Abstract
Purpose
This study aimed to identify the incidence and risk factors of early post-operative cognitive dysfunction (POCD) in middle-aged patients undergoing cardiac surgery.
Methods
Data were examined retrospectively from 71 patients aged 46–64 years who underwent elective cardiac surgery. Magnetic resonance imaging (MRI) and MR angiography were obtained preoperatively to assess prior cerebral infarctions, carotid artery stenosis, and intracranial arterial stenosis. Patients also completed six neuropsychological tests of memory, attention, and executive function before and after surgery. Mild cognitive impairment (MCI) was defined as performance 1.5 standard deviations (SD) below the population means on any neurocognitive battery, whereas POCD was defined as a decrease of 1 SD population means on at least two in the test battery. Patient characteristics were analyzed using univariate analysis, and independent predictors were analyzed using multivariate logistic regression analysis.
Results
After surgery, 25 patients (35%) were assessed with POCD. Patients with POCD had significantly higher rates of preoperative MCI and cerebral infarcts on MRI. Multivariate logistic regression analysis identified preoperative MCI and cerebral infarctions detected by MRI as a predictor of POCD.
Conclusion
More than one-third of middle-aged patients undergoing cardiac surgery developed POCD. Our findings suggested preoperative MCI and infarcts detected by MRI were risk factors for POCD in these middle-aged patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Postoperative cognitive dysfunction (POCD) is characterized by temporary or long-term cognitive decline measured by neuropsychological tests after anesthesia and surgery. POCD adverse impact on quality of life may result in prolonged hospital stay, increased health care costs, and may contribute to leaving works prematurely, as well as increased 1-year mortality [1,2,3,4]. POCD is more prevalent in the elderly, but its pathogenesis is still unclear. Early POCD observed within 3 months after surgery can occur in adult surgical patients [1]. When POCD occurs in middle-aged patients during their working years, there are greater social and economic losses from reduced social activity and disengagement from work. However, the incidence and the risk factors for POCD in middle-aged patients have not been fully investigated. Identifying these risk factors can guide patients to make informed decisions prior to major surgery, as well as allow medical providers to provide additional support to high-risk patients during their post-operative recovery.
Mild cognitive impairment (MCI) is garnering a lot of interest and is referred to as the intermediate stage between normal cognition and dementia. These patients do not have dementia and are able to maintain activities of daily living; however, neuropsychological testing objectively confirms cognitive decline [5]. MCI predicts future cognitive decline for Alzheimer's disease, which is the most common cause of dementia, vascular dementia, other rare dementias, or a combination of these. MCI progresses to Alzheimer’s disease at an estimated rate of 10–15% per year in the general elderly population [6, 7]. Although the prevalence of MCI increases with age, its prevalence ranges from 7 to 33% in the middle-aged population [8,9,10]. Moreover, patients undergoing cardiac surgery already have cognitive decline due to their cardiovascular risk [11, 12], suggesting a higher frequency of MCI in middle-aged patients undergoing cardiac surgery. However, the association between MCI and the development of POCD in middle-aged patients remains unclear.
The purpose of this study was to retrospectively identify the incidence and risk factors for early POCD in middle-aged patients undergoing cardiac surgery. In addition, we examined whether MCI is associated with the development of early POCD in middle-aged patients.
Materials and methods
Patients
The Medical Ethics Committee of the Kumamoto Chuo Hospital approved the study protocol (No 60–04). The requirement for written informed consent was waived because of the retrospective nature of study. In Kumamoto Chuo Hospital, preoperative magnetic resonance imaging (MRI), MR angiography (MRA), and pre- and post-operative neuropsychological tests have been performed routinely in all patients who underwent elective cardiac surgery.
Data were examined retrospectively from 110 consecutive patients aged 46–64 years who underwent elective cardiac surgery by a single surgeon between January 2012 and June 2017. These included cases of coronary artery grafting with or without cardiopulmonary bypass (CPB), valve repair, and replacement. We excluded patients with congenital heart diseases, aortic surgeries, cardiac tumors, renal failures requiring dialysis, vison defects, physical disabilities, or poor conditions unfit for testing. Subjects were also excluded if their preoperative Mini-Mental Score Examination score was less than 26 points.
We gathered the following demographic and clinical information: age, sex, education level, obesity (body mass index > 25), smoking (previous or current), history of hypertension with medication, diabetes mellitus (with medication or strict dietary remedy), dyslipidemia (total cholesterol ≥ 220 mg/dl, triglyceride ≥ 150 mg/dl, or antihyperlipidemic therapy), estimated glomerular filtration rate, atrial fibrillation, peripheral artery disease (resting ankle–brachial pressure index < 0.90 or previous surgical treatment), history of cerebrovascular disease with stroke or transient ischemic attack, score in Mini-Mental State Examination, and prevalence of MCI. The following intraoperative and post-operative variables were also evaluated: type of surgery, operative time, CPB time, length of ICU stay, and length of hospital stay.
Neuropsychological testing
Patients underwent the following neuropsychological tests 24 h before surgery and at 1 week after surgery after the effects of sedatives have worn off. The test battery included several cognitive domains as recommended in an expert consensus statement [13]. Verbal memory was measured through digit span subtests of the Wechsler memory Scale-Revised that require short-term memory (digit span forward) and working memory (digit span backward). Attentional performance was assessed with the digit symbol substitution test of the Wechsler Adult Intelligence Scale, in which participants transcribed number–symbol pairs under timed conditions. The Kana Pick-out test measured executive function. Patients read a children’s fable and picked out all vowels, while also remembering the meaning of sentences. In the Trail Making Test A and B, participants connect numbered and then alternately numbered and lettered dots in order under timed conditions to assess attention and mental flexibility. All the tests were repeated postoperatively by a single investigator, who was blinded to the surgical procedure performed.
MCI was defined as performance 1.5 standard deviations (SD) below population means on any cognitive domain on the neurocognitive battery. This definition was based on a diagnostic guideline for MCI and dementia related to Alzheimer’s disease by the National Institute on Aging- Alzheimer’s Association [14]. POCD was defined as a decrease of 1 SD population means in at least two out of six variables in the test battery [2, 15]. This definition is associated with fewer false-positive results than alternative definitions [16].
Magnetic resonance imaging scans
MRI and MRA scans were obtained 1–14 days before surgery using a 1.5 T system. The imaging protocol included turbo fluid-attenuated inversion recovery (FLAIR) and T2-weighted turbo spin echo sequences. MRA included intracranial and neck vessels and was performed using a three-dimensional, time-of-flight technique. The MRI findings (FLAIR and T2) were classified as no infarct, some infarcts with a diameter ≥ 3 mm, or multiple infarcts. The degree of stenosis of intracranial arteries was graded bilaterally from MRA as normal or mild narrowing < 50%, moderate narrowing ≥ 50%, or occluded [17]. The degree of stenosis in the carotid arteries was graded based on MRA as normal or mild narrowing < 50%, moderate narrowing of 50–75%, severe narrowing (> 75%) or obstructed [18, 19]. A Fazekas rating scale was used to grade the lesion load of MRI hyper-intensities in the white matter of the brain [20]. White matter lesions were defined as punctate foci of MRI hyper-intensities, beginning confluence of foci, and large confluent areas. The apparent lesions on MRI and MRA were the consensus of two experienced neuroradiologists blinded to the clinical and neuropsychological data.
Anesthesia and sedation management
All of the patients were pre-medicated with 6 mg of morphine intramuscularly. Diazepam and fentanyl were used for induction and maintenance of anesthesia, supplemented with propofol or sevoflurane during surgery. After surgery, sedation was maintained with propofol. After ICU admission, sedation was adjusted with propofol to Richmond Agitation-Sedation Scale 0 to -2 until extubation.
Statistical analysis
We used all available data to maximize the power and generalizability of the results. Demographic and perioperative parameters were compared between those with and without POCD using Student’s t-test or Mann–Whitney U test for continuous data and χ2 test or Fisher exact test for discrete variables. To identify the risk factors of POCD in middle-age patients, a multivariate logistic analysis was performed. Prior studies showed that age, education, cerebrovascular disease, operative time, and preexisting cognitive impairment were risk factors for POCD [21], and those had been candidates as cofounders before the analysis. However, because of concerns about overfitting in our sample size, we ultimately included age, cerebral infarction, and MCI in the model based on our previous study [12]. All probabilities were two-tailed, with P-value < 0.05 considered statistically significant. All statistical analyses were performed with EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan) [22], which is a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria). More precisely, it is a modified version of R commander designed to add statistical functions frequently used in biostatistics.
Results
Out of the 110 patients, 39 patients were excluded from the analysis because of the following reasons: eleven had congenital heart disease, aortic aneurysm, or cardiac tumors, eight had renal failure requiring dialysis, three had a visual disorder or physical disability, 14 had a low MMSE score (< 26), two were unable to participate in post-operative neurocognitive assessments because of their poor condition, and one had missing data. Accordingly, 71 patients were included in the final data analysis, with a mean age of 58.4 years (SD: 4.4). The study group included 23 women and 48 men.
POCD was identified in 25 out of 71 patients (35%). Table 1 showed baseline characteristics of patients with and without POCD. Patients with POCD had significantly higher rates of preoperative MCI. There were no differences between groups in age, gender, educational history, and type of surgical procedure.
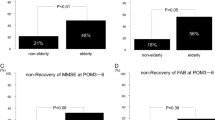
The neuropsychological test results before and one week after surgery compared between patients with and without POCD are shown in Table 2. At baseline, POCD patients had significantly lower Trail making B. The degree of decline in digit span backward, Trail making A, and Trail making B was significantly greater in POCD patients compared to non-POCD patients. Hence, POCD patients suffered from impaired attention and mental flexibility postoperatively.
The preoperative brain MRI findings are shown in Table 3. Notably, three patients with POCD patients and one patient without POCD did not undergo preoperative MRI evaluation. Patients with POCD had significantly higher rates of cerebral infarcts on MRI than patients without POCD.
The multivariate logistic analysis identified preoperative MCI (OR, 5.76: 95% CI 1.62–20.5; P < 0.001) and cerebral infarctions detected by MRI (OR, per grade 4.75; 95% CI 1.36–16.4; P = 0.01) as independent predictors of POCD. The respective variance inflation factors in the logistic regression model were checked and no multicollinearity was found. The result of the Hosmer–Lemeshow test was P = 0.349, and the ROC of a logistic regression model was fair discrimination of 0.779 for AUC (95% CI, 0.666–0.893).
Discussion
This study demonstrated that middle-aged patients who experienced POCD after cardiac surgery had significantly higher rates of preoperative MCI than patients who did not experience POCD. Furthermore, patients with POCD had significantly higher rates of preexisting cerebral infarcts on MRI than patients without POCD. Multivariate analysis revealed that preoperative MCI and cerebral infarctions were independent predictors of POCD. Of 71 middle-aged patients who underwent cardiac surgery, 25 (35%) were determined to have POCD. The incidence of early POCD in elderly patients undergoing cardiac surgery has been reported to be 20–50% [2, 22], although the reported incidence depends on a variety of factors including timing of measurement, assessment method used, and sensitivity of the assessment method. Our results are comparable to the incidences in elderly studies. In a large multicenter study (International Study of Post-Operative Cognitive Dysfunction [ISPOCD 1]), the incidence of POCD was 25.8% in patients aged 60 years or older who underwent various non-cardiac surgeries [23], and in the subsequent ISPOCD2, the incidence of POCD in middle-aged patients was 19.8% [24]. We should keep in mind that the incidence of early POCD in middle-aged patients is not much lower than that in elderly patients.
Pre-surgical cognitive function has been a factor of interest in predicting adverse surgical outcomes. Pre-surgical cognitive dysfunction in older adults has been associated with higher rates of post-operative delirium and cognitive decline, longer hospital stay, and reduced likelihood of hospital discharge [26,27,28]. In this study, pre-surgical cognitive dysfunction predicted POCD even in middle-aged adults. Therefore, given that middle-aged adults have significant responsibilities in the labor market and in the family, it is crucial to assess their pre-surgical cognitive function so that high-risk patients can receive the necessary medical support. In this study, the prevalence of MCI among middle-aged patients undergoing scheduled cardiac surgery was 52%, clearly higher than that of the same age group in the general population. Notably, this difference influenced the methods for assessing cognitive function. However, because of the systemic nature of atherosclerotic disease, the cardiovascular surgical population may be at particular risk for cognitive impairment. Moreover, the higher prevalence of MCI means that many of these patients will progress to dementia at a rate above population norms. Our findings support the recent research that in patients aged ≥ 55 years undergoing coronary artery bypass graft surgery, the prevalence of dementia at 7.5 years after surgery exceeded greatly exceeded population norms [29].
There are two possible reasons why cardiac patients are prone to preoperative cognitive decline. One is the possibility of neurodegenerative diseases such as MCI, as demonstrated in this study. It is well established that patients with MCI and Alzheimer’s disease have brain atrophy, particularly in the hippocampus. Recent structural MRI studies have shown decreased gray matter and whole brain volume in patients with coronary artery disease [30] and low cardiac output [31] who had significant cognitive decline. These findings suggest that neurodegenerative disease may be present in patients undergoing cardiac surgery with coronary disease or heart failure.
Another possibility is potential cerebrovascular disease. Patients undergoing cardiac surgery have a high rate of cerebrovascular complications due to their many cardiovascular risks. We previously reported that half of elderly patients undergoing cardiac surgery have symptomatic or asymptomatic cerebral infarction [32]. In the current study, the prevalence of cerebral infarction in middle-aged patients was 28%, which is still higher than the prevalence of 3–12% in the same age group [33, 34]. Maekawa et al. also showed that cerebral ischemic lesions on MRI in cardiac surgery patients were associated with preoperative cognitive impairment and an increased risk of POCD [12]. Notably, neurodegenerative disease and cerebrovascular disease overlap with each other and do not occur in isolation. The development of systemic atherosclerosis and presence of cardiac failure in patients undergoing cardiac surgery can lead to cerebral small vessel lesions, vascular endothelial damage, and chronic cerebral hypo-perfusion. Eventually, vascular cognitive impairment and neurodegenerative disease can develop at the end of this cascade [35]. In any case, a higher percentage of patients undergoing cardiac surgery have these potential cognitive vulnerabilities, and their risk of developing POCD and future dementia may be increased by surgical invasion [36].
This study has several limitations. The main limitation of this study was the small sample size. It could lead to potential type II errors, and only a limited range of variables were analyzed in the multivariate model. Second, the results may not be generalizable to other populations because of differences in the propensity or prevalence of certain diseases to cluster together from our single site cohort. Third, because of the retrospective study design, the subjective complaints of cognitive decline were not assessed. As the common definition of MCI includes subjective complaints [14], its prevalence in our study may be overestimated compared to population-based studies. Finally, the long-term effects of surgery and anesthesia on cognition in middle-aged patients with or without MCI are unknown, as this study did not include post-discharge follow-up. While a large twin study has determined that the effects of surgery are negligible [37], another study has reported post-operative cognitive decline in healthy middle-aged patients [38]. Further prospective studies stratifying the presence of preoperative cognitive impairment are needed to elucidate the impact of surgery on each cognitive trajectory.
In conclusion, preoperative MCI and infarcts on MRI were both associated with early POCD in middle-aged patients undergoing cardiac surgery. Neurodegenerative diseases and cerebrovascular disorders may be associated with the development of POCD. Preoperative neuropsychological testing is recommended to identify these vulnerable patients in middle-aged patients as well as in the elderly. Further studies are needed to determine whether interventions for preoperative MCI can improve post-operative neurological outcomes.
Data Availability
The data that support the fndings of this report are available from the corresponding author, N.H., upon reasonable request.
References
Monk TG, Weldon BC, Garvan CW, Dede DE, van der Aa MT, Heilman KM, Gravenstein JS. Predictors of cognitive dysfunction after major noncardiac surgery. Anesthesiology. 2008;108(1):18–30.
Newman MF, Kirchner JL, Phillips-Bute B, Gaver V, Grocott H, Jones RH, Mark DB, Reves JG, Blumenthal JA. Longitudinal assessment of neurocognitive function after coronary-artery bypass surgery. N Engl J Med. 2001;344(6):395–402.
Newman MF, Grocott HP, Mathew JP, White WD, Landolfo K, Reves JG, Laskowitz DT, Mark DB, Blumenthal JA. Report of the substudy assessing the impact of neurocognitive function on quality of life 5 years after cardiac surgery. Stroke. 2001;32(12):2874–81.
Steinmetz J, Christensen KB, Lund T, Lohse N, Rasmussen LS, ISPOCD Group. Long-term consequences of postoperative cognitive dysfunction. Anesthesiology. 2009;110(3):548–55.
Petersen RC, Smith GE, Waring SC, Ivnik RJ, Tangalos EG, Kokmen E. Mild cognitive impairment: clinical characterization and outcome. Arch Neurol. 1999;56(3):303–8.
Lopez OL, Kuller LH, Becker JT, Dulberg C, Sweet RA, Gach HM, Dekosky ST. Incidence of dementia in mild cognitive impairment in the cardiovascular health study cognition study. Arch Neurol. 2007;64(3):416–20.
Petersen RC, Roberts RO, Knopman DS, Boeve BF, Geda YE, Ivnik RJ, Smith GE, Jack CR. Mild cognitive impairment: ten years later. Arch Neurol. 2009;66(12):1447–55.
Lu Y, Liu C, Yu D, Fawkes S, Ma J, Zhang M, Li C. Prevalence of mild cognitive impairment in community-dwelling Chinese populations aged over 55 years: a meta-analysis and systematic review. BMC Geriatr. 2021;21(1):10.
González HM, Tarraf W, Schneiderman N, Fornage M, Vásquez PM, Zeng D, Youngblood M, Gallo LC, Daviglus ML, Lipton RB, Kaplan R, Ramos AR, Lamar M, Thomas S, Chai A, DeCarli C. Prevalence and correlates of mild cognitive impairment among diverse Hispanics/Latinos: study of latinos-Investigation of neurocognitive aging results. Alzheimers Dement. 2019;15(12):1507–15.
Szcześniak D, Rymaszewska J, Zimny A, Sąsiadek M, Połtyn-Zaradna K, Smith EE, Zatońska K, Zatoński T, Rangarajan S, Yusuf S, Szuba A. Cerebral small vessel disease and other influential factors of cognitive impairment in the middle-aged: a long-term observational cohort PURE-MIND study in Poland. GeroScience. 2021;43(1):279–95.
Rosengart TK, Sweet J, Finnin EB, Wolfe P, Cashy J, Hahn E, Marymont J, Sanborn T. Neurocognitive functioning in patients undergoing coronary artery bypass graft surgery or percutaneous coronary intervention: evidence of impairment before intervention compared with normal controls. Ann Thorac Surg. 2005;80(4):1327–35.
Maekawa K, Goto T, Baba T, Yoshitake A, Katahira K, Yamamoto T. Impaired cognition preceding cardiac surgery is related to cerebral ischemic lesions. J Anesth. 2011;25(3):330–6.
Murkin JM, Newman SP, Stump DA, Blumenthal JA. Statement of consensus on assessment of neurobehavioral outcomes after cardiac surgery. Ann Thorac Surg. 1995;59(5):1289–95.
Albert MS, DeKosky ST, Dickson D, Dubois B, Feldman HH, Fox NC, Gamst A, Holtzman DM, Jagust WJ, Petersen RC, Snyder PJ, Carrillo MC, Thies B, Phelps CH. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the national institute on aging-Alzheimer’s association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7(3):270–9.
Rasmussen LS, Larsen K, Houx P, Skovgaard LT, Hanning CD, Moller JT, ISPOCD group. The assessment of postoperative cognitive function. Acta Anaesthesiol Scand. 2001;45(3):275–89.
Lewis MS, Maruff P, Silbert BS, Evered LA, Scott DA. The sensitivity and specificity of three common statistical rules for the classification of post-operative cognitive dysfunction following coronary artery bypass graft surgery. Acta Anaesthesiol Scand. 2006;50(1):50–7.
Heiserman JE, Drayer BP, Keller PJ, Fram EK. Intracranial vascular stenosis and occlusion: Evaluation with three-dimensional time-of-flight MR angiography. Radiology. 1992;185(3):667–73.
Atlas SW. MR angiography in neurologic disease. Radiology. 1994;193(1):1–16.
Masaryk TJ, Lewin JS, Laub G. Magnetic resonance angiography. In: Stark DD, Bradley WG, editors. Magnetic resonance imaging. 2nd ed. St Louis: Mosby Year Book; 1992. p. 299–313.
Fazekas F, Chawluk JB, Alavi A, Hurtig HI, Zimmerman RA. MR signal abnormalities at 1.5 T in Alzheimer’s dementia and normal aging. AJR Am J Roentgenol. 1987;149(2):351–6.
Needham MJ, Webb CE, Bryden DC, (2017) Postoperative cognitive dysfunction and dementia: what we need to know and do. Br J Anaesth 119 (suppl_1) i115-i125
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48(3):452–8.
Rudolph JL, Schreiber KA, Culley DJ, McGlinchey RE, Crosby G, Levitsky S, Marcantonio ER. Measurement of post-operative cognitive dysfunction after cardiac surgery: a systematic review. Acta Anaesthesiol Scand. 2010;54(6):663–77.
Moller JT, Cluitmans P, Rasmussen LS, Houx P, Rasmussen H, Canet J, Rabbitt P,Jolles J, Larsen K, Hanning CD, Langeron O, Johnson T, Lauven PM, Kristensen PA, Biedler A, van Beem H, Fraidakis O, Silverstein JH, Beneken JE, Gravenstein JS. (1998) Long-term postoperative cognitive dysfunction in the elderly ISPOCD1 study. ISPOCD investigators. International Study of Post-Operative Cognitive Dysfunction. Lancet. Mar 351 (9106) 857–61.
Johnson T, Monk T, Rasmussen LS, Abildstrom H, Houx P, Korttila K, Kuipers HM, Hanning CD, Siersma VD, Kristensen D, Canet J, Ibañaz MT, Moller JT. Postoperative cognitive dysfunction in middle-aged patients. Anesthesiology. 2002;96(6):1351–7.
Culley DJ, Flaherty D, Fahey MC, Rudolph JL, Javedan H, Huang CC, Wright J, Bader AM, Hyman BT, Blacker D, Crosby G. Poor performance on a preoperative cognitive screening test predicts postoperative complications in older orthopedic surgical patients. Anesthesiology. 2017;127(5):765–74.
Silbert B, Evered L, Scott DA, McMahon S, Choong P, Ames D, Maruff P, Jamrozik K. Preexisting cognitive impairment is associated with postoperative cognitive dysfunction after hip joint replacement surgery. Anesthesiology. 2015;122(6):1224–34.
Zietlow K, McDonald SR, Sloane R, Browndyke J, Lagoo-Deenadayalan S, Heflin MT. Preoperative cognitive impairment as a predictor of postoperative outcomes in a collaborative care model. J Am Geriatr Soc. 2018;66(3):584–9.
Evered LA, Silbert BS, Scott DA, Maruff P, Ames D. Prevalence of dementia 7.5 years after coronary artery bypass graft surgery. Anesthesiology. 2016;125(1):62–71.
Vidal JS, Sigurdsson S, Jonsdottir MK, Eiriksdottir G, Thorgeirsson G, Kjartansson O, Garcia ME, van Buchem MA, Harris TB, Gudnason V, Launer LJ. Coronary artery calcium, brain function and structure: the AGES-Reykjavik study. Stroke. 2010;41(5):891–7.
Sabayan B, van Buchem MA, Sigurdsson S, Zhang Q, Harris TB, Gudnason V, Arai AE, Launer LJ. Cardiac hemodynamics are linked with structural and functional features of brain aging: the age, gene/environment susceptibility (AGES)-Reykjavik study. J Am Heart Assoc. 2015;4(1): e001294.
Ito A, Goto T, Maekawa K, Baba T, Mishima Y, Ushijima K. Postoperative neurological complications and risk factors for pre-existing silent brain infarction in elderly patients undergoing coronary artery bypass grafting. J Anesth. 2012;26(3):405–11.
DeCarli C, Massaro J, Harvey D, Hald J, Tullberg M, Au R, Beiser A, D’Agostino R, Wolf PA. Measures of brain morphology and infarction in the framingham heart study: establishing what is normal. Neurobiol Aging. 2005;26(4):491–510.
Smith EE, O’Donnell M, Dagenais G, Lear SA, Wielgosz A, Sharma M, Poirier P, Stotts G, Black SE, Strother S, Noseworthy MD, Benavente O, Modi J, Goyal M, Batool S, Sanchez K, Hill V, McCreary CR, Frayne R, Islam S, DeJesus J, Rangarajan S, Teo K, Yusuf S. Early cerebral small vessel disease and brain volume cognition and gait. Ann Neurol. 2015;77(2):251–61.
Tini G, Scagliola R, Monacelli F, Malfa GL, Porto I, Brunelli C, Rosa GM. Alzheimer’s disease and cardiovascular disease: a particular association. Cardiol Res Pract. 2020;2020:2617970.
Kuźma E, Airdrie J, Littlejohns TJ, Lourida I, Thompson-Coon J, Lang IA, Scrobotovici M, Thacker EL, Fitzpatrick A, Kuller LH, Lopez OL, Longstreth WT Jr, Ukoumunne OC, Llewellyn DJ. Coronary artery bypass graft surgery and dementia risk in the cardiovascular health study. Alzheimer Dis Assoc Disord. 2017;31(2):120–7.
Dokkedal U, Hansen TG, Rasmussen LS, Mengel-From J, Christensen K. Cognitive functioning after surgery in middle-aged and elderly Danish twins. Anesthesiology. 2016;124(2):312–21.
Bratzke LC, Koscik RL, Schenning KJ, et al. Cognitive decline in the middle-aged after surgery and anaesthesia: results from the wisconsin registry for Alzheimer’s prevention cohort. Anaesthesia. 2018;73(5):549–55.
Acknowledgements
The authors would like to thank Dr. Tatsuo Yamamoto for the valuable comments and suggestions.
Author information
Authors and Affiliations
Contributions
TO and KM contributed to the study conception and design. TO, KM, and YM conducted the study, data collection, and analysis. The first draft of the manuscript was written by TO and it was revised by KM and NH. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
There is no conflict of interest regarding the publication of this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Oyoshi, T., Maekawa, K., Mitsuta, Y. et al. Predictors of early postoperative cognitive dysfunction in middle-aged patients undergoing cardiac surgery: retrospective observational study. J Anesth 37, 357–363 (2023). https://doi.org/10.1007/s00540-023-03164-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-023-03164-w