Abstract
Purpose
Breast cancer is the most common non-cutaneous cancer in women with an estimated 268,600 new cases diagnosed in 2019, joining the over 3 million women living with the disease. To reduce cancer recurrence, postmenopausal women (highest incidence and prevalence of breast cancer) who test positive for hormone receptors in their tumors are candidates for adjuvant endocrine therapy (i.e., aromatase inhibitors [AIs]). Despite the benefits of AIs in the treatment for breast cancer, many women remain at risk for complications, including osteoporosis and fractures, all of which can adversely affect health-related quality of life (HRQoL). Increased attention is being paid to the role physical activity (PA) may have in improving health outcomes in survivors of breast cancer, but few studies focus on postmenopausal women. We sought to examine (1) the percentage of women in our sample meeting (or not meeting) the American College of Sports Medicine (ACSM) PA recommendations, (2) the relationship between AI use and three types of PA (leisure time, strength training, and walking), and (3) the relationship between PA and HRQoL by AI use, controlling for covariates.
Methods
Postmenopausal women with breast cancer (n = 170), ages 50–95 years (M = 68.7), diagnosed with stage 1–3 disease, 45% on AIs, were recruited. Demographic, HRQoL, and PA data were collected via patient self-report, while clinical data (AI use) were abstracted from patient medical records. To address study aims, we utilized descriptive statistics, chi-square analyses, and multiple linear regressions, respectively.
Results
Half of the sample met the ACSM recommendations for total leisure-time PA (vigorous and moderate intensity combined), and 65.3% (n = 111) weekly walking. With regard to strength training, 36.5% of the women met these ACSM recommendations. Generally, there were positive relationships between AI use and most HRQoL domains. There were no statistically significant relationships between PA (meeting recommendations or not) and HRQoL by AI use.
Conclusion
The proportion of women meeting guidelines for walking activity was encouraging. It is imperative that healthcare professionals providing care to breast cancer survivors follow up regarding symptoms, side effects, and physical activity in tandem to fully understand their relationship on an individual level.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer remains the most common non-cutaneous cancer in women with an estimated 268,600 new cases diagnosed in the USA during 2019 [1]. Advances in early detection and treatment for breast cancer have resulted in an overall 5- and 10-year survival rate of 93% and 80%, respectively [2]. Postmenopausal women over age 50 have the highest incidence (23.8%) of breast cancer [3] compared with younger women (6.6%) [4, 5]. Breast cancer outcomes, including morbidity, treatment success, and health-related quality of life (HRQoL), are worse among postmenopausal women compared with those among premenopausal women [6, 7].
Treatment(s) vary based on the type of breast cancer, staging, and the overall health of the individual [6]. Typically, treatment options include some combination of surgery, radiation, and chemotherapy, all of which have short- and long-term side effects including hair loss, loss of appetite, nausea/vomiting, fatigue, and immune deficiency [2]. A recent form of therapy, aromatase inhibitors (AI), is included in treatment regimens for those whose tumor tissue immunochemistry identifies the presence of estrogen receptors (ER) or progesterone receptors (PR). Studies have found treatments for breast cancer, including AIs, place women at increased risk for bone health issues [8,9,10,11], in addition to the aforementioned side effects, all of which can adversely affect HRQoL.
In recent years, increased attention is being paid to the role lifestyle modifications (i.e., physical activity) may have in improving health outcomes, including HRQoL, in survivors of breast cancer [12, 13]. According to the American College of Sports Medicine (ACSM) [14], breast cancer survivors may benefit from a variety of exercise approaches to attenuate side effects of treatment and improve HRQoL [15]. Historically, oncologists have not recommended exercise for breast cancer patients, but research now suggests an active lifestyle is safe for many women and should be recommended by healthcare providers, both during and after treatment [14]. A study found the most influential factor in physical activity uptake in cancer survivors is physician recommendation [16]. Exercise has been found to be an effective intervention to improve overall HRQoL [17,18,19,20], increase energy and mobility, and improve bone health [21,22,23]. Previous literature has found that women who have taken AI therapies and concurrently engage in strength training and aerobic exercises have a lower risk for bone fracture than controls [24]. Likewise, other researches have suggested a combination of calcium-enriched diets and resistance and weight-bearing physical activity to protect against bone loss [25]. Yet, no research exists, that we are aware of, examining the prevalence of different types of physical activity in postmenopausal women with breast cancer taking AIs.
The aims of the current study are to examine the associations among three types of physical activity (i.e., strength training, [moderate and vigorous intensity] leisure-time physical activity (PA), and walking) and HRQoL among postmenopausal women with breast cancer by use of AI therapy. The current study’s research questions are, in our sample of postmenopausal breast cancer survivors, (1) What percentage of the sample is meeting the ACSM recommendations within each PA type?, (2) What is the relationship between AI use (taking AIs, not taking AIs) and meeting the ACSM-recommended PA?, and (3) What is the relationship between meeting the PA ACSM recommendations [14], AI use, and HRQoL, when controlling for covariates?
Methods
Study overview
Study participants were postmenopausal breast cancer survivors recruited from University of Connecticut Health (UConn Health; the branch of the university that oversees clinical care and academic education in medicine) in Farmington, CT, from February 2016 to May 2016. Study personnel abstracted clinical data via patient medical records, and HRQoL and physical activity data were collected via mail-based surveys. All potential participants received a packet in the mail which included an invitation letter from their treating oncologist, an information sheet detailing the study, a consent form, a Health Insurance Portability and Accountability Act (HIPAA) authorization form, and a paper copy of the survey. The study was performed with the approval of the Institutional Review Boards of UConn Health and the University of Connecticut (UConn) Storrs (the main campus of the public research university located in Storrs, CT).
Women were identified and prescreened by study personnel through hospital registries at UConn Health. A query was created from the hospital medical record database to locate names and addresses of patients who fit the following criteria: diagnosed with stage 0–3a breast cancer, postmenopausal, and completed treatment for their cancer. Women who could not read or speak English were excluded. Of the 606 participant packets mailed, 170 (28%) were returned and 22 (3.6%) were undeliverable. Sixty-eight percent (n = 121) returned both the survey and HIPAA waiver, while 53 women completed only the mailed survey, with two participants not completing the survey. Medical information was only extracted for those who completed the HIPAA authorization waiver. Hence, AI usage data were abstracted from 121 patients reducing our analytic sample for research questions 2 and 3.
Measures
Demographic and medical information
Participant self-reported demographic information including age, marital status, education, employment status, race/ethnicity, household income, and menopausal status were collected via mail-based survey (n = 170). Medical data were abstracted from those participants who completed the HIPAA waiver for this study (n = 121). Medical information abstracted included date of diagnosis, stage of disease, type of treatment(s), number of comorbid conditions, and whether a patient had taken AI therapy. Bone density scores, number of fractures, bone health medication (if any), supplements, medication history, and clinical bone health information (urine N-telopeptide cross-links (NTX), bone-specific alkaline phosphatase (BSAP), 25-OH vitamin D level, serum calcium/albumin, and urine calcium/creatinine) were also abstracted but not included in the current analyses.
Health-related quality of life
HRQoL was measured using the Functional Assessment of Cancer Therapy – Breast (FACT-B), a 44-item self-report instrument designed to measure multidimensional HRQoL in patients with breast cancer. Domains assessed included physical (PWB), social/family (SWB), emotional (EWB), and functional well-being (FWB), in addition to composite scores for physicality, emotionality, and overall HRQoL. The breast cancer subscale (BCS) of the FACT-B was also included measuring the perceptions of breast cancer, side effects, and femininity. The FACT-G score (PWB+SWB+EWB+FWB) reflects a generalized HRQoL dimension that does not consider breast cancer, while the FACT-B (or TOTAL) score (PWB+SWB+EWB+FWB+BCS) indicates HRQoL regarding the breast cancer experience. Lastly, the total outcome index (TOI) score (PWB+FWB+BCS) focuses primarily on physical functioning in relation to the breast cancer experience [26]. Internal reliability coefficients for the subscales in our sample were moderate to strong (FACT-G (α = 0.88), FACT-B (α = 0.73), TOI (α = 0.82), PWB (α = 0.81), SWB (α = 0.74), EWB (α = 0.71), and FWB (α = 0.83)) [27].
Physical activity
Self-reported physical activity was measured using components of the Physical Activity Questionnaire (PAQ), as done within the National Health and Nutrition Examination Survey (NHANES) [28]. Types of physical activity assessed were moderate-intensity leisure time (e.g., carrying light loads, bicycling at a regular pace, excluding walking), vigorous-intensity leisure time (e.g., running, calisthenics, and fast bicycling), strength training, and walking. Questions for moderate- and vigorous-intensity leisure-time physical activity and walking were the following: during the last 7 days, how many days per week did you perform that physical activity?; and on those days you performed that physical activity, how many minutes or hours per day did you spend performing that physical activity? According to the ACSM guidelines for PA [14], adults should engage in at least 150 to 300 min of moderate-to-vigorous intensity per week or 75 to 150 min of vigorous intensity per week or some combination of the two [14]. Questions for strength training were as follows: during the past month, how many days per week did you perform strength training?; and on those days you performed strength training, how many minutes or hours per day did you spend strength training? Strength training recommendations of involving all major muscle groups should occur on two or more days per week involving 2–3 sets of 10–12 repetitions of weights of choice [14]. Walking was defined as encompassing all intensities of PA (e.g., amount of time you walked to place-to-place) and could be part of an exercise sessions’ warm-up and cool-down or comprise a given exercise session in total [14], determined by minutes per week of the above activities. According to the ACSM [14], adults should engage in at least 150 to 300 min of moderate-to-vigorous intensity PA per week or 75 to 150 min of vigorous intensity per week or some combination of the two.
Previous research has assessed ACSM recommendations either as a binary variable (met recommendations or did not meet recommendations) or as a continuous variable (PA minutes per week). Pinto, Dunsiger, and Waldemore [29] implemented both methods, finding that, among breast cancer patients, exercising at least 150 min/week (or binarily identified as meeting recommendations) of leisure-time physical activity was associated with improved physical functioning and quality of life. Multiple binary variables were created to classify participants as meeting or not meeting ACSM recommendations for each type of PA. For each PA minutes per week variable, a binary ACSM recommendation (met or did not meet) variable was created. Using the recommended minutes per week of each type of PA [14], leisure-time moderate, leisure-time vigorous, total leisure time (vigorous + moderate combined), strength training, and walking, each participant was determined to have either met or did not meet recommendations for moderate-intensity leisure time, vigorous-intensity leisure time, moderate and vigorous intensity combined leisure-time physical activity, strength training, and walking. Specifically, leisure-time PA was comprised of moderate- and vigorous-intensity PA, with the possibility of each participant being able to identify with moderate and/or vigorous in the self-report survey.
Statistical analysis
All study variables were inspected using descriptive statistics and graphical techniques to assess distributional assumptions and identify outliers. Demographic and medical/clinical variables were examined using one-way analyses of variance (ANOVA), independent samples t tests, or correlation methods to determine which variables were significantly individually associated (p < .05) with HRQoL outcomes. Variables that were individually significant in relation to HRQoL outcomes in the current analyses and/or previous literature were used as covariates across all analyses: patient age, education, time since last treatment, and number of comorbid conditions.
To address the first research question, descriptive statistics were used to determine the percentage of the current sample meeting (or not meeting) the ACSM recommendations within each PA type. The binary ACSM recommendation (met or did not meet) variable was used to categorize the sample based on minutes per week of each PA type.
To examine the second research question, we analyzed a subset of the current sample regarding (n = 121) postmenopausal women for whom we have clinical information (i.e., AI status) available. A chi-square test of independence was conducted to examine the relation between those who had taken AI therapies and those who had not, and meeting ACSM-recommended [14] PA (moderate-intensity leisure time, vigorous-intensity leisure time, and total leisure time (moderate + vigorous combined), strength training, and walking).
To examine the third research question, multiple (single response) regression models were conducted, where one regression model was constructed per type of HRQoL domain, focusing on the use of AI therapy (no, yes), meeting recommendations for types of PA (no, yes), their interaction, and including the variables of patient age, education, time since last treatment, and number of comorbid conditions as covariates. Multiple comparison adjustments were conducted using a Bonferroni correction across HRQoL domains to ensure a conservative approach.
Results
Sample characteristics
A total of 170 postmenopausal breast cancer survivors aged 50 to 95 years (M = 68.7 years, SD = 10.3) participated. The sample was mostly Caucasian (94.3%) and married or living as married (66.0%), and all participants had completed breast cancer treatment at least 6 months prior to participation in the study (Table 1). Of the 121 participants that provided authorization for access to medical records, 53 had stage I disease, 36 had stage II disease, six had stage III, and two had atypical ductal hyperplasia or lobular carcinoma in situ. The average time since diagnosis was 10.1 years (SD = 6.58) and 13 participants had experienced a recurrence (7.6%). Treatment(s) ranged from chemotherapy alone (1.7%), radiation alone (1.7%), mastectomy alone (1.7%), and lumpectomy alone (0.8%) to having combination therapies (including different combinations of the aforementioned) without AI therapy (39.7%). The most common treatment (or combination of treatments) for those on AI therapies was lumpectomy/radiation combination (6.5%) followed by chemotherapy/lumpectomy (4.1%) or chemotherapy/mastectomy combinations (4.1%; see Table 1). Data on the start of AI treatment was available for 71 participants (97.2%). The average length of time from AI treatment start to the date of medical record abstraction was 6.81 years (SD = 3.48).
Percentage of postmenopausal breast cancer survivors meeting ACSM physical activity recommendations
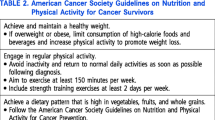
Half of the sample met the ACSM recommendations [14] for total leisure-time activity (vigorous and moderate combined; n = 85), 21.2% reported meeting moderate-intensity (n = 36), and 39.1% met vigorous-intensity leisure-time activity recommendations (n = 66). The majority (n = 111; 65.3%) met recommendations for weekly walking (see Table 1). With regard to strength training, approximately a third (36.5%) of the women in our sample met the ACSM guidelines for this type of PA activity. The physical activity profile of the current sample, including whether or not they met the ACSM recommendations [14], is depicted in Tables 1 and 2.
AI therapy and physical activity
Overall, and in both groups (AIs, no AIs), a high proportion of participants did not meet weekly ACSM-recommended PA in the three types examined (see Table 2). There were no significant differences between those on AI therapies (or not on AI therapies) between whether or not participants met ACSM recommendations [14] for moderate leisure-time (χ(1) = 1.01, p = .353), vigorous leisure-time (χ(1) = .210, p = .704), total leisure-time (moderate + vigorous combined) (χ(1) = .931, p = .358), strength training (χ(1) = .083, p = .845), and walking activities (χ(1) = .316, p = .700). Of note, one-third (32.9%) of women on AIs were meeting the ACSM recommendations for strength training compared with the 27.6% of the general population in 2018 [30].
Meeting PA recommendations and HRQoL by AI use
Multiple linear regressions were conducted to address the third research question, one per each HRQoL domain. Various effects were significant without multiple comparison adjustments, such as significant AI use predictors, but no interactions between AI use and meeting PA recommendations were significant. Specifically, AI use was found to be a significant predictor in strength training models, but only in TOTAL and TOI domains, as well as in moderate PA models, only in FWB, FACT-G, and TOTAL domains. These non-adjusted findings are depicted in Table 3. After adjusting for multiple comparisons, none of the results was significant.
Discussion
This study was one of the first studies to examine the prevalence of meeting the ACSM PA recommendations in postmenopausal women with breast cancer being treated with AI therapy, and the association between physical activity and HRQoL. In spite of the known benefits of PA in breast cancer survivors, the prevalence of meeting the guidelines was remarkably low, similar to previous findings [18]. Of significance, around one-third (32.9%) of women on AIs are meeting PA guidelines for strength training, a prevalence higher than the general population at 27.6% reported in 2018 [30]. Since AI use places women at risk for musculoskeletal issues, including osteopenia, osteoporosis, and fractures, it is promising to see this statistic higher than that of the general population, as these side effects can be attenuated by strength training [31]. Perhaps healthcare providers are more likely to encourage physical activity in this population of breast cancer survivors because of the known bone health risks of AI use.
While the proportion of women in this study meeting the ACSM recommendations for walking (66.7%) and total leisure time (54.2%) was encouraging, two-thirds of women in our study were not meeting the ACSM recommendations for strength training. Compared with the general population, these numbers were similar and raise concerns for the overall health of the US population [30]. Similarly, our findings are similar to other studies of PA in breast cancer survivors which found about a third of the women meet 30% of PA recommendations set by both ACSM [14] and, similarly, the CDC [32,33,34]. Despite consistency with the general population and studies of PA in breast cancer survivors, these findings are particularly troublesome for breast cancer survivors on AIs who are at significant risk for treatment-related effects, which can be attenuated by physical activity.
Although physical activity has the possibility of helping attenuate some treatment-related side effects in breast cancer survivors using AIs, side effects associated with AI use (e.g., joint and muscle pain, hot flashes, night sweats) may negatively impact survivors’ exercise routine. The current study utilized the FACT-G physical and functional well-being subscales which include both pain and sleep quality and found that both were significantly associated with reported vigorous PA minutes per week. While it is possible that physical side effects of AI treatment may negatively impact exercise routines and overall functionality in this population, it is important to note that these side effects occur in 15% of the population [8,9,10,11]. Oncologists and nurses are in the best position to provide PA resources and health promotion messages to survivors, yet a recent report suggests that this communication may be imperative for continued adherence to long-term treatment(s) in light of higher self-management of side effects [35].
Because treatment for breast cancer is increasingly customized according to specific tumor characteristics, fitness trainers who work with postmenopausal women with breast cancer on AIs could benefit from specific knowledge about the cancer diagnosis and treatment to make informed, safe choices about exercise prescription. AI use may adversely affect the musculoskeletal system, among other systems, possibly affecting domains relating to HRQoL. Emerging evidence suggests resistance exercise training can improve lean body mass (LBM) and decrease body mass index (BMI) and percent body fat (%FM) in breast cancer survivors taking AIs [31].
While healthcare providers should be promoting physical activity to their patients, breast cancer survivors can also play a role. Survivors need to be proactive and educated about the late health effects of cancer treatment and the role physical activity may plan in attenuating those effects. They should recognize that there is not a one size fits all approach and that PA should be approached based on specific doses of aerobic, combined aerobic plus strength training, and/or strength training [21]. Breast cancer patients, under the guidance of fitness experts, should explore different types of exercises and find what works for their individual goals and desires. Many breast cancer survivors engage in walking, as found in this study. Perhaps using this positive behavior as a self-motivating starting point to introduce other forms of PA might be more effective than focusing on what is absent.
Previous research has demonstrated a positive relationship between physical activity and HRQoL [29, 36]. Our results have mirrored this, although these relationships were not significant, most likely due to the small sample of women meeting PA recommendations. Our results indicated that AI use led to significantly better HRQoL outcomes for specific domains (without a multiple comparison adjustment) and that associations with other domains were positive, but not significant. Clinically, there exists a general cost-benefit relationship between AI use and specific HRQoL domains and should be discussed with patients prior to treatment. Although interactions between AI use and meeting PA recommendations were not significant, the trend in Table 3 suggests that the magnitude of improvement in these HRQoL domains due to meeting the indicated PA guidelines may be smaller for those taking AI therapies than for those who do not, holding all other variables constant. More research is needed, among larger groups of women within this demographic, to substantiate this finding.
While our findings provide important information for clinicians and those who provide follow-up care to breast cancer survivors on AIs, the results must be interpreted with caution. Despite not finding support between PA and HRQoL, a larger sample size would have increased the statistical power of the analyses and perhaps provided results to be in line with past research. The current sample uses non-random survey data and was recruited using targeted sampling. Related, clinical information (e.g., cancer staging, clinical samples, date of last treatment, date of diagnosis) was not abstracted for all 170 participants. A total of 53 participants did not sign the HIPAA waiver allowing researchers to access their medical records for pertinent information. Our analytic sample was limited due to lack of HIPAA approval for medical record abstraction among some of our participants. Additionally, we only abstracted the start date of AI therapy and not the end date (if applicable). Therefore, we were able to calculate the total time from AI start to medical record abstraction, but not assess if AI therapy had stopped prior to medical record abstraction. On average, our participants had been on AIs for 6.80 years, which is in line with current AI treatment guidelines [37]. Our main independent variable, AI use, was only collected via medical records, limiting our analytic sample to 121 regarding the second and third hypotheses. Lastly, the current study was cross-sectional and relied on physical activity self-report which often overestimates actual PA levels. It is quite possible these estimates are lower than reported.
Future directions
The current study provides potentially important information to inform future PA interventions among postmenopausal breast cancer survivors on AI therapies. Clinicians and those that care for breast cancer survivors can use this information to target health promotion physical activity messages and referrals to patients on AIs as this group is at significant risk for bone loss and ultimately poor HRQoL. Future research should replicate this study with a larger sample size and a randomized PA design. While self-report was used to gauge HRQoL in the current study, physical activity can be assessed in future studies using accelerometer devices to provide a more accurate measure instead of relying on participant recall and report.
Conclusions
The results of this study indicate that, overall, the prevalence of breast cancer survivors meeting the ACSM guidelines is low (with the exception of walking) across PA types, even those who are on AI therapies. While PA has been shown in previous research to help retain bone density, support musculoskeletal health [8,9,10,11], and increase HRQoL [29, 37, 38], survivors are not meeting current recommendations. Healthcare providers should continue to promote physical activity in this population, including educating their patients about the late health effects of AI use and the benefits of physical activity to help attenuate those risks. Integrating the risks of AI treatment as well as the benefits of physical activity into survivorship care plans may help play a role in improving the quality of cancer survivorship in postmenopausal women with breast cancer.
Data availability
The data and materials are available if requested.
References
National Cancer Institute (NCI) (2019) Cancer stat facts: Common cancer sites. National Cancer Institute (NCI), Bethesda https://seer.cancer.gov/statfacts/html/common.html
American Cancer Society (ACS) (2017) How common is breast cancer?. https://www.cancer.org/cancer/breast-cancer/about/how-common-is-breast-cancer.html
Centers for Disease Control and Prevention (CDC) (2016) What are the risk factors for breast cancer? https://www.cdc.gov/cancer/breast/basic_info/risk_factors.htm
Anders A, Johnson CK, Litton R, Phillips J, Bleyer M (2009) Breast cancer before age 40 years Semin. Oncol 36:237–249
Howlader CK, Noone N, Krapcho AM, Neyman M, Aminou N, Waldron R, Altekruse W, Kosary SF, Ruhl CL, Tatalovich J, Cho Z, Mariotto H, Eisner A, Lewis MP, Chen DR, Feuer HS, SEER Cancer Statistics Review, 1975-2009 (Vintage 2009 Populations) (2012). National Cancer Institute, Bethesda
DeSantis A, Fedewa CE, Sauer SA, Kramer AG, Smith JL, Jemal RA (2015) Breast cancer statistics, 2015: convergence of incidence rates between black and white women. CA Cancer J Clin 66:31–42
McPherson JM, Steel K, Dixon CM (2000) Breast cancer - epidemiology, risk factors, and genetics. Br Med J 321:624–628
Cella LJ, Fallowfield D (2008) Recognition and management of treatment-related side effects for breast cancer patients receiving adjuvant endocrine therapy. Breast Cancer Res Treat 107:167–180
Chen RT, Maricic Z, Aragaki M, Mouton AK, Arendell C, Lopez L, Chlebowski AM (2009) Fracture risk increases after diagnosis of breast cancer or other cancers in postmenopausal women: results from the Women’s Health Initiative. Osteoporos Int 20:527–536
Choski C, Williams P, Clark M, Van Poznak PM, (2013) Skeletal manifestations of treatment of breast cancer Curr Osteoporos Rep. 11:319–328.
Taxel P, Choski C, Van Poznak P (2012) The management of osteoporosis in breast cancer survivors. Maturitas 73:275–279
Bellizzi KM, Rowland DD, Jeffrey JH (2005) Current health behaviors of cancer survivors: examining opportunities for cancer control intervention. J Clin Oncol 23:8884–8893
Green EL, Steinnagel HJ, Morris G, Laasko G (2014) Health behavior models and patient preferences regarding nutrition and physical activity after breast or prostate cancer diagnosis. Eur J Cancer 23:640–652
American College of Sports Medicine (ACSM) (2018) ACSM’s guidelines for exercising testing and prescription, 10th edn. American College of Sports Medicine, Indianapolis
Brown JA, Ligibel JC (2019) Putting exercise into oncology practice: state-of-the- science, innovation, and future directions. Cancer J 25:316–319
Sallis MF, Hovell JF (1990) Determinants of exercise behavior Exerc. Sport Sci Rev 18:301–330
Files S, Ko JA, Pruthi MG (2010) Managing aromatase inhibitors in breast cancer survivors: not just for oncologists. Mayo Clin Proc 85:560–566
Irwin ML, McTiernan A, Bernstein L, Gilliland FD, Baumgartner R, Baumgartner K, Ballard-Barbash R (2004) Physical activity levels among breast cancer survivors. Med Sci Sports Exerc 36:1096–1108
McNeely KS, Campbell ML, Rowe KL, Klassen BH, Mackey TP, Courneya JR (2006) Effects of exercise on breast cancer patients and survivors: a systematic review and meta-analysis. Can Med Assoc J 175:34–41
Zeng WKW, Huang Y, Cheng M, Zhou ASK, So Y (2014) Meta-analysis of the effects of exercise intervention on quality of life in breast cancer survivors. Breast Cancer 21:262–274
Campbell C, Winters-Stone KL, Wiskemann KM, May J, Schwartz AM, Zucker KHKS, Matthews DS, Ligibel CE, Gerber JA, Morris LH, Patel GS, Hue AV, Perna TF, Schmitz FM (2019) Exercise guidelines for cancer survivors: consensus statement from international multidisciplinary roundtable. Med Sci Sports Exerc 51:2375–2390
Judge G, Kleppinger JO, Kenny A, Smith A, Biskup JA, Marcella B (2005) Home- based resistance training improves femoral bone mineral density in women on hormone therapy. Osteoporosis 16:1096–1108
Nyrop LF, Muss KA, Hackney H, Clevalend B, Callahan R (2014) Joint pain and physical activity among breast cancer survivors on aromatase inhibitor therapy. J Clin Oncol 32:15
Winters-Stone KM, Dobek A, Nail J, Bennett L, Leo JA, Naik MC, Schwartz A (2011) Strength training stops bone loss and builds muscle in postmenopausal breast cancer survivors: a randomized, controlled trial. Breast Cancer Res Treat 127:447
Hadji P (2015) Cancer treatment-induced bone loss in women with breast cancer. Bonekey Rep 4:1–43
Avis J, Crawford NE, Manuel S (2005) Quality of life among younger women with breast cancer. J Clin Oncol 23:3322–3330
Victorson D, Barocas D, Song J, Cella J (2008) Reliability across studies from the functional assessment of cancer therapy-general (FACT-G) and its subscales: a reliability generalization. Qual Life Res 17:1137–1146
National Center for Health Statistics (2016) National health and nutrition examination survey (NHANES) https://wwwn.cdc.gov/Nchs/Nhanes/continuousnhanes/default.aspx? BeginYear=2015
Pinto M, Dunsiger BM, Waldemore S (2013) Physical activity and psychosocial benefits among breast cancer patients. Psychooncology 22:2193–2199
HealthyPeople.gov (2020) Physical activity, https://www.healthypeople.gov/2020/data-search/Search-the-Data#topic-area=3504
Thomas E, Cartmel GA, Harrigan B, Fiellin M, Capozza M, Zhou S, Ercolano Y, Gross ML, Hershman CP, Ligibel D, Schmitz J, Li K, Sanft T, Irwin SY (2017) The effect of exercise on body composition and bone mineral density in breast cancer survivors taking aromatase inhibitors. Obesity 25:346–351
Centers for Disease Control and Prevention (CDC) (2008) US Department of Health and Human Services physical activity guidelines for Americans 2008, Washington, DC.
de Groef D, Geraerts A, Demeyer I, Van der Gucht H, Dams E, de Kinkelder L, van Althuis CN, Van Kampen S, Devoogdt M (2018) Physical activity levels after treatment for breast cancer: two-year follow-up. Breast 40:23–28
Yan AV, Wang AF, Ng Y (2018) Physical activity and annual medical outlay in U.S. colorectal, breast, and prostate cancer survivors. Prev Med Rep 9:118–123
Farias B, Ornelas AJ, Hohl IJ, Zeliadt SD, Hansen SB, Li RN, Thompson CI (2016) Exploring the role of physician communication about adjuvant endocrine therapy among breast cancer patients on active treatment: a qualitative analysis. Support Care Cancer 25:75–83
Bellizzi KM, Smith A, Schmidt S, Keegan TH, Zebrack B, Lynch CF, Deapen D, Shnorhavorian M, Tompkins BJ, Simon M, Adolescent and Young Adult Health Outcomes and Patient Experience (AYA HOPE) Study Collaborative Group (2012) Positive and negative psychosocial impact of being diagnosed with cancer as an adolescent or young adult. Cancer 118:5155–5162
Goss PE, Ingle JN, Pritchard KI, Robert NJ, Muss H, Gralow J, Gelmon K, Whelan T, Strasser-Weippl K, Rubin S, Sturtz K, Wolff AC, Winer E, Hudis C, Stopeck A, Beck JT, Kaur JS, Whelan K, Tu D, Parulekar WR (2016) Extending aromatase-inhibitor adjuvant therapy to 10 years. N Engl J Med 375:209–219
Courneya DC, Segal KS, Mackey RJ, Gelmon JR, McKenzie K (2007) Effects of the aerobic and resistance exercise in breast cancer patients receiving adjuvant chemotherapy: a multicenter randomized controlled trial. J Clin Oncol 25:4396–4404
Acknowledgments
The authors would like to acknowledge the funding organization of the University of Connecticut’s InCHIP as well as the participants of the current study.
Funding
The research of the current study was funded by an internal seed grant from the University of Connecticut’s Institute for Collaboration on Health, Intervention, and Policy (InCHIP).
Author information
Authors and Affiliations
Contributions
All authors listed have actively participated in composition, editing, and review of the current manuscript.
Corresponding author
Ethics declarations
The study was performed with the approval of the Institutional Review Boards of UConn Health and the University of Connecticut (UConn) Storrs (the main campus of the public research university located in Storrs, CT).
Conflict of interest
The authors declare that they have no conflict of interest.
Code availability
N/A.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dibble, K.E., Bellizzi, K.M., Taxel, P. et al. Physical activity and health-related quality of life among postmenopausal women with breast cancer treated with aromatase inhibitors. Support Care Cancer 29, 2385–2394 (2021). https://doi.org/10.1007/s00520-020-05741-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-020-05741-1