Abstract
Purpose
Olanzapine-containing regimens have been reported to be effective in preventing CINV following highly emetogenic chemotherapy (HEC), but it is unsure whether it is cost-effective. There has been no cost-effectiveness analysis conducted for olanzapine using costs from the USA. The aim of this study is to determine whether olanzapine-containing antiemetic regimens are cost-effective in patients receiving HEC.
Methods
A decision tree model was constructed to evaluate the cost and health outcomes associated with olanzapine-containing antiemetic regimens and otherwise-identical regimens. One-way sensitivity analyses were conducted to individually investigate the effect of (i) lower complete response (CR) rates of olanzapine, closer to non-olanzapine-containing regimens; (ii) higher FLIE scores for patients who achieved no/incomplete response, closer to FLIE scores of patients achieving a complete response; (iii) differing costs of olanzapine to reflect different costs per hospitals, globally, due to different insurance systems and drug costs; and (iv) varying costs for uncontrolled CINV, to account for varying durations of chemotherapy and accompanying uncontrolled CINV.
Results
Olanzapine regimens have an expected cost of $325.24, compared with $551.23 for non-olanzapine regimens. Meanwhile, olanzapine regimens have an expected utility/index of 0.89, relative to 0.87 for non-olanzapine regimens. Olanzapine-containing regimens dominate non-olanzapine-containing regimens even if CR of olanzapine-containing regimens fall to 0.63. Only when CR is between 0.60 and 0.62 is olanzapine both more effective and more costly.
Conclusion
Olanzapine-containing regimens are both cheaper and more effective in the prophylaxis of CINV in HEC patients, compared with non-olanzapine-containing regimens. Future CINV trial resources should be allocated to understand newer antiemetics and compare them to olanzapine-containing regimens as the control arm. Further analysis should use nationally representative data to examine medication costs by payer type.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients receiving chemotherapy for cancer frequently experience nausea and vomiting (CINV), two burdensome adverse events associated with significant morbidity, and deterioration of patient quality of life [1]. Significant CINV can also lead to other concerning clinical conditions, such as dehydration and malnutrition [2]. As a result, this can lead to non-adherence with chemotherapy treatments [3].
To control CINV, many different classes of antiemetic agents have been developed. Biochemically, the majority of these agents work as antagonists by targeting dopamine2 (D2) receptors (prochlorperazine, metoclopramide, domperidone, metopimazine), dopamine3 (D3) receptors (amisulpride), serotonin3 (5-HT3) receptors (ondansetron, granisetron, palonosetron, ramosetron), or neurokinin1 (NK1) receptors (aprepitant, netupitant, rolapitant). Cannabinoids act as agonists at cannabinoid1 (CB1) receptors, whereas the mechanism of action of corticosteroids (dexamethasone, prednisolone) is unknown [4,5,6,7,8,9]. Prior to 2017, the recommended prophylactic regimen by the American Society of Clinical Oncology (ASCO) [10] and the Multinational Association of Supportive Care in Cancer (MASCC)/European Society for Medical Oncology (ESMO) [11] was a three-drug regimen of a 5-HT3 receptor antagonist, dexamethasone, and a NK1 receptor antagonist for patients receiving highly emetogenic chemotherapy (HEC).
Over the past decade, olanzapine has been used off-label for both the prophylaxis and rescue of chemotherapy-induced nausea and vomiting. Olanzapine was originally approved by the Food and Drug Administration (FDA) for the treatment of psychotic disorders and was previously unproven in CINV. The rationale for employing it in the CINV setting is its biochemical properties—it is an inhibitor of serotonergic 5-HT2a, 5-HT2c, 5-HT3, and 5-HT6 receptors; dopaminergic D1, D2, D3, and D4 receptors; adrenergic α-1 receptors; and histaminic H1 receptors; conceptually, its binding affinity to multiple receptors showed promise in treating the effects of CINV [12, 13], in particular nausea.
Olanzapine has been studied in a number of phases 1–2, uncontrolled trials, and subsequently in randomized controlled trials (RCTs) [14, 15], and several reviews of the effect and safety of olanzapine have been published. In 2016, a systematic review and meta-analysis was conducted, comparing olanzapine-containing regimens to other antiemetic regimens, in both the prophylaxis and rescue of CINV [16]. Amalgamating data across 10 RCTs, the meta-analysis reported that olanzapine is more efficacious than other standard antiemetics for the rescue of CINV and its inclusion improves control in the prevention setting. In the overall phase (0–120 h post-chemotherapy), olanzapine achieved better emetic control (risk ratio (RR) = 1.41; 95% CI 1.18–1.68) and better nausea control (RR = 1.53; 95% CI 1.18–1.97).
In updated CINV guidelines, both ASCO [17] and MASCC/ESMO [18] recommend (with some differences) a new four-drug regimen for patients receiving HEC; olanzapine is now an option in addition to the three-drug regimen of a 5-HT3 receptor antagonist, dexamethasone, and a NK1 receptor antagonist. However, this recommendation was made without any cost analyses. Since then, Chanthawong et al. has conducted a cost-effectiveness analysis (CEA) in this setting, specifically using cost figures from Southeast Asian countries [19]. However, there has been no CEA conducted using costs from the USA, where spending on health care is higher than in any other country [20]. In the USA, the average treatment cost for all care associated with chemotherapy-induced nausea and vomiting (CINV) has been reported to be a burdensome $1854.70/day, speculating the need for cost-effective prophylactic CINV management [21]. Given the proven efficacy of olanzapine and recent recommendation in international guidelines, a CEA would further inform clinical guidelines and treatment practices in the USA. The aim of this study is to determine whether olanzapine-containing antiemetic regimens are cost-effective from a hospital perspective compared with other otherwise-identical regimens (i.e. solely excluding olanzapine) in patients receiving HEC.
Methods
A decision tree model (Fig. 1) was constructed to evaluate the cost and health outcomes associated with olanzapine-containing antiemetic regimens and otherwise-identical regimens, in TreeAge Pro Healthcare Version 2020 R1.1 by TreeAge Software Inc.
Probability values
The probability of complete response (CR), defined as no emesis without use of rescue medication in the overall phase, was extracted from risk values as reported by Bahbah et al. [22]—one of the most recent high-quality systematic review and meta-analysis published to-date in 2020. They reported risk ratios (RR) comparing olanzapine with non-olanzapine-containing regimens, in the prophylaxis setting. The majority of included studies reported on HEC patients; the risk values per group were extracted for the model. Additionally, they meta-analyzed only trials with 10 mg olanzapine regimens, the standard of care as recommended by guidelines.
Utility/index values
The quality of life for chemotherapy patients experiencing complete response or no/impartial response was extracted from Wang et al. [23] as the mean quality of life score for patients experiencing and not experiencing complete response, respectively. They evaluated quality of life using a rating scale—the functional living index-emesis questionnaire, an 18-item questionnaire with 7 points per item [24]. Patients who experienced complete response had an average FLIE of 115.2, and those who did not experience a complete response had an average FLIE of 102.6. A higher FLIE score denoted better quality of life. FLIE scores were linearly converted to a 0-1 utility/index scale, where a score of 1 denotes the highest possible FLIE score.
Cost values
The only difference in costs between olanzapine-containing and non-olanzapine-containing regimens is the cost of olanzapine, a 10-mg oral tablet administered from days 1 to 4 post-chemotherapy. The maximum cost of 1 tablet in the USA was extracted from Drugs.com, and multiplied 4 times to determine the total cost of olanzapine [25]. The cost of uncontrolled CINV is reported by Shih et al. as $1383 [26], the medical costs associated with 1 month of chemotherapy and accompanying uncontrolled CINV.
Base case analysis
The primary outcomes were the expected costs and expected utilities per regimen, to determine the incremental cost-effectiveness ratio (ICER), of olanzapine-containing compared with non-olanzapine-containing regimens in the event of lack of dominance (one regimen being both cheaper and more effective than the other).
Sensitivity analyses
One-way sensitivity analyses were conducted to individually investigate the effect of (i) lower CR rates of olanzapine, closer to non-olanzapine-containing regimens; (ii) higher index (FLIE scores) for patients who achieved no/incomplete response, closer to FLIE scores of patients achieving a complete response, to account for a smaller index gained from complete response; (iii) differing costs of olanzapine to reflect different costs per hospitals, globally, due to different insurance systems and drug costs in an attempt to extrapolate beyond the USA; and (iv) varying costs for uncontrolled CINV, to account for varying durations of chemotherapy and accompanying uncontrolled CINV.
Results
Base case analysis
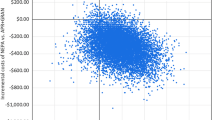
Olanzapine-containing regimens dominated non-olanzapine-containing regimens; no ICER values were calculated. Olanzapine regimens have an expected cost of only $325.24, compared with $551.23 to non-olanzapine-containing regimens. Meanwhile, olanzapine regimens have an expected index of 0.89, relative to 0.87 for non-olanzapine regimens (Fig. 2).
Sensitivity analyses
Olanzapine-containing regimens dominate non-olanzapine-containing regimens even if CR of olanzapine-containing regimens falls to 0.63. Only when CR is between 0.60 and 0.62 is olanzapine both more effective and more costly. Olanzapine-containing regimens are dominating, when CR is equal to those of non-olanzapine-containing regimens (Table 1). Olanzapine regimens dominate for all simulations where index for no/impartial response is higher and approaches the index of complete response (Table 2). Olanzapine regimens dominate in all scenarios, where drug costs vary between $0 and $60 (Table 3). When the cost of uncontrolled CINV is either increased or decreased, olanzapine regimens still dominate (Table 4).
Discussion
This is the first CEA analysis of olanzapine, using US cost data. US spending on health care is higher than in any other country, with the clinical and economic burden of CINV specifically, shown to be approximately $1854.70/day between 2007 and 2009 [21]. In this study, olanzapine-containing regimens dominate non-olanzapine-containing regimens—they are demonstrated to be both cheaper and more effective. Given the proven efficacy of olanzapine and recent recommendation/option in international guidelines to employ olanzapine as part of a four-drug regimen for patients receiving HEC, the results of this study provide further support for the clinical guidelines in recommending olanzapine for prophylaxis of CINV.
The probability values for our model are sourced from Bahbah et al. [22]. There are other more-recent systematic review and meta-analysis, but they were not appropriate for this study. Zhou et al. [27], published in 2020, appropriately reported RR comparing olanzapine to non-olanzapine regimens, but pooled the efficacy data of both prophylaxis and rescue regimens. Other reviews, by Yang et al. [28] and Chelkeba et al. [29], were not as recent and undertook less-than-ideal methodology—not reporting complete response endpoint, pooling olanzapine studies of both 5 and 10 mg, and pooling prophylaxis and breakthrough regimens, respectively.
Our conclusions mirror a CEA analysis done in Southeast Asia by Chanthawong et al., who reported olanzapine as cost-effective [19]. Chanthawong et al. concluded olanzapine-containing regimens to be cost-effective based on the CEA’s ICER falling below an assumed cost-effectiveness threshold. The results reported in our study reports olanzapine-containing regimens to be both cheaper and more effective. While Chanthawong et al.’s conclusion may change based on the magnitude of the cost-effectiveness threshold, our results find olanzapine-containing regimens to be more cost-effective than non-olanzapine-containing regimens, regardless of willingness to pay.
Sensitivity analyses do note that olanzapine-containing regimens no longer dominate non-olanzapine-containing regimens only when CR of olanzapine-containing regimens falls below 0.62. Such a large downward revision of CR from 0.78 to 0.63 is unlikely, given the fact that olanzapine has already been extensively studied with over 1000 patients in randomized controlled trials [22]. It is therefore unlikely that olanzapine-containing regimens will not dominate non-olanzapine-containing regimens when accounting for uncertainty in the base case analysis.
This CEA is not without limitations. CR, FLIE scores, and costs may differ based on clinical practice and healthcare pay structure. Sensitivity analyses were performed to account for uncertainty, and the results remain unchanged. In fact, one-way sensitivity analyses of cost data may even allow for extrapolation of these results to countries with different healthcare costs. Additionally, the employed model did not factor in explicit consideration of adverse events known to be associated with olanzapine, such as sedation [30]. However, one-way sensitivity analyses of FLIE scores and uncontrolled CINV costs decreased the differences in index and cost between olanzapine-containing and non-olanzapine-containing regimens, thereby simulating a smaller gain in quality of life and greater cost associated with sedation for olanzapine regimens. Olanzapine still dominates in these sensitivity analyses; olanzapine is still cheaper and more effective. Therefore, although there is uncertainty around the base case analysis, the results are nevertheless robust. Finally, this analysis is conducted from a hospital rather than larger societal perspective; it does not account for out-of-pocket costs and the burden of costs incurred by public and private payers and patients and caregivers.
In conclusion, olanzapine-containing regimens are both cheaper and more effective in the prophylaxis of CINV in HEC patients than non-olanzapine-containing regimens. Future CINV trial resources should be allocated to understand newer antiemetics and compare them to olanzapine-containing regimens as the control arm.
Data availability
N/A
References
Cohen L, de Moor CA, Eisenberg P et al (2007) Chemotherapy-induced nausea and vomiting: incidence and impact on patient quality of life at community oncology settings. Support Care Cancer 15:491–503
Osoba D, Zee B, Warr D et al (1997) Effect of postchemotherapy nausea and vomiting on health-related quality of life. Support Care Cancer 5:307–313
Gralla RJ, de Wit R, Herrstedt J et al (2005) Antiemetic efficacy of the neurokinin-1 antagonist, aprepitant, plus a 5-HT3 antagonist and a corticosteroid in patients receiving anthracyclines or cyclophosphamide in addition to high-dose cisplatin: analysis of combined data from two phase III randomized clinical trials. Cancer 104:864–868
Chow R, Chiu L, Navari R et al (2016) Efficacy and safety of olanzapine for the prophylaxis of chemotherapy-induced nausea and vomiting (CINV) as reported in phase I and phase II studies: a systematic review. Support Care Cancer 24:1001–1008
Chow R, Valdez C, Chow N et al (2020) Oral cannabinoid for the prophylaxis of chemotherapy-induced nausea and vomiting – a systematic review and meta-analysis. Support Care Cancer 28:2095–2103
Gyawali B, Poudyal B, Iddawela M (2016) Cheaper options in the prevention of chemotherapy-induced nausea and vomiting. J Glob Oncol 3:145–153
Chow R, Warr DG, Navari RM et al (2016) Should palonosetron be a preferred 5-HT3 receptor antagonist for chemotherapy-induced nausea and vomiting? An updated systematic review and meta-analysis. Support Care Cancer 26:2519–2549
Di Maio M, Baratelli C, Bironzo P et al (2018) Efficacy of neurokinin-1 receptor antagonists in the prevention of chemotherapy-induced nausea and vomiting in patients receiving carboplatin-based chemotherapy: a systematic review and meta-analysis. Crit Rev Oncol Hematol 124:21–28
Chow R, Warr DG, Navari RM et al (2018) Efficacy and safety of 1-day versus 3-day dexamethasone for the prophylaxis of chemotherapy-induced nausea and vomiting: a systematic review and meta-analysis of randomized controlled trials. J Hosp Manag Health Policy 2:25
Basch E, Prestrud AA, Hesketh PJ et al (2011) Antiemetic American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol 29:4189–4198
Roila F, Molassiotis A, Herrstedt J et al (2016) 2016 MASCC and ESMO guidelines update for the prevention of chemotherapy- and radiotherapy-induced nausea and vomiting and of nausea and vomiting in advanced cancer patients. Ann Oncol 27(suppl 5):v119–v133
Hocking CM, Kichenadasse G (2014) Olanzapine for chemotherapy-induced nausea and vomiting: a systematic review. Support Care Cancer 22:1143–1151
Srivasta M, Brito-Dellan N, Davis MP et al (2003) Olanzapine as an antiemetic in refractory nausea and vomiting in advanced cancer. J Pain Symptom Manag 25:578–582
Navari RM, Nagy CK, Gray SE (2013) The use of olanzapine versus metoclopramide for the treatment of breakthrough chemotherapy-induced nausea and vomiting in patients receiving highly emetogenic chemotherapy. Support Care Cancer 21:1655–1663
Navari RM, Gray SE, Kerr AC (2011) Olanzapine versus aprepitant for the prevention of chemotherapy-induced nausea and vomiting: a randomized phase III trial. J Support Oncol 9:188–195
Chiu L, Chow R, Popovic M et al (2016) Efficacy of olanzapine for the prophylaxis and rescue of chemotherapy-induced nausea and vomiting (CINV): a systematic review and meta-analysis. Support Care Cancer 24:2381–2392
Hesketh PJ, Kris MG, Basch E et al (2017) Antiemetics: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol 28:3240–3261
Herrstedt J (2018) The latest consensus on antiemetics. Curr Opin Oncol 30:233–239
Chanthawong S, Lim YH, Subongkot S et al (2019) Cost-effectiveness analysis of olanzapine-containing antiemetic therapy for managing highly emetogenic chemotherapy in Southeast Asia: a multinational study. Support Care Cancer 27:1109–1119
Shrank W, Rogstad T, Parekh N (2019) Waste in the US health care system. JAMA 322:1501
Craver C, Gayle J, Balu S et al (2011) Clinical and economic burden of chemotherapy-induced nausea and vomiting among patients with cancer in a hospital outpatient setting in the United States. J Med Econ 14:87–98
Bahbah EI, Abdalla AR, Abdelshafy K et al (2019) Should olanzapine be advocated over conventional anti-emetics for the prevention of chemotherapy-induced nausea and vomiting? An updated meta-analysis of randomized control trials. Curr Enzym Inhib 15:80–90
Wang W, Lou G, Zhang Y (2018) Olanzapine with ondansetron and dexamethasone for the prevention of cisplatin-based chemotherapy-induced nausea and vomiting in lung cancer. Medicine 97:37
Martin AR, Pearson JD, Cai B et al (2003) Assessing the impact of chemotherapy-induced nausea and vomiting on patients’ daily lives: a modified version of the Functional Living Index – Emesis (FLIE) with 5-day recall. Support Care Cancer 11:522–527
Olanzapine prices, coupons and patient assistance programs [Internet]. 2020 Mar 2 [cited 2020 Mar 5]. Available from: https://www.drugs.com/price-guide/olanzapine
Shih Y, Xu Y, Elting L (2007) Costs of uncontrolled chemotherapy-induced nausea and vomiting among working-age cancer patients receiving highly or moderately emetogenic chemotherapy. Cancer 110:678–685
Zhou JG, Huang L, Jin SH et al (2020) Olanzapine combined with 5-hydroxytryptamine type 3 receptor antagonist (5-HT3 RA) plus dexamethasone for prevention and treatment of chemotherapy-induced nausea and vomiting in high and moderate emetogenic chemotherapy: a systematic review and meta-analysis of randomised controlled trials. ESMO Open e000621:5
Yang T, Liu Q, Lu M et al (2017) Efficacy of olanzapine for the prophylaxis of chemotherapy-induced nausea and vomiting: a meta-analysis. Br J Clin Pharmacol 83:1369–1379
Chelkeba L, Gidey K, Mamo et al (2017) Olanzapine for chemotherapy-induced nausea and vomiting: systematic review and meta-analysis. Pharm Pract (Grenada) 15:877
Navari RM, Qin R, Ruddy KJ et al (2016) Olanzapine for the prevention of chemotherapy-induced nausea and vomiting. N Engl J Med 375:134–142
Author information
Authors and Affiliations
Contributions
All authors contributed substantially to conception and design, or acquisition of data, or analysis and interpretation of data. All authors contributed in drafting the article or revising it critically for important intellectual content. All authors approve the version to be published.
Corresponding author
Ethics declarations
Conflict of interest
Mr. Chow has nothing to disclose. Mr. Chiu has nothing to disclose. Dr. Herrstedt reports personal fees from SOBI, personal fees from GSK, outside the submitted work. Dr. Aapro reports personal fees and non-financial support from Multinational Association for Supportive Care in Cancer, personal fees and non-financial support from European Society of Medical Oncology, personal fees and non-financial support from European Cancer Organisation, grants and personal fees from Helsinn, personal fees from Tesaro, grants and personal fees from Sandoz, personal fees from Merck USA, personal fees from Vifor, personal fees from Pfizer, personal fees from Taiho, and personal fees from Kyowa Kirin, outside the submitted work. Dr. Lock reports consulting fees from Ferring, Abbvie, Sanofi, and AstraZeneca in the past 10 years outside the submitted work. Dr. DeAngelis has nothing to disclose. Dr. Navari has nothing to disclose.
Ethics approval
N/A
Consent to participate
N/A
Consent to publication
N/A
Code availability
N/A
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chow, R., Chiu, L., Herrstedt, J. et al. Cost-effectiveness analysis of olanzapine-containing antiemetic therapy for the prophylaxis of chemotherapy-induced nausea and vomiting (CINV) in highly emetogenic chemotherapy (HEC) patients. Support Care Cancer 29, 4269–4275 (2021). https://doi.org/10.1007/s00520-020-05977-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-020-05977-x