Abstract
Purpose
Studies evaluating oncological inpatient rehabilitation rarely include follow-up intervals beyond 6 months and larger proportions of patients other than those with breast cancer. Therefore, this study investigated changes in health-related quality of life (HRQoL), depression, and fear of progression of patients with breast, colorectal, or prostate cancer from the beginning to the end of oncological rehabilitation and a 9-month follow-up.
Methods
Three hundred seventy-seven patients with breast, colorectal, or prostate cancer undergoing oncological inpatient rehabilitation (median age 61 years, 49% female) completed the EORTC QLQ-C30, the PHQ-9, and the FoP-Q-SF at each measurement point. Data analysis used 3 (tumor site) × 3 (time of measurement) repeated measures ANCOVAs with patient age and time since diagnosis as covariates. At each time point, we also compared our sample to the general population on the measures used.
Results
Having controlled for the covariates, we found significant effects of tumor site, which were small except for Diarrhea. Effects of time of measurement were often significant and in part at least medium in size indicating improvement of HRQoL and depression during rehabilitation. At follow-up, some HRQoL domains and depression deteriorated. Women with breast cancer, in particular, showed a greater decrease in emotional functioning then. Compared to the general population, the sample’s HRQoL and depression were significantly worse on most occasions.
Conclusion
Oncological inpatient rehabilitation may improve HRQoL. The subsequent and in part differential deterioration in some HRQoL domains suggests a need for further follow-up care within survivorship programs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The diagnosis of cancer and cancer treatment is frequently associated with acute, long-term, and late sequelae affecting the patient’s physical and psychological functioning, including, e.g., health-related quality of life (HRQoL) [1], emotional distress [2, 3], anxiety and depression [4,5,6], and fear of progression (FoP) [7]. Aimed at reducing the impact of such disabling and handicapping conditions, oncological rehabilitation attempts to enable patients to adapt to their new situation by regaining physical, social, psychological, and work-related functioning [8]. Its interventions range from techniques targeting specific limitations to more comprehensive multi-modal inpatient approaches. Given current epidemiological trends in cancer incidence and survival, the relevance of cancer rehabilitation with respect to survivorship is expected to even increase in the future [8].
In German-speaking countries, oncological rehabilitation is provided either in an inpatient format at specialized centers over a 3-week period on average or in an outpatient format. In line with the overall goals of oncological rehabilitation, it may include medical treatment, diet counseling, exercise and physical training, health education, psychological support, mind–body interventions, and social counseling tailored to the individual patient’s needs. Addressing key areas of impairment referred to above, studies evaluating the effects of oncological inpatient rehabilitation have frequently included HRQoL, depression, anxiety, or FoP as patient-reported outcomes (PRO) [9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29]. Primarily employing quasi-experimental, longitudinal designs, the majority of these studies [9, 12, 13, 15, 16, 18, 19, 21, 23, 24, 27, 28] included more than two measurement points demonstrating mostly positive and in part stable changes. However, only seven of these studies covered follow-up intervals beyond 6 months after the end of rehabilitation [12, 15, 18, 19, 21, 23, 27]. In addition, even fewer studies included larger proportions of patients with other than breast cancer, like, e.g., colorectal [11, 22, 24, 26] or prostate cancer [15, 23, 24]. Consequently, knowledge on the development of HRQoL, depression, and FoP beyond the end of oncological inpatient rehabilitation is largely scarce as is knowledge on whether patients with different cancers might differ in their development in regard to these outcomes in the long term. Information on these outcomes might, among other things, help identify potential differences in rehabilitation and care needs between different tumor diagnostic groups.
Given these limitations of research in this field of oncological inpatient rehabilitation, the present study aimed to investigate whether.
-
(a)
HRQoL, depression, and FoP change during oncological inpatient rehabilitation and the subsequent 9 months
-
(b)
Breast, colorectal, and prostate cancer differ in regard to their potential changes in these PROs
-
(c)
And to compare the sample’s HRQoL, depression, and FoP to reference values of the general population [30, 31] and to a recommended cut-off for dysfunctional FoP [32]
The study was part of a larger research project focusing upon the measurement of patient competencies in the context of cancer, their potential change during rehabilitation and beyond, and their relationship with HRQoL, depression, and FoP. Results on the first two of these issues have already been reported elsewhere [33, 34].
Methods
Design and procedure
The study included N = 377 patients from the overall project who received inpatient rehabilitation for breast, colorectal, or prostate cancer in nine clinics for oncological rehabilitation. These cancer types had been chosen to represent three of the most frequent tumor entities. Eligibility criteria further required patients to be at least 18 years old, sufficiently fluent in German, willing to participate in a questionnaire study and not suffering from acute psychiatric illness were eligible for the study. After having been informed about the study by clinic staff and providing written consent, patients completed questionnaires at the beginning and at the end of rehabilitation, and 9 months later. As twenty of the patients had experienced a local recurrence lately, they were excluded from data analyses in order to create a more homogeneous sample in regard to potential treatments received during rehabilitation, resulting in N = 357 for analysis.
The study was approved by the University of Freiburg Ethics Committee (No. 359/12) and registered at the German Register of Clinical Studies (No. DRKS00004410).
Measures
HRQoL was measured with the EORTC Quality of Life Questionnaire C-30 (EORTC QLQ-C30) [35]. It includes 30 items covering several domains of functioning and symptoms of cancer patients (global health, physical functioning, fatigue, etc.). Functioning and symptom scale scores represent sums of item sets and are transformed to range from 0 to 100. Higher scores on the global health and functioning scales indicate better quality of life, and higher scores on the symptom scales indicate higher symptom burden. In the present sample, the median internal consistency (Cronbach’s α) of the EORTC QLQ-C30 multi-item scales was Mdn = 0.85 at baseline.
Depression was measured with the German version of the PHQ-9 [36], a module of the Patient Health Questionnaire assessing symptoms of a major depressive disorder by nine items. Summing across item responses gives a scale score ranging from 0 to 27, with higher scores indicating higher depression. In this sample, the internal consistency at baseline was 0.82.
FoP was measured with the Fear of Progression Questionnaire short form (FoP-Q-SF) [37]. Its 12 items address various cognitive and emotional facets of FoP. Summing across all items yields a score ranging from 12 to 60, with higher scores reflecting higher FoP. A score of 34 or above is assumed to be indicative of a dysfunctional level of FoP [32]. At baseline, the internal consistency in this sample was 0.82.
Selected sociodemographic data were provided by patients’ self-reports. Medical data were obtained from patients’ medical records at the collaborating centers.
Statistical methods
Power calculations for the overall project were specified for a 3 × 2 × 3 repeated measures design with the between groups factors of tumor site and curative vs. palliative treatment situation and three measurement points [34]. Consulting appropriate statistical tables [38], a sample size of N = 288 appeared adequate for detecting small (f = 0.1) interaction effects of these three factors given a type one error of 0.01 and a power (1–β) of 0.80. In order to improve the chances of detecting a smaller than medium effect of the tumor site somewhat, we increased the intended cell size per site to 136, totaling N = 408. Assuming a dropout of 25%, the overall project aimed to recruit 512 participants at baseline in order to meet this requirement.
Data analysis included descriptive statistics for sociodemographic and medical variables and χ2-tests and one-way ANOVAs in order to determine baseline differences by tumor site. In order to analyze changes across time, we employed a 3 (tumor site: S) × 3 (time of measurement, T) repeated measures analysis of covariance (RM-ANCOVA) design that included patient age and TsD as covariates controlling for respective baseline between groups differences described further below. Testing the effects involving time of measurement, we used Huyn-Feldt-adjusted F-values where indicated. Post-hoc between-group comparisons included Bonferroni adjustments. Comparing the sample’s PRO overall means to a respective reference value [30,31,32], we used two-tailed one-sample t-tests. As effect size measures, Cohen’s d, ϕ, or (partial) η2 were employed. Throughout, missing values were not imputed. Employing χ2-techniques or t-tests, we compared patients available at follow-up with dropouts on selected sociodemographic and medical variables and baseline PROs in order to determine potential bias from dropouts.
Results
Sample
Patients were 61.1 years old on average (SD = 9.4). Mean age varied significantly as a function of tumor site (F = 24.0, df: 2, 350; p < 0.001, η2 = 0.12; breast cancer: M = 56.8, colorectal cancer: M = 60.8, and prostate cancer: M = 65.2 years). Median TsD was Mdn = 9.4 months (range 0.7–325). TsD also varied significantly as a function of the tumor site. It was longer in breast cancer women (Mdn = 12.8 months) compared to colorectal and prostate cancer patients (Mdn = 8.4 and 4.1 months, respectively; Kruskal–Wallis H = 42.3, df: 2, p < 0.001, η2 = 0.13.
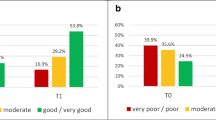
Table 1 presents further information on sociodemographic and medical sample baseline characteristics. In most of these, diagnostic groups differ significantly, with effect sizes being mostly small or medium, except for tumor size (T1: breast cancer 39%, colorectal cancer 11%, prostate cancer 5%, ϕ = 0.52).
At follow-up, 50 patients (14%) had dropped out of the study. Dropouts and completers were comparable on all PRO baseline measures except for Nausea and Vomiting (completers scoring lower, p < 0.05), the effect size being small, however (η2 < 0.05). Sociodemographic and medical characteristics showed only a few significant and small differences between completers and dropouts. Compared to dropouts, a higher proportion of completers received curative treatment and showed no metastases, while tumor stage was either “indeterminate” or T4 in a smaller proportion of them (p ≤ 0.01, ϕ being 0.19, 0.25, and 0.21, respectively).
Differences between tumor diagnostic groups and changes across time
Table 2 shows few significant and mostly small effects (η2 < 0.06) of the covariates patient age and TsD. The small effect of patient age on social functioning indicates that higher age is associated with better social functioning (β = 0.18, not in Table 2), while its moderate effect on financial difficulties implies higher age to go along with fewer difficulties (β = − 0.26). The small significant effects of TsD on fatigue, nausea and vomiting, pain, and constipation indicate a longer TsD to be associated with higher symptom burden (0.14 ≤ β ≤ 0.17).
Having controlled for both covariates, we find several significant effects of tumor site, which are large for diarrhea and small for physical functioning, cognitive functioning, depression, fatigue, pain, dyspnea, insomnia, appetite loss, and financial difficulties. On average, patients with breast cancer report lower physical and cognitive functioning, more depression, fatigue, dyspnea, and insomnia than patients with prostate cancer (Tables 3 and 4). Compared to patients with colorectal cancer, they report lower cognitive functioning, more pain, and insomnia. In contrast, patients with colorectal cancer report more diarrhea than patients with breast and prostate cancer. They also report more financial difficulties than patients with prostate cancer. Regarding appetite loss, the post-hoc comparisons reveal no significant differences between patient groups.
Effects of time of measurement are significant and mostly at least moderate (η2 ≥ 0.06) on all but three outcomes (fear of progression, nausea and vomiting, and financial difficulties). They primarily indicate improvement during rehabilitation that is stable at 9 months (Tables 3 and 4). Regarding emotional and cognitive functioning, depression, appetite loss, and diarrhea, there also is some deterioration at 9 months, however.
Finally, there are some significant and generally small interaction effects between tumor site and time of measurement indicating differential change across time (Tables 2, 3, 4). Compared to patients with colorectal or prostate cancer, patients with breast cancer improve to a greater extent during rehabilitation in emotional functioning but deteriorate again to a greater extent thereafter. Depression follows a similar pattern. Regarding dyspnea, patients with breast cancer show greater improvement during rehabilitation and thereafter appear to be stable. Patients with colorectal cancer show a comparable change regarding appetite loss.
Comparison with reference values
Compared to EORTC QLQ-C30 norms from the German general population [30] (see last column of Tables 3 and 4), the present sample scores significantly lower on average on all EORTC QLQ-C30 functioning scales on nearly all time points except for physical functioning and the Global Health scale. The mean effect size (|d|= 0.74) is moderate (d > 0.50) at the beginning of rehabilitation, and smaller afterwards (mean |d’s| being 0.32 and 0.36, respectively, values not given in Table 3). Complementarily, the sample scores significantly higher throughout on 5 of the 9 symptom scales, whereby moderate to large effect sizes result in fatigue and insomnia (0.81 and 0.51, respectively, values not given in Table 4), which decrease thereafter. Similarly, the sample’s mean depression score at each time point is significantly higher than the suggested reference value [31] with moderate effect sizes at the beginning of rehabilitation and at follow-up. In contrast, FoP means are significantly lower than the cutoff for dysfunctional FoP [32].
Discussion
Employing an RM-ANCOVA design that included comparable proportions of patients with breast, colorectal, and prostate cancer attending inpatient rehabilitation and the covariates patient age and TsD, this study investigated effects of tumor site, time of measurement, and their interaction on HRQoL, depression, and FoP. Given their effect sizes being small, even where significant, we found the influence of the covariates to be weak except for the association between higher patient age and lesser financial difficulties. The latter may in part reflect the sample composition, which included about 31% of retired participants living on regular pension. In addition, it should be noted that the relationship of patient age with social functioning and financial difficulties, respectively, is in line with previous research [1]. Regarding effects of tumor site, we found significant differences between patients with breast, colorectal, and prostate cancer in HRQoL and depression across time independent of patient age and TsD. Albeit mostly small in terms of effect size, these differences may be understood as partly reflecting persisting care needs specific to a particular group of patients. Primarily, this applies to patients with colorectal cancer who report a comparatively higher diarrhea symptom burden, thus reflecting the only larger effect (η2 ≥ 0.14) of tumor site. It also applies to patients with breast cancer, however, who show greater impairment on the EORTC QLQ-C30 scales of physical and cognitive functioning as well as on six of the symptom scales and on PHQ-9 depression. These differences may at least in part be due to the effects of prior treatment under acute care or surgery. In particular, receiving endocrine therapy, e.g., might have contributed to breast cancer patients’ higher levels of functional impairment or symptoms. Unfortunately, subsample sizes of breast cancer patients not having received, having completed, or still receiving endocrine therapy, respectively, did not allow valid testing of this hypothesis here. Therefore, further research aimed at explaining such differences between tumor diagnostic groups is required, as these thus far have often been covered merely descriptively by previous studies [24, 29].
The significant and in terms of effect size moderate to large changes in most HRQoL domains and depression during oncological inpatient rehabilitation and beyond may be seen as the main result of the present study. As to be expected from previous research, these changes indicate general improvement during rehabilitation. These are most prominent in role, emotional, and social functioning, fatigue, and depression. However, while improvement in most of these outcomes remained stable 9 months after rehabilitation, there was significant deterioration in some others, which in part also appeared to apply only to subgroups of patients, like, e.g., emotional functioning in patients with breast cancer or diarrhea in patients with colorectal cancer. Here again, the question of how to explain these differential changes arises. In the present study, ex-post analyses suggested that compared to colorectal or prostate cancer patients a higher proportion of patients with breast cancer indicated having experienced “distressing life events” (without further specification) during the previous 6 months (51.2%, 43.6%, and 27.1%, respectively, p < 0.005) and hospital re-admissions related to their disease and surgery (25%, 11%, and 7%, respectively, p < 0.05). Of course, this may not generalize beyond the current sample. However, as some previous studies have in part observed indications of differential deterioration in HRQoL after inpatient rehabilitation [23, 24], too, further research on possible determinants of such trajectories is again called for.
Comparing the overall sample means of each measurement point to available reference values for HRQoL, depression, and FoP revealed that in spite of obvious improvement during rehabilitation, patients continued to score significantly lower than available reference values in some of these outcomes. This is in line with the results of earlier studies [23, 25]. Although effect sizes for differences had decreased at follow-up, moderate ones were still observed there for emotional, cognitive, and social functioning. Regarding FoP, the sample’s mean scores were significantly lower than the cutoff suggested for dysfunctional FoP [32] from the first measurement point onwards. This might suggest the majority of the sample had no need for treatment in this respect, thus leading to no detectable improvement in FoP in contrast to other studies [19, 21]. In fact, the latter of these studies reports post-and follow-up FoP mean scores of about M = 32 that are only slightly higher than those reported here.
Aside from providing suggestions for further research, the results of this study may inform the practice of oncological rehabilitation and follow-up care. Implementing screening for distress in its various forms at the beginning of rehabilitation, e.g., may help tailor rehabilitative treatments even better to the individual patient’s needs and thus achieve a major principle of rehabilitative services. When compared to available norms for the German general population, patients scored still notably worse in some HRQoL domains and symptoms and higher on depression at the end of rehabilitation or at the 9-month follow-up in spite of prior improvement. This obviously suggests the need for additional follow-up care. The deterioration observed in breast cancer patients, e.g., in emotional functioning at follow-up, points in the same direction. The task of providing appropriate follow-up care would imply integrating the detection of respective care needs and the provision of appropriate interventions. This might be accomplished through currently discussed national survivorship programs that integrate a wide range of medical and psychosocial services and the collaboration of acute care, in- and outpatient rehabilitation, and cancer counseling centers [39,40,41,42].
Strength and limitations
Strengths of this study include its multi-factorial and multi-center approach, the inclusion of three major tumor entities to comparable proportions, the comparatively large sample size, and a follow-up interval covering 9 months. However, some limitations also need to be considered. First, the longitudinal observational design precludes causal inferences on rehabilitation effects. Second, in spite of the largely positive results of the dropout analyses, selection effects cannot completely be excluded as the response rate at study entry could not be recorded. Third, the final sample size is somewhat lower than originally planned, so some other than main effects may have been missed. Fourth, gender and tumor site are in part confounded. Fifth, generalizing findings to other tumor entities and other than inpatient settings is not possible, thus indicating the need for further research.
Conclusion
Oncological inpatient rehabilitation has the potential to significantly improve patients’ HRQoL and depression. Some HRQoL functions and symptoms may deteriorate again somewhat later, indicating the need for subsequent follow-up care that can be addressed through survivorship programs. Research addressing the possible differential change of HRQoL outcomes after rehabilitation and its determinants might help improve rehabilitation and survivorship services further.
Data availability
The data on which the present analyses are based will be available from the corresponding author upon reasonable request.
References
Quinten C et al (2015) The effects of age on health-related quality of life in cancer populations: a pooled analysis of randomized controlled trials using the European Organisation for Research and Treatment of Cancer (EORTC) QLQ-C30 involving 6024 cancer patients. Eur J Cancer 51(18):2808–2819
Carlson LE et al (2019) Prevalence of psychosocial distress in cancer patients across 55 North American cancer centers. J Psychosoc Oncol 37(1):5–21
Mehnert A et al (2018) One in two cancer patients is significantly distressed: prevalence and indicators of distress. Psychooncology 27(1):75–82
Goerling U et al (2023) Prevalence and severity of anxiety in cancer patients: results from a multi-center cohort study in Germany. J Cancer Res Clin Oncol 149(9):6371–6379
Bach A et al (2022) Psychiatric comorbidities in cancer survivors across tumor subtypes: a systematic review. World J Psychiatry 12(4):623–635
Vehling S et al (2012) Prevalence of affective and anxiety disorders in cancer: systematic literature review and meta-analysis. Psychother Psychosom Med Psychol 62(7):249–258
Luigjes-Huizer YL et al (2022) What is the prevalence of fear of cancer recurrence in cancer survivors and patients? A systematic review and individual participant data meta-analysis. Psychooncology 31(6):879–892
Silver JK et al (2018) The State of Cancer Rehabilitation in the United States. J Cancer Rehabil 1:1–8
Heim ME, Kunert S, Ozkan I (2001) Effects of inpatient rehabilitation on health-related quality of life in breast cancer patients. Onkologie 24(3):268–272
Schäfer H et al. (2001) [Changes in the psychosocial burden of patients with breast cancer during oncological inpatient rehabilitation]. Praxis Klinische Verhaltensmedizin und Rehabilitation. 14(Heft 56): p. 307–322
Teichmann JV (2002) Oncological rehabilitation: evaluation of the efficiency of inpatient rehabilitation. Rehabilitation (Stuttg) 41(1):53–63
Weis J, Moser MT, Bartsch HH (2002) [Goal-oriented evaluation of oncological inpatient rehabilitation: the ZESOR-study. Final report, project D4. A sub-project of the rehabilitation research network Freiburg/Bad Säckingen]. Tumor Biology Center, Institute of Rehabilitation Research and Prevention
Kramer R et al (2003) Long-term study of psychological effects in clinical rehabilitation (VESPER-study). Dtsch Med Wochenschr 128(27):1470–1474
Hartmann U, Ring C, Reuss-Borst MA (2004) Improvement of health-related quality of life in breast cancer patients by inpatient rehabilitation. Med Klin (Munich) 99(8):422–429
Dombo O, Otto U (2005) Quality of life after radical urologic pelvic surgery and impact of inpatient rehabilitation. Urologe A 44(1):11–28
Strauss-Blasche G et al (2005) Combined inpatient rehabilitation and spa therapy for breast cancer patients: effects on quality of life and CA 15–3. Cancer Nurs 28(5):390–398
Hartmann U et al (2006) Improvement of anxiety and depression in women with breast cancer during inpatient oncological rehabilitation - results of a prospective study. Rehabilitation (Stuttg) 45(2):88–94
Hartmann U, Muche R, Reuss-Borst M (2007) Effects of a step-by-step inpatient rehabilitation programme on quality of life in breast cancer patients. A prospective randomised study. Oncol Res Treat 30(4): p. 177–182
Kruger A et al (2009) Course of psychosocial distress and health-related quality of life in patients at different age groups during cancer rehabilitation. Z Psychosom Med Psychother 55(2):141–161
Riesenberg H, Lubbe AS (2010) In-patient rehabilitation of lung cancer patients–a prospective study. Support Care Cancer 18(7):877–882
Mehnert A et al (2013) Predictors of fear of recurrence in patients one year after cancer rehabilitation: a prospective study. Acta Oncol 52(6):1102–1109
Peters E, Mendoza Schulz L, Reuss-Borst M (2016) Quality of life after cancer-how the extent of impairment is influenced by patient characteristics. BMC Cancer 16(1): p. 787
Rath HM et al (2016) Psychosocial and physical outcomes of in- and outpatient rehabilitation in prostate cancer patients treated with radical prostatectomy. Support Care Cancer 24(6):2717–2726
Lamprecht J, Thyrolf A, Mau W (2017) Health-related quality of life in rehabilitants with different cancer entities. Eur J Cancer Care (Engl) 26(5)
Riedl D et al (2017) Improvement of quality of life and psychological distress after inpatient cancer rehabilitation: results of a longitudinal observational study. Wien Klin Wochenschr 129(19–20):692–701
Ture M et al (2017) Short-term effectiveness of inpatient cancer rehabilitation: a longitudinal controlled cohort study. J Cancer 8(10):1717–1725
Klocker J et al (2018) Long-term improvement of the bio-psycho-social state of cancer patients after 3 weeks of inpatient oncological rehabilitation: a long-term study at the Humanomed Zentrum Althofen. Wien Med Wochenschr 168(13–14):350–360
Heim ME et al (2019) Sustained improvement of quality of life following integrative oncological rehabilitation. Complement Med Res 26(3):166–173
Licht T et al (2021) Evaluation by electronic patient-reported outcomes of cancer survivors’ needs and the efficacy of inpatient cancer rehabilitation in different tumor entities. Support Care Cancer 29(10):5853–5864
Nolte S et al (2020) Updated EORTC QLQ-C30 general population norm data for Germany. Eur J Cancer 137:161–170
Kocalevent RD, Hinz A, Brahler E (2013) Standardization of the depression screener patient health questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatry 35(5):551–555
Herschbach P et al (2010) Group psychotherapy of dysfunctional fear of progression in patients with chronic arthritis or cancer. Psychother Psychosom 79:31–38. https://doi.org/10.1159/000254903
Giesler JM, Weis J (2021) Patient competence in the context of cancer: its dimensions and their relationships with coping, coping self-efficacy, fear of progression, and depression. Support Care Cancer 29(4):2133–2143
Giesler JM et al (2022) Patient competencies, coping self-efficacy, and coping: do they change during oncological inpatient rehabilitation and beyond? Psychooncology 31(4):577–586
Aaronson NK et al (1993) The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 85(5):365–376
Löwe B et al (2004) Measuring depression outcome with a brief self-report instrument: sensitivity to change of the Patient Health Questionnaire (PHQ-9). J Affect Disord 81(1):61–66
Mehnert A et al (2006) Fear of progression in breast cancer patients – validation of the short form of the Fear of Progression Questionnaire (FoP-Q-SF). Z Psychosom Med Psychother 52(3):274–288
Bortz J, Döring N (2006) Forschungsmethoden und Evaluation für Human- und Sozialwissenschaftler. 4th, revised ed. Heidelberg: Springer-Medizin-Verl. 897
Stout NL et al (2019) Long-term survivorship care after cancer treatment: a new emphasis on the role of rehabilitation services. Phys Ther 99(1):10–13
Bergelt C et al (2022) Long-term survival in cancer: definitions, concepts, and design principles of survivorship programs. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 65(4):406–411
Sleight A et al (2022) Systematic review of functional outcomes in cancer rehabilitation. Arch Phys Med Rehabil 103(9):1807–1826
Giesler J et al (2015) Ambulante psychoonkologische Versorgung durch Krebsberatungsstellen – Leistungsspektrum und Inanspruchnahme durch Patienten und Angehörige. Psychother Psychosom Med Psychol 65(12):450–458
Acknowledgements
We thank the participating patients and survivors. Our thanks also go to the following colleagues who supported this multi-center study in their role as former Medical Directors or physicians at their rehabilitation centers: Dres. G. Adam and C. Zeller, Asklepios Clinic for Oncological Rehabilitation, Triberg; Prof. Dr. H.H. Bartsch, Clinic for Oncological Rehabilitation, Clinic for Tumor Biology, Freiburg; PD Dr. R. Caspari, Paracelsus Clinic by the Lake, Clinic for Oncological Rehabilitation, Bad Gandersheim; Dr. T. Dauelsberg, Winkelwald Clinic, Clinic for Oncological Rehabilitation, Nordrach; Dr. W. Hoffmann, Clinic for Oncological Rehabilitation, Park Therme, Badenweiler; Dr. R. Kobes-Schrödel, Adelsberg Clinic for Oncological Rehabilitation, Bad Berka; Dr. J. Körber, Nahetal Clinic for Oncological Rehabilitation, Bad Kreuznach; Dr. H. Schäfer, Wehrawald Clinic, Rehabilitation Center Todtmoos, Todtmoos; PD Dr. J. Teichmann and Dr. C. Fernandes Almeida, Rehabilitation Center Oberharz, Clausthal-Zellerfeld.
Funding
Open Access funding enabled and organized by Projekt DEAL. The German Federal Ministry of Education and Research funded this study under Grant No. 01GX1051.
Author information
Authors and Affiliations
Contributions
Both authors contributed to the conceptualization of the study design, the acquisition, statistical analysis and interpretation of the data, to drafting and revising the paper, and to finally approving the version to be submitted.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. It was approved by the University of Freiburg Ethics Committee (No. 359/12) and registered at the German Register of Clinical Studies (No. DRKS00004410).
Consent to participate
Informed consent was obtained from all participants included in the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Giesler, J.M., Weis, J. Changes in health-related quality of life, depression, and fear of progression during oncological inpatient rehabilitation and beyond: a longitudinal study. Support Care Cancer 32, 626 (2024). https://doi.org/10.1007/s00520-024-08800-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-024-08800-z