Abstract
Objectives
The purpose of this study was to clarify which panoramic radiographic features can predict the development of bisphosphonate-related osteonecrosis of the jaw (BRONJ).
Methods
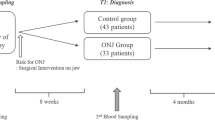
Participants included 24 patients treated with bisphosphonates (BP) for osteoporosis who developed osteonecrosis of the jaw (ONJ+ group). Controls included 179 patients treated with BP who did not have osteonecrosis (ONJ− group) and 200 patients with no history of BP administration (unmedicated group). The mandibular cortical width, mandibular cortical index (MCI), sclerosis of trabecular bone, and thickening of the lamina dura were evaluated on panoramic radiographs.
Results
The mandibular cortical width was significantly smaller in the ONJ– group than in the other groups. Class II MCI (semilunar defects of endosteal margin) was frequently noted on the affected and contralateral sides in the ONJ+ group but not in the ONJ− or unmedicated groups. Sclerosis of the trabecular bone was significantly more frequently observed on the affected side in the ONJ+ group than in the other groups. Thickening of the lamina dura was observed significantly more frequently in the BP-treated groups than in the unmedicated group.
Conclusions
Class II MCI may be an indicator to predict the development of BRONJ. Sclerosis of trabecular bone was a characteristic imaging feature of BRONJ. Thickening of the lamina dura may be an imaging feature caused by BP administration.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Bisphosphonate-related osteonecrosis of the jaw (BRONJ) has become well known since its first description by Marx in 2003 [1]. The imaging features of BRONJ are non-specific, including unremodeled extraction sockets, osteosclerosis, osteolysis, cortical disruption, and widening of the periodontal ligament [2,3,4,5]. The most common imaging finding is osteosclerosis, varying from subtle thickening of the lamina dura and alveolar crest to osteopetrosis-like sclerosis [2].
Various risk factors for the development of BRONJ have been reported [6,7,8,9,10,11,12], although the mechanism of BRONJ pathogenesis is not well understood. Invasive dental procedures, especially tooth extraction [8,9,10,11,12], as well as inflammatory conditions of the jaw are considered the most critical risk factors [12, 13].
If the imaging features related to the development and early stages of BRONJ could be detected before dental procedures, clinicians could use this knowledge to help prevent worsening of the condition. Our previous study using computed tomography confirmed that cancellous bone in BP-treated patients, including early BRONJ patients, recorded high CT values [14]. However, there is a need to investigate BRONJ indicators on panoramic radiographs, which are more commonly taken at the first visit to a dental clinic. Klingelhöffer et al. were unable to find any indicators of BRONJ development on panoramic radiographs [15]. However, Torres et al. showed that the width of the inferior mandibular cortex was related to the cumulative dose of bisphosphonates (BP) and that changes in this width could be a useful indicator of BRONJ [16]. Further investigation of the reliability of indicators of BRONJ development is required.
This study aimed to clarify which features on panoramic radiographs can be used to predict the development of BRONJ.
Materials and methods
Patients
This retrospective study was planned in accordance with the code of ethics of the World Medical Association (Declaration of Helsinki) and was carried out with the approval of the Aichi Gakuin University Ethics Committee (No. 388).
Cases were selected from the image database at the Department of Radiology and Diagnostic Imaging of Aichi Gakuin University Dental Hospital between April 2011 and August 2016. Twenty-four patients who were treated with BP for osteoporosis and developed osteonecrosis of the jaw were enrolled in this study (ONJ+ group). The patients included 23 women and one man, with an average age of 76.9 ± 7.1 years (range 62–91 years). All patients received an oral examination at the initial visit, including panoramic radiographs for diagnosis and treatment planning of BRONJ.
Diagnosis of BRONJ was based on the criteria outlined in the position paper of the American Association of Oral and Maxillofacial Surgeons [17, 18]. These criteria include the current or previous treatment with antiresorptive or antiangiogenic agents, exposed bone or bone that can be probed through an intraoral or extraoral fistula in the maxillofacial region that has persisted for longer than 8 weeks, and no history of radiation therapy of the jaw or obvious metastatic disease of the jaw.
The patients in the control groups were selected consecutively from data collected during the same time period, ensuring that age and sex distribution matched the study group. One control group consisted of 179 patients who were treated with BP for osteoporosis but had no osteonecrosis (ONJ− group); these patients had visited the hospital for treatment of other conditions. This group included 165 women and 14 men (mean age 76.0 ± 7.7 years; range 54–94 years). The second control group consisted of 200 patients with no history of BP administration and no large lesions of the jaw (unmedicated group). That group included 184 women and 16 men (mean age 74.7 ± 7.8 years; range 59–92 years). All patients in both control groups underwent an oral examination including panoramic radiographs for diagnosis and treatment planning of their chief complaints, which included periodontitis, apical periodontitis, and small radicular cysts.
Clinical characteristics
The number of patients taking cardiovascular disease medication, antidiabetic agents, thyroid hormones, anticancer agents, and corticosteroids in each group is shown in Table 1.
BP administration status
The number of patients taking BP in each group is shown in Table 2. All patients in the ONJ+ group received oral BP, whereas in the ONJ− group, 97% of patients received oral BP and 3% received intravenous BP. Alendronate was the most frequently administered BP, followed by risedronate. The duration of BP administration was 63.3 ± 35.7 months in the ONJ+ group and 8.1 ± 31.5 months in the ONJ− group.
Evaluation of panoramic radiographs
Panoramic radiography was performed with a Veraviewepocs unit (J. Morita Mfg. Co., Kyoto, Japan). The following four parameters were evaluated on the digital panoramic radiographs.
The mandibular cortical width (MCW) was analyzed with a bone morphology analysis system (Fig. 1). This system was developed through joint research between Gifu and Asahi Universities to screen for osteoporosis [19,20,21] and enables automatic measurement of MCW and evaluation of the mandibular cortical index (MCI) according to the methods of Taguchi et al. [22,23,24,25] and Klemetti et al. [26]. Muramatsu et al. demonstrated the high accuracy of this system [19, 20]. The reproducibility of MCW measurements was preliminarily determined with Dahlberg’s double determination method, using the equation Sx = (Σd 2/2n)1/2, where d is the difference between duplicate measurements and n is the number of double measurements.
Evaluation of MCI on the more severely affected side was obtained with this system. Referring to these results, two specialists in oral and maxillofacial radiology (YA and EA) evaluated MCI on both sides, without access to clinical information. MCI classifications according to Klemetti et al. [26] were as follows: Class I, the endosteal margin of the cortex was even and sharp on both sides; Class II, the endosteal margin showed semilunar defects or endosteal cortical residues on one or both sides; Class III, the cortical layer formed heavy endosteal cortical residues and was clearly porous.
The same two specialists evaluated sclerosis of trabecular bone and thickening of the lamina dura in comparison with a presented typical image. When sclerosis was observed in a wide range beyond the alveolar region, it was evaluated as positive (Fig. 2). When thickening of the lamina dura was observed around more than two teeth, it was evaluated as positive (Fig. 3).
When two observers had different assessments of MCI, sclerosis of trabecular bone, or thickening of the lamina dura, consensus was reached by discussion.
Statistical analysis
MCW, MCI, sclerosis of trabecular bone, and thickening of the lamina dura were evaluated bilaterally. In the ONJ+ group, the affected and unaffected sides were compared. In the two control groups, the evaluations on the right side were used for analysis, because there were no significant differences between the right and left evaluations. The evaluations were compared among the three groups.
MCW was compared between the affected and unaffected sides in the ONJ+ group with the Wilcoxon signed-rank test, and among the three groups with the Tukey–Kramer test. MCI was compared with the χ 2 test. Sclerosis of trabecular bone and thickening of the lamina dura were compared between the affected and unaffected sides in the ONJ+ group with Fisher’s exact test, and among the three groups with the χ 2 test. A P value of <0.05 was considered statistically significant.
Logistic regression analysis was performed to examine the factors in the clinical and imaging findings that predicted the development of BRONJ.
Results
Patients’ clinical information is shown in Table 1. The three groups showed no significant difference in age distribution (Table 1, Tukey–Kramer test) or sex ratio (χ 2 test, P = 0.3591). Regarding medication status, there were significant differences in the percentage of patients taking cardiovascular disease medication and corticosteroids among the three groups (χ 2 test, P = 0.0003 and P < 0.0001, respectively).
BP administration status is shown in Table 2. There was no significant difference between the two groups in administration method (Fisher’s exact test, P = 1.0000) or type of BP administered (χ 2 test, P = 0.6169). A significant difference was found in duration of BP administration between the two groups (t test, P = 0.0114).
Regarding the reproducibility of MCW measurements, Sx was sufficiently small at 0.09. The interobserver kappa values for MCI, sclerosis of trabecular bone, and thickening of the lamina dura were 0.704, 0.738, and 0.798, respectively.
The results of the MCW measurements are shown in Fig. 4. The mean MCW on the affected and unaffected sides in the ONJ+ group was 3.25 ± 1.08 and 2.93 ± 0.98 mm, respectively. The mean MCW in the ONJ− and the unmedicated groups was 2.90 ± 0.74 and 3.03 ± 0.78 mm, respectively.
In the ONJ+ group, the MCW was significantly larger on the affected side than on the unaffected side (Wilcoxon signed-rank test, P = 0.0148). There was a significant difference between the MCW on the affected side in the ONJ+ group and the MCW in the ONJ− group (Tukey–Kramer test, P = 0.0396). The MCW was significantly smaller in the ONJ− group than in the unmedicated group (Tukey–Kramer test, P = 0.0243); in other words, the MCW in the ONJ− group was significantly smaller than the MCW in the other groups. The MCW on the unaffected side in the ONJ+ group was not significantly different from the MCW in the other groups (Tukey–Kramer test).
The results of evaluation of the MCI are shown in Fig. 5. Class II MCI was frequently seen on both sides in the ONJ+ group. The distribution of MCI classes on the affected side in the ONJ+ group was significantly different from those in the ONJ− and unmedicated groups (χ 2 test, P = 0.0131 and P = 0.0195, respectively). A significant difference in the distribution of MCI classes was also found between the ONJ− and the unmedicated groups (χ 2 test, P = 0.0427). Although the distribution of MCI classes on the unaffected side in the ONJ+ group was not significantly different from that in the ONJ− group, the P value was borderline (χ 2 test, P = 0.0511).
The results of the evaluation of sclerosis of trabecular bone are shown in Fig. 6. Sclerosis of trabecular bone was observed significantly more frequently on the affected side in the ONJ+ group than on the contralateral side in the same group (Fisher’s exact test, P = 0.0003). Similar results were seen in comparison with the two control groups (χ 2 test, P < 0.0001).
The results of the evaluation of thickening of the lamina dura are shown in Fig. 7. There was no difference in the prevalence of thickening of the lamina dura between the two sides in the ONJ+ group (Fisher’s exact test, P = 0.3726). Comparison among the three groups demonstrated that the frequency of thickening of the lamina dura was significantly lower in the unmedicated group than in the BP administration groups (χ 2 test, P < 0.0001 compared with the affected side in the ONJ+ group, P = 0.0049 compared with the unaffected side in the ONJ+ group, and P < 0.0001 compared with the ONJ− group).
To examine which factors in the clinical and imaging findings could predict the development of BRONJ, logistic regression analysis was performed. The results are shown in Table 3. Age, duration of BP administration, and Class II MCI were considered significant factors to predict the development of BRONJ. Although the odds ratios for age and duration of BP administration were close to 1, the odds ratio for Class II MCI was 3.63.
Discussion
Various clinical risk factors for BRONJ have been reported since its first description more than 10 years ago [7,8,9,10,11,12,13]. BRONJ has predominantly been observed in cancer patients treated with high-dose intravenous BP [11]. This study targeted patients treated with BP for osteoporosis, most of whom were treated with oral BP. The duration of BP administration has been implicated as a potential risk factor for the development of BRONJ [8]. Other local factors associated with the development of BRONJ include dental procedures (especially tooth extraction [8,9,10, 12]), inflammatory conditions [12, 13], and oral hygiene [8].
There are several systemic risk factors for the development of BRONJ. The risk increases with the severity of osteoporosis [9]. Steroid intake has also been implicated as a potential risk factor [8]. Factors inhibiting angiogenesis have also been considered, and it has been shown that patients with hyperlipidemia and rheumatoid arthritis have a high risk of developing BRONJ [7]. In this study, these risk factors were re-examined, as well as factors relating to the imaging findings. Univariate analysis revealed that the ONJ+ group had the highest percentage of patients taking corticosteroid medication. However, multivariate analysis (logistic analysis) indicated that other parameters were more significant risk factors for the development of BRONJ. Corticosteroid administration can still be considered a possible factor related to BRONJ.
This study aimed to explore which imaging features predict the development of BRONJ. According to the previous reports, BPs accumulate in the bone and cause thickening of the lamina dura and sclerosis of trabecular bone [2]. BRONJ is frequently accompanied by inflammation; imaging findings such as osteolysis, osteosclerosis, sequestration, and periosteal reactions have been observed in the jaw, similar to the findings in osteomyelitis [3, 4, 27]. In our study, the jaw on the contralateral side in the ONJ+ group, which had not been modified by inflammation, was carefully evaluated. Differences in the imaging findings between the contralateral side of the ONJ+ group and the ONJ− group could indicate possible imaging features that are risk factors for the development of BRONJ.
Several studies have investigated whether certain imaging features could predict the development of BRONJ. Klingelhöffer et al. were unable to find any imaging features that acted as indicators [15]. Our previous study using CT images suggested that sclerosis of cancellous bone may be an indicator of BRONJ development [14]. However, not all patients treated with BP necessarily undergo CT examination. Panoramic radiography is the method most frequently used at the first dental visit. Therefore, indicators that can be evaluated on panoramic radiographs would be of clinical use.
Torres et al. proposed MCW as an indicator of BRONJ [16]. However, MCW was not found to be an indicator in the present study. The MCW was larger on the affected side than on the contralateral side in the ONJ+ group. The comparison among the three groups indicated that the MCW in the ONJ− group was smaller than MCW in the other groups. The cortical width may vary under the complicated influence of several factors, including the severity of osteoporosis, the effect of BP administration, and inflammatory changes in the jaw. The MCW on the affected side in ONJ+ patients may have been larger because of inflammatory changes in the jaw. The MCW may have been larger in the ONJ+ group than in the ONJ− group because of the greater cumulative effects of long-term BP administration. The MCW in the ONJ− group may have been smaller than the unmedicated group because of changes caused by osteoporosis. Differences between our study and Torres’ report may have been caused by differences in patient ratios.
The definition of Class II MCI according to Klemetti et al. includes the presence of semilunar defects of the endosteal margin and the formation of endosteal cortical residues [26]. In this study, the frequency of Class II MCI on the affected side in the ONJ+ group was significantly higher than in the other groups. Class II MCI on the affected side may not indicate the presence of a bone defect as in the original definition. Treatment with BPs could cause additional bone formation on the thinned cortex, resulting in roughening of the endosteal margin and thus evaluation as Class II. The frequency of Class II MCI on the unaffected side in the ONJ+ group also tended to be higher than in the ONJ− group, although this difference was not significant, with a borderline P value. If jaws with Class II MCI become inflamed, a higher frequency of BRONJ development is predicted, that is, Class II MCI should be listed as a possible factor leading to the development of BRONJ. This association was confirmed by the results of logistic regression analysis, which revealed an odds ratio near 3.00. It was predicted that Class II MCI according to the original definition would usually increase with age, even in the unmedicated group. Alternatively, Class II MCI in this study may represent BP-related thickening of the cortex previously thinned by osteoporosis. In any case, follow-up is important in BP-treated patients.
Sclerosis of trabecular bone was more frequently observed on the affected side in the ONJ+ group than on the contralateral side or in the other groups. Therefore, sclerosis was considered a characteristic finding leading to the development of BRONJ.
The frequency of thickening of the lamina dura was significantly higher in the BP-medicated (ONJ+ and ONJ−) groups than in the unmedicated group. Thus, thickening of the lamina dura was considered a characteristic finding caused by BP administration.
A weak point of this study is the difficulty of image evaluation. MCW and MCI have been used worldwide as screening tools for diagnosing osteoporosis [22,23,24,25,26]. However, evaluation of MCI is difficult, even when undertaken by specialists [28]. The analysis system used in this study, which was developed for osteoporosis screening, can record MCW and MCI at the same time [20,21,22]. In this study, MCW was obtained with the system and MCI was evaluated with reference to the results of the system. The system’s accuracy in the diagnosis of osteoporosis is more than 90% [20,21,22]. Clinical evaluation may be improved by the development of advances such as computer-assisted diagnosis.
Qualitative evaluation of sclerosis and thickening is problematic, because there are no measurable indicators such as CT values. Evaluation of sclerosis of trabecular bone and thickening of the lamina dura in our study was undertaken by two specialists, and showed fair-to-good agreement as measured by κ values. If clinicians are trained in the evaluation of images, the results of this study may be clinically useful.
In conclusion, Class II MCI could be useful as an indicator to predict the development of BRONJ. Sclerosis of trabecular bone can be considered a characteristic imaging finding in BRONJ. Thickening of the lamina dura could be an imaging feature caused by BP administration.
References
Marx RE. Pamidronate (Aredia) and zoledronate (Zometa) induced avascular necrosis of the jaws: a growing epidemic. J Oral Maxillofac Surg. 2003;61:1115–7.
Phal PM, Myall RW, Assael LA, Weissman JL. Imaging findings of bisphosphonate-associated osteonecrosis of the jaws. AJNR Am J Neuroradiol. 2007;28:1139–45.
Guo Y, Wang D, Wang Y, Peng X, Guo C. Imaging features of medicine-related osteonecrosis of the jaws: comparison between panoramic radiography and computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol. 2016;122:e69–76.
Farias DS, Zen Filho EV, de Oliveira TF, Tinôco-Araújo JE, Sampieri MB, Antunes HS, et al. Clinical and image findings in bisphosphonate-related osteonecrosis of the jaws. J Craniofac Surg. 2013;24:1248–51.
Krishnan A, Arslanoglu A, Yildirm N, Silbergleit R, Aygun N. Imaging findings of bisphosphonate-related osteonecrosis of the jaw with emphasis on early magnetic resonance imaging findings. J Comput Assist Tomogr. 2009;33:298–304.
Mücke T, Deppe H, Hein J, Wolff KD, Mitchell DA, Kesting MR, et al. Prevention of bisphosphonate-related osteonecrosis of the jaws in patients with prostate cancer treated with zoledronic acid—a prospective study over 6 years. J Craniomaxillofac Surg. 2016;44:1689–93.
Paek SJ, Park WJ, Shin HS, Choi MG, Kwon KH, Choi EJ. Diseases having an influence on inhibition of angiogenesis as risk factors of osteonecrosis of the jaw. J Korean Assoc Oral Maxillofac Surg. 2016;42:271–7.
Otto S, Tröltzsch M, Jambrovic V, Panya S, Probst F, Ristow O, et al. Tooth extraction in patients receiving oral or intravenous bisphosphonate administration: a trigger for BRONJ development? J Craniomaxillofac Surg. 2015;43:847–54.
Huang YF, Chang CT, Muo CH, Tsai CH, Shen YF, Wu CZ. Impact of bisphosphonate-related osteonecrosis of the jaw on osteoporotic patients after dental extraction: a population-based cohort study. PLoS One. 2015;10:e0120756.
Reiss S, Sultan D. Risk factors in the development of oral bisphosphonate-induced osteonecrosis. N Y State Dent J. 2015;81:30–3.
Polymeri AA, Kodovazenitis GJ, Polymeris AD, Komboli M. Bisphosphonates: clinical applications and adverse events in dentistry. Oral Health Prev Dent. 2015;13:289–99.
Mücke T, Krestan CR, Mitchell DA, Kirschke JS, Wutzl A. Bisphosphonate and medication-related osteonecrosis of the jaw: a review. Semin Musculoskelet Radiol. 2016;20:305–14.
Kim HY, Kim JW, Kim SJ, Lee SH, Lee HS. Uncertainty of current algorithm for bisphosphonate-related osteonecrosis of the jaw in population-based studies: a systematic review. J Bone Miner Res. 2016 (in press).
Taniguchi T, Ariji Y, Nozawa M, Naitoh M, Kuroiwa Y, Kurita K, et al. Computed tomographic assessment of early changes of the mandible in bisphosphonate-treated patients. Oral Surg Oral Med Oral Pathol Oral Radiol. 2016;122:362–72.
Klingelhöffer C, Klingelhöffer M, Müller S, Ettl T, Wahlmann U. Can dental panoramic radiographic findings serve as indicators for the development of medication-related osteonecrosis of the jaw? Dentomaxillofac Radiol. 2016;45:20160065.
Torres SR, Chen CS, Leroux BG, Lee PP, Hollender LG, Lloid M, et al. Mandibular inferior cortical bone thickness on panoramic radiographs in patients using bisphosphonates. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;119:584–92.
Ruggiero SL, Dodson TB, Fantasia J, Goodday R, Aghaloo T, Mehrotra B, et al. American Association of Oral and Maxillofacial Surgeons. American Association of Oral and Maxillofacial Surgeons position paper on medication-related osteonecrosis of the jaw–2014 update. J Oral Maxillofac Surg. 2014;72:1938–56.
Ruggiero SL, Dodson TB, Assael LA, Landesberg R, Marx RE, Mehrotra B. American Association of Oral and Maxillofacial Surgeons position paper on bisphosphonate-related osteonecrosis of the jaws–2009 update. J Oral Maxillofac Surg. 2009;67:2–12.
Muramatsu C, Matsumoto T, Hayashi T, Hara T, Katsumata A, Zhou X, et al. Automated measurement of mandibular cortical width on dental panoramic radiographs. Int J Comput Assist Radiol Surg. 2013;8:877–85.
Muramatsu C, Horiba K, Hayashi T, Fukui T, Hara T, Katsumata A, et al. Quantitative assessment of mandibular cortical erosion on dental panoramic radiographs for screening osteoporosis. Int J Comput Assist Radiol Surg. 2016;11:2021–32.
Katsumata A, Fujita H, Taguchi A, Ariji Y, Ariji E. Computer analysis of mandibular cortex morphology for screening of osteoporosis. J Jpn Stomatol Soc. 2016;65:256–63 (in Japanese).
Taguchi A, Suei Y, Sanada M, Ohtsuka M, Nakamoto T, Sumida H, et al. Validation of dental panoramic radiography measures for identifying postmenopausal women with spinal osteoporosis. AJR Am J Roentgenol. 2004;183:1755–60.
Taguchi A, Suei Y, Ohtsuka M, Otani K, Tanimoto K, Ohtaki M. Usefulness of panoramic radiography in the diagnosis of postmenopausal osteoporosis in women. Width and morphology of inferior cortex of the mandible. Dentomaxillofac Radiol. 1996;25:263–7.
Taguchi A, Tanimoto K, Suei Y, Wada T. Tooth loss and mandibular osteopenia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;79:127–32.
Taguchi A, Suei Y, Sanada M, Higashi Y, Ohtsuka M, Nakamoto T, et al. Detection of vascular disease risk in women by panoramic radiography. J Dent Res. 2003;82:838–43.
Klemetti E, Kolmakov S, Kröger H. Pantomography in assessment of the osteoporosis risk group. Scand J Dent Res. 1994;102:68–72.
Leite AF, dos Santos Ogata F, de Melo NS, de Souza Figueiredo PT. Imaging findings of bisphosphonate-related osteonecrosis of the jaws: a critical review of the quantitative studies. Int J Dent. 2014;2014:784348.
Ariji Y, Katsumata A, Kubo R, Taguchi A, Fujita H, Ariji E. Factors affecting observer agreement in morphological evaluation of mandibular cortical bone on panoramic radiographs. Oral Radiol. 2017;33:117–23.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The authors received no funding for this study.
Conflict of interest
Ryota Kubo, Yoshiko Ariji, Tohru Taniguchi, Michihito Nozawa, Akitoshi Katsuma, and Eiichiro Ariji declare that they have no conflicts of interest.
Human rights statements
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later versions.
Informed consent
Informed consent was obtained from all patients for being included in the study.
Animal rights statement
This article does not contain any studies with human or animal subjects performed by any of the authors. Panoramic radiographic features predict the development of bisphosphonate-related osteonecrosis of the jaw.
Rights and permissions
About this article
Cite this article
Kubo, R., Ariji, Y., Taniguchi, T. et al. Panoramic radiographic features that predict the development of bisphosphonate-related osteonecrosis of the jaw. Oral Radiol 34, 151–160 (2018). https://doi.org/10.1007/s11282-017-0293-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11282-017-0293-9