Abstract
Background
Patients initiating highly emetic chemotherapy (HEC) are at a 90% risk of chemotherapy-induced nausea and vomiting (CINV). Despite guideline-concordant antiemetic prescribing preventing CINV in up to 80% of patients, studies suggest that guideline-concordant antiemetic regimen use by patients initiating HEC is sub-optimal. However, these studies have been limited to single-site or single-cancer type with limited generalizability. The objective of this study was to describe antiemetic fill regimens and to assess predictors of underuse in the USA.
Methods
Our study population was adult patients under the age of 65 with cancer initiating intravenous HEC between 2013 and 2015 with employer-sponsored insurance in the IBM Watson/Truven MarketScan Commercial Claims database (N = 31,923). Descriptive statistics were used to explain antiemetic prescribing patterns, including antiemetic underuse. Modified Poisson regression was used to identify factors associated with antiemetic underuse.
Results
Among individuals initiating HEC, 49% underused guideline-concordant antiemetics. Most classified as under-using lacked an NK1 fill. While dexamethasone and 5HT3A uptake was over 80%, olanzapine use was minimal. Having lower generosity for prescription and medical benefits (paying more versus less than 20% out-of-pocket) increased the underuse risk by 3% and 4% (RR,1.03; 95% CI,1.01–1.05; P = 0.01 and RR,1.04; CI, 1.00–1.09; P = 0.03), respectively. Additionally, compared to receiving chemotherapy in the physician office setting, patients were at a 28% (RR, 1.28; 95% CI, 1.25–1.30; P < 0.0001) higher underuse risk in the outpatient hospital setting.
Conclusion
Antiemetic underuse is high in patients initiating HEC, potentially leading to avoidable CINV events. We found that insurance generosity has a minimal effect on antiemetic guideline concordance in this population, suggesting discordance may be the result of site of care as well as gaps in provider knowledge or accountability.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the USA, the increased attention on reducing healthcare spending has led to an emphasis on high-quality, evidence-based care. Oncology is a promising target for such efforts given the high costs associated with cancer care [1, 2] and the need to balance patient preferences regarding quality of life and survival. Evidence is emerging that promoting value-based cancer treatment and supportive care is effective in reducing cancer-associated spending [3, 4].
Despite their benefit, certain types of chemotherapy result in severe nausea and vomiting. Chemotherapy-induced nausea and vomiting (CINV) not only has significant clinical impacts, but also reduces patients’ quality of life [5,6,7]. Studies have also consistently demonstrated that direct costs are higher in patients with uncontrolled CINV versus those who do not experience CINV [8,9,10,11,12,13]. Average CINV costs among those who experience an event range from $1280 to $5826 [8,9,10]. Patients also highly fear CINV, which may also inhibit chemotherapy treatment adherence [6, 14,15,16,17].
Evidence has overwhelmingly demonstrated that the type of chemotherapy initiated is the best determinant of CINV-risk, which is > 90% among those at high risk [18, 19]. However, antiemetic drugs are a highly effective prophylaxis to prevent CINV and subsequently improve downstream quality of life and potentially generate cost-savings by avoiding CINV-associated healthcare resource use [5, 11, 14, 16]. Conventional antiemetic drugs used to prevent acute and delayed CINV, in order of least to most potent, are glucocorticoids, 5-HT3 receptor antagonists (5HT3A), and NK1 receptor antagonists. (Other antiemetics are also used as rescue therapy for breakthrough CINV events.) US-based guidelines developed by the American Society of Clinical Oncology (ASCO) and the National Comprehensive Cancer Network (NCCN) offer recommendations on the appropriate use of antiemetic drugs to prevent acute and delayed CINV based on the classification of the likelihood of emesis of the chemotherapy regimen [18, 19]. Notably, there are many guideline-concordant CINV prophylactic antiemetic strategies for patients initiating highly emetogenic chemotherapy (HEC) with varying costs, and there is no preferred option.
Despite clinical trial data suggesting that guideline-concordant antiemetic use could prevent CINV in 80% of patients, it is suggested that antiemetic use in the USA is suboptimal in patients initiating HEC [20,21,22,23,24]. However, these studies have been limited to single-site or single-cancer type with limited generalizability. The purposes of our study were to understand antiemetic underuse among patients initiating intravenous HEC by characterizing patterns of antiemetic use and identify factors associated with antiemetic underuse among a large sample of commercially insured patients receiving anticancer therapy.
Methods
Data source
We used the IBM Watson/Truven MarketScan Commercial Claims and Encounters Database to identify patients with employer-sponsored insurance initiating HEC between January 2013 and December 2015 in the USA. The study was reviewed by the University of North Carolina at Chapel Hill’s Institutional Review Board (IRB) and was exempt.
Cohort selection
We included adult patients (age 18–64) with cancer who newly initiated HEC in a physician office or outpatient hospital-affiliated setting between 2013 and 2015. Highly emetogenic chemotherapies were identified using NCCN and ASCO guidelines available in 2015 (Supplement Table 1) [25,26,27,28,29,30,31]. Chemotherapies with body surface area-based risk were categorized as highly emetogenic since body surface area is unmeasured in our data source. For assessing predictors of antiemetic underuse, we further restricted the cohort to those diagnosed before October 1, 2015 (due to changes in medical coding between ICD-9 and ICD-10 in October 2015 and beyond). We also required patients to have at least 6 months of continuous health plan enrollment prior to their first observed (index) chemotherapy claim to ensure they are newly initiating HEC, and to have a follow-up of at least 1 month after chemotherapy initiation to ensure adequate follow-up time for assessing antiemetic claims. Next, we required that patients have a primary diagnosis of cancer recorded on the claim with the chemotherapy infusion. Cancer diagnosis codes were identified using the Agency for Healthcare Research and Quality ICD-9 and ICD-10 Clinical Classification Software (CCS)) for “neoplasm.” We excluded patients who were pregnant and those with schizophrenia and bipolar disorder (to avoid antiemetic misclassification since olanzapine may be used to treat mood disorders). Finally, we required patients to have their prescription drug data available through MarketScan to ensure that a lack of fills was not due to missing data.
Measurement
To identify antiemetics, we created binary indicator variables for each antiemetic product (0 = no/1 = yes) for each patient, including preventative and breakthrough medications (Supplement Table 2) [30, 31]. Antiemetics were identified using Healthcare Common Procedure Coding System codes for physician-administered products billed in outpatient settings (physician office or hospital-affiliated outpatient practices) and National Drug Codes for oral products billed through the outpatient pharmacy benefit.
Intravenously (IV) administered antiemetics were assessed on the day of chemotherapy administration. Oral products were assessed from the day of chemotherapy administration through 32 days prior to chemotherapy administration. This timeframe was selected as physicians often prescribe oral antiemetics prior to chemotherapy administration, allowing the patient time to fill these products in advance. We found that a look-back period of 32 days captured 75% of antiemetic fills that were obtained prior to highly emetogenic intravenous chemotherapy administration.
We characterized antiemetics by product, class, administration route, and number. We also calculated the associated total and out-of-pocket costs for all filled medications. All costs were inflation-adjusted to 2016 USD using the medical component of the Consumer Price Index. Claims with “zero-dollar” total costs or negative copay, deductible, coinsurance, or net pay were excluded. To assess guideline concordance for preventing CINV in patients initiating HEC, we compared the combination of antiemetic products against the ASCO and NCCN antiemetic guidelines available in 2015 (Supplement Table 3) [25,26,27,28]. Regimens that were concordant in prior years were generally still considered concordant in more recent years. We also examined the frequency of products used by class to determine which products are most and least frequently used among guideline-concordant users. Some chemotherapy regimens (i.e., cyclophosphamide-only and anthracycline-only regimens) are considered highly emetogenic based on a surface area threshold level, which was not available in the claims data. Subsequently, we also assessed underuse by type of chemotherapy received (i.e., anthracycline + cyclophosphamide on the same day, cyclophosphamide only, anthracycline only, and other).
Predictors of interest included chemotherapy setting (physician office or hospital-affiliated outpatient clinic), urban/rural location, geographic region, patient gender, age, health insurance type, insurance generosity, year and quarter of chemotherapy administration, chemotherapy regimen, number of comorbid conditions, number of concomitant medications, prior antiemetic use, prior non-highly emetic chemotherapy (IV), and prior radiation therapy [32].
Statistical analysis
Descriptive statistics were calculated to assess patterns of use, guideline-concordant antiemetic drug use. Factors associated with antiemetic underuse were assessed using a modified Poisson regression, which directly estimates risks and risk ratios (while controlling for the influence of other factors in the model) [33]. The overestimated standard error was corrected using Huber-White standard errors.
Results
We identified 56,744 adult patients (age 18–64) initiating HEC between 2013 and 2015. (Of these patients, 55,096 were diagnosed before October 1, 2015, prior to the implementation of ICD-10.) Next, we excluded 13,632 patients lacking 6 months of continuous enrollment prior to initiating chemotherapy and 1-month follow-up. Subsequently, we excluded 2040 patients lacking a cancer diagnosis on the claim associated with the HEC administration. We then excluded 1621 patients for being pregnant and 473 for having a diagnosis of either schizophrenia or bipolar disorder. Finally, 7055 patients who lacked prescription drug data were excluded.
Cohort descriptive statistics
Baseline characteristics are detailed in Table 1. Most patients were female (69.9%) and were between the ages of 50 and 64 (68.3%). Among patients in the cohort 44.4% had breast cancer, and 34.9% used a chemotherapy regimen consisting of an anthracycline and cyclophosphamide. Prior use of antiemetics, prior or concomitant use of IV chemotherapy, or prior or concomitant use of radiation therapy, was used by 42.8%, 15.9%, and 16.7% of the population, respectively. The average number of comorbid conditions, excluding cancer, was 0.2 (SD = 0.7), with patients taking on average, 3.6 (SD = 2.9) concomitant medications, excluding antiemetics, in the past 30 days. Approximately 85% of patients resided in an urban setting, with the highest proportion of patients in the Southern US (40.4%). These regional differences are expected based on the distribution of data contributors providing claims to the MarketScan in the study period. Over half of patients had a PPO plan, and 90.9% and 38.0% of patients had good medical benefit and prescription drug generosity, respectively (i.e., the proportion of out-of-pocket costs is less than 20% of the total healthcare cost). Chemotherapy was primarily administered in the physician office (53.6%) and outpatient hospital settings (45.2%).
Characterization of antiemetic filled in the pre-period
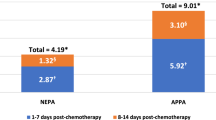
Approximately 97% of patients (N = 31,047) receiving highly emetogenic intravenous chemotherapy filled at least one antiemetic drug, with a median of three unique products (Fig. 1). Dexamethasone, 5HT3A, NK1, and rescue therapies had at least one fill for 85%, 88%, 58%, and 68% of patients (Fig. 2). Less than 1% of patients had at least one olanzapine fill. Of the 119,728 antiemetic claims, aprepitant and fosaprepitant were the primary NK1s filled (12% and 88%, respectively) (Supplement Fig. 1). Among the 5HT3As, the second-generation 5HT3A product (palonosetron) was filled more frequently than first generation products (67% versus 33% of fills, respectively). Out-of-pocket costs were generally low across preventative antiemetics, with physician-administered products having $0 median out-of-pocket costs (not displayed).
Percent of patients using at least one antiemetic among all patients initiating highly emetogenic chemotherapy. First-generation 5HT3A: ondansetron, granisetron, dolasetron; second-generation 5HT3A: palonosetron; NK1: aprepitant, fosaprepitant, rolapitant, netupitant-palonosetron combination (NK1 + 5HT3A combo)
Guideline concordance of antiemetics filled in the pre-period
Approximately 49% of patients filled antiemetic regimens that are considered underuse by guidelines (Fig. 3). Of the concordant strategies, only 0.19% consisted of olanzapine + palonosetron + dexamethasone, while the rest were NK1-based (not displayed). The most common reason for underuse was not filling an NK1 (85%). Interestingly, among the 58% of patients filling an NK1, most (87%) were concordant. The most common reason for discordance among patients who filled an NK1 was lacking a dexamethasone fill. Among those who filled at least one second-generation 5HT3A, the concordance rate was 65% versus 41% among those who filled at least one first-generation 5HT3A. Among patients initiating anthracycline + cyclophosphamide regimens and non-surface-area-based chemotherapy regimens, guideline underuse decreased to 35% and 39%, respectively (Fig. 4). For surface-area-based chemotherapies, underuse was high at 69% for anthracycline-only regimens and 78% for cyclophosphamide therapies.
Chemotherapy type concordance versus underuse of antiemetic strategies by chemotherapy type. Anth + cyclo cyclophosphamide + anthracycline (doxorubicin, epirubicin, idarubicin) on the same day. Surface area chemotherapies = anthracycline and cyclophosphamide. Other HEC: given the limited frequencies (< 1%) of carmustine, dacarbazine, mechlorethamine, streptozocin, and ifosfamide, we grouped them together with cisplatin (76%)
Predictors of antiemetic underuse
Multivariable regression results assessing predictors of antiemetic underuse are detailed in Table 2. Type of chemotherapy initiated was the greatest predictor of antiemetic underuse. In fact, the risk of antiemetic underuse among anthracycline-only, cyclophosphamide-only, and carmustine regimen users was 1.78 (95% confidence interval (CI), 1.73–1.84; P < 0.0001), 2.01 (CI, 1.79–2.26; P < 0.0001), and 2.19 (CI, 2.12–2.25; P < 0.0001) times compared to combination anthracycline and cyclophosphamide regimens. Receiving chemotherapy in an outpatient hospital setting compared to a physician office (RR = 1.28; CI, 1.25–1.30; P < 0.0001) and having prior/concomitant chemotherapy (RR = 1.22; CI, 1.18–1.25; P < 0.0001) were the other largest predictors of antiemetic underuse. The risk of underuse was 3% and 4% higher among those having more than 20% out-of-pocket costs versus having less than 20% out-of-pocket costs (RR = 1.03; CI, 1.01–1.05; P = 0.01 and RR, 1.04; CI, 1.00–1.09; P = 0.03) in the prescription drug benefit and medical benefit, respectively.
Discussion
The primary purposes of this study were to describe antiemetic fill regimens, to assess the proportion of antiemetic underuse, and to assess the predictors of underuse in patients with cancer who are initiating highly emetogenic, intravenous chemotherapy. We found that 97% of commercially insured adult patients under the age of 65 newly initiating HEC filled at least one antiemetic drug, aligning with prior US studies [21, 24]. Furthermore, more than 80% of patients filled at least one 5HT3A and dexamethasone, indicative of provider understanding that patients initiating emetogenic chemotherapy should be prescribed an antiemetic strategy to prevent CINV. In contrast, only 58% of patients filled NK1s, which is still a higher proportion than in a study conducted between 2006 and 2008 that found only 11% of patients filled NK1s [24].
Despite NCCN recommending olanzapine for preventative use since 2014 and its low costs, limited olanzapine fills were seen [25]. We hypothesize few reasons for this. First, providers may have concerns about the safety of olanzapine, including a black box warning for death in elderly patients with dementia-related psychosis, despite the short duration of use and evidence demonstrating that adverse event rates with olanzapine strategies were similar to the comparator arm [34]. Second, because this indication for olanzapine is not FDA-approved, manufacturers are unable to market this indication to providers, so dissemination of evidence of olanzapine’s use for CINV prevention is limited compared to that of other antiemetic products, which have an FDA-approved indication [35]. Third, there is a limited evidence base for olanzapine use prior to 2016 [36]. Given the new randomized controlled evidence published in 2016, as well as olanzapine’s incorporation into the ASCO guidelines in 2017, higher uptake is anticipated in the future [18, 34].
Underuse of guideline-concordant antiemetic fills was high at 49%. These results align with a prior study that found that 56.4% of breast cancer patients on anthracycline-based therapy received guideline-concordant antiemetic use in the commercial claims population in 2013 [22]. Another US study estimated guideline-concordance to be 91% on day 1 in a practice group in the southeast; however, these providers used an EMR system embedded with a standardized antiemetic protocol [21]. We found that the most common reason for discordance in the current study was patients not receiving an NK1 (85%). This aligns with prior studies that estimate that a lack of an NK1 constitutes 51–80% of the reasons for guideline discordances [21,22,23, 37, 38]. The high underuse of NK1s is surprising given their inclusion in treatment guidelines since 2006. This highlights an opportunity for further provider education as there is a robust evidence base supporting the superiority of NK1s over 5HT3As for achieving clinical outcomes and reducing downstream economic impacts. However, it is important to note that the study data source, claims data, is limited to drugs filled by the patient versus drugs prescribed by the provider.
A potential explanation for low NK1 fills is treatment acquisition cost, as they are the most expensive class of antiemetics. However, median out-of-pocket costs for NK1s was low among patients who filled these products. Importantly, we are unable to discern the costs of drugs that were not filled which may result in our underestimation of out-of-pocket expenses for patients. We attempted to address this by using a marker for insurance generosity based on prior health services use and found that patients with more generous medical benefit and prescription drug coverage were less likely to underuse antiemetics than those with less generous coverage; but, these effect sizes were small (≤ 4%) suggesting that NK1 cost may not be the driving issue. Furthermore, a higher proportion of patients filled second-generation 5HT3A (palonosetron) versus cheaper, first-generation 5HT3As (as low as $1.10/treatment cycle) despite a lack of prioritization by guidelines [18]. Intravenous palonosetron costs $229 (2016 USD)/treatment cycle, just slightly less expensive than the cheapest NK1, intravenous fosaprepitant at $299 (2016 USD)/treatment cycle.
We found that compared to receiving chemotherapy in the physician office setting, patients receiving chemotherapy in an outpatient hospital setting were at a 28% (P < 0.0001) higher risk of underuse. This may be the result of increased marketing access to providers in non-hospital and non-health system physicians versus those that are part of a hospital or healthcare system or because physicians in the community setting may be incentivized to use more expensive drugs [39,40,41]. We also found that concordance increases by about 10% in both populations when assessing anthracycline + cyclophosphamide-regimens and non-surface-area-based regimens, which are strictly HEC regimens, and we found that patients receiving anthracycline and cyclophosphamide combination regimens are less likely to underuse compared to anthracycline-only and cyclophosphamide-only regimens. High underuse in the anthracycline- and cyclophosphamide-only populations is expected given that a limitation of claims-based data sources does not provide surface-area-based dosage levels for infused products, and patients may be receiving doses that are considered moderately emetogenic chemotherapy versus HEC. To the extent that this is the case, we overestimated antiemetic underuse in these populations.
Other limitations including the total price of the drugs used to calculate total and out-of-pocket costs were based on the transaction price between the manufacturers and the payer listed in MarketScan, which does not reflect rebates and discounts received by payers and thus may overestimate the cost to payers for antiemetics. However, because rebates and discount are not typically shared with the patients, we anticipated out-of-pocket estimates to be accurate. Additionally, the preventative antiemetic look-back period chosen a priori based on expert opinion incorporated a minimum rate of antiemetic use in the measure, which increases the risk of capturing antiemetics not intended for CINV prevention. To address this, we limited the look-back period calculation to only preventative antiemetic drugs. However, this may still underestimate the proportion of patients who underused antiemetics. Next, our data had limited overlap following the approval of the netupitant-palonosetron combination in late 2014 and rolapitant in late 2015 potentially contributing to the low uptake observed for these products. Additionally, while phase III studies supporting the use of olanzapine as a prophylactic antiemetic in the USA were published as early as 2011, NCCN included it as a recommendation only in 2014, ASCO highlighted it as a highly promising therapy in 2015, and the largest trial to date was published in 2016, again providing limited overlap with our study period [25, 28, 34, 42, 43]. We also do not have data on provider-level or facility-level characteristics such as whether an automated electronic medical record prescribing system existed that may be dictating antiemetic use versus a patient’s characteristics. Finally, we have no information regarding patient or provider preference for antiemetic use, which may influence uptake of these products.
This study provides new evidence of antiemetic underuse among commercially insured chemotherapy users who are under 65 years of age, an important and understudied age group. Specifically, our study found that preventive antiemetic use is alarmingly high in patients initiating HEC, with NK1 underuse largely explaining this discordance. Whether guideline-discordant prescribing is due to a gap in provider knowledge or provider accountability is unknown. If it is the former, provider education by professional societies, patient advocacy groups, payers, and manufacturers are necessary. If it is the latter, one solution is the development of a validated, appropriate antiemetic prescribing measure for patients initiating HEC that is implemented into commercial plan quality programs and the CMS Merit-Based Incentive Payment System. Notably, ASCO’s Quality Oncology Practice Initiative program includes an antiemetic measure for patients initiating highly emetogenic and moderately emetogenic chemotherapy under its symptom/toxicity management module [44]. However, it requires only that providers prescribe a 5HT3A and dexamethasone for patients initiating HEC, in contradiction with guidelines that also recommend an NK1. It also does not allow for olanzapine-based strategies to fulfill the measure. This highlights the importance of quality initiatives appropriately incorporating guideline recommendations into their measures as over 8000 oncologists are registered for QOPI across the USA [45].
Future studies should assess the uptake of newer antiemetic products and regimens in patients initiating HEC with more recent data to understand their fill trends. Supplementing claims analysis, which provides data on what medications were filled, with other data sources could help triangulate occurrences of care failure and address them. For example, EMRs include antiemetic prescribing data and chemotherapy dosing information while patient diaries include data on what antiemetics patients actually took. Additionally, understanding the real world outcomes (i.e., CINV events and their associated healthcare resource) and subsequent activities (e.g., future antiemetic prescribing and chemotherapy adherence) associated with antiemetic underuse will support the value of appropriate prescribing.
References
Mariotto AB, Yabroff KR, Shao Y, Feuer EJ, Brown ML (2011) Projections of the cost of cancer care in the United States: 2010-2020. J Natl Cancer Inst 103(2):117–128
National Cancer Institute (2011) Cancer prevalence and cost of care projections. https://costprojections.cancer.gov. Accessed 19 Jan 2017
Feinberg BA, Lang J, Grzegorczyk J et al (2012) Implementation of cancer clinical care pathways: a successful model of collaboration between payers and providers. J Oncol Pract 8(3 Suppl):e38s–e43s
Newcomer LN, Gould B, Page RD, Donelan SA, Perkins M (2014) Changing physician incentives for affordable, quality cancer care: results of an episode payment model. J Oncol Pract 10(5):322–326
Sommariva S, Pongiglione B, Tarricone R (2016) Impact of chemotherapy-induced nausea and vomiting on health-related quality of life and resource utilization: a systematic review. Crit Rev Oncol Hematol 99:13–36
Cohen L, de Moor CA, Eisenberg P, Ming EE, Hu H (2007) Chemotherapy-induced nausea and vomiting: incidence and impact on patient quality of life at community oncology settings. Supporti Care Cancer 15(5):497–503
Osoba D, Zee B, Warr D, Latreille J, Kaizer L, Pater J (1997) Effect of postchemotherapy nausea and vomiting on health-related quality of life. The Quality of Life and Symptom Control Committees of the National Cancer Institute of Canada Clinical Trials Group. Support Care Cancer 5(4):307–313
Burke TA, Wisniewski T, Ernst FR (2011) Resource utilization and costs associated with chemotherapy-induced nausea and vomiting (CINV) following highly or moderately emetogenic chemotherapy administered in the US outpatient hospital setting. Support Care Cancer 19(1):131–140
Tina Shih YC, Xu Y, Elting LS (2007) Costs of uncontrolled chemotherapy-induced nausea and vomiting among working-age cancer patients receiving highly or moderately emetogenic chemotherapy. Cancer. 110(3):678–685
Haiderali A, Menditto L, Good M, Teitelbaum A, Wegner J (2011) Impact on daily functioning and indirect/direct costs associated with chemotherapy-induced nausea and vomiting (CINV) in a U.S. population. Support Care Cancer 19(6):843–851
Craver C, Gayle J, Balu S, Buchner D (2011) Clinical and economic burden of chemotherapy-induced nausea and vomiting among patients with cancer in a hospital outpatient setting in the United States. J Med Econ 14(1):87–98
Ihbe-Heffinger A, Ehlken B, Bernard R, Berger K, Peschel C, Eichler HG, Deuson R, Thödtmann J, Lordick F (2004) The impact of delayed chemotherapy-induced nausea and vomiting on patients, health resource utilization and costs in German cancer centers. Ann Oncol 15(3):526–536
Lordick F, Ehlken B, Ihbe-Heffinger A et al (2007) Health outcomes and cost-effectiveness of aprepitant in outpatients receiving antiemetic prophylaxis for highly emetogenic chemotherapy in Germany. Eur J Cancer 43(2):299–307
Viale PH, Grande C, Moore S (2012) Efficacy and cost: avoiding undertreatment of chemotherapy-induced nausea and vomiting. Clin J Oncol Nurs 16(4):E133–E141
Jordan K, Sippel C, Schmoll HJ (2007) Guidelines for antiemetic treatment of chemotherapy-induced nausea and vomiting: past, present, and future recommendations. Oncologist 12(9):1143–1150
Navari RM, Aapro M (2016) Antiemetic prophylaxis for chemotherapy-induced nausea and vomiting. N Engl J Med 374(14):1356–1367
National Cancer Institute (2017) Treatment-Related Nausea and Vomiting (PDQ®)–Health Professional Version. https://www.cancer.gov/about-cancer/treatment/side-effects/nausea/nausea-hp-pdq. Accessed 19 Jan 2017
Hesketh PJ, Kris MG, Basch E, Bohlke K, Barbour SY, Clark-Snow RA, Danso MA, Dennis K, Dupuis LL, Dusetzina SB, Eng C, Feyer PC, Jordan K, Noonan K, Sparacio D, Somerfield MR, Lyman GH (2017) Antiemetics: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol 35(28):3240–3261
National Comprehensive Cancer Network (2017) NCCN clinical practice guidelines in oncology: antiemesis V1. 2017
Jordan K, Gralla R, Jahn F, Molassiotis A (2014) International antiemetic guidelines on chemotherapy induced nausea and vomiting (CINV): content and implementation in daily routine practice. Eur J Pharmacol 722:197–202
Gilmore JW, Peacock NW, Gu A, Szabo S, Rammage M, Sharpe J, Haislip ST, Perry T, Boozan TL, Meador K, Cao X, Burke TA (2014) Antiemetic guideline consistency and incidence of chemotherapy-induced nausea and vomiting in US community oncology practice: INSPIRE Study. J Oncol Pract 10(1):68–74
Chavez-MacGregor M, He W, Zhao H et al (2015) Antiemesis prophylaxis among breast cancer (BC) patients receiving anthracyline-based chemotherapy: a population-based study. 2015 Multinational Association of Supportive Care in Cancer/International Society of Oral Oncology International Symposium on Supportive Care in Cancer; June 25–27, 2015, Copenhagen, Denmark
Check DK, Reeder-Hayes KE, Basch EM, Zullig LL, Weinberger M, Dusetzina SB (2016) Investigating racial disparities in use of NK1 receptor antagonists to prevent chemotherapy-induced nausea and vomiting among women with breast cancer. Breast Cancer Res Treat 156(2):351–359
Rogers MP, Blackburn L (2010) Use of neurokinin-1 receptor antagonists in patients receiving moderately or highly emetogenic chemotherapy. Clin J Oncol Nurs 14(4):500–504
National Comprehensive Cancer Network (2014) Clinical practice guidelines in oncology: antiemesis. Version 2. 2014. https://www.nccn.org/store/login/login.aspx?ReturnURL=https://www.nccn.org/professionals/physician_gls/pdf/antiemesis.pdf. Accessed 19 Jan 2017
National Comprehensive Cancer Network (2015) Clinical practice guidelines in oncology: antiemesis (Version 2.2015)
Basch E, Prestrud AA, Hesketh PJ, Kris MG, Feyer PC, Somerfield MR, Chesney M, Clark-Snow RA, Flaherty AM, Freundlich B, Morrow G, Rao KV, Schwartz RN, Lyman GH, American Society of Clinical Oncology (2011) Antiemetics: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol 29(31):4189–4198
Hesketh PJ, Bohlke K, Lyman GH, Basch E, Chesney M, Clark-Snow RA, Danso MA, Jordan K, Somerfield MR, Kris MG, American Society of Clinical Oncology (2016) Antiemetics: American Society of Clinical Oncology focused guideline update. J Clin Oncol 34(4):381–386
National Cancer Institute (2017) Cancer therapy look-up tables - chemotherapy, hormone therapy, and immunotherapy. https://crn.cancer.gov/resources/codes.html. Accessed 20 Jan 2018
Centers for Medicare & Medicaid Services (2017) ASP drug pricing files 2017. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Part-B-Drugs/McrPartBDrugAvgSalesPrice/2017ASPFiles.html. Accessed 1 Jan 2018
Centers for Medicare & Medicaid Services (2016) Table of Drugs. https://www.cms.gov/Medicare/Coding/HCPCSReleaseCodeSets/Downloads/2016-Table-of-Drugs.pdf. Accessed 16 Jan 2018
National Cancer Institute (2017) NCI Comorbidity Index Overview. SEER-Medicare LInked Database - Comorbidity Index Overview https://healthcaredelivery.cancer.gov/seermedicare//considerations/comorbidity.html. Accessed 05/29/2017
Zou G (2004) A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol 159(7):702–706
Navari RM, Qin R, Ruddy KJ, Liu H, Powell SF, Bajaj M, Dietrich L, Biggs D, Lafky JM, Loprinzi CL (2016) Olanzapine for the prevention of chemotherapy-induced nausea and vomiting. N Engl J Med 375(2):134–142
Food and Drug Administration Modernization Act of 1997, 21 U.S.C. (1997)
Fonte C, Fatigoni S, Roila F (2015) A review of olanzapine as an antiemetic in chemotherapy-induced nausea and vomiting and in palliative care patients. Crit Rev Oncol Hematol 95(2):214–221
Aapro M, Molassiotis A, Dicato M, Peláez I, Rodríguez-Lescure Á, Pastorelli D, Ma L, Burke T, Gu A, Gascon P, Roila F, on behalf of the PEER investigators (2012) The effect of guideline-consistent antiemetic therapy on chemotherapy-induced nausea and vomiting (CINV): the Pan European Emesis Registry (PEER). Ann Oncol 23(8):1986–1992
Burmeister H, Aebi S, Studer C, Fey MF, Gautschi O (2012) Adherence to ESMO clinical recommendations for prophylaxis of chemotherapy-induced nausea and vomiting. Support Care Cancer 20(1):141–147
Bach PB, Jain RH (2017) Physician’s office and hospital outpatient setting in oncology: it’s about prices, not use. J Oncol Pract 13(1):4–5
Malin JL, Weeks JC, Potosky AL, Hornbrook MC, Keating NL (2013) Medical oncologists’ perceptions of financial incentives in cancer care. J Clin Oncol 31(5):530–535
IQVIA (SK&A) (2017) Commercial Access to Physicians: Medical Industry Sales Reps Accessibility to U.S. Physicians. SK&A
Chiu L, Chow R, Popovic M, Navari RM, Shumway NM, Chiu N, Lam H, Milakovic M, Pasetka M, Vuong S, Chow E, DeAngelis C (2016) Efficacy of olanzapine for the prophylaxis and rescue of chemotherapy-induced nausea and vomiting (CINV): a systematic review and meta-analysis. Support Care Cancer 24(5):2381–2392
Navari RM, Gray SE, Kerr AC (2011) Olanzapine versus aprepitant for the prevention of chemotherapy-induced nausea and vomiting: a randomized phase III trial. J Support Oncol 9(5):188–195
ASCO Institute for Quality (2018) Quality oncology practice initiative measures overview. https://www.instituteforquality.org/qopi/measures. Accessed 16 Jan 2018
ASCO Institute for Quality (2018) Quality oncology practice initiative participating practices. https://www.instituteforquality.org/qopi/participating-practices. Accessed 16 Jan 2018
Acknowledgements
The database infrastructure used for this project was funded by the Department of Epidemiology, UNC Gillings School of Global Public Health; the Cecil G. Sheps Center for Health Services Research, UNC; the CER Strategic Initiative of UNC’s Clinical Translational Science Award (UL1TR001111); and the UNC School of Medicine.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Mahendraratnam was a Worldwide Health Economics and Outcomes Research Pre-doctoral Fellow at Bristol-Myers Squibb and a Fellow at the Duke-Margolis Center for Health Policy. She completed an internship a Genentech, a member of the Roche Group in 2015. Dr. Wheeler received served as the Primary Investigator for a project funded by Pfizer, but it is unrelated to this work. Dr. Dusetzina is a member of the Institute for Clinical and Economic Review (ICER) Midwest Comparative Effectiveness Public Advisory Council and served on the National Academy of Sciences, Engineering, and Medicine Committee “Ensuring Patient Access to Affordable Drug Therapies.” All the other authors declare that they have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mahendraratnam, N., Farley, J.F., Basch, E. et al. Characterizing and assessing antiemetic underuse in patients initiating highly emetogenic chemotherapy. Support Care Cancer 27, 4525–4534 (2019). https://doi.org/10.1007/s00520-019-04730-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-019-04730-3