Abstract
Purpose
The purpose of this study was to conduct a systematic review to assess the effect of exercise on symptoms and quality of life in lung cancer patients.
Methods
We conducted a systematic review using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. PubMed, Medline, Embase, Scopus, Web of Science, and SciELO were searched for studies published from January 1998 to January 2019. The review included all randomized controlled trials that evaluated the effect of exercise on symptoms and quality of life of lung cancer patients. Two reviewers independently assessed the quality of all the included studies using the Physiotherapy Evidence Database scale.
Results
In total, ten studies (835 participants) met all inclusion criteria. Three studies investigated the effect of exercise after lung resection, whereas four studies investigated it as a pre-surgery intervention. Two studies investigated the effect of exercise in patients under systemic treatment only, and one study included patients on diverse treatment plans. Exercise protocols consisted of different combinations of strength, aerobic, and inspiratory muscle training. Two trials, including 101 participants, found significant difference in quality of life between groups, favoring the intervention group; and five trials, including 549 participants, found significant inter-group differences in isolated symptoms, also favoring the intervention group.
Conclusions
Exercise can lead to improvements of symptoms and of quality of life in lung cancer survivors. Providing resistance training combined with high-intensity interval aerobic exercise after lung resection seems to be particularly effective. Further studies are warranted to investigate exercise for patients with poor performance status.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Evidence supports that exercise is safe and may improve daily life and tolerance to treatment in oncological patients [1]. According to the current American College of Sports Medicine (ACSM) exercise guidelines for cancer survivors, there is strong evidence supporting that combining moderate-intensity aerobic and resistance exercise performed two to three times per week for at least 12 weeks results in improvements in fatigue and in quality of life (QOL) in this population [2]. Though this consensus is of a tremendous contribution to deliver evidence-based multidisciplinary care in oncology, diagnosis-specific recommendations could provide additional benefits to cancer patients [3], particularly when it comes to treatment tolerance [2] and end-of-life care [4].
Lung neoplasms are the leading cause of cancer-related deaths worldwide [4]. Non-small cell is the most common histological type, accounting for 80–90% of the cases [5, 6]. Approximately 40% of all cases of non-small cell lung cancer (NSCLC) are diagnosed with metastatic disease [7, 8] and early palliative care leads to significant improvements in QOL of these patients [9]. For those diagnosed at stages I and II, and at stage IIIA in selected cases, surgery can be done with curative intent (followed by adjuvant therapies if needed) [10], but resection for lung cancer is related to permanent and irreversible reductions in QOL, in contrast with other major visceral operations [11].
Physical training benefits lung cancer survivors who are eligible for surgical treatment [12] and provides additional comfort for those under exclusive palliative care [6], but ideal methods to implement it, considering the heterogeneity of those groups, are yet to be established. Thereby, here we conducted a systematic review of randomized controlled trials which investigated the effect of exercise interventions for lung cancer patients. We aimed to provide evidence-based exercise prescriptions that may safely result in improvements in their symptom burden and QOL.
Methods
Protocol and registration
The review was conducted and reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses [13] guidelines, and the protocol is registered on the PROSPERO database [14] (CRD42018079429).
Search strategy
A thorough search on PubMed Central, Medline, Embase, Scopus, Web of Science, and SciELO was started in July 2018, and alerts in each database were set to keep returns up to date until January 2019. We started with PubMed Central and took its search algorithm as a reference to the other databases. The search was set to consider title, abstract, and index terms. The search terms were as follows: (((((“Lung Neoplasms”[Mesh] OR Pulmonary Neoplasms OR Neoplasms, Lung OR Lung Neoplasm OR Neoplasm, Lung OR Neoplasms, Pulmonary OR Neoplasm, Pulmonary OR Pulmonary Neoplasm OR Lung Cancer OR Cancer, Lung OR Cancers, Lung OR Lung Cancers OR Pulmonary Cancer OR Cancer, Pulmonary OR Cancers, Pulmonary OR Pulmonary Cancers OR Cancer of the Lung OR Cancer of Lung)) AND (((((((“Exercise”[Mesh] OR Exercises OR Physical Activity OR Activities, Physical OR Activity, Physical OR Physical Activities OR Exercise, Physical OR Exercises, Physical OR Physical Exercise OR Physical Exercises OR Exercise, Aerobic OR Aerobic Exercise OR Aerobic Exercises OR Exercises, Aerobic OR Exercise Training OR Exercise Trainings OR Training, Exercise OR Trainings, Exercise)) OR (“Exercise Therapy”[Mesh] OR Therapy, Exercise OR Exercise Therapies OR Therapies, Exercise OR Rehabilitation Exercise OR Exercise, Rehabilitation OR Exercises, Rehabilitation OR Rehabilitation Exercises OR Remedial Exercise OR Exercise, Remedial OR Exercises, Remedial OR Remedial Exercises)) OR (“Resistance Training”[Mesh] Training, Resistance OR Strength Training OR Training, Strength)) OR “Walking”[Mesh]) OR (“Rehabilitation”[Mesh] OR Pulmonary rehabilitation OR Physical rehabilitation)))) AND (randomized controlled trial [pt] OR controlled clinical trial [pt] OR randomized [tiab] OR placebo [tiab] OR clinical trials as topic[mesh:noexp] OR randomly [tiab] OR trial [tiab] NOT (animals[mh] NOT humans[mh]))))).
Eligibility criteria
Types of studies
Only randomized controlled trials published in peer-reviewed journals, in English, from January 1998 to January 2019 were considered eligible.
Participants
The participants were defined as lung cancer patients. Studies which also included patients with other types of neoplasms were not considered eligible.
Intervention and comparison
The inclusion criteria regarding intervention and comparison were as follows: (1) the intervention group underwent an exercise protocol, regardless if further components such as counseling sessions and nutrition support were also provided, and (2) there had to be a control group, which could have been compared with the intervention arm by (a) having just regular care without exercising, (b) having a different exercise regimen, or (c) having the same exercise regimen on a different period.
Outcomes
The studies were required to report QOL and/or symptoms as outcome measure.
Study selection
Selection was done by (1) merging search results using reference and removing duplicate records of the same report; (2) assessing titles and abstracts to remove obviously irrelevant reports; (3) retrieving full text of the potentially relevant reports; (4) linking together multiple reports of the same study; (5) examining full-text reports for compliance of studies with eligibility criteria; (6) contacting the authors to obtain additional information if needed; and (7) making final decisions on study inclusion and proceeding to quality assessment. All papers identified by the search strategy were blindly assessed by three independent reviewers through Rayyan QCRI web application. After this process, an open-label discussion clarified occasional disagreements, and a randomized controlled trial could be included for quality assessment if at least two reviewers agreed that it was eligible.
Quality assessment
The quality assessment was based on the Physiotherapy Evidence Database (PEDro) scale [15]. It measures the quality of randomized controlled trials which investigated physical therapy interventions [16, 17] by assessing external validity (item 1), internal validity (items 2–9), and results (items 10–11). The items consist of (1) eligibility criteria were specified; (2) subjects were randomly allocated to groups; (3) allocation was concealed; (4) the groups were similar at baseline regarding the most important prognostic indicators; (5) there was blinding of all subjects; (6) there was blinding of all therapists who administered the therapy; (7) there was blinding of all assessors who measured at least one key outcome; (8) measures of at least one key outcome were obtained from more than 85% of the subjects initially allocated to groups; (9) all subjects for whom outcome measures were available received the treatment or control condition as allocated or, where this was not the case, data for at least one key outcome was analyzed by “intention to treat”; (10) the results of between-group statistical comparisons are reported for at least one key outcome; (11) the study provides both point measures and measures of variability for at least one key outcome. Item 1 is not considered on the summary score, despite being sufficient to exclude a study if not accomplished. Taking into account the inherent difficulty to maintain therapists and subjects blinded under exercise intervention, we considered that losing two points on items 5 and 6 could still maintain studies at high quality standards. Thus, since some of our highest-quality trials would probably reach up to 8 points, we considered scores equal or superior to 6 as carrying a low risk of bias and only those studies were included for full-text review.
Data extraction and analysis
The data were extracted from the included articles using a data extraction form. Population sizes with mean age were collected, and details of the interventions were recorded including the exercise types, intensities, duration and setting of each session, frequency, and the total length of the interventions. The outcomes were collected including the assessment tool, results on QOL and symptoms, dropout rates, and adverse events related to exercise. One investigator performed the data extraction, which was verified by a second investigator. In accordance with the Cochrane Handbook for Systematic Reviews of Interventions [18], due to the heterogeneity of the interventions in the studies included for full-text review (e.g., Tai Chi, cardiovascular training, combined or not with resistance training (RT)), we did not perform a meta-analysis.
Results
Study searching and selection
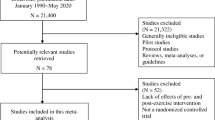
We identified 1998 studies based on the database searches. After removing duplicates and studies that did not fulfill the criteria, 17 studies were considered eligible for quality assessment (Fig. 1).
Quality assessment
Table 1 shows details of the results of the quality assessment. Ten studies, including 835 participants, were considered to have low risk of bias and included for full-text review [19,20,21,22,23,24,25,26,27,28]. Two studies were excluded for not satisfying criterion 1, either by not clearly reporting the source of subjects [29] or by not presenting a list of eligibility criteria [29, 30]. Five other studies were excluded for carrying high risk of bias [31,32,33,34,35]. When information was not clearly reported, criteria were considered as not fulfilled.
Description of the studies
The details of each exercise intervention in the perspective of the FITT principle (frequency/intensity/time/type), adopted by the current ACSM exercise guidelines for cancer survivors [2], are provided in Table 2. A sum of 835 participants living with lung cancer at different stages was randomized. Two studies recruited lung cancer patients with no restrictions on histologic diagnosis and/or molecular drivers [26, 27], and eight studies recruited NSCLC patients exclusively, including one study in which all patients had tumors presenting EGFR-activating mutations [28]. Five studies included patients staged as I–IV [19, 20, 26, 34, 36], two studies included patients at stages I–IIIa [23, 24], one study included patients at stages IIIa–IV [28], one study included patients at stages I–II [27], and one study did not report staging [25]. Sample size ranged from 24 [23, 28] to 235 [24] participants.
As performance status is a strong prognostic factor in lung cancer patients, we searched in each study the Eastern Cooperative Oncology Group (ECOG) Performance Status (PS) classification of included patients. ECOG-PS is a 5-point scale, where higher scores indicate greater disability [37]. One study included patients within the ECOG-PS 0–1 range [28], and two studies included patients within ECOG-PS 0–2 range [24, 26]. The remaining studies did not report on PS.
Three studies investigated the effect of exercise in the postoperative setting [24, 27, 36]. Four studies investigated the effect of exercise as a pre-surgery intervention [19, 20, 23, 25]. Two studies investigated the effect of exercise in patients under systemic treatment only, either targeted therapy [28] or chemotherapy [26]. One study included a pool of patients on diverse treatments or no treatment at all [21].
The terms “moderate” and “high,” here applied to characterize the intensity of exercise in the different protocols, are in accordance with the American Heart Association Scientific Statement [38]. Three interventions combined RT with high-intensity interval training (HIIT) and breathing exercises [24, 25, 36]. One intervention combined RT with moderate-intensity continuous aerobic training and stretching exercises [27]. Three interventions consisted of aerobic exercises only, either as a moderate-intensity interval protocol [28] or as moderate-intensity continuous aerobic training [21]. One intervention combined high-intensity continuous aerobic exercise with stretching exercises, inspiratory muscle training (IMT), and proprioceptive neuromuscular facilitation (PNF) exercises [23]. Two interventions combined respiratory exercises with aerobic training at intensities chosen by patients either to just stay comfortable [19] or to achieve up to level 6 at the Borg Dyspnea Score [20]. One intervention consisted of Tai Chi sessions [26]. No intervention consisted of resistance training only.
The duration of the training sessions varied from 30 min [19, 20] to 60 min [24, 26, 27, 36], and one study did not report on duration [23]. The frequency of the sessions ranged between twice per week [24] and daily exercises [19, 20]. Exercise sessions were partially supervised in two studies [26, 27], and not supervised in one study [21]. Exercise sessions were all supervised in the remaining studies. The lengths of the protocols were heterogeneous, varying between 1 week [19, 20] amd 20 weeks [36].
Outcomes
Two trials, including 101 participants, found significant difference in QOL favoring the intervention group after concluding their protocols, either in both the Physical and Mental Component Summaries of the Short Form (36) Health Survey (SF-36) [36], or in its Physical Component Summary only [25].
Other five trials, including 549 participants, found significant difference between intervention and control groups in isolated symptoms favoring the intervention group. Significant differences in anxiety and depression levels [23] and in depression levels only [21] were found through the Hospital Anxiety and Depression Scale (HDAS). Significant differences in fatigue levels were shown either through the European Organization for Research and Treatment of Cancer - Core Quality of Life Questionnaire, version 3.0 (EORTC QLQ-C30) [24] or through the Multidimensional Fatigue Symptom Inventory-Short Form (MFSI-SF) [26], and significant difference in bodily pain was found through the SF-36 [27].
Three studies [19, 20, 28] did not show any significant between-group difference concerning the outcomes of interest of this review.
Dropout rates ranged between 0 [23] and 55% [25] in the intervention groups and between 0 [19, 20, 23] and 50% [25] in the control groups. The study arms which had exercise (including all intervention groups, both early and late rehabilitation arms in Quist et al. [24], and the control group in Zhang et al. [26]) had an average dropout rate of 25.6%. The groups which received usual care had an average dropout rate of 8.8%.
Two adverse events related to exercise were reported: one case of hip fracture, occurred during a balance training [36], and one case of knee pain [19].
Discussion
This review aimed to identify effective exercise methods for improvements of symptoms and of QOL in lung cancer patients. Lung cancer survivors might have poor interest in physical rehabilitation for reasons including fear of extra burden and a perception of limited potential benefits [39], which may partially explain the limited number of high-quality trials we found and the high dropout rates of some studies. In this context, some of the successful programs here reviewed included the exercise program in an individualized and comprehensive plan of care, featuring counseling sessions and addressing issues as emotional support, pain management, nutrition, sexual activity, and smoking cessation.
Supervised and group-based exercise sessions, by counting with support by the personnel and promoting social interaction between participants, also seem to improve adherence. In Brocki et al. [27], considering subjects available for analysis, only 43% of the intervention group and 15% of the control group self-reported adherence to at-home resistance and aerobic training at least twice weekly. On the other hand, the intervention arm had an attendance of 97% to at least 8 out of the 10 supervised sessions, which consisted essentially of moderate-intensity continuous aerobic training and RT. These sessions were provided only once per week due to geographical issues. Four months after the surgery, the intervention group showed significantly less bodily pain than the control group (p = 0.01). The lack of inter-group difference in QOL was considered to be a consequence of the low frequency of training and the fact that some patients were enduring treatment-related side effects on the day of the sessions. In Edvardsen et al. [36], the sessions were postponed when patients receiving chemotherapy did not have conditions to exercise. In addition, the physical training was supervised three times per week at fitness centers close to each participant’s home and was group-based 1 h per week if possible. With such a great accessibility, a total of 55 sessions had an attendance of 88 ± 29% (participants were permitted to exceed the total hours proposed). Compared with the control group, the intervention group showed significantly less dyspnea (p = 0.03), and higher scores on both the Physical (p = 0.006) and Mental (p = 0.015) Component Summaries of SF-36. The protocol consisted essentially of RT and HIIT in the same sessions. RT has been shown to prevent surgery-associated muscular atrophy, thus enhancing recovery and function in operated patients [40]. For additional safety and optimized results, there was a focus on technique of execution during the first 4 weeks and a continuous management of exercise intensity based on the progress of individual participants. For its part, HIIT was the choice for cardiovascular exercise in this study. HIIT is effective in stimulating both metabolic and neuromuscular systems simultaneously [41], and has been shown to be superior to moderate-intensity continuous aerobic training in reducing systemic inflammation in patients with several clinical conditions [42]. We shall remark that the length of intervals between the high-intensity rounds of cardiovascular exercise was not reported in this trial, however. That information would have been valuable for a deeper interpretation of findings and for future research in this field. Furthermore, appropriately reporting it would facilitate the application of this method in community settings.
The protocol in Quist et al. [24] was also based on RT and HIIT, with progression of the exercise intensity. The sessions were all group-based and distributed twice per week, which, taking Edvardsen et al. [36] as a benchmark, makes this program more realistic for a number of health care teams. Both early and late rehabilitation groups had greater global health status at the week 26 compared with their pre-surgery conditions (p = 0.02 and p < 0.002 respectively). These findings are particularly important given that it takes 2 years for NSCLC patients who underwent lung resection to achieve their pre-surgery global health levels [11]. Furthermore, the benefits were observed to be persistent. The ERG (early rehabilitation group) started exercising as early as 14 days after operation and showed lower fatigue levels (p = 0.0017) at week 14 compared with those who were not exercising. Then, from week 14 to week 26, the LRG (late rehabilitation group) went through the same exercise protocol and had a significant greater improvement in fatigue levels than the ERG within that period (p < 0.0020). However, no inter-group difference could be found at this point, suggesting that the earlier benefits achieved by the ERG were sustained through the following 12 weeks.
Overall, the three above-referenced trials had a sum of 374 cases of lung cancer status post lung resection and, with a rate of adverse events related to exercise of 3.3:1000, they demonstrated that exercise can improve QOL and the symptom burden in this population. The observed late and durable effects shall also be explored by pre-surgery rehabilitation programs, as they may preemptively help on the initial recovery phase after lung resection, when NSCLC patients have the most consistent decline in QOL [43]. However, the time frame can be particularly challenging as surgeries may be scheduled shortly in advance. The 7-day interventions in Lai, Su et al. [20] and in Lai, Huang et al. [19] were found to decrease hospital stay and prevent postoperative pulmonary complications (PPCs), but QOL was not reassessed on the recovery phase in none of these studies. After training five times per week for 4 weeks prior to surgery, the participants in Morano et al. [23] had lower anxiety (p = 0.002) and depression (p = 0.02) levels 1 month after the operation. In Sebio García et al. [25], the pre-rehabilitation arm attended a median of 16 sessions including RT and HIIT, with progression of volume and intensity after the 10th session, and showed superior scores in the Physical Component Summary of the SF-36 3 months after the operation (p = 0.001) compared with the control group. However, due to the high dropout rates, data was per-protocol analyzed in this trial. In addition, we only considered the study arms to be comparable at the baseline assessment because the greater pulmonary function and lower body mass index (BMI) of the patients receiving usual care did not lead them to have a significant lower frequency of sub-lobar resection (p = 0.229). Although the authors affirmed that a univariate general linear model showed no interaction between the exercise capacity and the extent of the resection, one could consider that baseline unbalance as an extra source of bias added to the per-protocol analysis. Thus, more studies are warranted to assess the actual extent of the benefits of a few sessions of HIIT and RT prior to surgery in this population.
In patients not eligible for surgical treatment, RT holds potential to prevent functional dependence and QOL deterioration by counteracting the massive loss of skeletal muscle they may endure as the disease progresses [44, 45]. Nevertheless, a number of people living with advanced lung cancer will initially not be able to engage to conventional RT. Bedridden patients may benefit from sessions of sitting up at the bedside several times per day [46], which may gradually improve their mental and physical health, leveraging them into more robust training later on. Individual preferences shall also be taken into account in this process. Both study arms in Zhang et al. [26] were provided gentle metabolic and neuromuscular stimuli, but the likely pleasurable component of Tai Chi for Chinese patients may have contributed to the lower fatigue levels it induced compared with low-impact exercise (p < 0.05). This was the only study in which the interventions took place exclusively during chemotherapy cycles, when the associated side effects can mitigate compliance and outcomes. Under those circumstances, traditional programs may complement the management of intensity, volume, and frequency with eventual shifts to pleasurable and gentle modalities, adding up to a periodization method. Periodization can be defined as the systematic manipulation of training variables to elicit targeted adaptations at specific time points throughout the rehabilitation process [47]. It may optimize exercise response and prevent the onset of overtraining in a population already overwhelmed with fatigue [48]. Other transitory adjustments such as providing individual sessions with increased attention to equipment sanitization in cases of neutropenia, or just allowing a flexible schedule when minor acute symptoms arise, may also be considered for additional safety, compliance, and better outcomes. Importantly, for patients who underwent lung surgery or who present with a remarkable decline in their physical condition, extreme fatigue, or bone pain, providing evaluation or re-evaluation by the medical team is imperative for appropriate planning or modifications to the exercise program [2].
The main limitation of this review was the low availability of high-quality trials, which prevented us from drawing deeper conclusions. The lack of trials focused on patients with poor performance status was an additional flaw. It narrows our findings by excluding a large population of people living with lung cancer.
Conclusions
Despite the few high-quality studies available, results from this systematic review ratify that an exercise program can lead to improvements of symptoms and of QOL in lung cancer survivors. For patients who underwent lung resections, combining resistance training with high-intensity interval aerobic exercise at the same session at least twice per week seems to be particularly effective. Further studies are warranted to investigate training methods for patients with poor performance status.
References
Ferioli M, Zauli G, Martelli AM et al (2018) Impact of physical exercise in cancer survivors during and after antineoplastic treatments. Oncotarget 9:14005–14034. https://doi.org/10.18632/oncotarget.24456
Campbell KL, Winters-Stone KM, Wiskemann J et al (2019) Exercise guidelines for cancer survivors. Med Sci Sport Exerc 51:2375–2390. https://doi.org/10.1249/MSS.0000000000002116
Hayes SC, Newton RU, Spence RR, Galvão DA (2019) The Exercise and Sports Science Australia position statement: exercise medicine in cancer management. J Sci Med Sport 22:1175–1199. https://doi.org/10.1016/j.jsams.2019.05.003
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394–424. https://doi.org/10.3322/caac.21492
Lu T, Yang X, Huang Y, Zhao M, Li M, Ma K, Yin J, Zhan C, Wang Q (2019) Trends in the incidence, treatment, and survival of patients with lung cancer in the last four decades. Cancer Manag Res 11:943–953. https://doi.org/10.2147/CMAR.S187317
Planchard D, Popat S, Kerr K et al (2018) Metastatic non-small cell lung cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 29:iv192–iv237. https://doi.org/10.1093/annonc/mdy275
Morgensztern D, Ng SH, Gao F, Govindan R (2010) Trends in stage distribution for patients with non-small cell lung cancer: a National Cancer Database survey. J Thorac Oncol 5:29–33. https://doi.org/10.1097/JTO.0b013e3181c5920c
Herbst RS, Morgensztern D, Boshoff C (2018) The biology and management of non-small cell lung cancer. Nature 553:446–454. https://doi.org/10.1038/nature25183
Temel JS, Greer JA, Muzikansky A, Gallagher ER, Admane S, Jackson VA, Dahlin CM, Blinderman CD, Jacobsen J, Pirl WF, Billings JA, Lynch TJ (2010) Early palliative care for patients with metastatic non–small-cell lung cancer. N Engl J Med 363:733–742. https://doi.org/10.1056/NEJMoa1000678
Postmus PE, Kerr KM, Oudkerk M et al (2017) Early and locally advanced non-small-cell lung cancer (NSCLC): ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 28:iv1–iv21. https://doi.org/10.1093/annonc/mdx222
Schulte T, Schniewind B, Dohrmann P, Küchler T, Kurdow R (2009) The extent of lung parenchyma resection significantly impacts long-term quality of life in patients with non-small cell lung cancer. Chest 135:322–329. https://doi.org/10.1378/chest.08-1114
Rosero ID, Ramírez-Vélez R, Lucia A, Martínez-Velilla N, Santos-Lozano A, Valenzuela PL, Morilla I, Izquierdo M (2019) Systematic review and meta-analysis of randomized, controlled trials on preoperative physical exercise interventions in patients with non-small-cell lung cancer. Cancers (Basel) 11:944. https://doi.org/10.3390/cancers11070944
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. J Clin Epidemiol 62:1006–1012. https://doi.org/10.1016/j.jclinepi.2009.06.005
Booth A, Clarke M, Ghersi D, Moher D, Petticrew M, Stewart L (2011) An international registry of systematic-review protocols. Lancet 377:108–109. https://doi.org/10.1016/S0140-6736(10)60903-8
Blobaum P (2006) Physiotherapy Evidence Database (PEDro). J Med Libr Assoc 94:477–478
Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M (2003) Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther 83:713–721
De Morton NA (2009) The PEDro scale is a valid measure of the methodological quality of clinical trials : a demographic study. Aust J Physiother 55:129–133. https://doi.org/10.1016/s0004-9514(09)70043-1
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane handbook for systematic reviews of interventions version 6.0 (updated July 2019). Session 10-10-1. Cochrane, 2019. Available at www.training.cochrane.org/handbook/current.Available
Lai Y, Huang J, Yang M, Su J, Liu J, Che G (2017) Seven-day intensive preoperative rehabilitation for elderly patients with lung cancer: a randomized controlled trial. J Surg Res 209:30–36. https://doi.org/10.1016/j.jss.2016.09.033
Lai Y, Su J, Qiu P, Wang M, Zhou K, Tang Y, Che G (2017) Systematic short-term pulmonary rehabilitation before lung cancer lobectomy: a randomized trial. Interact Cardiovasc Thorac Surg 25:476–483. https://doi.org/10.1093/icvts/ivx141
Chen H-M, Tsai C-M, Wu Y-C, Lin KC, Lin CC (2015) Randomised controlled trial on the effectiveness of home-based walking exercise on anxiety, depression and cancer-related symptoms in patients with lung cancer. Br J Cancer 112:438–445. https://doi.org/10.1038/bjc.2014.612
Edvardsen E, Skjønsberg OH, Holme I et al (2014) High-intensity training following lung cancer surgery: a randomised controlled trial. Thorax 1–7. https://doi.org/10.1136/thoraxjnl-2014-205944
Morano MTAP, Mesquita R, Da Silva GPF et al (2014) Comparison of the effects of pulmonary rehabilitation with chest physical therapy on the levels of fibrinogen and albumin in patients with lung cancer awaiting lung resection: a randomized clinical trial. BMC Pulm Med 14:121. https://doi.org/10.1186/1471-2466-14-121
Quist M, Sommer MS, Vibe-Petersen J, Stærkind MB, Langer SW, Larsen KR, Trier K, Christensen M, Clementsen PF, Missel M, Henriksen C, Christensen KB, Lillelund C, Langberg H, Pedersen JH (2018) Early initiated postoperative rehabilitation reduces fatigue in patients with operable lung cancer: a randomized trial. Lung Cancer 126:125–132. https://doi.org/10.1016/j.lungcan.2018.10.025
Sebio García R, Yáñez-Brage MI, Giménez Moolhuyzen E, Salorio Riobo M, Lista Paz A, Borro Mate JM (2017) Preoperative exercise training prevents functional decline after lung resection surgery: a randomized, single-blind controlled trial. Clin Rehabil 31:1057–1067. https://doi.org/10.1177/0269215516684179
Zhang LL, Wang SZ, Chen HL, Yuan AZ (2016) Tai Chi exercise for cancer-related fatigue in patients with lung cancer undergoing chemotherapy: a randomized controlled trial. J Pain Symptom Manag 51:504–511. https://doi.org/10.1016/j.jpainsymman.2015.11.020
Brocki BC, Andreasen J, Nielsen LR, Nekrasas V, Gorst-Rasmussen A, Westerdahl E (2014) Short and long-term effects of supervised versus unsupervised exercise training on health-related quality of life and functional outcomes following lung cancer surgery – a randomized controlled trial. Lung Cancer 83:102–108. https://doi.org/10.1016/j.lungcan.2013.10.015
Hwang CL, Yu CJ, Shih JY, Yang PC, Wu YT (2012) Effects of exercise training on exercise capacity in patients with non-small cell lung cancer receiving targeted therapy. Support Care Cancer 20:3169–3177. https://doi.org/10.1007/s00520-012-1452-5
Jastrzębski D, Maksymiak M, Kostorz S et al (2015) Pulmonary rehabilitation in advanced lung cancer patients during chemotherapy. In: Advances in experimental medicine and biology. pp 57–64
Arbane G, Tropman D, Jackson D, Garrod R (2011) Evaluation of an early exercise intervention after thoracotomy for non-small cell lung cancer (NSCLC), effects on quality of life, muscle strength and exercise tolerance: randomised controlled trial. Lung Cancer 71:229–234. https://doi.org/10.1016/j.lungcan.2010.04.025
Stigt JA, Uil SM, van Riesen SJH, Simons FJNA, Denekamp M, Shahin GM, Groen HJM (2013) A randomized controlled trial of postthoracotomy pulmonary rehabilitation in patients with resectable lung cancer. J Thorac Oncol 8:214–221. https://doi.org/10.1097/JTO.0b013e318279d52a
Arbane G, Douiri A, Hart N, Hopkinson NS, Singh S, Speed C, Valladares B, Garrod R (2014) Effect of postoperative physical training on activity after curative surgery for non-small cell lung cancer: a multicentre randomised controlled trial. Physiother (United Kingdom) 100:100–107. https://doi.org/10.1016/j.physio.2013.12.002
Henke CC, Cabri J, Fricke L, Pankow W, Kandilakis G, Feyer PC, de Wit M (2014) Strength and endurance training in the treatment of lung cancer patients in stages IIIA/IIIB/IV. Support Care Cancer 22:95–101. https://doi.org/10.1007/s00520-013-1925-1
Chen H-M, Tsai C-M, Wu Y-C, Lin KC, Lin CC (2016) Effect of walking on circadian rhythms and sleep quality of patients with lung cancer: a randomised controlled trial. Br J Cancer 115:1304–1312. https://doi.org/10.1038/bjc.2016.356
Dhillon HM, Bell ML, van der Ploeg HP, Turner JD, Kabourakis M, Spencer L, Lewis C, Hui R, Blinman P, Clarke SJ, Boyer MJ, Vardy JL (2017) Impact of physical activity on fatigue and quality of life in people with advanced lung cancer: a randomized controlled trial. Ann Oncol 28:1889–1897. https://doi.org/10.1093/annonc/mdx205
Edvardsen E, Skjonsberg OH, Holme I, Nordsletten L, Borchsenius F, Anderssen SA (2015) High-intensity training following lung cancer surgery: a randomised controlled trial. Thorax 70:244–250. https://doi.org/10.1136/thoraxjnl-2014-205944
Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, Carbone PP (1982) Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 5:649–656. https://doi.org/10.1097/00000421-198212000-00014
Fletcher GF, Ades PA, Kligfield P, Arena R, Balady GJ, Bittner VA, Coke LA, Fleg JL, Forman DE, Gerber TC, Gulati M, Madan K, Rhodes J, Thompson PD, Williams MA, American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee of the Council on Clinical Cardiology, Council on Nutrition, Physical Activity and Metabolism, Council on Cardiovascular and Stroke Nursing, and Council on Epidemiology and Prevention (2013) Exercise standards for testing and training: a scientific statement from the American Heart Association. Circulation 128:873–934. https://doi.org/10.1161/CIR.0b013e31829b5b44
Cheville AL, Rhudy L, Basford JR, Griffin JM, Flores AM (2017) How receptive are patients with late stage cancer to rehabilitation services and what are the sources of their resistance? Arch Phys Med Rehabil 98:203–210. https://doi.org/10.1016/j.apmr.2016.08.459
Suetta C, Magnusson SP, Beyer N, Kjaer M (2007) Effect of strength training on muscle function in elderly hospitalized patients. Scand J Med Sci Sports 17:464–472. https://doi.org/10.1111/j.1600-0838.2007.00712.x
Buchheit M, Laursen PB (2013) High-intensity interval training, solutions to the programming puzzle. Sport Med 43:313–338. https://doi.org/10.1007/s40279-013-0029-x
Papadopoulos E, Santa Mina D (2018) Can we HIIT cancer if we attack inflammation? Cancer Causes Control 29:7–11. https://doi.org/10.1007/s10552-017-0983-y
Stamatis G, Leschber G, Schwarz B, Brintrup DL, Ose C, Weinreich G, Passlick B, Hecker E, Kugler C, Dienemann H, Krbek T, Eggeling S, Hatz R, Müller MR, Weder W, Aigner C, Jöckel KH (2019) Perioperative course and quality of life in a prospective randomized multicenter phase III trial, comparing standard lobectomy versus anatomical segmentectomy in patients with non-small cell lung cancer up to 2 cm, stage IA (7th edition of TNM staging system). Lung Cancer 138:19–26. https://doi.org/10.1016/j.lungcan.2019.09.021
Brown JC, Cespedes Feliciano EM, Caan BJ (2018) The evolution of body composition in oncology-epidemiology, clinical trials, and the future of patient care: facts and numbers. J Cachexia Sarcopenia Muscle 9:1200–1208. https://doi.org/10.1002/jcsm.12379
Hardee JP, Counts BR, Carson JA (2019) Understanding the role of exercise in cancer cachexia therapy. Am J Lifestyle Med 13:46–60. https://doi.org/10.1177/1559827617725283
Radbruch L, Strasser F, Elsner F, Gonçalves JF, Løge J, Kaasa S, Nauck F, Stone P, the Research Steering Committee of the European Association for Palliative Care (EAPC) (2008) Fatigue in palliative care patients — an EAPC approach. Palliat Med 22:13–32. https://doi.org/10.1177/0269216307085183
Lorenz D, Morrison S (2015) Current concepts in periodization of strength and conditioning for the sports physical therapist. Int J Sports Phys Ther 10:734–747
Fairman CM, Zourdos MC, Helms ER, Focht BC (2017) A scientific rationale to improve resistance training prescription in exercise oncology. Sport Med 47:1457–1465. https://doi.org/10.1007/s40279-017-0673-7
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Codima, A., das Neves Silva, W., de Souza Borges, A.P. et al. Exercise prescription for symptoms and quality of life improvements in lung cancer patients: a systematic review. Support Care Cancer 29, 445–457 (2021). https://doi.org/10.1007/s00520-020-05499-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-020-05499-6