Abstract
Caring for a family member with cancer is often associated with significant cognitive, emotional, and physical demands. Although considerable research has explored informal cancer caregiver role burden, research has seldom focused on the experiences of individuals who hold the dual role of informal caregiver and healthcare professional. This qualitative study begins to explore this dual role experience. Participants (N = 12) who had at least 1 year of prior professional experience and cared for a family member with cancer were recruited conveniently from a large university-affiliated hospital in Montreal, Quebec. Individual face-to-face semi-structured interviews were conducted. Using thematic analysis, key themes were developed from verbatim transcripts: (1) salient dual role advantages, (2) significant challenges related to this role, (3) changes in professional practice as a consequence of informal caregiving, and (4) important palliative and end-of-life care access issues. Whereas professional knowledge helped advocate on behalf of patients, the dual role often came with over-solicitation from others, enhanced sense of responsibility, increased burden, and significant distress. Further study of critical ramifications linked to jointly enacting informal and professional caregiving across various health contexts should continue to inform supportive care strategies for this understudied yet increasingly prevalent segment of the caregiver population.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Dual roles in healthcare refer to contexts whereby an individual adopts at least two institutionally recognized roles [1]. Dual roles such as being a formal and informal caregiver can blur formal professional boundaries exposing the embedded, hidden assumptions associated with each role. Moreover, this duality can foster a re-examining of processes and practices that may not otherwise transpire and yield critical insights into professional training and supportive care strategies [2]. Previous research has primarily focused on healthcare professionals’ roles as educators, managers, or patients [3, 4 and 5], with less attention to healthcare professionals’ role as informal caregivers for medically ill family members. Moreover, due to the documented increased responsibility placed on informal caregivers [6] of patients with serious illnesses, cancer-related caregiving is particularly relevant to the study of dual role experiences. This context is particularly timely as healthcare and families face multiple challenges related to the provision of cancer care during the COVID-19 pandemic [7]. Thus, the present study aims to explore the experiences of health professionals who also provide informal support to a family member with cancer.
Caregiving in the context of cancer: benefits and challenges
Medical and technological advances such as more effective cancer treatment modalities have resulted in significant increases in cancer survivorship post-treatment [8]. This occurrence, coupled with demands for more home-care workers and services, has placed significant pressure on family members to provide informal care to individuals diagnosed with cancer [8]. An estimated 7.8 million Canadians serve as caregivers for a family member or close friend with a long-term health condition, disability, or aging-related issues [9], with cancer representing the second most common ailment requiring assistance from a caregiver [10]. These informal caregivers are often involved in multidimensional care while also taking on a wide range of other daily occupational tasks [10]. Both benefits and adverse consequences have been documented among informal cancer caregivers. According to a systematic review conducted by Li and Loke [11], informal cancer caregivers perceive various positive experiences in their supportive role across the cancer trajectory, including an enhanced relationship with the affected individual, the feeling of being rewarded by caregiving, overall life satisfaction, and a sense of personal growth. Similarly, Harvey and Berndt [12] identified multiple areas of informal cancer caregivers’ perceived personal growth, such as a greater desire to live in the moment and enhanced personal and spiritual connections. In addition, de Camargos et al.13 found that informal cancer caregivers (compared to the general population) reported more happiness and satisfaction with life despite also reporting lower positive affect and higher negative affect. These authors explain this counterintuitive finding by suggesting that informal cancer caregivers have “changed expectations about the future and increased valuing of simpler aspects of everyday life” [13].(p7)
Additional studies highlight that caregivers often feel ill-prepared to fulfill the caregiving role while experiencing psychological distress and negative health consequences [14, 15]. In some instances, physical and mental health consequences can be more significant for caregivers than patients [15,16,17]. A study assessing the prevalence of depression and anxiety in patients and their caregivers, for instance, found that caregivers reported significantly higher clinical depression rates than community norms [18]. While examining the long-term effects of depression and anxiety symptoms due to caregiving, another study found that these symptoms persisted or slightly decreased at 12-month post-diagnosis [16]. Further, patients’ and caregivers’ mental and physical health were found to influence each other and evolve in similar patterns. [19,20,21,22,23,24]
These findings prompted a call for cancer care teams to treat patients and their caregivers as dyads instead of as individual entities [23]. Consequently, Tolbert et al. [15] sought to identify the needs and expectations of caregivers across the cancer care trajectory. They found that caregivers were often expected to (a) be physically present in cancer clinics, communicate with providers, obtain and process information, and assist in decision-making; (b) provide medical care at home, communicate and provide emotional support, while assisting with unfamiliar or new tasks; and (c) adjust to a “new normal” by checking in with providers regarding patient’s needs, anticipate relationship changes, address emotional and physical needs, and cope with caregiver-patient disagreements on care needs and how to address them. These authors also found that caregiver burden could be reduced when provided with additional emotional, informational, and instrumental support in daily care activities at home. Although such support is undoubtedly beneficial, caregivers must often contend with co-existing and competing roles [25], adding to their caregiving needs and expectations. Moreover, informal cancer caregivers who are also healthcare professionals (ICC-HCPs) represent a particularly important segment of the population that may uniquely experience this duality in caregiving.
Healthcare-related dual role experiences in the context of cancer
ICC-HCPs can bring knowledge and skills acquired through their training and professional experiences that may buffer burden and enhance the caregiver role—hence, also benefiting patients [26]. These caregivers may be in a strategic position to mobilize support, access specialized cancer services, and obtain information that can further guide cancer-related decision-making, physical and emotional care, and follow-up [15]. However, this role duality may place additional pressure on them. Kim et al. [25] report that informal cancer caregivers’ psychological distress can significantly increase as a function of the number of social/occupational roles held. Moreover, adverse physical and emotional consequences have been documented among healthcare professionals who cared for family members or close friends [26,27,28]. However, this research has primarily focused on nurses’ experiences with less attention to physicians’ experiences. To our knowledge, the particular demand of cancer-related informal caregiving in the context of also being a healthcare professional has yet to be explored.
Using dual role experiences to inform formal and informal training
Health professional education and training hold key components that combine theory and practice with active clinical service [29]. ICC-HCPs possess both an “insider” and an “outsider” perspective as cancer caregivers. This duality can prompt distinct challenges that must be accounted for in curriculum development [29, 30]. Specifically, ICC-HCPs as “privileged informants” [2](p111) with experiential knowledge (i.e., learning by doing) may provide valuable insights into the nature of caregiving practices and processes. [2, 31]
Study purpose
The overarching goal of this study was to begin to explore participants’ views of their dual role as ICC-HCPs. The following questions guided this exploratory study:
-
(1)
What perceptions do ICC-HCPs have regarding their dual caregiving role?
-
(2)
How can these perceptions be used to guide efforts to support this increasingly prevalent group of caregivers?
Methods
Participants
Healthcare professionals were eligible to participate if they reported at least 1 year of professional work experience as a nurse or a physician and had cared for a family member diagnosed with cancer who has received treatment (e.g., chemotherapy, radiation, or surgery) within the last 10 years. They had to have been involved in informal caregiving at diagnosis, during treatment, or post-treatment and speak English or French fluently (the study was conducted in Quebec, Canada). Retired health professionals were also eligible. Enrolled participants (N = 12; 11 females and 1 male) were between the age of 31 and 83 (μ = 47) and included 7 nurses and 5 physicians. Participants’ relationships with patients included being a partner (n = 3), an adult child (n = 4), a sibling (n = 1), a parent (n = 1), in-laws (n = 2), or being a grandparent (n = 1).
Design
An exploratory descriptive qualitative design was used [32]. This design is generally used to explore an understudied phenomenon with the goal of providing detailed accounts [33]. This design is favored herein, given the scarcity of research concerning the ICC-HCP dual role.
Exploratory design and research reflexivity
The concept of reflexivity refers to the capacity to examine one’s beliefs and values during the research process and take an analytical stance toward those beliefs and values in light of study participants’ accounts [34]. Given the subjective nature of qualitative research, reflexivity is essential in better understanding how researchers are positioned relative to the research questions. In the current study, all authors have a background in health care. Specifically, AST was trained in counseling psychology, TLB and AK are psychologists, and CGL holds a doctorate in both nursing and psychology. In addition, two authors have experience with informal and formal cancer caregiving. Authors’ involvement in reflexivity included open dialog regarding each other’s personal and professional experiences and perceptions regarding the study’s main topic.
Procedures
Between August 2018 and April 2019, potential participants were primarily recruited via a volunteer-based organization of a large university-affiliated cancer center in Montreal, Quebec. Recruitment strategies included posting flyers, social media announcements, information booths, and word-of-mouth. Word-of-mouth was particularly effective. Interested participants were contacted by telephone to explain the study in more detail, screen for eligibility, and schedule a date, time, and place for the interview. Interviews lasted between 40 and 60 min and took place in the hospital, in a private location, or at the participant’s home. All interviews were conducted and transcribed by the senior author (AST). The McGill University Research Ethics Board approved this study and all participants provided written informed consent.
Based on pragmatic considerations and judgment, it was initially estimated that twelve to fifteen participants would be needed—a sample size consistent with an inductive, exploratory methodology [35, 36]. A semi-structured interview guide was developed by AST and CGL. Table 1 presents sample questions. In addition, socio-demographic information was collected post-interview using a brief self-report questionnaire.
Thematic analysis
Interviews were digitally audio-recorded, transcribed verbatim, and analyzed thematically [37, 38]. As per Braun and Clarke [39], thematic analysis combines new knowledge from the data (i.e., participants’ verbatim) with the existing literature to enrich understanding and meanings attributed to the phenomenon of interest. Initially, the senior author (AST) prepared and reviewed the transcripts several times to produce key content. Particular sentences or words were highlighted and inductively coded according to their relationships to the dual role concept. Next, codes were compared and contrasted to capture similarities and differences among them and a preliminary coding structure was created with key themes and sub-themes. AST then re-read the transcripts and highlighted quotes that appeared to best capture these themes. Subsequently, CGL and AK reviewed the preliminary coding, themes, and comments. Last, all authors discussed the findings and impressions and resolved potential interpretation discrepancies resulting in several interpreted themes and representative participant quotes.
Findings
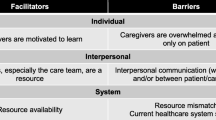
Participants reported several benefits and challenges related to the performance of their dual role. A salient advantage was that they felt well prepared to provide direct, hands-on care while drawing upon their professional knowledge and experience. They also reported feeling confident in guiding the patient as he or she navigated the complexities of the healthcare system. Ready access to pre-existing professional networks and contacts was reported to be beneficial to access the most relevant services, inform treatment-related decisions, and identify next steps in care. Already having medical knowledge and related vocabulary was reported as essential for effective communication with cancer care team members across the cancer trajectory from diagnosis, treatment, survivorship, or palliative care. When prompted about potential challenges, all participants reported feeling pressured, at times, to enact their professional roles while providing informal care. They also felt compelled to remain hyper-vigilant through the monitoring of their family member’s medical condition as it evolved. Many also struggled with the perceived pressure (internal and external) to provide sustained hands-on care. Their own sense of professional responsibility was particularly heightened when confronting care gaps or flaws in the health care delivery system. In addition, participants often struggled to find a balance between work and informal caregiving demands. More details are provided below with representative participant quotes.
Theme 1: salient dual role advantages
Participants reported that their professional experience consistently helped carry out their informal caregiving role; they felt well equipped to guide their affected family member regarding topics such as where to seek information, which healthcare profession to prioritize given a particular situation, what tests to request, and which medical steps should come next. A participant recalled instructing her family member who caught a cold a week before surgery to contact her general practitioner (GP) rather than the surgeon:
“You don’t call the surgeon when you have a respiratory infection, it is not his/her job. (…). The GP knew the surgery was planned in a week’s time. The GP told her to come right away for a scan and get antibiotics (P4).”
Another participant summed it up as follows:
“So you kind of take a role like explaining the healthcare system and honestly the initial challenges are navigating the healthcare system. Who do you talk to? What do you get? Who does what, you know? You will get the scan, but they will not tell you the result as soon as the scan is done (P13).”
Participants reported that having a network of contacts within the healthcare system also provided valuable guidance to their family member, such as obtaining referrals, seeking cancer-related information, or benefitting from a second opinion while contemplating treatment decisions. A participant recalled having reached out to colleagues to discuss a medication that the patient was prescribed:
“I can think of a few times that I would email physicians with whom I had been working with: Does it make sense that we jump up to this level of fentanyl (P4)?”
Participants all agreed that once their family member entered the healthcare system and became formally a patient, care became consistent and well-integrated, and the patient experience with cancer care evolved quite smoothly. They underscored that the real difficulty was health care system access at the outset—something made easier by participants already having access to a network of professionals and colleagues. Participants reported that their medical knowledge and associated professional vocabulary facilitated communication with cancer care team members. Most participants reported that they either readily disclosed their professional background or it became quickly evident as they exchanged medical terms and “jargon.”
“While discussing with the medical team, I felt like they went further in their reflection because I challenged them a little (P11).”
Some participants underscored how appreciative they were for having been included in tumor board meetings or invited to contribute their own expertise. Participants also reported having been welcomed within healthcare settings, whether they were employed on-site or not.
They also felt that their dual role was of great benefit when it came to providing direct, hands-on care for family members, such as assessing health status, treatment-related symptoms, and managing potential complications. They also got involved in medication administration, injections, wound care, and surgical stitch removal—circumventing time consuming visits to the hospital. One participant explains:
“… there was a small dosing problem with the tamoxifen she was taking. So rather than trying to set up an appointment with the specialist, which would have taken weeks and weeks, I was able to solve the question of dosage. Surely, we talked to the physician afterwards, but when we spoke to him it had already been three months since I had solved the problem (…) because I was able to look up how tamoxifen works (P3).”
Moreover, participants described being asked by their family member to advocate and make decisions on their behalf, a request they attributed to patient trust in their professional judgment. A participant recounted that her husband with cancer asked her to “protect him” and advocate on his behalf because he did not understand the medical terms used and counted on her to enforce his decision not to undergo treatment that would prolong his life (P9).
Some participants also recalled having a mediating role between the patient and the cancer care team when it came to interpreting medical information:
“My sister-in-law asked me to go with her. And when we got there, she went in with her husband and I stayed in the waiting room and then she came to get me. She needed me to come in because she did not understand [what the doctor was saying] (P5).”
Participants recounted that their role was not only limited to supporting the ill family member, but also included members of the extended family who had questions and wished to be kept in the loop in terms of the patient’s medical condition. All participants felt that their ICC-HCP role had saved time and energy and created a “safety net” for both the patient and extended family members.
Theme 2: significant challenges related to the dual role
Participants discussed disadvantages linked to this dual role. At times, they felt significant pressure from family and health care professionals (explicitly or implicitly) to enact their professional role. A participant recalled having recognized the rapidly declining health condition of her family member well ahead of anyone else:
“When I started to see signs of deterioration, signs of shortness of breath, other signs that the disease had progressed, that it had metastasized… I could see it way before anybody else, even before any scans or anything else, and thinking this is not good (…) So that is very hard. Because of the knowledge that you have as a healthcare provider, you know what is coming up, you know the risks… of chemotherapy, signs and symptoms of sepsis, risks of hospitalization, risks of post-op complications. So, you are looking at all these things and you are trying to keep the person calm, but you are understanding the risks much more than they are… (P5).”
Another participant, whose family member was nearing death, remembered having to decide whether to share her suspicions with other family members or let the medical team communicate the information:
“I shared my relative’s condition with my family because otherwise he could have died alone, but, on the other hand, I was wearing my nurse’s hat, staying vigilant and alert, feeling like [I was] taking away [their] hope (P8).”
A result of relying on their professional role in informal caregiving, participants felt they had to remain hyper-vigilant to detect potential changes in their family member’s condition and inform the medical team and other family members. For some, this type of vigilance hindered their ability to initiate the process of grieving the upcoming loss of their loved ones.
One participant described having flashbacks for several months after her family member’s death, remembering his agony and questioning the medical decisions she had made and whether she had done enough (P4). This often disrupted the ability to “let things go” and let other healthcare workers take responsibility for proving care to their family member; this was potentiated by having witnessed “incidents” or “errors” regarding their family member’s care. One participant explained:
“I could see certain things that I felt could be improved but then feeling like you cannot do everything for them, you know what I mean. So that was hard (P13).”
Another participant described that her attitude had completely changed after her family member experienced an allergic reaction to the medication:
“My attitude changed completely. Each time I was like: OK what did you give him? Did you give him that before? After that, I was there every time he had to get chemotherapy (P12).”
Participants also underscored feeling pressure—from themselves as well as members of the cancer care team—to be more directly involved in their family member’s care. A participant described that the medical team failed to refer her husband to the community clinic for dressing changes and medication monitoring. The team had assumed that as an ICC-HCP, she would take on those tasks (P1). Another participant recalled that the medical team expected her to perform demanding care tasks (e.g., to turn a bedridden family member) but refrain from performing other care tasks:
“It’s like, if it is convenient to them it is OK, but if they have to work a bit more…it’s a different story (P12).”
Being confronted with gaps/flaws in the healthcare system, paired with their own heightened sense of professional responsibility, was challenging for some. The monitoring of healthcare professional practices such as differing hand washing procedures or the lack of professionalism in introducing themselves was discussed. One participant recounts:
“The number of times I saw nurses walk in not even look at my father-in-law and write their names on the board. Like no introduction, be like: Do you have any pain? I am like: Who are you? What is your role, like just the basics you know? (P13).”
Participants reported struggling to find a balance between being a formal and an informal cancer caregiver. Many tried to cope with the initial shock of the diagnosis and the ensuing distress upon witnessing their family member’s decline, all while attending to other important life demands, such as working/studying full-time, raising children, and caring for other family members. Many reported not having any respite from caregiving and they compared this to a grueling marathon. One participant recalled:
“It is physically stressful. To be a caregiver, you become aware of your helplessness (P7).”
Participants also described having difficulty setting aside their professional role as they were constantly either working or caregiving:
“That was hard, I was not able to escape (…) It was not easy. You go outside and it is like the sun is brighter than usual. Like you have to reconnect with a lot of things, you had turned off (P8).”
Another described: “Because I went with her to each appointment…and they would tell her this news and I would support her. So, in a way it was good because it was very supportive for her, but for me it was detrimental (P5).”
Participants who worked at the same hospital where their family member was being treated reported learning about the family member’s new health issues during working hours, making it difficult to cope and continue working. Also, some said that this dual role made them more likely to be solicited by another family member. One participant said:
“But then you think of yourself: I cannot go through this again, I cannot do it again. Like if my husband gets sick, I won’t be able, you know. So, you just hope that it doesn’t happen… but you know it will happen again and you will just have to deal with it. It is not something you can run away from when you are part of the system (P5).”
Theme 3: changes in professional practice as a consequence of informal caregiving
Participants reported that the caregiving experience changed their personal approach to professional practice, as well as their relationships with patients and co-workers. On a personal level, participants reported having gained a deeper understanding of patient and family’s contributors to burden. One participant shared:
“When you live it, it’s different. You cannot say that you understand what the person is going through, but you understand a little. Not exactly everything, but you can understand because you have been there. It is not easy, especially for caregivers (P2).”
They described having realized how wait times, for instance, can negatively affect patients and caregivers’ morale. Participants acknowledged that whereas delays are often inevitable, demonstrating empathy and listening to concerns can be comforting. Participants reported that their experience as a caregiver reminded them of the degree to which “basics”—such as introducing themselves, repeating information periodically, and conveying courtesy toward differing family values and beliefs is important.
One participant shared: “This experience allowed me to see how patients and caregivers actually feel about what might seem like harmless to a nurse (P11).” She also mentioned learning from the approach of her mother’s doctor: “I learn a lot about how she [the doctor] treats her patients, the way she approaches them, listens and talks to them, she is really amazing. I think it will have repercussions [on my practice] because it inspired me so much. (P11).” Another participant recalled: “When you are a caregiver and the nurse explains how to provide certain types of care and it is not working, you feel lost. This feeling, I had. I understand completely how families can feel. You try to do things and it is not working (P2).” Yet another participant reported that she now touches base with family caregivers and discusses self-care with them: “I have to say I spend much more time pulling caregivers aside and making sure not only that they know the right things to do for the patient but also focusing on the [caregiver] health (P4).”
Regarding changes in co-worker relationships, one participant mentioned that she was able to recognize difficult family situations and advocate on their behalf in multidisciplinary meetings. Another mentioned that she was able to share and discuss her experience with professional colleagues (P12). One participant noted that she uses examples from her own caregiving experience when teaching medical students (P13).
Theme 4: important palliative and end-of-life care access issues
Participants who reported caring for a family member with advanced cancer while also working in oncology commented on the rarity of team discussions about palliative/end-of-life within the team and with patients and family members. One participant reported: “Except when it is time for palliative or end-of-life care, people don’t talk about it. His doctor did not tell him that he was in palliative care. Even the treating doctor said nothing when we decided not to do the biopsy, nor continue treatment (P8).”
Participants discussed the need for addressing palliative care options early to help their family member navigate the different services available and explore symptom management options related to advanced cancer to ensure comfort at end-of-life. A participant explained: “And, so that hurt me, knowing that there was limited time… it doesn’t bother them [cancer team members] because they don’t see it any differently but I was like, maybe his last few months could have been better. Pain-free, you know (P13).” Participants expressed concerns regarding confusion over what palliative care entails, when to talk about it, and patients’ rights: “I am sure that 75% of the population does not know that they have the right to have palliative care at home, to have a private room at the hospital, that it is about control and ease the pain, that you don’t have to endure pain symptoms and that there are solutions.” They also talked about how difficult it was to have access to palliative care services, particularly when the patient condition was deteriorating rapidly: “I wondered if he would have gotten more attention to his mental health if he would have been in palliative care earlier, like months prior to when he was. (…) So, my in-law received no resources from the cancer center really. It was so quick and such a decline that they were not able to tap into any type of family counseling even though they said they were interested in it (P13).” Participants also expressed concerns regarding the negative undertones of the term “palliative care,” suggesting that “supportive care” may serve as a more accurate and less frightening term, given its primary goal is to optimize quality of life, reduce physical and psychological symptoms, help adjust to imminent death, and support families through the process and following death. Participants also shared that caring for a family member at end-of-life altered their beliefs and values. One participant discussed the importance of working toward “a good death” and that decisions about extending a patient’s life should consider quality over quantity of life.
Discussion
In exploring ICC-HCPs’ experiences, key insights, meanings, and consequences were gained linking formal and informal caregiving roles. ICC-HCPs’ knowledge of the healthcare system, for instance, was often instrumental in assisting patients to readily access care, saving time and energy for both patients and caregivers, and informing next steps in hospitalization, treatment, and follow-up care. Reliance on their professional knowledge was construed as a positive, providing them with a sense of control and empowerment. This point is consistent with previous findings whereby caregivers’ self-efficacy was increased when symptom management training strategies were part of supportive interventions. [40, 41]
The ICC-HCP dual role was also reported, at times, to increase overall caregiving burden. Having the propensity to do more, participants reported feeling internal and external pressures to be more actively involved in caregiving tasks and advocate for affected family members. Enacting their professional role within the cancer care system often hindered their ability to take time away from these demands. In addition, some even felt that their professional background prevented them from actively grieving, as they felt that they had to remain strong even during and post end-of-life. These observations are consistent with previous findings indicating that caregiver burden increases in response to co-existing and competing roles [25]. Moreover, considering previous findings that caregivers still experience unmet needs up to 24 months following a patient diagnosis [20], more attention concerning ICC-HCPs’ needs is warranted. It is also critical that greater awareness surrounding ICC-HCPs’ supportive resources be promoted such as psychosocial oncology interventions offered by cancer care settings and community support services.
ICC-HCPs reported that the caregiving experience influenced their professional practice (and vice-versa), particularly with a renewed focus on patient-caregiver communication. They began paying more attention to caregivers (in addition to patients) while encouraging the former to take time away from their caregiver role and re-engage in self-care. In addition, some reported being inspired by the cancer care team and wanting to enact those behaviors and integrate this new knowledge into their professional practice. Such findings are consistent with the view that clinical skills are context-specific and best learned over time in authentic and supportive settings [42, 43]. As this study shows, these settings can extend to ones where boundaries between the personal and professional domains are imprecise. Such findings also illustrate the value of immersion and perspective taking in healthcare education and practice and the need for emerging digital technologies to support experiential learning. [44]
Some ICC-HCPs also reported important access issues pertaining to palliative and end-of-life care. For instance, service gaps were particularly salient at crucial transition points on the cancer care trajectory with definitional uncertainty about what palliative and end-of-life care entailed. Likewise, Ryan et al. [45] argue for a redefinition of palliative and end-of-life care to “reduce misconceptions, facilitate clinical and academic development, and promote effective communication.” [45](p1), particularly around end-of-life discussions. A recent systematic review [46] found that end-of-life discussions were associated with significantly lower likelihood of being admitted into an acute or intensive care unit, more reliance on hospice care, and more likelihood of death outside hospitals. Some of our participants reiterated the need for better integration of palliative and end-of-life care to more readily address patients’ and caregivers’ needs and preferences.
Overall, the study findings bring forth key aspects of ICC-HCPs’ experiences and suggest that even if professional knowledge is beneficial, there is a higher risk of being over-solicited by close and extended social networks. Therefore, caregiving can be a significant burden even for individuals familiar with the health care system who possess extant professional experience and knowledge. Consequently, with the current health care system putting increased responsibilities on family members to care for patients, addressing informal and formal caregivers’ potential distress and burnout should be a priority [47]. In sum, caregivers may need professional support during and after caregiving episodes, regardless of their professional background. This support is paramount as research shows that in the year following diagnosis, caregivers’ physical and psychological health tends to significantly decline even if the patient’s health improves. [48]
Implications for healthcare professional education and training
The present study’s findings can shed insight into professional education and training priorities and opportunities. Trainees can be encouraged to reflect on their personal and professional caregiving experiences (e.g., using deliberate introspection activities). This practice is essential as burnout significantly contributes to staff absenteeism and turnover [49, 50]. Moreover, through greater dual role awareness, healthcare professionals may be better equipped to identify and respond to distress in family caregivers, fostering an increased capacity to relate to and engage with them as whole persons. [51]
Furthermore, professionals in training should be provided with more palliative and end-of-life curriculum content. This focus aligns with the World Health Organization’s assertion that the integration of palliative care services has been hindered due to a lack of health professional education and training [52]. From a clinical perspective, Hawley [53] states several reasons for low referrals to palliative care services. The author cites “ignorance [among healthcare professionals] regarding what palliative care is.” [53](p 2) Likewise, Artioli et al. [54] have pressed for the need to systematically assess palliative care knowledge and skills among healthcare professionals in training.
Limitations
There are a few limitations to this study. First, the sample consisted mainly of women, with only one male participant. Hence, the findings may reflect, in large part, a female perspective on the phenomenon of interest. Second, because of its cross-sectional nature, investigators did not return to participants to clarify or deepen the meaning of the verbatim collected. Third, exploration of the dual role was restricted to nurses and physicians only. A broader perspective would extend to the experiences of psychosocial oncology professionals such as psychologists and social workers.
Future research
Future work would further address the specific supportive unmet needs of ICC-HCPs according to more varied contexts. In addition, how ICC-HCPs’ experiences evolve throughout the cancer trajectory, including during the survivorship phase, advanced cancer stages, and post-death among bereaved caregivers. With this new knowledge, person-centered supportive interventions could be developed, tested, and implemented for this unique caregiving group.
Data availability
Data from this study are available from the senior author upon request.
Code availability
Not applicable.
References
Reitz R, Simmons PD, Runyan C, Hodgson J, Carter-Henry S (2013) Multiple role relationships in healthcare education. Fam Syst Health 31(1):96–107. https://doi.org/10.1037/a0031862
Rowland P, Kuper A (2018) Beyond vulnerability: how the dual role of patient-health care provider can inform health professions education. Adv Health Sci Educ Theory Pract 23(1):115–131. https://doi.org/10.1007/s10459-017-9777-y
Prenkert M, Carlsson E, Svantesson M, Anderzén-Carlsson A (2017) Healthcare-professional patients’ conceptions of being ill and hospitalised - a phenomenographic study. J Clin Nurs 26(11–12):1725–1736. https://doi.org/10.1111/jocn.13604
Imran D, Rog K, Gallichio J, Alston L (2021) The challenges of becoming and being a clinician manager: a qualitative exploration of the perception of medical doctors in senior leadership roles at a large Australian health service. BMC Health Serv Res 21(1):1–9. https://doi.org/10.1186/s12913-021-06356-w
Spehar I, Frich JC, Kjekshus LE (2012) Clinicians’ experiences of becoming a clinical manager: a qualitative study. BMC Health Serv Res 12(1):1–11. https://doi.org/10.1186/1472-6963-12-421
van Ryn M, Sanders S, Kahn K et al (2011) Objective burden, resources, and other stressors among informal cancer caregivers: a hidden quality issue? Psychooncology 20(1):44–52. https://doi.org/10.1002/pon.1703
Lawler M. Cancer must not be the forgotten “C” in the fight against COVID-19. The BMJ Opinion. Published May 11, 2021. Accessed June 14, 2021. https://blogs.bmj.com/bmj/2021/05/11/cancer-must-not-be-the-forgotten-c-in-the-fight-against-covid-19/
Gilmour H. Unmet home care needs in Canada. Health Rep. 2018;29(11):3–11. https://www150.statcan.gc.ca/n1/pub/82-003-x/2018011/article/00002-eng.pdf. Accessed June 14, 2021
Statistics Canada. Caregivers in Canada, 2018. The Daily. Published 2020. Accessed June 14, 2021. https://www150.statcan.gc.ca/n1/daily-quotidien/200108/dq200108a-eng.htm
Sinha M. Portrait of caregivers, 2012. Statistics Canada. Published 2013. Accessed June 14, 2021. https://www150.statcan.gc.ca/n1/pub/89-652-x/89-652-x2013001-eng.htm
Li Q, Loke AY (2013) The positive aspects of caregiving for cancer patients: a critical review of the literature and directions for future research. Psychooncology 22(11):2399–2407. https://doi.org/10.1002/pon.3311
Harvey J, Berndt M (2020) Cancer caregiver reports of post-traumatic growth following spousal hematopoietic stem cell transplant. Anxiety Stress Coping 34(4):397–410. https://doi.org/10.1080/10615806.2020.1845432
de Camargos MG, Paiva BSR, de Oliveira MA et al (2020) An explorative analysis of the differences in levels of happiness between cancer patients, informal caregivers and the general population. BMC Palliat Care 19(1):106. https://doi.org/10.1186/s12904-020-00594-1
Dri E, Bressan V, Cadorin L et al (2020) Providing care to a family member affected by head and neck cancer: a phenomenological study. Supportive Care Cancer 28(5):2105–2112. https://doi.org/10.1007/s00520-019-05026-2
Tolbert E, Bowie J, Snyder C, Bantug E, Smith K (2018) A qualitative exploration of the experiences, needs, and roles of caregivers during and after cancer treatment: “That’s what I say. I’m a relative survivor.” J Cancer Surviv. 12(1):134–144. https://doi.org/10.1007/s11764-017-0652-x
Lambert SD, Girgis A, Lecathelinais C, Stacey F (2013) Walking a mile in their shoes: anxiety and depression among partners and caregivers of cancer survivors at 6 and 12 months post-diagnosis. Support Care Cancer 21(1):75–85. https://doi.org/10.1007/s00520-012-1495-7
Teixeira RJ, Applebaum AJ, Bhatia S, Brandão T (2018) The impact of coping strategies of cancer caregivers on psychophysiological outcomes: an integrative review. Psychol Res Behav Manag 11:207–215. https://doi.org/10.2147/PRBM.S164946
Price MA, Butow PN, Costa DSJ et al (2010) Prevalence and predictors of anxiety and depression in women with invasive ovarian cancer and their caregivers. Med J Aust 193(S5):S52–S57. https://doi.org/10.5694/j.1326-5377.2010.tb03929.x
Beesley VL, Price MA, Webb PM (2011) Australian Ovarian Cancer Study Group, Australian Ovarian Cancer Study—Quality of Life Study Investigators. Loss of lifestyle: health behaviour and weight changes after becoming a caregiver of a family member diagnosed with ovarian cancer. Support Care Cancer. 19(12):1949–1956. https://doi.org/10.1007/s00520-010-1035-2
Girgis A, Lambert S, Johnson C, Waller A, Currow D (2013) Physical, psychosocial, relationship, and economic burden of caring for people with cancer: a review. J Oncol Pract 9(4):197–202. https://doi.org/10.1200/JOP.2012.000690
Hagedoorn M, Sanderman R, Bolks HN, Tuinstra J, Coyne JC (2008) Distress in couples coping with cancer: a meta-analysis and critical review of role and gender effects. Psychol Bull 134(1):1–30. https://doi.org/10.1037/0033-2909.134.1.1
Kurtz ME, Kurtz JC, Given CW, Given BA (2004) Depression and physical health among family caregivers of geriatric patients with cancer—a longitudinal view. Med Sci Monit. 10(8):CR447-CR456. https://pubmed.ncbi.nlm.nih.gov/15277994/. Accessed June 14, 2021
Kershaw T, Ellis KR, Yoon H, Schafenacker A, Katapodi M, Northouse L (2015) The interdependence of advanced cancer patients’ and their family caregivers’ mental health, physical health, and self-efficacy over time. Ann Behav Med 49(6):901–911. https://doi.org/10.1007/s12160-015-9743-y
Rohleder N, Marin TJ, Ma R, Miller GE (2009) Biologic cost of caring for a cancer patient: dysregulation of pro- and anti-inflammatory signaling pathways. J Clin Oncol 27(18):2909–2915. https://doi.org/10.1200/JCO.2008.18.7435
Kim Y, Baker F, Spillers RL, Wellisch DK (2006) Psychological adjustment of cancer caregivers with multiple roles. Psychooncology 15(9):795–804. https://doi.org/10.1002/pon.1013
Detaille SI, de Lange A, Engels J et al (2020) Supporting double duty caregiving and good employment practices in health care within an aging society. Front Psychol 11:535353. https://doi.org/10.3389/fpsyg.2020.535353
Boumans NPG, Dorant E (2014) Double-duty caregivers: healthcare professionals juggling employment and informal caregiving. A survey on personal health and work experiences. J Adv Nurs. 70(7):1604–1615. https://doi.org/10.1111/jan.12320
Giles TM, Williamson V (2015) Torn between dual roles: the experiences of nurse-family members when a loved one is hospitalised in a critical condition. J Clin Nurs 24(21–22):3095–3106. https://doi.org/10.1111/jocn.12900
Hays RB, Ramani S, Hassell A (2020) Healthcare systems and the sciences of health professional education. Adv Health Sci Educ Theory Pract 25(5):1149–1162. https://doi.org/10.1007/s10459-020-10010-1
Thibault GE (2020) The future of health professions education: emerging trends in the United States. FASEB Bioadv 2(12):685–694. https://doi.org/10.1096/fba.2020-00061
Castro EM, Van Regenmortel T, Sermeus W, Vanhaecht K (2019) Patients’ experiential knowledge and expertise in health care: a hybrid concept analysis. Soc Theory Health 17(3):307–330. https://doi.org/10.1057/s41285-018-0081-6
Polit DF, Beck CT (2017) Nursing research: generating and assessing evidence for nursing practice. Tenth edn. Philadelphia, PA: Wolters Kluwer Health
Hunter DJ, McCallum J, Howes D (2019) Defining exploratory-descriptive (EDQ) research and considering its application in healthcare. J Nurs Healthc 4(1):180272
Lazard L, McAvoy J (2020) Doing reflexivity in psychological research: what’s the point? What’s the practice? Qual Res Psychol 17(2):159–177. https://doi.org/10.1080/14780887.2017.1400144
Braun V, Clarke V (2021) To saturate or not saturate? Questioning data saturation as a useful concept for thematic analysis and sample-size rationales. Qual Res Sport Exerc Health 13(2):201–216. https://doi.org/10.1080/2159676X.2019.1704846
Sim J, Saunders B, Waterfield J, Kingston T (2018) Can sample size in qualitative research be determined a priori? Int J Soc Res Methodol. 21(5):619–634. https://doi.org/10.1080/13645579.2018.1454643
Creswell JW, Poth CN (2018) Qualitative inquiry & research design: choosing among five approaches. Fourth edn. Thousand Oaks, CA: SAGE
Meadows L, Morse J (2001) Constructing evidence within the qualitative project. In: Morse J, Swanson J, Kuzel A (eds) The nature of qualitative evidence. Thousand Oaks, CA: SAGE: 188–202
Braun V, Clarke V (2006) Using thematic analysis in psychology. Qual Res Psychol 3(2):77–101. https://doi.org/10.1191/1478088706qp063oa
Hendrix CC, Bailey DE, Steinhauser KE et al (2016) Effects of enhanced caregiver training program on cancer caregiver’s self-efficacy, preparedness, and psychological well-being. Support Care Cancer 24(1):327–336. https://doi.org/10.1007/s00520-015-2797-3
Hendrix CC, Landerman R, Abernethy AP (2013) Effects of an individualized caregiver training intervention on self-efficacy of cancer caregivers. West J Nurs Res 35(5):590–610. https://doi.org/10.1177/0193945911420742
Patel S, Pelletier-Bui A, Smith S et al (2019) Curricula for empathy and compassion training in medical education: a systematic review. PLoS ONE 14(8):e0221412. https://doi.org/10.1371/journal.pone.0221412
van der Vleuten C, van den Eertwegh V, Giroldi E (2019) Assessment of communication skills. Patient Educ Couns 102(11):2110–2113. https://doi.org/10.1016/j.pec.2019.07.007
Schulz R, Hara T, Martinez, S (2019) Immersion and perspective taking in healthcare technology supporting healthcare professionals with daily tasks and clinical procedures. Proceedings of the 17th Scandinavian conference on health informatics. November 12-13. Oslo, Norway. https://ep.liu.se/en/conference-article.aspx?series=&issue=161&Article_No=12. Accessed 27 Oct 2021
Ryan S, Wong J, Chow R, Zimmermann C (2020) Evolving definitions of palliative care: upstream migration or confusion? Curr Treat Options Oncol 21(3):1–7. https://doi.org/10.1007/s11864-202-0716-4
Starr LT, Ulrich CM, Corey KL, Meghani SH (2019) Associations among end-of-life discussions, health-care utilization, and costs in persons with advanced cancer: a systematic review. Am J Hosp and Palliat Care 36(10):913–926. https://doi.org/10.1177/10499091198448148
Wittenberg E, Goldsmith J, Parnell TA (2020) Development of a communication and health literacy curriculum: optimizing the informal cancer caregiver role. Psychooncology 29(4):766–774. https://doi.org/10.1002/pon.5341
Shaffer KM, Kim Y, Carver CS (2016) Physical and mental health trajectories of cancer patients and caregivers across the year post-diagnosis: a dyadic investigation. Psychol Health 31(6):655–674. https://doi.org/10.1080/08870446.2015.1131826
Willard-Grace R, Knox M, Huang B, Hammer H, Kivlahan C, Grumbach K (2019) Burnout and health care workforce turnover. Ann Fam Med 17(1):36–41. https://doi.org/10.1370/afm.2338
Windover AK, Martinez K, Mercer MB, Neuendorf K, Boissy A, Rothberg MB (2018) Correlates and outcomes of physician burnout within a large academic medical center. JAMA Intern Med 178(6):856–858. https://doi.org/10.1001/jamainternmed.2018.0019
Sanchez-Reilly S, Morrison LJ, Carey E et al (2013) Caring for oneself to care for others: physicians and their self-care. J Support Oncol. 11(2):75–81. https://doi.org/10.12788/j.suponc.0003
World Health Organization (2014) Strengthening of palliative care as a component of integrated treatment throughout the life course. J Pain Palliat Care Pharmacother 28(2):130–134. https://doi.org/10.3109/15360288.2014.911801
Hawley P (2017) Barriers to access to palliative care. Palliat Care 10:1178224216688887. https://doi.org/10.1177/1178224216688887
Artioli G, Bedini G, Bertocchi E et al (2019) Palliative care training addressed to hospital healthcare professionals by palliative care specialists: a mixed-method evaluation. BMC Palliat Care 18(1):1–10. https://doi.org/10.1186/s12904-019-0476-8
Funding
We acknowledge the financial support of the Rossy Cancer Network to the senior author (AST). The McGill University Christine and Herschel Victor/Hope & Cope Chair in Psychosocial Oncology supports CGL’s research program.
Author information
Authors and Affiliations
Contributions
CGL conceived the original idea and designed the study. All authors performed the literature review. AST, CGL, and AK drafted the manuscript and conducted the thematic analysis. TLB revised the manuscript critically for important intellectual content and oversight. All authors contributed to the writing of the manuscript and approved the submitted version.
Corresponding author
Ethics declarations
Ethics approval
Approval was obtained from McGill University’s Research Ethics Board.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Santerre-Theil, A., Brown, T.L., Körner, A. et al. Exploring healthcare professionals’ experiences with informal family cancer caregiving. Support Care Cancer 30, 7745–7754 (2022). https://doi.org/10.1007/s00520-022-07207-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-022-07207-y