Abstract
Purpose
To assess radiographic presentation of anatomical structures, bony changes and soft tissue calcifications on panoramic radiographs of oncologic patients under high dose antiresorptive drug therapy (ART) before exposure to dental extraction.
Methods
Panoramic radiographs of 57 patients under ART, taken previously to tooth extraction, and 57 control patients were evaluated by two oral radiologists regarding bone pattern, anatomical structures visibility, estimation of cortical width, mandibular cortical index (MCI), and presence of soft tissue calcifications. Parameters were compared between ART and age- and gender-matched healthy control groups. Bone patterns were further assessed by regions with or without tooth extractions and according to uneventful healing or MRONJ development. All comparisons were made using chi-square test with significance level set at 5%.
Results
Mandible and posterior maxilla presented more sclerotic bone patterns in patients under ART, regardless of tooth extraction and MRONJ development status (p < 0.05). Heterogeneous bone pattern was identified in two regions that both were subsequently affected by MRONJ. Anatomical structure visibility and presence of soft tissue calcifications was not different among groups (p > 0.05). ART patients showed significantly more C0 (thickening) and C1 MCI (p < 0.05).
Conclusion
Sclerotic bone pattern and thicker mandibular cortices may represent a consequence of ART rather than MRONJ specific findings. Prospective studies on larger patient samples radiographically followed-up during the ART treatment are advised, with specific attention to heterogenous trabecular bone pattern as a possible MRONJ predictor.
Similar content being viewed by others

Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Antiresorptive therapy (ART) is an essential part of the treatment of oncologic patients aimed to prevent skeletal-related events and hypercalcemia associated with bony metastasis of malignant tumors [1]. ART promote inhibition of the osteoclastic activity, favoring bone deposition, which has shown to improve oncologic patients’ quality of life [2]. However, there is an uncommon, yet severe, adverse effect associated with the ART that results in necrosis of the jaw bones, namely medication-related osteonecrosis of the jaws (MRONJ). MRONJ presents higher risk of development in oncologic patients under high doses of ART and followed by tooth extraction as a triggering factor [1, 2].
A widely accepted and recently updated position paper of the American Association of Oral and Maxillofacial Surgeons defines MRONJ as a condition of necrotic bone exposed to the oral cavity for at least 8 weeks in patients receiving, or that had formerly received ART and no history of radiotherapy of the head and neck [3]. Moreover, they propose a staging system based on the clinical aspect/extent of the osteonecrosis (stages 1, 2, and 3), a prodromic stage (stage 0), and a “at risk” category that includes all patients that have never manifested any signs or symptoms of necrosis but have current or previous history of ART [3].
Imaging exams are adjuvant in the MRONJ diagnosis, which is predominantly clinical. However, the clinical diagnosis may come too late once the true extent of a clinically visible lesion may be greater than expected [4]. Thus, imaging exams are paramount for a correct and early diagnosis. Current challenges in MRONJ diagnosis include the identification of its radiographic characteristics in the earlier stages (i.e., without clinical bone exposure) or predictive radiographic findings for the occurrence of MRONJ [5,6,7,8].
Cone beam computed tomography (CBCT) has been suggested as the imaging modality of choice for early detection of bone necrotic development. However, panoramic radiography is an easy and accessible imaging modality which allows visualization of both arches and adjacent structures. In addition, it has a relatively low radiation dose to the patient and may be useful in identifying predictive characteristics for MRONJ [9].
Different mandibular radiomorphometric indices have been applied to panoramic images in an attempt to identify patients with bone-affecting conditions, such as low bone mineral density in post-menopausal women. Often those indices present good results in terms of accuracy [10, 11] and may be used either quantitatively (i.e., cortical thickness measures) or qualitatively (i.e. mandibular cortical shape and structure). Although the quantitative indices have shown to be effective, qualitative indices are typically simpler and more efficient, and therefore more clinically applicable. The visual estimation of cortical width (ECW) and the mandibular cortical index (MCI) are examples of qualitative indices that have been demonstrated to be reliable in identifying low bone mineral density [10].
Therefore, the aim of the present study was to assess radiographic findings of anatomical structures, bony changes, qualitative radiomorphometric indices, and soft tissue calcifications in panoramic radiographs of oncologic patients under high dose ART before exposure to dental extraction, in an attempt to associate these with bone necrosis development.
Methods
Approval from the local review board was granted for the present study (protocol S63934), following the ethical principles and standards from Helsinki Declaration.
Sample selection
Patients from the department of Oral and Maxillofacial Surgery at the University Hospitals Leuven databank were selected according to the following inclusion criteria: patients in high dose ART for oncologic reasons, indicated for tooth extraction, presenting panoramic radiograph while on “at risk” stage for MRONJ development. Records of their clinical follow-up after the tooth extraction should be available for at least an 8-week period to demonstrate uneventful healing or to confirm diagnosis of MRONJ if the wound persisted [3]. Following the diagnostic criteria proposed by the AAOMS, patients with history of radiation therapy of the head and neck were excluded. A total of 57 patients meeting these criteria were included and formed the ART group. In addition to those, a control group of healthy individuals was selected, pairing with the ART group by age, gender, and tooth number indicated for extraction. Teeth of all patients were surgically extracted following the department protocol, with prophylactic antibiotics coverage when indicated.
Image assessment
Images were exported in DICOM format from the PACS server and randomized for the independent assessment by 2 oral radiologists, in a dimly lit environment, using a high-resolution monitor (MD Barco MDRC-2221; Barco, Kortrijk, Belgium). Image assessments were done considering different aspects of the structures, as follows:
-
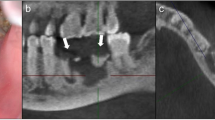
Bone pattern: bone pattern was evaluated considering 6 different regions of the dental arches: 1—right posterior maxilla; 2—anterior maxilla; 3—left posterior maxilla; 4—left posterior mandible; 5—anterior mandible; 6—right posterior mandible [12]. In each of these regions, observers scored trabecular bone pattern as normal (sparse or alternating dense and sparse), sclerotic (dense bone with small intertrabecular spaces to absent spaces), or heterogeneous (mixed sclerotic and lytic bone) (Fig. 1), adapted from the study by Jonasson et al. [13]. Edentulous regions with extensive bone resorption were excluded from the assessment.
-
Anatomical structure visualization: mandibular canal cortices, mental foramina, and maxillary sinus floors were classified as visible, partially visible or not visible, considering the radiopaque limits of these structures.
-
Estimation of mandibular cortical width (ECW) [11]: thin, normal, or thickened (Fig. 2).
-
Mandibular cortical index (MCI) [14]: C1, C2, or C3. In addition, a new index was proposed as C0, when thickening of the mandibular cortical was detected, including periosteal reaction (Fig. 2).
-
Soft tissue calcifications: absent or present, considering any of the possible soft tissue calcifications observable on a panoramic radiograph (e.g., carotid artery calcification/atheroma, tonsillolith, sialolith, and stylohyoid ligament mineralization).
Prior to assessment, a training and calibration session was held to explain the parameters under assessment and solve any questions. Immediately after the assessment by the two observers, the results were confronted to reach consensus, and if necessary, a third oral radiologist was invited to solve any disagreements.
Statistical analysis
Data was analyzed using GraphPad Prism software (GraphPad Inc., La Jolla, CA, USA) and SPSS Statistics software version 25.0 (IBM Corp., Armonk, NY, USA). For bone pattern comparison, each region was classified as: control, ART when no tooth extraction was performed in that region, MRONJ − when tooth was extracted but there was uneventful healing, or MRONJ + when tooth was extracted and there was subsequent development of necrosis. For the other radiographic parameters, patients were divided as control or ART. Data was expressed as absolute and relative frequencies, and all comparisons between groups were done using the chi-square test, with a significance level of 5% (α = 0.05). For multiple comparisons, the Bonferroni correction was applied and post hoc of the chi-square was carried out following the adjusted residuals analysis [15].
Results
One hundred fourteen panoramic radiographs (57 patients under ART and 57 control patients) were evaluated. The mean age of the patients was 55.5 years (31–89 age range) for both groups. In the ART group, 18 patients were under ART for less than one year, 15 patients were between 1 and 2 years under ART, and 24 were over 2 years under high-dose ART. Of the 57 patients under ART, 22 had uneventful healing after tooth extraction. A total of 35 patients presented clinically with necrosis after tooth extraction. Twenty-six patients developed necrosis in only one region, while 9 patients presented necrosis in multiple regions. Regarding the teeth extracted in that group, 145 teeth were extracted from 107 regions, of which 48 regions developed necrosis, and 59 regions healed uneventfully.
Bone pattern
Table 1 shows data regarding the bone pattern classification in all the different anatomical regions analyzed, considering control patients, ART regions, MRONJ − regions, and MRONJ + regions. Maxillary bone presented higher prevalence of normal bone pattern, without significant differences among the groups (p = 0.510). In the posterior maxilla, the prevalence of sclerotic bone pattern was slightly higher in MRONJ + groups (p = 0.020; not significant according to Bonferroni correction). Mandibular bone showed higher prevalence of sclerotic bone pattern in the anterior mandible for MRONJ − and MRONJ + groups (p = 0.023; not significant according to Bonferroni correction), and in the posterior mandible for ART, MRONJ − , and MRONJ + groups (p < 0.001). Overall, MRONJ + sites presented higher prevalence of sclerotic bone (p < 0.001). No statistically significant differences in the bone pattern among different regions were observed between MRONJ − and MRONJ + (p > 0.05).
Anatomical structure visualization and calcifications
Concerning anatomical structures visibility, no differences (p > 0.05) were detected between patients under ART and controls for any of the structures assessed (mandibular canal, mental foramen, maxillary sinus; Fig. 3). Soft tissue calcifications were detected in 40% of the control group and 38% of ART group, without significant differences among groups (p = 0.848).
Mandibular cortical estimation and index
Regarding the mandibular cortical indexes assessed (Fig. 4), no differences were observed for the ECW (p = 0.197), however, for MCI, patients under ART were classified more often as types C0 or C1 compared to control patients (p < 0.001).
Discussion
MRONJ causes changes in the jaws that can be assessed by means of panoramic radiography, such as changes in bone pattern (dense, sclerotic, or heterogeneous bone), presence of bone sequestration, increased periodontal ligament space, thickened lamina dura, and narrowing of the mandibular cortex. Those are characteristics already established in the literature associated with patients affected by MRONJ [8, 16, 17] and were not in the scope of our evaluation. Nevertheless, some of these characteristics, such as lamina dura thickening, are also present in ART “at risk” patients and should not be not mistaken as MRONJ predictors, but rather as a common effect of ART [8, 18]. Radiographic characteristics of the jawbone of these individuals before performing invasive procedures (i.e., tooth extraction) can be essential key points to assess the propensity of specific sites with increased risk of developing MRONJ [4, 18]. Therefore, the images included in our sample and the radiographic characteristics depicted were from patients before tooth extraction and with potential MRONJ manifestation.
The bone pattern observed in the anterior maxilla proved to be mostly sparse or alternating sparse/dense in patients of all groups evaluated in the present study, but sclerotic in the posterior maxilla for the ART patients, and MRONJ − and MRONJ + regions. In contrast, the mandibular bone was more often rated as sclerotic pattern for patients under ART, regardless of the future development of MRONJ. Such denser bone pattern, when observed radiographically before invasive procedures, may represent the bone modification resulting from the ART osteoclast inhibition, rather than indicating increased MRONJ susceptibility [18].
Dense, or sclerotic bone pattern in the jaws, as observed in the results of the present study, are commonly expected radiographic findings in individuals undergoing ART, due to osteoclast inhibition or reduced osteoclast differentiation [5, 18]. However, a heterogeneous bone pattern, depicted as mixed sclerotic and lytic bone, can also be seen in these individuals. In the present study, two patients presented this heterogenous bone in the posterior region of the maxilla and mandible, and both developed MRONJ after tooth extraction. These findings emphasize that the presence of mixed heterogeneous bone can be a high-risk predictor for MRONJ development. However, the conditions making overall bone changes becoming susceptible to MRONJ involvement remains unknown [18, 19].
The visibility of anatomical structures has been assessed in previous studies [5, 7, 17]. In these studies, it was observed that the different stages of MRONJ involvement may present, for example, an increase in the cortices of the mandibular canal, a thickening of the lamina dura, as well as enhancement of the external oblique crest. In contrast, the present study was not able to identify these patterns, most likely because the images evaluated were from patients under ART prior to extraction, while the other studies evaluated patients at different stages of MRONJ [5, 7]. Thus, the pathology by itself may cause dense sclerosis of the bone and enhance anatomical structures cortices.
We assessed the presence of soft tissue calcifications observed on panoramic radiographs in patients under ART. Our results show that, despite the effect of ART on bone metabolism and possible circulating calcium level, the prevalence of those calcifications is not expected to differ significantly from non-ART patients.
Radiomorphometric indices (ECW and MCI) in panoramic radiographs make it possible to subjectively predict a decrease in bone mineral density in the mandible [6, 20]. The ECW is an estimate of the cortical thickening and in the present study, it was not found different between control and ART groups. Yet, a numerical quantification of the cortical thickness by Torres et al. [21] showed thicker cortices in patients with MRONJ and patients under ART as compared to controls. In contrast, Kubo et al. [6] also measured the mandibular inferior cortical bone thickness and found thicker cortices for control group compared to patients under ART. Differences among studies may be related to patient-specific variables, such as age, gender, basis condition, medication, duration of treatment, dosage, and time of the measurement.
For the MCI, there was a higher prevalence of the newly introduced index C0, and C1 classification in ART patients. This is an important finding, as it may represent the consequence of ART in thickening the mandibular cortices. Therefore, the proposal of the C0 classification that indicates bone deposition in the mandibular cortex may be considered for further studies assessing MCI in these patients. These results concur with the previous study by Kubo et al. [6] that elucidated a higher prevalence of the C1 index when comparing patients under ART and controls. The authors [6] also suggested that C2 may be a predictor for necrosis as this classification was more common in patients affected by MRONJ. However, they considered this not to be a thinning of the mandibular cortices characterizing C2, but a thickening of previously defected cortices related to the use of ART in osteoporotic patients. We believe that the C0 and C1 stages may be related to inhibition of bone resorption. Therefore, in patients under ART with no clinical indication of necrosis, the thickening of the mandibular cortices and a more sclerotic pattern of the bone in the mandible may represent a therapy consequence. Nevertheless, in patients with known necrosis, both findings can be also found as a result of the chronic osteomyelitis process [4], surely when considering that osteonecrotic lesions may also show a chronic osteomyelitis component.
Conclusion
In conclusion, sclerotic bone pattern and thicker mandibular cortices are radiographic characteristics of patients under ART, regardless of the development of MRONJ after tooth extraction. Heterogeneous trabecular bone pattern may be related to the occurrence of necrosis and should be further investigated.
Data Availability
The datasets generated and analyzed during the current study are available from the corresponding author upon reasonable request.
References
Nicolatou-Galitis O, Schiødt M, Mendes RA et al (2019) Medication-related osteonecrosis of the jaw: definition and best practice for prevention, diagnosis, and treatment. Oral Surg Oral Med Oral Pathol Oral Radiol 127:117–135. https://doi.org/10.1016/j.oooo.2018.09.008
Kuroshima S, Sasaki M, Sawase T (2019) Medication-related osteonecrosis of the jaw: a literature review. J Oral Biosci 61:99–104. https://doi.org/10.1016/j.job.2019.03.005
Ruggiero SL, Dodson TB, Aghaloo T et al (2022) American Association of Oral and Maxillofacial Surgeons’ Position Paper on Medication-Related Osteonecrosis of the Jaws—2022 Update. J Oral Maxillofac Surg 80:920–943. https://doi.org/10.1016/j.joms.2022.02.008
Gaêta-Araujo H, Vanderhaeghen O, de Vasconcelos KF et al (2021) Osteomyelitis, osteoradionecrosis, or medication-related osteonecrosis of the jaws? Can CBCT enhance radiographic diagnosis? Oral Dis 27:312–319. https://doi.org/10.1111/odi.13534
Klingelhöffer C, Klingelhöffer M, Müller S et al (2016) Can dental panoramic radiographic findings serve as indicators for the development of medication-related osteonecrosis of the jaw? Dentomaxillofac Radiol 45:20160065. https://doi.org/10.1259/dmfr.20160065
Kubo R, Ariji Y, Taniguchi T et al (2018) Panoramic radiographic features that predict the development of bisphosphonate-related osteonecrosis of the jaw. Oral Radiol 34:151–160. https://doi.org/10.1007/s11282-017-0293-9
Sahin O, Odabasi O, Demiralp KOÖ et al (2019) Comparison of findings of radiographic and fractal dimension analyses on panoramic radiographs of patients with early-stage and advanced-stage medication-related osteonecrosis of the jaw. Oral Surg Oral Med Oral Pathol Oral Radiol 128:78–86. https://doi.org/10.1016/j.oooo.2019.03.002
Moreno-Rabié C, Gaêta-Araujo H, Oliveira-Santos C et al (2020) Early imaging signs of the use of antiresorptive medication and MRONJ: a systematic review. Clin Oral Investig 24:2973–2989. https://doi.org/10.1007/s00784-020-03423-0
Shin JW, Kim J-E, Huh K-H et al (2019) Clinical and panoramic radiographic features of osteomyelitis of the jaw: a comparison between antiresorptive medication-related and medication-unrelated conditions. Imaging Sci Dent 49:287. https://doi.org/10.5624/isd.2019.49.4.287
Leite AF, de Figueiredo PT, S, Guia CM, et al (2010) Correlations between seven panoramic radiomorphometric indices and bone mineral density in postmenopausal women. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol 109:449–456. https://doi.org/10.1016/j.tripleo.2009.02.028
Lee K, Taguchi A, Ishii K et al (2005) Visual assessment of the mandibular cortex on panoramic radiographs to identify postmenopausal women with low bone mineral densities. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol 100:226–231. https://doi.org/10.1016/j.tripleo.2004.11.052
Koth VS, Figueiredo MA, Salum FG, Cherubini K (2017) Interrelationship of clinical, radiographic and haematological features in patients under bisphosphonate therapy. Dentomaxillofac Radiol 46:20160260. https://doi.org/10.1259/dmfr.20160260
Jonasson G, Alstad T, Vahedi F et al (2009) Trabecular pattern in the mandible as bone fracture predictor. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol 108:e42–e51. https://doi.org/10.1016/j.tripleo.2009.05.018
Klemetti E, Kolmakov S, Kröger H (1994) Pantomography in assessment of the osteoporosis risk group. Eur J Oral Sci 102:68–72. https://doi.org/10.1111/j.1600-0722.1994.tb01156.x
García-Pérez MA, Núñez-Antón VV (2003) Cellwise residual analysis in two-way contingency tables. Educ Psychol Meas 63:825–839. https://doi.org/10.1177/0013164403251280
Koth VS, Figueiredo MA, Salum FG, Cherubini K (2016) Bisphosphonate-related osteonecrosis of the jaw: from the sine qua non condition of bone exposure to a non-exposed BRONJ entity. Dentomaxillofac Radiol 45:20160049. https://doi.org/10.1259/dmfr.20160049
Dutra KL, Haas LF, Zimmermann GS et al (2019) Prevalence of radiographic findings on jaws exposed to antiresorptive therapy: a meta-analysis. Dentomaxillofac Radiol 48:20180112. https://doi.org/10.1259/dmfr.20180112
Gaêta-Araujo H, Ferreira Leite A, de Faria VK et al (2021) Why do some extraction sites develop medication-related osteonecrosis of the jaw and others do not? A within-patient study assessing radiographic predictors. Int J Oral Implantol (Berl) 14:87–98
Devlin H, Greenwall-Cohen J, Benton J et al (2018) Detecting the earliest radiological signs of bisphosphonate-related osteonecrosis. Br Dent J 224:26–31. https://doi.org/10.1038/sj.bdj.2017.1001
Ogura I, Sasaki Y, Kameta A et al (2018) Characteristic multimodal imaging of medication- related osteonecrosis of the jaw: comparison between oral and parenteral routes of medication administration. Pol J Radiol 82:551–560. https://doi.org/10.12659/pjr.902513
Torres SR, Chen CSK, Leroux BG et al (2015) Mandibular inferior cortical bone thickness on panoramic radiographs in patients using bisphosphonates. Oral Surg Oral Med Oral Pathol Oral Radiol 119:584–592. https://doi.org/10.1016/j.oooo.2015.02.005
Funding
This study was financed in part by the Coordenação de Desenvolvimento de Pessoal de Nível Superior (CAPES), finance code 001.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Hugo Gâeta-Araujo, Maria Clara Rodrigues Pinheiro, André Ferreira Leite, and Karla de Faria Vasconcelos. The first draft of the manuscript was written by Hugo Gaêta-Araujo and Maria Clara Rodrigues Pinheiro and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Approval was obtained from the ethics committee of University Hospitals Leuven (UZ Leuven). The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gaêta-Araujo, H., Pinheiro, M.C.R., Leite, A.F. et al. Radiographic perception of anatomical structures and bony changes in oncologic patients under antiresorptive therapy. Support Care Cancer 31, 149 (2023). https://doi.org/10.1007/s00520-023-07613-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-023-07613-w