better woven bone and vascular tissue formation was yielded on collagen-coated scaffold in vivo (Liao et al. 2013). Moreover, Liu et al. showed in 2013 that hybrid scaffold consists of collagen, and demineralized bone powder seeded with human periosteal-derived cells has good osteoinductive potential (Oryan et al. 2014a). In another study, Xuan et al. studied polycaprolactone/HA tissue scaffolds with individualized grooves manufactured by fused deposition modeling technique alone and seeded with bone marrow-derived MSCs to reconstruct partial sternal defect and they resulted that the scaffold seeded with MSCs could induce new bone union and enhance the amount of bone ingrowth (Xuan et al. 2014).
Another approach in bone tissue engineering is using a natural or synthetic scaffold without seeded stem cells to allow host cell ingrowth and neovascularization and stimulate bone repair and regeneration (McMahon et al. 2013; Oryan et al. 2014a). Natural-based scaffolds have several remarkable advantages in comparison to synthetic scaffolds as a suitable bone substitute which include superior biocompatibility, biodegradability, osteoconduction, osteoinduction, osteogenesis, and osteointegration, but their immunological behavior is variable in different species and is also related to the type of application (Oryan et al. 2014a). Acellularization as a novel manufactural technique for constructing scaffolds reduces or even eliminate immunological associated issues; though recently, it has opened a new insight in tissue engineering. Heretofore, researchers have used various decellularization methods to construct antigen-free collagen-based scaffolds from animal sources (Oryan et al. 2014a; Quan et al. 2014; Funamoto et al. 2010; Dong et al. 2012; Chen et al. 2015; Chen et al. 2016; Farnebo et al. 2014). It should be noted that present article authors have used decellularization techniques on different tissues of ostrich in order to provide suitable xenograft scaffolds promoting healing and regeneration (Saadinam et al. 2014; Farahani et al. 2015; Fatourehchi et al. 2015). In these studies, acellular cornea, skin, tendon, meniscus, and biphasic osteochondral composite (unpublished data) derived from ostrich was grafted to rabbit and guinea pig, and promising results were obtained. Since bone is mainly composed of collagen and HA, scaffolds containing these organic materials function better than other bone substitutes. Nakamura et al. investigated high hydrostatic pressure as a modern method of decellularization in 2014 and tested the obtained scaffold in vivo and in vitro (Quan et al. 2014). They assured that this method would completely remove cells, antigen molecules, and viruses while preserving structure and the composition of the native tissue (Quan et al. 2014). In a study performed by Chen and collaborators in 2015, cell-free bone coated with collagen and HA was used as a three-dimensional scaffold for evaluating repair efficacy in vivo and osteogenic differentiation in vitro (Chen et al. 2016). Recently, cultural and religious limitations and the high risk of zoonotic disease transmission have attracted researchers toward utilizing other sources of collagen such as marine sources (Silva et al. 2014; Pati et al. 2012; Chou et al. 2014; Yamamoto et al. 2014). Accessibility, availability, cost-effectiveness, and possessing similar composition to bone are the most important advantages of marine sources (Oryan et al. 2014a; Silva et al. 2014). Hoyer et al. in 2012 used mineralized salmon skin collagen and HA to assemble an appropriate scaffold for bone regeneration, possessing good elasticity, absorbability, and porosity (Hoyer et al. 2012). In another study in 2014, Cheng-Hung and colleagues used acellular fish scale to prepare a pin for internal fixation of femoral fracture in rabbit and achieved promising results (Chou et al. 2014). Presently, the role of fish scale and its decellularized scaffold with PRP on healing of tibial bone defect in rabbit is under investigation by present article authors.
To overcome limitations of bone repair methods and to find an ideal bone substitute, calcium-phosphate-based biomaterials are widely used in the past decades (Dimitriou et al. 2011; Oryan et al. 2014a; Navarro et al. 2008). Of these, HA, the most important structural component of natural hard tissues, is attractive as a source for biomedical applications nowadays due to its non-toxicity, excellent biocompatibility, osteoconductivity, and osteogenicity (Wang et al. 2013; Kim et al. 2014; Ivankovic et al. 2010; Venkatesan et al. 2014; Michel et al. 2015). The scaffold constructed from HA acts as a temporary substrate or template, providing the necessary support for the cell and vascular ingrowth such as oxygen and nutrients and maintains their differentiated functions. Furthermore, its architecture defines the final shape of the new bone (Ivankovic et al. 2010; Michel et al. 2015). Heretofore, several natural sources of calcium and phosphate have been used as raw material to provide HA scaffolds including egg shell, animal skeleton, and marine sources like coral and nacre (Kim et al. 2013; Cadman et al. 2012; Ni and Ratner 2003; Gao et al. 2007). Coralline-based xenografts introduced as bone graft substitutes in the mid-1970s could be used either simply in their natural calcium carbonate form for better resorption of the graft by the natural bone or transformed industrially into HA through a hydrothermal process for promoting biological activity (Hannouche et al. 2001; Campana et al. 2014; Kim et al. 2013). For instance, Gao et al. in 2007 obtained HA from coral exoskeleton under different thermal conditions and intervals (Gao et al. 2007). In addition to coral, marine environment is rich in porous organisms containing minerals that make them appropriate for bone replacement (Kim et al. 2013; Clarke et al. 2011). Cuttlebone, the internal hard organ of cuttlefish, is an ultra-lightweight highly porous structure consists of calcium carbonate which plays an important role in organism protection and functions as a floating tank. Its chemistry and crystallography are similar to coral, and it is also low cost and readily available (Kim et al. 2014; Kim et al. 2013; Cadman et al. 2012). It also has osteoconductivity, biocompatibility, and plasticity due to its morphological and chemical characteristics (Dogan and Okumus 2014). It should be noted that its pore diameter varies between 200 and 600 μm in different species and therefore, it is suitable for new bone formation and neovascularization (Hoyer et al. 2012; Dogan and Okumus 2014). Several researches have investigated the effect of raw or processed cuttlebone in bone repair and regeneration during the last decades (Hoyer et al. 2012; Kim et al. 2014; Ivankovic et al. 2010; Kim et al. 2013; Cadman et al. 2012; Dogan and Okumus 2014; Hongmin et al. 2015; Tkalčec et al. 2014; Kim et al. 2012; Yi et al. 2011; Liu et al. 2013; Ivankovic et al. 2009). For instance, a porous polycaprolactone (PCL) scaffold incorporating cuttlebone-derived HA powder was fabricated using the solvent casting and particulate leaching method by Kim and collaborators in 2013 for application in tissue engineering (Kim et al. 2014). In a similar study, Hongmin et al. demonstrated that cuttlebone-derived HA has a high surface protein adsorption, it supports MSC differentiation as a scaffold and it also induces new bone formation without using exogenous growth factors and cells after subcutaneous implantation (Hongmin et al. 2015). Presently, the role of calcium carbonate and cuttlefish-derived HA with PRP on healing of tibial bone defect in rabbit is under investigation by present article authors.
Growth factors as tissue inducer
Promising results from several experimental and clinical trials have suggested administration of growth factors and other bioactive molecules to promote bone formation and repair in preclinical and clinical conditions (Campana et al. 2014). Heretofore, many researchers have studied a combination of different growth factors and supportive scaffolds (Oryan et al. 2014a; Oryan et al. 2014b). For instance, Ozturk et al. evaluated the efficacy of VEGF combined with HA-containing gelatin scaffold in treatment of critical-sized tibial bone defect in rabbit model and showed that it is more effective in early phase of fracture healing than the scaffold without VEGF (Oryan et al. 2014b). Another prospect in using growth factor is as a tissue inducer. A variety of administration methods have been investigated including bolus injection, surface-adsorbed protein release, osmotic pumps, and controlled release from biodegradable scaffolds (Campana et al. 2014). More recently, drug delivery techniques such as entrapment within a matrix allowing growth factors to be released at a desirable rate and concentration from the scaffold to aid the regenerating tissue have been applied (Campana et al. 2014). For instance, Subbiah et al. designed a novel dual growth factor delivery system by combining polylactic-co-glycolic acid (PLGA) nanoparticle-encapsulated bone morphogenetic protein and VEGF which included alginate microcapsules via an electro-dropping method. They assessed the scaffold for umbilical cord blood-derived MSC osteogenesis in vitro. Furthermore, they applied the scaffold in an 8-mm diameter rat calvarial defect model with collagen and obtained positive results including vascularized bone regeneration, 82.3% bone healing, and 12.6% vessel-occupied area confirmed by computed tomography and histology analyses (Subbiah et al. 2015). Some other newer approaches for controlled growth factor delivery are under investigation recently; for example, a unique scaffolding system is synthesized by Ma and collaborators via encapsulating BMP-2-binding nanospheres into nanofibrous microspheres. They used heparin-conjugated gelatin as a domain for BMP-2 to stabilize this growth factor, protect it from denaturation and proteolytic degradation, and subsequently prolong its sustained release. Finally, they reported that this microsphere is an excellent osteoinductive scaffold for enhanced bone regeneration by evaluating the system in calvarial defect model (Ma et al. 2015).
Three-dimensional printing
Among all the biofabrication approaches, three-dimensional bioprinting technology based on inkjet printing of a liquid binder onto powder biomaterials is becoming a dominant technological platform and is suggested as a new paradigm for twenty-first century tissue engineering (Oryan et al. 2014a; Gao and Cui 2016). This approach has several advantageous properties such as delivering and creating biomimicked tissue with high throughput, digital control, and the capacity of single cell manipulation. Therefore, this enabling technology may be our next step in surpassing the hurdles and limitations of conventional scaffold-based tissue engineering and has great potential in regenerative medicine and translational applications (Jeong and Atala 2015; Gao and Cui 2016). In this regard, Zeng et al. evaluated the efficacy and feasibility of three-dimensional printing (3D printing)-assisted internal fixation of unstable pelvic fracture from minimal invasive para-rectus abdominis approach in 38 patients, retrospectively (Zeng et al. 2015). They reported that all patients have achieved clinical healing, with mean healing time of 8 weeks, and suggested that this method has the advantages of trauma minimally, bleeding less, healing rapidly and satisfactory reduction, and worthwhile for spreading in clinical practice. In another study with similar purpose, Ishack and colleagues created custom 3D scaffolds of 15% HA and 85% β-TCP coated with dipyridamole, bone morphogenetic protein 2, or saline and assessed it by implanting in a 3-mm cranial critical bone defect. Histological analysis showed increased bone formation and a trend toward increased remodeling in both coated scaffold and suggested that these coated scaffolds may be very useful for treating critical bone defects due to trauma, infection, or other causes (Gomez-Barrena et al. 2011). 3D bioprinting is yet to successfully overcome the many challenges related to building 3D structures that closely resemble native organs and tissues, which are complex structures with defined microarchitecture and a variety of cell types in a confined area. An integrated approach with a combination of technologies from the fields of engineering, biomaterial science, cell biology, physics, and medicine is required to address these complexities (Zhang and Zhang 2015).
Conclusion and perspectives
Heretofore, researchers have been using various methods such as grafts, natural and synthetic bone substitutes, healing promotive factors, stem cells and gene therapy, and 3D-printing in order to enhance bone regeneration; each of these options possesses specific advantages. For instance, bone grafts are ideal for restoring the continuity of injured long bones, may be helpful in fusion of joints, filling major bone defects, and achieving some degrees of union in delayed and non-union fractures (Millis and Martinez 2003). Ceramics can be characterized as bioinert, bioactive, and bioresorbable. Some of the ceramics, such as HA and TCP, possess high compressive strength and hardness along with good biocompatibility; therefore, these materials are appropriate as bone substitutes (McMahon et al. 2013). Healing promotive factors are appropriate when migration, proliferation and differentiation of cells, and vascularization is required in the site of injury (Balmayor and van Griensven 2015; Moeinzadeh and Jabbari 2015; Zhao et al. 2015; Civinini et al. 2011). However, growth factors are expensive, instable in vivo, and needed in high supraphysiological doses due to their susceptibility to burst in the body and their short half-life (Balmayor and van Griensven 2015; Moeinzadeh and Jabbari 2015; Zhao et al. 2015; Civinini et al. 2011). The effectiveness of BMP, one of the popular healing promoters, is still controversial (Cray et al. 2014). The use of gene therapy depends on weighing the advantages like flexibility to express the protein locally against the disadvantages including transinfection of the target cells with the foreign genes and hardship of targeting the right gene at the right location in the right cells (Oryan et al. 2014a). Although stem cell therapy showed promising results in several studies, some restrictive factors such as immune rejection of cells that are not of autologous origin and variations in individual characteristics affecting on cell function have been mentioned (Zigdon-Giladi et al. 2015; Gomez-Barrena et al. 2011). In addition, cell therapy alone is not sufficient to regenerate large tissue defects and replace whole organs; therefore, the approach of combining stem cells and biocompatible scaffolds is a more promising strategy (Oryan et al. 2014a; Rai et al. 2015). 3D printing is a novel approach that has great potential in regenerative medicine and translational applications and could resolve conventional scaffold-based tissue engineering-related problems (Jeong and Atala 2015; Gao and Cui 2016).
It is somehow difficult to note a single method as an ideal and best option to promote bone regeneration in different clinical conditions. We tried to discuss advantages and disadvantages of each method but there are still some blind aspects in bone regenerative medicine in which bone regeneration is insufficient or compromised such as large bone defects, delayed and non-unions, and skeletal abnormalities. Therefore, these conditions demand further investigations, and bone regeneration is an active research area. Development of innovative approaches is expected in the near future due to progressive expansion of bone biological and molecular knowledge. Natural materials often entail a certain level of immunoinertness and biodegradability and can be included in scaffolds for differentiative purposes. Conversely, synthetic materials are modifiable and often mass producible, a desirable trait when considering scale-up for various patients and/or large defect areas. By combining synthetic and natural materials, the benefits of each can be combined into a single scaffold (Michel et al. 2015).
References
Alsousou J, Thompson M, Hulley P, Noble A, Willett K (2009) The biology of platelet-rich plasma and its application in trauma and orthopaedic surgery: a review of the literature. J Bone Joint Surg Br 91(8):987–996
Aurrekoetxea M, Garcia-Gallastegui P, Irastorza I, Luzuriaga J, Uribe-Etxebarria V, Unda F et al (2015) Dental pulp stem cells as a multifaceted tool for bioengineering and the regeneration of craniomaxillofacial tissues. Front Physiol 6:289
Balmayor ER, van Griensven M (2015) Gene therapy for bone engineering. Front Bioeng Biotechnol 3:9
Barba M, Cicione C, Bernardini C, Michetti F, Lattanzi W (2013) Adipose-derived mesenchymal cells for bone regereneration: state of the art. Biomed Res Int 2013:416391
Barnes K, Lanz O, Werre S, Clapp K, Gilley R (2015) Comparison of autogenous cancellous bone grafting and extracorporeal shock wave therapy on osteotomy healing in the tibial tuberosity advancement procedure in dogs. Radiographic densitometric evaluation. Vet Comp Orthop Traumatol 28(3):207–214
Buckwalter JA, Cooper RR (1987) Bone structure and function. Instr Course Lect 36:2748
Cadman J, Zhou S, Chen Y, Li Q (2012) Cuttlebone: characterisation, application and development of biomimetic materials. J Bionic Eng 9(3):367–376
Calori GM, D'Avino M, Tagliabue L, Albisetti W, d'Imporzano M, Peretti G (2006) An ongoing research for evaluation of treatment with BMPs or AGFs in long bone non-union: protocol description and preliminary results. Injury 37(Suppl 3):S43–S50
Campana V, Milano G, Pagano E, Barba M, Cicione C, Salonna G et al (2014) Bone substitutes in orthopaedic surgery: from basic science to clinical practice. J Mater Sci Mater Med 25(10):2445–2461
Cha JK, Lee JS, Kim MS, Choi SH, Cho KS, Jung UW (2014) Sinus augmentation using BMP-2 in a bovine hydroxyapatite/collagen carrier in dogs. J Clin Periodontol 41(1):86–93
Chen YC, Chen RN, Jhan HJ, Liu DZ, Ho HO, Mao Y et al (2015) Development and characterization of acellular extracellular matrix scaffolds from porcine menisci for use in cartilage tissue engineering. Tissue Eng Part C Methods 21(9):971–986
Chen G, Yang L, Lv Y (2016) Cell-free scaffolds with different stiffness but same microstructure promote bone regeneration in rabbit large bone defect model. J Biomed Mater Res A 104(4):833–841
Chou CH, Chen YG, Lin CC, Lin SM, Yang KC, Chang SH (2014) Bioabsorbable fish scale for the internal fixation of fracture: a preliminary study. Tissue Eng Part A 20(17–18):2493–2502
Civinini R, Macera A, Nistri L, Redl B, Innocenti M (2011) The use of autologous blood-derived growth factors in bone regeneration. Clin Cases Miner Bone Metab 8(1):25–31
Clarke B (2008) Normal bone anatomy and physiology. Clin J Am Soc Nephrol 3(Suppl 3):S131–S139
Clarke SA, Walsh P, Maggs CA, Buchanan F (2011) Designs from the deep: marine organisms for bone tissue engineering. Biotechnol Adv 29(6):610–617
Cray J Jr, Henderson SE, Smith DM, Kinsella CR Jr, Bykowski M, Cooper GM et al (2014) BMP-2-regenerated calvarial bone: a biomechanical appraisal in a large animal model. Ann Plast Surg 73(5):591–597
De Baat P, Heijboer MP, De Baat C (2005) Development, physiology, and cell activity of bone. Ned Tijdschr Tandheelkd 112(7):258–263
Denny HR, Butterworth SJ (2000) A guide to canine and feline orthopaedic surgery, 4th edn. Blackwell, Australia
Dewi AH, Ana ID, Wolke J, Jansen J (2015) Behavior of POP-calcium carbonate hydrogel as bone substitute with controlled release capability: a study in rat. J Biomed Mater Res A 103(10):3273–3283
Dhillon RS, Schwarz EM, Maloney MD (2012) Platelet-rich plasma therapy—future or trend? Arthritis Res Ther 14(4):219
Dimitriou R, Jones E, McGonagle D, Giannoudis PV (2011) Bone regeneration: current concepts and future directions. BMC Med 9:66
Dogan E, Okumus Z (2014) Cuttlebone used as a bone xenograft in bone healing. Vet Med (Praha) 59(5):254–260
Dong J, Mo X, Li Y, Chen D (2012) Recent research progress of decellularization of native tissues. Sheng Wu Yi Xue Gong Cheng Xue Za Zhi 29(5):1007–1013
DurmuŞlar MC, Alpaslan C, Alpaslan G, Çakır M (2014) Clinical and radiographic evaluation of the efficacy of plateletrich plasma combined with hydroxyapatite bone graft substitutes in the treatment of intrabony defects in maxillofacial region. Acta Odontol Scand 72(8):948–953
EL Backly RM, Zaky SH, Canciani B, Saad MM, Eweida AM, Brun F et al (2014) Platelet rich plasma enhances osteoconductive properties of a hydroxyapatite/β-tricalcium phosphate scaffold (Skelite) for late healing of critical size rabbit calvarial defects. J Craniomaxillofac Surg 42(5):e70–e79
Farahani F, Fattahian HR, Kajbafzadeh AM (2015) Experimental study on ostrich dermal acellular matrix in repair of full thickness wounds of guinea pig. Kafkas Univ Vet Fak 21(5):697
Farnebo S, Woon CY, Bronstein JA, Schmitt T, Lindsey DP, Pham H et al (2014 Jan) Decellularized tendon-bone composite grafts for extremity reconstruction: an experimental study. Plast Reconstr Surg 133(1):79–89
Fatourehchi M, Fattahian HR, Kajbafzadeh AM (2015) The experimental study of bio-engineered free-cell ostrich cornea as xenograft. Comp Pathobiol. Comp pathbiol 12(2)
Funamoto S, Nam K, Kimura T, Murakoshi A, Hashimoto Y, Niwaya K et al (2010) The use of high-hydrostatic pressure treatment to decellularize blood vessels. Biomaterials 31(13):3590–3595
Gao G, Cui X (2016) Three-dimensional bioprinting in tissue engineering and regenerative medicine. Biotechnol Lett 38(2):203–211
Gao Z, Mao TQ, Chen FL, He LS, Hou R, Yang YW et al (2007) The preparation of series of controllable degredation coral-hydroxyapatite (SCHA-200R) and the on its application as the scaffold in bone tissue-engineering. Zhonghua Zheng Xing Wai Ke Za Zhi 23(3):236–240
Gomez-Barrena E, Rosset P, Muller I, Giordano R, Bunu C, Layrolle P et al (2011) Bone regeneration: stem cell therapies and clinical studies in orthopaedics and traumatology. J Cell Mol Med 15(6):1266–1286
Gomez-Barrena E, Rosset P, Lozano D, Stanovici J, Ermthaller C, Gerbhard F (2015) Bone fracture healing: cell therapy in delayed unions and nonunions. Bone 70:93–101
Gong T, Xie J, Liao J, Zhang T, Lin S, Lin Y (2015) Nanomaterials and bone regeneration. Bone Res 3:15029
Hakimi M, Jungbluth P, Sager M, Betsch M, Herten M, Becker J et al (2010) Combined use of plateletrich plasma and autologous bone grafts in the treatment of long bone defects in minipigs. Injury 41(7):71723
Hannouche D, Petite H, Sedel L (2001) Current trends in the enhancement of fracture healing. J Bone Joint Surg Br 83(2):157–164
Harwood PJ, Giannoudis PV (2005) Application of bone morphogenetic proteins in orthopaedic practice: their efficacy and side effects. Expert Opin Drug Saf 4(1):75–89
Hayakawa S, Kanaya T, Tsuru K, Shirosaki Y, Osaka A, Fujii E et al (2013) Heterogeneous structure and in vitro degradation behavior of wet-chemically derived nanocrystalline silicon-containing hydroxyapatite particles. Acta Biomater 9(1):4856–4867
Heyde M, Partridge KA, Oreffo RO, Howdle SM, Shakesheff KM, Garnett MC (2007) Gene therapy used for tissue engineering applications. J Pharm Pharmacol 59(3):329–350
Hongmin L, Wei Z, Xingrong Y, Jing W, Wenxin G, Jihong C et al (2015) Osteoinductive nanohydroxyapatite bone substitute prepared via in situ hydrothermal transformation of cuttlefish bone. J Biomed Mater Res B Appl Biomater 103(4):816–824
Hoyer B, Bernhardt A, Heinemann S, Stachel A, Meyer M, Gelinsky M (2012) Biomimetically mineralized salmon collagen scaffolds for application in bone tissue engineering. Biomacromolecules 13(4):1059–1066
Hu J, Yang Z, Zhou Y, Liu Y, Li K, Lu H (2015) Porous biphasic calcium phosphate ceramics coated with nano-hydroxyapatite and seeded with mesenchymal stem cells for reconstruction of radius segmental defects in rabbits. J Mater Sci Mater Med 26(11):257
Ivankovic H, Gallego Ferrer G, Tkalcec E, Orlic S, Ivankovic M (2009) Preparation of highly porous hydroxyapatite from cuttlefish bone. J Mater Sci Mater Med 20(5):1039–1046
Ivankovic H, Tkalcec E, Orlic S, Ferrer GG, Schauperl Z (2010) Hydroxyapatite formation from cuttlefish bones: kinetics. J Mater Sci Mater Med 21(10):2711–2722
Jeong CG, Atala A (2015) 3D printing and biofabrication for load bearing tissue engineering. Adv Exp Med Biol 881:3–14
Kim SJ, Shin YW, Yang KH, Kim SB, Yoo MJ, Han SK et al (2009) A multi-center, randomized, clinical study to compare the effect and safety of autologous cultured osteoblast (Ossron) injection to treat fractures. BMC Musculoskelet Disord 10:20
Kim BS, Kim JS, Sung HM, You HK, Lee J (2012) Cellular attachment and osteoblast differentiation of mesenchymal stem cells on natural cuttlefish bone. J Biomed Mater Res A 100(7):1673–1679
Kim BS, Kang HJ, Lee J (2013) Improvement of the compressive strength of a cuttlefish bone-derived porous hydroxyapatite scaffold via polycaprolactone coating. J Biomed Mater Res B Appl Biomater 101(7):1302–1309
Kim BS, Yang SS, Lee J (2014) A polycaprolactone/cuttlefish bone-derived hydroxyapatite composite porous scaffold for bone tissue engineering. J Biomed Mater Res B Appl Biomater 102(5):943–951
Kisiel AH, McDuffee LA, Masaoud E, Bailey TR, Esparza Gonzalez BP, Nino-Fong R (2012) Isolation, characterization, and in vitro proliferation of canine mesenchymal stem cells derived from bone marrow, adipose tissue, muscle, and periosteum. Am J Vet Res 73(8):1305–1317
Knight MN, Hankenson KD (2013) Mesenchymal stem cells in bone regeneration. Adv Wound Care (New Rochelle) 2(6):306–316
Kovach TK, Dighe AS, Lobo PI, Cui Q (2015) Interactions between MSCs and immune cells: implications for bone healing. J Immunol Res 2015:752510
Kraus KH (2012) Bone grafts and substitutes. In: Tobias KM, Johnston SA (eds) Veterinary surgery: small animal. Saunders, Canada, pp 676–684
Levi B, Longaker MT (2011) Concise review: adipose-derived stromal cells for skeletal regenerative medicine. Stem Cells 29(4):576–582
Liao X, Lu S, Zhou Y, Winter C, Xu W, Li B et al (2011) Bone physiology, biomaterial and the effect of mechanical/physical microenvironment on MSC osteogenesis. Cell Mol Bioeng 4(4):579–590
Liao HT, Lee MY, Tsai WW, Wang HC, Lu WC (2013) Osteogenesis of adipose-derived stem cells on polycaprolactone-beta-tricalcium phosphate scaffold fabricated via selective laser sintering and surface coating with collagen type I. J Tissue Eng Regen Med. doi:10.1002/term.1811
Liu Y, Yu J, Bai J, Gu JS, Cai B, Zhou X (2013) Effects of cuttlefish bone-bone morphogenetic protein composite material on osteogenesis and revascularization of bone defect in rats. Zhonghua Shao Shang Za Zhi 29(6):54853
Ma C, Jing Y, Sun H, Liu X (2015) Hierarchical nanofibrous microspheres with controlled growth factor delivery for bone regeneration. Adv Healthc Mater 4(17):2699–2708
Marcucio RS, Nauth A, Giannoudis PV, Bahney C, Piuzzi NS, Muschler G et al (2015) Stem cell therapies in orthopaedic trauma. J Orthop Trauma 29(Suppl 12):S24–S27
Marsell R, Einhorn TA (2011) The biology of fracture healing. Injury 42(6):551–555
McMahon RE, Wang L, Skoracki R, Mathur AB (2013) Development of nanomaterials for bone repair and regeneration. J Biomed Mater Res B Appl Biomater 101(2):387–397
Michel J, Penna M, Kochen J, Cheung H (2015) Recent advances in hydroxyapatite scaffolds containing mesenchymal stem cells. Stem Cells Int 2015:305217
Millis DL, Martinez SA (2003) Bone Grafts. In: Douglas S (ed) Textbook of small animal surgery, 3th edn. Saunders, United States of America, pp 1875–1891
Miyazaki M, Tsumura H, Wang JC, Alanay A (2009) An update on bone substitutes for spinal fusion. Eur Spine J 18(6):783–799
Moeinzadeh S, Jabbari E (2015) Morphogenic peptides in regeneration of load bearing tissues. Adv Exp Med Biol 881:95–110
Navarro M, Michiardi M, Castaño O, Planell A (2008) Biomaterials in orthopaedics. J R Soc Interface 5(27):1137–1158
Neves PC, Abib Sde C, Neves RF, Pircchio O, Saad KR, Saad PF et al (2013) Effect of hyperbaric oxygen therapy combined with autologous platelet concentrate applied in rabbit fibula fraction healing. Clinics (Sao Paulo) 68(9):1239–1246
Ni M, Ratner BD (2003) Nacre surface transformation to hydroxyapatite in a phosphate buffer solution. Biomaterials 24(23):4323–4331
Oryan A, Alidadi S, Moshiri A, Maffulli N (2014a) Bone regenerative medicine: classic options, novel strategies, and future directions. J Orthop Surg Res 9:18
Oryan A, Alidadi S, Moshiri A, Maffulli N (2014b) Bone regenerative medicine: classic options, novel strategies, and future directions. J Orthop Surg Res 9(1):18
Parrilla C, Saulnier N, Bernardini C, Patti R, Tartaglione T, Fetoni AR et al (2011) Undifferentiated human adipose tissue-derived stromal cells induce mandibular bone healing in rats. Arch Otolaryngol Head Neck Surg 137(5):463–470
Parsons P, Butcher A, Hesselden K, Ellis K, Maughan J, Milner R et al (2008) Platelet-rich concentrate supports human mesenchymal stem cell proliferation, bone morphogenetic protein-2 messenger RNA expression, alkaline phosphatase activity, and bone formation in vitro: a mode of action to enhance bone repair. J Orthop Trauma 22(9):595–604
Pati F, Datta P, Adhikari B, Dhara S, Ghosh K, Das Mohapatra PK (2012) Collagen scaffolds derived from fresh water fish origin and their biocompatibility. J Biomed Mater Res A 100(4):1068–1079
Piermattei DL, Flo G, Decamp CH (2006) Handbook of small animal orthopaedics and fracture repair. 4th ed. United States of America: Saunders. Chapter 3. Bone grafting; p.160
Poth N, Seiffart V, Gross G, Menzel H, Dempwolf W (2015) Biodegradable chitosan nanoparticle coatings on titanium for the delivery of BMP-2. Biomol Ther 5(1):3–19
Quan TM, Vu DN, Ha TLB (2014) Decellularization of xenogenic bone grafts for potential use as tissue engineering scaffolds. JJLSR 4(4):38–46
Rai R, Raval R, Khandeparker RV, Chidrawar SK, Khan AA, Ganpat MS (2015) Tissue engineering: step ahead in maxillofacial reconstruction. J Int Oral Health 7(9):138–142
Rodriguez-Vazquez M, Vega-Ruiz B, Ramos-Zuniga R, Saldana-Koppel DA, Quinones-Olvera LF (2015) Chitosan and its potential use as a scaffold for tissue engineering in regenerative medicine. Biomed Res Int 2015:821279
Roffi A, Filardo G, Kon E, Marcacci M (2013) Does PRP enhance bone integration with grafts, graft substitutes, or implants? A systematic review. BMC Musculoskelet Disord 14:330
Saadinam F, Fattahian HR, Kajbafzadeh AM (2014) Meniscal lesions and their healing: new aspects. Comp clin pathol
Salamanna F, Veronesi F, Maglio M, Della Bella E, Sartori M, Fini M (2015) New and emerging strategies in platelet rich plasma application in musculoskeletal regenerative procedures: general overview on still open questions and outlook. Biomed Res Int 2015:846045
Santo VE, Duarte AR, Popa EG, Gomes ME, Mano JF, Reis RL (2012) Enhancement of osteogenic differentiation of human adipose derived stem cells by the controlled release of platelet lysates from hybrid scaffolds produced by supercritical fluid foaming. J Control Release 162(1):19–27
Sarkar SK, Lee BT (2015) Hard tissue regeneration using bone substitutes: an update on innovations in materials. Korean J Intern Med 30(3):279–293
Shafiei Z, Bigham AS, Dehghani SN, Nezhad ST (2009) Fresh cortical autograft versus fresh cortical allograft effects on experimental bone healing in rabbits: radiological, histopathological and biomechanical evaluation. Cell Tissue Bank 10(1):19–26
Silva TH, Silva JM, Marques ALP, Domingues A, Bayon Y, Reis RL (2014) Marine origin collagens and its potential applications. Mar Drugs 12(12):5881–5901
Subbiah R, Hwang MP, Van SY, Do SH, Park H, Lee K et al (2015) Osteogenic/angiogenic dual growth factor delivery microcapsules for regeneration of vascularized bone tissue. Adv Healthc Mater 4(13):1982–1992
Taniyama T, Masaoka T, Yamada T, Wei X, Yasuda H, Yoshii T et al (2015) Repair of osteochondral defects in a rabbit model using a porous hydroxyapatite collagen composite impregnated with bone morphogenetic protein-2. Artif Organs 39(6):529–535
Tkalčec E, Popović J, Orlić S, Milardović S, Ivanković H (2014) Hydrothermal synthesis and thermal evolution of carbonate-fluorhydroxyapatite scaffold from cuttlefish bones. Mater Sci Eng C Mater Biol Appl 42:578–586
Venkatesan J, Vinodhini PA, Sudha PN, Kim SK (2014) Chitin and chitosan composites for bone tissue regeneration. Adv Food Nutr Res 73:59–81
Wang Q, Gu Z, Jamal S, Detamore MS, Berkland C (2013) Hybrid hydroxyapatite nanoparticle colloidal gels are injectable fillers for bone tissue engineering. Tissue Eng A 19(23–24):2586–2593
Xu FT, Li HM, Yin QS, Liang ZJ, Huang MH, Chi GY et al (2015) Effect of activated autologous platelet-rich plasma on proliferation and osteogenic differentiation of human adipose-derived stem cells in vitro. Am J Transl Res 7(2):257–270
Xuan Y, Tang H, Wu B, Ding X, Lu Z, Li W et al (2014) A specific groove design for individualized healing in a canine partial sternal defect model by a polycaprolactone/hydroxyapatite scaffold coated with bone marrow stromal cells. J Biomed Mater Res A 102(10):3401–3408
Yamamoto K, Igawa K, Sugimoto K, Yoshizawa Y, Yanagiguchi K, Ikeda T et al (2014) Biological safety of fish (tilapia) collagen. Biomed Res Int 2014:630757
Yi HC, Tang LH, Zhang XP (2011) Experimental study on bone defect treated by combined autologous bone marrow transplantation, cuttlebone, and sodium hyaluronate. Zhongguo Zhong Xi Yi Jie He Za Zhi 31(8):11226
Zeng C, Xiao J, Wu Z, Huang W (2015) Evaluation of three-dimensional printing for internal fixation of unstable pelvic fracture from minimal invasive para-rectus abdominis approach: a preliminary report. Int J Clin Exp Med 8(8):13039–13044
Zhang X, Zhang Y (2015) Tissue engineering applications of three-dimensional bioprinting. Cell Biochem Biophys
Zhao SF, Jiang QH, Peel S, Wang XX, He FM (2013) Effects of magnesium-substituted nanohydroxyapatite coating on implant osseointegration. Clin Oral Implants Res 24(Suppl A100):34–41
Zhao HY, Wu J, Zhu JJ, Xiao ZC, He CC, Shi HX et al (2015) Research advances in tissue engineering materials for sustained release of growth factors. Biomed Res Int 2015:808202
Zigdon-Giladi H, Rudich U, Michaeli Geller G, Evron A (2015) Recent advances in bone regeneration using adult stem cells. World J Stem Cells 7(3):630–640
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Fattahian, H., Mansouri, K. & Mansouri, N. Biomaterials, substitutes, and tissue engineering in bone repair: current and future concepts. Comp Clin Pathol 28, 879–891 (2019). https://doi.org/10.1007/s00580-017-2507-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00580-017-2507-2