Abstract
Background
Several reports on immunoglobulin (Ig)G4-related disease (IgG4-RD) with gastrointestinal involvement (IgG4-related gastrointestinal disease; IgG4-GID) have been published, although this entity has not been fully established clinicopathologically. Thus, we carried out a multicenter survey.
Methods
Patients with possible IgG4-GID who underwent resection were collected. Histologic slides were reevaluated, and eight cases with diffuse lymphoplasmacytic infiltration but without numerous neutrophils, granulations or epithelioid granulomas were further analyzed.
Results
Overall, the IgG4 counts (87–345/high-power field) and IgG4/IgG-positive ratio were high (44–115%). The demographic findings included advanced age among the patients (55–80 years) and male preponderance (six cases). Six lesions (five gastric, one esophageal), consisting of lymphoplasmacytic infiltration with neural involvement in the muscularis propria and/or bottom-heavy plasmacytosis in the gastric mucosa, were histologically regarded as highly suggestive of IgG4-RD. Storiform fibrosis and obliterative phlebitis were found in two cases, and the former gave rise to a 7-cm-sized inflammatory pseudotumor (IPT) in one case. Ulceration and carcinoma co-existed in three and two lesions, respectively. All the patients had other organ involvement (OOI), and serum IgG4 levels were markedly elevated (four of five patients). The remaining two cases with gastric IPTs featuring reactive nodular fibrous pseudotumor or nodular lymphoid hyperplasia were regarded as possible cases of IgG4-RD because of the histologic findings and lack of OOI.
Conclusions
IgG4-GID is found in the setting of IgG4-RD, often with ulceration or cancer. Characteristic histologic findings are observed in the muscularis propria and gastric mucosa. Cases with IPT may be heterogeneous, and there may be mimickers of IgG4-GID.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Immunoglobulin (Ig)G4-related disease (IgG4-RD) is a systemic inflammatory condition of unknown etiology characterized by abnormal increases in serum IgG4 and in the number of IgG4-positive cells in affected tissues [1, 2]. Common locations of involvement are the pancreas, biliary tract, salivary glands, retroperitoneum, aorta, kidney, orbit and lung, but other organs may also be involved.
Gastrointestinal (GI) tract involvement of IgG4-RD (IgG4-related GI disease, IgG4-GID) is rare, but is known to occur based on anecdotal case reports. The clinical descriptions of IgG4-GID in these reports range widely and include ulceration [3,4,5,6,7,8], polyps [9, 10], wall thickening [5, 11,12,13,14,15,16], submucosal tumor [8, 17,18,19,20,21,22,23,24,25,26,27], GI obstruction due to extramural inflammation [28], vasculitis [6, 29, 30], fistula [7] and increases in IgG4-positive cells without obvious morphologic abnormalities [31, 32]. Some authors have argued that preexisting entities of GI inflammation, such as reactive nodular fibrous pseudotumor [33,34,35], calcifying fibrous pseudotumor [36,37,38] and enterocolic lymphocytic phlebitis [29, 30], may represent IgG4-GID. In most of these reports, the diagnosis of IgG4-GID depended on immunostaining for IgG4. However, other inflammatory conditions that involve the GI tract, such as inflammatory bowel disease [39,40,41], celiac disease [42], Rosai-Dorfman disease [43, 44] and Cronkhite-Canada syndrome [45], may also reveal the same phenomenon, suggesting that an increase in IgG4-positive cells alone is not specific to IgG4-GID. Thus, the concept of IgG4-GID is still vague and needs to be characterized through a series of cases.
For diagnosing IgG4-RD, histologic features are important because, as stated in the previous paragraph, elevated serum IgG4 or an increase in IgG4-positive cells may be observed in other diseases. In particular, storiform fibrosis and obliterative phlebitis are pathologically so important that they are adopted in the consensus statement for the pathologic diagnosis of IgG4-RD [46] and occur in some organospecific diagnostic criteria of IgG4-RD, such as autoimmune pancreatitis (AIP) [47], sclerosing cholangitis [48] and renal disease [49]. However, at the same time, the histologic features of IgG4-RD are different depending on the organs involved. For instance, storiform fibrosis and obliterative phlebitis are almost always absent in IgG4-related ophthalmic disease [50]. Unfortunately, such histologic data are lacking in IgG4-GID.
Thus, to clarify the clinicopathologic features of IgG4-GID, we carried out a study by collecting possible cases of IgG4-GID from among the members of the Research Committee of IgG4-RD sponsored by Health and Labour Sciences Research Grants (Intractable Diseases) from Japan’s Ministry of Health, Labour and Welfare and the Committee for AIP of the Japan Pancreas Society.
Methods
This study was approved by the Ethical Review Boards of Kyoto University Graduate School of Medicine, Tokyo Metropolitan Komagome Hospital and Kurashiki Central Hospital.
Case selection
Each member was asked to provide cases with a tumor or marked wall thickening in the GI tract that was resected and showed at least ten IgG4-positive cells in a high-power field (HPF). The author groups of case reports of possible IgG4-GID that were searched for using a database (ICHUSHI) provided by the Japan Medical Abstracts Society were also invited to join this project. Hematoxylin-eosin (H&E)-stained slides and immunostained slides for IgG4 and IgG underwent histologic reevaluation. Clinical data were provided through a questionnaire.
Pathologic examination
Cases with at least one of the following three histologically inconsistent features with the diagnosis of IgG4-RD were excluded: (1) lack of diffuse lymphoplasmacytic infiltration, (2) presence of marked neutrophilic infiltration and/or formation of granulation tissue except for areas around ulcerations and (3) presence of granulomas, including xanthogranulomatous inflammation. Cases with IgG4-positive cells > 50/HPF and IgG4/IgG-positive cell ratio > 40% observed in the three foci with the most abundant IgG4-positive cells [46] were regarded as possible IgG4-GID, and if storiform fibrosis, obliterative phlebitis and/or perineural inflammation was further present, cases were regarded as highly suggestive of IgG4-GID.
Results
Pathologic findings (Table 1)
Eight cases that lacked all exclusion criteria remained for further evaluation. In all the specimens, the number of IgG4-positive cells was > 50/HPF (range: 87–345/HPF) and the IgG4/IgG-positive cell ratio was > 40% (range: 44–115%). The lesions were located in the stomach (seven cases, including a case that also involved the duodenum) and esophagus (one case, case 6). Four of these (cases 2, 3, 5, and 6) were published previously as case reports [15, 16, 27, 51].
Cases with highly suggestive histologic features of IgG4-GID (cases 1–6)
There were five gastric lesions and one esophageal lesion. Three cases (cases 1, 2 and 6) had ulceration, and two other cases (cases 3 and 4) were accompanied by intramucosal adenocarcinoma.
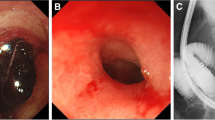
The muscularis propria was the main location of inflammation in every case, and the subserosa was also involved in one case (case 5). The histologic features comprised strands of dense lymphoplasmacytic infiltration within the thickened muscularis propria (striated inflammatory lesion; Fig. 1a, b). Notably, inflammatory cells that had infiltrated around the myenteric nerve plexus were easily identified in all of the cases (Fig. 1b). The smooth muscle cells and peripheral nerve parenchyma did not seem to be severely damaged. Eosinophilic infiltration was identified in all the cases.
Cases with highly suggestive histologic features of IgG4-GID in the muscularis propria. a, b Striated inflammatory lesion within the well-preserved muscularis propria. The infiltration contained plasma cells, lymphocytes and eosinophils. The myenteric nerve plexus was always involved in the inflammation (b). c A portion of a mass (IPT) with storiform fibrosis in case 5. d Numerous IgG4-positive cells were found in every case
Storiform fibrosis (Fig. 1c) and obliterative phlebitis were found focally in the muscularis propria in two cases (cases 4 and 5) and one case (case 5), respectively. In case 5, storiform fibrosis gave rise to a 7-cm-sized inflammatory pseudotumor (IPT). IgG4-positive cells were numerous and were diffusely distributed in every case (Fig. 1d); the average number of IgG4-positive cells was 235/HPF (range: 149–345), and the average ratio of IgG4/IgG-positive cells was 86% (range: 64–115).
In three gastric cases (cases 2, 4 and 5), we also identified a unique inflammatory lesion in the mucosal lamina propria that was distinct from Helicobacter pylori-associated gastritis. Rather than the typical superficial inflammation seen in cases with H. pylori-associated gastritis, plasma cells were found aggregating in the deeper portion of the mucosa (bottom-heavy plasmacytosis; Fig. 2a). In two cases (cases 4 and 5), numerous eosinophils were also intermingled at the bottom of the mucosa (Fig. 2b). In two cases (cases 4 and 5), small aggregates of lymphoplasmacytic infiltration were also found beneath the muscularis mucosae (Fig. 2c), where storiform fibrosis and obliterative phlebitis were focally identified in both cases and one case (case 4), respectively. IgG4-positive cells were numerous (190/HPF), and the IgG4/IgG-positive cell ratio was high (88%) in one case (case 4) in which immunohistochemical evaluation was available for the mucosal portion. In the background mucosa, active chronic gastritis or chronic atrophic gastritis with intestinal metaplasia was found in two cases (cases 4 and 5), but no evidence of gastritis was found in one case (case 2).
Bottom-heavy plasmacytosis in the mucosal lamina propria. a Dense plasmacytic infiltration was found at the deeper portion of the mucosal lamina propria. b Numerous eosinophils were intermingled in two cases. c The shallow level of the submucosa was commonly involved. d In case 4, a signet-ring cell carcinoma found at the upper portion collided with the bottom-heavy inflammation
Cases with possible histologic features of IgG4-GID (cases 7 and 8)
Both of these cases seemed to be IPTs with a transmural lesion. Storiform fibrosis, obliterative phlebitis and perineural inflammation were absent.
In case 7, the preexisting architecture, including the muscularis propria, almost completely disappeared and was replaced predominantly by keloidal fibrosis with a nodular configuration (Fig. 3a). In some foci, aggregates of lymphocytes, plasma cells and lymphoid follicles were observed (Fig. 3b). These histologic findings were consistent with reactive nodular fibrous pseudotumor [33,34,35]. IgG4-positive cells were numerous (87/HPF), and the IgG4/IgG-positive cell ratio was high (44%).
Cases with possible histologic features of IgG4-GID. In case 7, keloidal fibrosis with a nodular configuration was the histologic feature (a). Aggregates of numerous lymphocytes, plasma cells and lymphoid follicles were found focally (b). Case 8 comprised nodular lymphoid follicular hyperplasia with intervening dense fibrosis (c). IgG4-positive cells were numerous (d)
In case 8, a mass consisting of florid follicular hyperplasia was present in the mucosa through subserosa (Fig. 3c). The lesion appeared to be lobulated by the intervening dense fibrosis. Plasma cells were numerous between the follicles. The number of IgG4-positive cells was markedly increased (266/HPF; Fig. 3d), and the IgG4/IgG-positive cell ratio was also high (84%).
Clinical and imaging findings (Table 2)
The median age of the eight patients was 71.5 years (range: 55–80), and six of the patients were male. Two patients (cases 1 and 6) had GI symptoms, such as increasing abdominal pain or dysphagia. The other six patients were free from GI symptoms, and the lesions were incidentally detected radiologically or pathologically. Computed tomographic (CT) scans demonstrated wall thickening (cases 1, 2 and 6) or a submucosal tumor (cases 5, 7 and 8). All three cases in which a CT scan demonstrated wall thickening histologically showed a striated inflammatory lesion.
Other organ involvement (OOI) in IgG4-RD was exclusively identified in the six cases with highly suggestive histologic features of IgG4-GID. Among the six patients with OOIs, serum IgG4 was examined in five and was markedly elevated (> 1000 mg/dl) in four who had multiple OOIs. Serum IgG4 was also mildly elevated (215 mg/dl) in one patient (case 8) with possible histologic features and without OOIs.
Follow-up information was available in six patients (average follow-up period: 3.3 years), and no patients had recurrent disease in the GI tract. Cases 1 and 4 developed OOIs 7 and 5 years after the surgery, respectively. Four patients in total were treated with a corticosteroid for OOIs. The treatment was effective in three patients, but one patient died of infection during the treatment.
Discussion
According to the consensus statement [46], four criteria were proposed by which IgG4-RD could be recognized in previously unrecognized organs: (1) characteristic histologic findings (notably storiform fibrosis and obliterative phlebitis), numerous IgG4-positive cells and an elevated IgG4/IgG-positive cell ratio; (2) an elevated serum IgG4 level; (3) an effective response to corticosteroid; (4) the coexistence of OOIs of IgG4-RD. Six cases with highly suggestive histologic features in the present series fulfilled three of the four criteria. Storiform fibrosis and obliterative phlebitis were identified in two cases. Both the number of IgG4-positive cells (the minimum criterion in the consensus statement is 50/HPF in the resected tissues of most organs) and the ratio of IgG4/IgG-positive cells (> 40% in the consensus statement) were far more than satisfactory in every case. All of the patients had OOIs (multiple lesions in most cases) that were typical for IgG4-RD, and the serum IgG4 level was markedly (> 1000 mg/dl) elevated in four of five patients for whom such data were available. The only patient (case 6) whose serum IgG4 was not elevated had a history of retroperitoneal fibrosis. When the operation was conducted, the esophagus was the only location of active disease, and it is conceivable that the serum IgG4 level was not elevated. In addition, these six cases had other consistent demographic and clinical features of IgG4-RD, such as advanced age (68–80 years), male preponderance (five cases) and no GI symptoms (four cases). Although the lesions were resected and we could not assess the steroid responsiveness, our cases with highly suggestive histologic features are likely to be examples of IgG4-GID.
In addition to storiform fibrosis and obliterative phlebitis, we included perineural inflammation as a supportive histologic finding of IgG4-GID. This is because the peripheral nerve involvement is one of the characteristic features of IgG4-RD in general, and it has been described in IgG4-related ophthalmic disease [50, 52], retroperitoneal fibrosis [53] and systematically (including the GI tract) in an IgG4-RD patient [54]. As a result, five cases with the striated inflammatory lesion were diagnosed as having highly suggestive histologic features. The diagnosis was justified by the development of storiform fibrosis out of the striated inflammatory lesion in two cases and OOIs in all patients.
We consider that the unique inflammation of the mucosal lamina propria in our three cases is similar to what Uehara and colleagues reported in gastritis cases in patients with AIP [55]. They found that mononuclear cell infiltration was significantly more common in the deeper portion of gastric mucosal biopsies in AIP patients compared to patients without AIP. They also identified a significantly increased IgG4/IgG-positive cell ratio in the deeper portion, which was also confirmed in one of our cases. In our series, a minute focus of submucosal involvement was found in two cases; such foci may give rise to a submucosal IPT [21].
Three and two lesions with highly suggestive histologic features were associated with ulceration and carcinoma, respectively. It is difficult to speculate on the causal relationship between IgG4-GID and ulceration or carcinoma, which could be incidental. The frequent complication of gastric ulcer was reported in patients with AIP by two groups [56, 57]. According to the reports, wall thickening was not a feature in these patients except in one, who, similarly to our cases, had marked wall thickening simulating scirrhous carcinoma [56]. In addition, Lee and colleagues reported an esophageal lesion with wall thickening and ulceration, which was confirmed histologically to be a fibrosing inflammation with plexitis and numerous IgG4-positive cells [12]. This case resembles our case 6. One hypothesis regarding the relationship between IgG4-GID and carcinoma is that the latter is the cause of the former. Patients with AIP are at a higher risk of malignancy, especially in the first year after the diagnosis of AIP, which suggests that AIP may be a paraneoplastic reaction rather than a cause of malignancy [58]. However, we could not find any case reports of IgG4-GID in patients with gastrointestinal malignancies. This may be because the immune responses seen around carcinomas may be easily regarded as reactions against carcinomas, and thus immunohistochemical evaluation for IgG4-RD was not performed.
The two cases with the possible histologic features of IgG4-GID (cases 7 and 8) were pathologically different from the others. Case 7 seems to be an example of a reactive nodular fibrous pseudotumor [33,34,35], which rarely involves the stomach [59]. Case 8 resembled pulmonary nodular lymphoid hyperplasia. It is tempting to consider the reactive nodular fibrous pseudotumor and pulmonary nodular lymphoid hyperplasia to be examples of IgG4-RD, because in those cases both the number of IgG4-positive cells and the ratio of IgG4/IgG-positive cells were high enough to qualify as IgG4-RD. In fact, we know that some groups reported these entities to be IgG4-RD [19, 60]. However, we hesitate to consider our cases IgG4-RD because the keloidal fibrosis predominantly seen in our case 7 is believed to be unlikely in IgG4-RD [61]. Regarding case 8, we agree with Calvo and colleagues that the histologic findings of nodular lymphoid hyperplasia are not suggestive of IgG4-RD [62]. More importantly, we are not aware of such lesions occurring in patients with obvious IgG4-RD. We need more data to be able to conclude whether reactive nodular fibrous pseudotumors and nodular fibrous pseudotumors are truly examples of IgG4-RD. From the clinical standpoint, we did not see any features that called into question the diagnosis of IgG4-RD, although OOIs were absent. It thus seems fair to conclude that these two lesions are histologically possible examples of IgG4-GID.
Although IPT is a well-known manifestation of IgG4-RD, further research on IPT cases in the GI tract is necessary. Except for cases in our series, we found 14 cases of IgG4-related IPT/inflammatory masses of the GI tract reported in the literature [17,18,19,20,21,22,23,24,25,26]. All of these lesions consisted of lymphoplasmacytic infiltration and fibrosis with numerous IgG4-positive cells. Although IgG4-RD is common among elderly males, three of these patients were younger than 30 years old, and females (8 out of 14 patients) were more commonly affected. Unusual clinical findings, such as acute illness and severe clinical symptoms, were also observed in some of these patients, and none of them had definite OOIs of IgG4-RD. We therefore suggest that tumefactive inflammatory lesions in the GI tract are diverse and that cases with the typical histologic features (storiform fibrosis, obliterative phlebitis and/or perineural inflammation) mainly involving the muscularis propria in the appropriate clinical setting can be reliably diagnosed as IgG4-GID at the present time.
IgG4-GID was found in patients with IgG4-RD. In one patient (case 1), the former was the first manifestation of the latter. In three cases, CT scans depicted wall thickening, which corresponded to the striated inflammatory lesion in the thickened muscularis propria. In cases with such an imaging finding, IgG4-GID needs to be included in the differential diagnosis. A CT scan may also demonstrate a mass in IgG4-GID cases, but on this occasion, the differential diagnosis may include other entities that belong under the umbrella category “IPT” as well as neoplastic conditions. Interestingly, ulceration or cancer was commonly associated; such findings can be clues to identifying IgG4-GID. The prognosis of IgG4-GID was excellent, and no recurrence of the GI lesions was found. To properly distinguish IgG4-GID from malignancy, we propose that IgG4-GID must be acknowledged as a clinical entity. In the diagnosis of IgG4-GID, the detection of bottom-heavy plasmacytosis by gastric biopsy may be useful.
In conclusion, IgG4-GID is found in the setting of IgG4-RD, often with ulceration or cancer. Two unique histologic patterns were identified: (1) a striated inflammatory lesion in the muscularis propria that gives rise to thickening of the layer and (2) bottom-heavy plasmacytosis in the mucosa. The former finding may be depicted as wall thickening on imaging studies, and IgG4-GID is a differential diagnosis in cases with such a findings. IgG4-related IPT may arise in the background of these histologic patterns of inflammation, but one should be cautious when diagnosing it because there may be other entities that show a tumefactive inflammation with numerous IgG4-positive cells. Among IPTs in the GI tract, the diagnosis of IgG4-GID is likely in cases with typical storiform fibrosis, obliterative phlebitis and/or perineural inflammation in the appropriate clinical settings.
References
Kamisawa T, Zen Y, Pillai S, et al. IgG4-related disease. Lancet. 2015;385(9976):1460–71.
Kamisawa T, Chari ST, Lerch MM, et al. Recent advances in autoimmune pancreatitis: type 1 and type 2. Gut. 2013;62(9):1373–80.
Fujita T, Ando T, Sakakibara M, et al. Refractory gastric ulcer with abundant IgG4-positive plasma cell infiltration: a case report. World J Gastroenterol. 2010;16(17):2183–6.
Bateman AC, Sommerlad M, Underwood TJ. Chronic gastric ulceration: a novel manifestation of IgG4-related disease? J Clin Pathol. 2012;65(6):569–70.
Fujita K, Naganuma M, Saito E, et al. Histologically confirmed IgG4-related small intestinal lesions diagnosed via double balloon enteroscopy. Dig Dis Sci. 2012;57(12):3303–6.
Wong DD, Pillai SR, Kumarasinghe MP, et al. IgG4-related sclerosing disease of the small bowel presenting as necrotizing mesenteric arteritis and a solitary jejunal ulcer. Am J Surg Pathol. 2012;36(6):929–34.
Frydman J, Grunner S, Kluger Y. IgG4-related disease manifesting as an acute gastric-pericardial fistula. World J Gastroenterol. 2014;20(44):16782–5.
Yang L, Jin P, Sheng JQ. Immunoglobulin G4-related disease (IgG4-RD) affecting the esophagus, stomach, and liver. Endoscopy. 2015;47(Suppl 1):E96–7.
Kaji R, Okabe Y, Ishida Y, et al. Autoimmune pancreatitis presenting with IgG4-positive multiple gastric polyps. Gastrointest Endosc. 2010;71(2):420–2.
Ueno K, Watanabe T, Kawata Y, et al. IgG4-related autoimmune pancreatitis involving the colonic mucosa. Eur J Gastroenterol Hepatol. 2008;20(11):1118–21.
Baez JC, Hamilton MJ, Bellizzi A, et al. Gastric involvement in autoimmune pancreatitis: MDCT and histopathologic features. JOP. 2010;11(6):610–3.
Lee H, Joo M, Song TJ, et al. IgG4-Related sclerosing esophagitis: a case report. Gastrointest Endosc. 2011;73(4):834–7.
Ko Y, Woo JY, Kim JW, et al. An immunoglobulin G4-related sclerosing disease of the small bowel: CT and small bowel series findings. Korean J Radiol. 2013;14(5):776–80.
Hiyoshi Y, Oki E, Zaitsu Y, et al. IgG4-related disease of the ileocecal region mimicking malignancy: a case report. Int J Surg Case Rep. 2014;5(10):669–72.
Kawano H, Ishii A, Kimura T, et al. IgG4-related disease manifesting the gastric wall thickening. Pathol Int. 2016;66(1):23–8.
Inoue K, Okubo T, Kato T, et al. IgG4-related stomach muscle lesion with a renal pseudotumor and multiple renal rim-like lesions: a rare manifestation of IgG4-related disease. Mod Rheumatol. 2015. https://doi.org/10.3109/14397595.2015.1081743
Lopes J, Hochwald SN, Lancia N, et al. Autoimmune esophagitis: IgG4-related tumors of the esophagus. J Gastrointest Surg. 2010;14(6):1031–4.
Rollins KE, Mehta SP, O’Donovan M, et al. Gastric IgG4-related autoimmune fibrosclerosing pseudotumour: a novel location. ISRN Gastroenterol. 2011;2011:873087.
Chetty R, Serra S, Gauchotte G, et al. Sclerosing nodular lesions of the gastrointestinal tract containing large numbers of IgG4 plasma cells. Pathology. 2011;43(1):31–5.
Kim do H, Kim J, Park do H, et al. Immunoglobulin G4-related inflammatory pseudotumor of the stomach. Gastrointest Endosc. 2012;76(2):451–2.
Na KY, Sung JY, Jang JY, et al. Gastric nodular lesion caused by IgG4-related disease. Pathol Int. 2012;62(10):716–8.
Oh JH, Lee TH, Kim HS, et al. Esophageal involvement of immunoglobulin G4-related disease: a case report and literature review. Medicine. 2015;94(50):e2122.
Cheong HR, Lee BE, Song GA, et al. Immunoglobulin G4-related inflammatory pseudotumor presenting as a solitary mass in the stomach. Clin Endosc. 2016;49(2):197–201.
Otsuka R, Kano M, Hayashi H, et al. Probable IgG4-related sclerosing disease presenting as a gastric submucosal tumor with an intense tracer uptake on PET/CT: a case report. Surg Case Rep. 2016;2(1):33.
Woo CG, Yook JH, Kim AY, et al. IgG4-related disease presented as a mural mass in the stomach. J Pathol Transl Med. 2016;50(1):67–70.
Choi SB, Lim CH, Cha MG, et al. IgG4-related disease of the rectum. Ann Surg Treat Res. 2016;90(5):292–5.
Inoue D, Yoneda N, Yoshida K, et al. Imaging and pathological features of gastric lesion of immunoglobulin G4-related disease: a case report and review of the recent literature. Mod Rheumatol. 2016. https://doi.org/10.1080/14397595.2016.1209819
Coulier B, Montfort L, Beniuga G, et al. Small bowel obstruction caused by peritoneal immunoglobulin g4-related disease mimicking carcinomatosis: case report. Korean J Radiol. 2014;15(1):66–71.
Comtesse S, Friemel J, Fankhauser R, et al. Enterocolic lymphocytic phlebitis of the cecal pole and appendix vermiformis with increase of IgG4-positive plasma cells. Virchows Arch. 2014;464(1):113–6.
Laco J, Orhalmi J, Bartova J, et al. Enterocolic lymphocytic phlebitis as a newly recognized manifestation of IgG4-related disease. Int J Surg Pathol. 2015;23(2):165–9.
Kamisawa T, Funata N, Hayashi Y, et al. A new clinicopathological entity of IgG4-related autoimmune disease. J Gastroenterol. 2003;38(10):982–4.
Kamisawa T, Nakajima H, Egawa N, et al. IgG4-Related sclerosing disease incorporating sclerosing pancreatitis, cholangitis, sialadenitis and retroperitoneal fibrosis with lymphadenopathy. Pancreatology. 2006;6(1–2):132–7.
Yantiss RK, Nielsen GP, Lauwers GY, et al. Reactive nodular fibrous pseudotumor of the gastrointestinal tract and mesentery: a clinicopathologic study of five cases. Am J Surg Pathol. 2003;27(4):532–40.
Daum O, Vanecek T, Sima R, et al. Reactive nodular fibrous pseudotumors of the gastrointestinal tract: report of 8 cases. Int J Surg Pathol. 2004;12(4):365–74.
Saglam EA, Usubutun A, Kart C, et al. Reactive nodular fibrous pseudotumor involving the pelvic and abdominal cavity: a case report and review of literature. Virchows Arch. 2005;447(5):879–82.
Acenero MJ, Vorwald PW, Yamauchi SC. Calcifying fibrous pseudotumor affecting the retroperitoneum: could it be a new entity within the spectrum of IgG-4 sclerosing disease? Virchows Arch. 2010;456(6):719–21.
Larson BK, Balzer B, Goldwasser J, et al. Calcifying fibrous tumor: an unrecognized IgG4-related disease? APMIS. 2015;123(1):72–6.
Zhang H, Jin Z, Ding S. Gastric calcifying fibrous tumor: a case of suspected immunoglobulin G4-related gastric disease. Saudi J Gastroenterol. 2015;21(6):423–6.
Navaneethan U, Liu X, Bennett AE, et al. IgG4-Associated ampullitis and cholangiopathy in Crohn’s disease. J Crohns Colitis. 2011;5(5):451–6.
Kuwata G, Kamisawa T, Koizumi K, et al. Ulcerative colitis and immunoglobulin G4. Gut Liver. 2014;8(1):29–34.
Topal F, Saritas Yuksel E, Ekinci N, et al. The prevalence of IgG4-positive plasma cell infiltrates in inflammatory bowel disease patients without autoimmune pancreatitis. Turk J Gastroenterol. 2014;25(5):558–62
Demirci H, Polat Z, Ozturk K, et al. The degree of mucosal damage to the small intestine and serum immunoglobulin G4 levels correlate with celiac disease. Eur J Gastroenterol Hepatol. 2015;27(7):781–4.
Wimmer DB, Ro JY, Lewis A, et al. Extranodal rosai-dorfman disease associated with increased numbers of immunoglobulin g4 plasma cells involving the colon: case report with literature review. Arch Pathol Lab Med. 2013;137(7):999–1004.
Zhao M, Li C, Zheng J, et al. Extranodal Rosai–Dorfman disease involving appendix and mesenteric nodes with a protracted course: report of a rare case lacking relationship to IgG4-related disease and review of the literature. Int J Clin Exp Pathol. 2013;6(11):2569–77.
Bettington M, Brown IS, Kumarasinghe MP, et al. The challenging diagnosis of Cronkhite–Canada syndrome in the upper gastrointestinal tract: a series of 7 cases with clinical follow-up. Am J Surg Pathol. 2014;38(2):215–23.
Deshpande V, Zen Y, Chan JK, et al. Consensus statement on the pathology of IgG4-related disease. Mod Pathol. 2012;25(9):1181–92.
Shimosegawa T, Chari ST, Frulloni L, et al. International consensus diagnostic criteria for autoimmune pancreatitis: guidelines of the International Association of Pancreatology. Pancreas. 2011;40(3):352–8.
Ohara H, Okazaki K, Tsubouchi H, et al. Clinical diagnostic criteria of IgG4-related sclerosing cholangitis 2012. J Hepatobiliary Pancreat Sci. 2012;19(5):536–42.
Kawano M, Saeki T, Nakashima H, et al. Proposal for diagnostic criteria for IgG4-related kidney disease. Clin Exp Nephrol. 2011;15(5):615–26.
Goto H, Takahira M, Azumi A. Diagnostic criteria for IgG4-related ophthalmic disease. Jpn J Ophthalmol. 2015;59(1):1–7.
Mori S, Tahashi Y, Uchida K, et al. Sclerosing esophagitis with IgG4-positive plasma cell infiltration: a case report. Intern Med 2017;56(22):3023–6
Watanabe T, Fujinaga Y, Kawakami S, et al. Infraorbital nerve swelling associated with autoimmune pancreatitis. Jpn J Radiol. 2011;29(3):194–201.
Zen Y, Onodera M, Inoue D, et al. Retroperitoneal fibrosis: a clinicopathologic study with respect to immunoglobulin G4. Am J Surg Pathol. 2009;33(12):1833–9.
Fujii M, Sato Y, Ohara N, et al. Systemic IgG4-related disease with extensive peripheral nerve involvement that progressed from localized IgG4-related lymphadenopathy: an autopsy case. Diagn Pathol. 2014;9:41.
Uehara T, Hamano H, Kawa S, et al. Chronic gastritis in the setting of autoimmune pancreatitis. Am J Surg Pathol. 2010;34(9):1241–9.
Shinji A, Sano K, Hamano H, et al. Autoimmune pancreatitis is closely associated with gastric ulcer presenting with abundant IgG4-bearing plasma cell infiltration. Gastrointest Endosc. 2004;59(4):506–11.
Chang MC, Chang YT, Wei SC, et al. Autoimmune pancreatitis associated with high prevalence of gastric ulcer independent of Helicobacter pylori infection status. Pancreas. 2009;38(4):442–6.
Shiokawa M, Kodama Y, Yoshimura K, et al. Risk of cancer in patients with autoimmune pancreatitis. Am J Gastroenterol. 2013;108(4):610–7.
Gauchotte G, Bressenot A, Serradori T, et al. Reactive nodular fibrous pseudotumor: a first report of gastric localization and clinicopathologic review. Gastroenterol Clin Biol. 2009;33(12):1076–81.
Guinee DG Jr, Franks TJ, Gerbino AJ, et al. Pulmonary nodular lymphoid hyperplasia (pulmonary pseudolymphoma): the significance of increased numbers of IgG4-positive plasma cells. Am J Surg Pathol. 2013;37(5):699–709.
Deshpande V. IgG4-related disease of the gastrointestinal tract: a 21st century chameleon. Arch Pathol Lab Med. 2015;139(6):742–9.
Calvo J, Carbonell N, Scatton O, et al. Hepatic nodular lymphoid lesion with increased IgG4-positive plasma cells associated with primary biliary cirrhosis: a report of two cases. Virchows Arch. 2015;467(5):613–7.
Acknowledgements
This work was supported by Health and Labour Sciences Research Grants (Intractable Diseases) from Japan’s Ministry of Health, Labour and Welfare.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Notohara, K., Kamisawa, T., Uchida, K. et al. Gastrointestinal manifestation of immunoglobulin G4-related disease: clarification through a multicenter survey. J Gastroenterol 53, 845–853 (2018). https://doi.org/10.1007/s00535-017-1420-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-017-1420-4