Abstract
Purpose
Colorectal cancer (CRC) survivors spend approximately 9 h per day in sedentary behavior (SED), despite recommendations to reduce sitting time. The purpose of this study was to examine predictors of SED among CRC survivors over a 1-year duration.
Methods
Male and female CRC survivors (< 5 years since diagnosis) participated in a 12-week moderate-to-vigorous physical activity randomized controlled trial. To measure SED, participants were given a CSA monitor to wear for three consecutive days (including one weekend day). Additionally, fitness (Treadmill walk test), body composition (bioelectrical impedance analysis) and questionnaires (Profile of Mood States, Exercise Processes of Change and Self-Efficacy for Exercise) were administered. Follow-up assessments were completed at a 3-month, 6-month, and 12-month follow-up.
Results
Forty-six colorectal survivors (average age = 57.3 ± 9.7 years) completed the 12-month study. Using latent class models, four classes of SED behavior over time were identified: class 1 (high and sustained SED over time), class 2 (low and sustain SED over time), class 3 (increasing SED over time), and class 4 (high SED through 6-months, followed be a marked decrease at 12-months). Males were more likely to be in class 1, while majority of females were in class 3. Those CRC survivors with a better mood at baseline were in class 2, while those with poor fitness, high body fat, and higher cognitive processes at baseline were in class 3.
Conclusion
Identifying the characteristics of survivors who engage in high SED can help healthcare providers to target their efforts to reduce SED.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sedentary behavior (SED), commonly defined as prolonged sitting or any activity accumulating < 1.5 metabolic equivalents (METs) is associated with chronic disease, cardiovascular disease, and all-cause mortality [1,2,3,4]. The American Cancer Society has advised adults to reduce prolonged periods of SED such as screen-based entertainment [5] in effort to maintain weight and reduce risk of developing certain types of cancers (e.g., breast, colon, endometrial) [6]. However, even with the recommendations and associated detriments to health, colorectal cancer (CRC) survivors spend approximately 8.75 h per day in objectively measured SED [7]; fairly consistent with other objectively assessed SED (~ 9.5 h) among breast and prostate cancer survivors [8]. Identifying ways to reduce SED among CRC and other cancer populations remains a challenging obstacle facing researchers and healthcare providers. Identifying survivors who may be at risk of high SED, based on their specific characteristics (i.e., demographics, mental, and physical health) may be a useful approach to steer them away from increased SED.
Researchers have begun to identify correlates significantly associated with SED among CRC survivors. In a cross sectional study, characteristics such as multiple comorbidities, being male, and having a higher body mass index (BMI) were significantly associated with increased SED among CRC survivors [7]. A two-armed randomized controlled trial evaluating a 6-month telephone delivered intervention for healthy behavior change (i.e., physical activity, dietary habits, smoking) among CRC survivors noted being older (> 60 years), male and non-obese were more likely to reduce SED in response to the intervention [9]. The need for additional longitudinal work to understand predictors of SED (as opposed to correlates) [10] can help healthcare providers to guide cancer survivors away from developing a sedentary lifestyle.
Very few studies have examined the longitudinal predictors of SED among CRC survivors such as body composition (i.e., fat mass), fitness, mood, self-efficacy for exercise, and exercise processes of change. Thus, the purpose of this exploratory study is to identify predictors of SED among CRC survivors over a 12-month duration. We hypothesized, those survivors who were less fit and had high body fat, lower self-efficacy for exercise, and low use of cognitive processes were more likely to have increased SED compared to their counterparts.
Methods
Male and female CRC survivors were invited to participate in a home-based PA intervention. Study methods have been previously reported [11]. Briefly, CRC survivors were randomized to participate in either (i) a 12-week, home-based PA program targeting moderate-intensity (PA group) or (ii) a contact control condition (control group). Participants were assessed at baseline, 3-months (3M), 6-months, (6M), and 12-months (12M). The Institutional Review Boards at The Miriam Hospital and the Women and Infants Hospital approved the study.
Participants
All interested participants completed a phone screener with research staff to determine initial eligibility. To be eligible for participation, the following criteria were used: (1) ≥ 18 years of age, (2) completed treatment and adjuvant treatment for colon or rectal cancer (Stage 0-3), (3) ≤ 5 years since treatment completion, (4) fluent in the English language, and (5) have access to a telephone. In addition, participants needed to be able to walk unassisted and be sedentary (defined as < 60 min/week of moderate-intensity PA or < 20 min/week of vigorous-intensity PA) over the past 6-months. Exclusion criteria included prior history of cancer and/or a medical or psychiatric illness.
All eligible participants signed an informed consent to participate in the study. Medical clearance was obtained from participant’s oncologist (additional clearance from physicians was provided for those with cardiovascular disease or diabetes).
Randomization
Upon completion of baseline assessments, participants were randomized based on age (< 65 years versus ≥ 65 years), cancer type (colon versus rectal), and gender. Randomization groups included the following: (1) a 12-week, home-based moderate-intensity PA program (PA group), or (2) a contact control condition (control group).
Physical activity group (PA group)
Upon randomization, participants in the PA group met in person with research staff to receive instructions on exercising at moderate-intensity. Specifically, participants were instructed on how to use the heart rate (HR) monitor and pedometer (Digiwalker, Yamax Corporation, Tokyo, Japan) for each PA session. Using the provided HR monitor, participants were instructed to exercise at 64–76% (moderate-intensity) of their estimated maximal HR. In addition to wearing the equipment, participants recorded their HR, steps, and activity on a PA log. Types of activities included brisk walking, biking, or use of home exercise videos. At the start of the program, all participants were encouraged to exercise time times/week for a 10-min duration. Over the 12-week intervention, those in the PA group progressed to 30 min/day on at least 5 days/week.
The PA intervention consisted of 12-weekly calls between the participant and the study Intervention Coordinator. During each call, the Intervention Coordinator reviewed the participant’s previous weeks’ activity, identified PA barriers and problem solved, and reviewed health-related information to ensure safety. If a participant reported physical symptoms that could cause harm such as chest pain or breathing difficulties during PA, they were instructed to halt all activity and contact their physician. Following the 12-weekly calls, the PA group began monthly calls for 3-months with the Intervention Coordinator to continue PA progress and develop a plan to remain active. Throughout the study, participants were never asked about their SED nor did they receive guidance on ways to reduce time spent sitting.
Contact control group (control group)
Control group participants also received weekly calls from research staff for 12-weeks. During these calls, the Intervention Coordinator administered the Symptom Questionnaire to monitor problems such as headaches [12]. Following the 12-weekly calls, the Intervention Coordinator completed monthly calls for 3-months in which the Symptom Questionnaire continued to be administered. SED and ways to reduce time spent sitting was never discussed during the weekly calls or at any point throughout the study duration.
Measures
At baseline, all participants completed demographic, medical, and treatment history questionnaires. Participants completed similar measurements at 3M, 6M, and 12M follow-up visits as described below.
-
a)
Accelerometer data. SED was measured using the Computer Sciences and Applications (CSA), Inc., PA monitor (CSA model 7164). SED was defined as < 100 counts per minutes [13]. Participants were required to wear the monitor during all waking hours on their right hip for three consecutive days (including at least one-weekend day). The monitor was removed during periods where it might get wet such as bathing or swimming. The CSA monitors have been validated among males and females [14]; in addition, PA intensities have been defined [13].
-
b)
Submaximal fitness test. The treadmill walk test was used to measure physical fitness by participants self-selecting the fastest speed in which they were able to walk 1 mile. Once the speed on the treadmill was selected, it was held constant until a mile was completed. Maximal oxygen update (VO2 peak) was calculated using a validated equation [15]. The treadmill walk test has been validated among young, fit adults [16] and older adults [15].
-
c)
Body composition. Using a bioelectrical impedance analysis (BIA), resistance and reactance was measured to calculate fat-free mass and fat mass [17]. With participants in the supine position, the BIA was performed with a single frequency (50 kHz) electrical current produced by a BIA-Quantum II RJL system analyzer (RJL systems, Clinton Township, MI).
-
d)
Mood. The Profile of Mood States (POMS) questionnaire was administered to assess mood and is a reliable method of assessing mood states (i.e., anxiety, confusion, fatigue, and anger) [18]. There are six subscales: depression-dejection, anger-hostility, vigor-activity, fatigue-inertia, tension-anxiety, and confusion-bewilderment within the POMS questionnaire. From these subscales, a Total Mood Disturbance (TMD) score is calculated by summing depression, anger, fatigue, tension, and confusion subscales and then subtracting the vigor subscale.
-
e)
Self-efficacy for exercise: The Exercise Self-Efficacy questionnaire is used to assess the participant’s confidence in exercise during different situations (e.g., when tired or on vacation) [19]. Participants responded to each question using a 5-point scale (1 = not at all confident, 5 = extremely confident). The responses were summed; higher scores indicated a greater confidence to exercise.
-
f)
Exercise processes of change: The exercise processes of change is a 30-item questionnaire used to assess ten processes of change which may affect exercise habits among adults [20]. Of the ten processes of change, five are behavioral (self-liberation, helping relationships, stimulus control, counter conditioning, reinforcement management) and five are cognitive (dramatic relief, environmental reevaluation, social liberation, self-reevaluation). For example, questions such as “I tell myself I am able to keep exercising if I want to” assesses behavioral process, while a cognitive process example is “I recall information people have personally given me on the benefits of exercise”. On a 5-point Likert scale, participants were asked to rate the frequency of use for each process (1 = never, 5 = repeatedly). Higher scores indicated a more common occurrence.
Statistical analyses
Baseline data (demographics, medical history, PA level, and psychosocial constructs) were summarized using means (standard deviations) for continuous data and percentages (N) for categorical variables. Between-group differences in baseline variables have been previously published [11]. Mean SED across study follow-ups (3M, 6M, and 12M) were summarized both between groups and within groups using independent and paired t tests, respectively.
For the purpose of this study, all randomized participants were included in the analysis. We did not impute missing outcomes, but rather, used models that make a missing at random assumption (MAR) with estimation via a likelihood-based approach (EM algorithm). First, using mixed-effects models with subject specific intercepts, we assessed between-group differences in SED over time. Models adjusted for baseline values of the outcome, potential confounders (employment, gender, disease stage), and adjusted standard errors for repeated measures within participant. Results did not suggest significant between group or within group differences over time in SED. Thus, as a subsequent step, we sought to identify patterns of change in SED in the aggregated sample using latent class models (LCM).
LCMs can be thought of as a data reduction technique; simply put, they map vectors of responses (SED at baseline and each follow-up) for each participant to a single class which represents a pattern of behavior change over time (SED in this case). This methodology has the advantage of objectively identifying patterns of behavior change supported by the data. Pattern can then be considered an outcome (or predictor) in subsequent analyses (e.g., we can identify predictors of sedentary pattern of behavior).
In order to identify the ideal number of classes in the data, we fit a series of LCMs with number of classes ranging from 2 to 5. Models were compared using Bayesian Information Criteria (BIC), with lower values indicative of better model fit. The final model (with lowest BIC value) was used to compute the most likely class for each participant, and the distribution of classes across the cohort of participants was summarized.
Analysis of Variance (ANOVA) and chi-squared tests were used to compare baseline demographics, medical history, fitness, and psychosocial constructs between classes. All analyses were carried out in R and SAS Version 9.3 and significance level set at alpha = 0.05 a priori.
Results
Forty-six CRC survivors were included in the final sample. The average age of participants was 57.3 years (SD = 9.73); the majority were female (57%), and nearly three quarters (70%) were diagnosed with Stage 0–2 CRC. A full description of the baseline data has been presented elsewhere [11] and is summarized across randomized groups (PA group vs. control group) in Table 1.
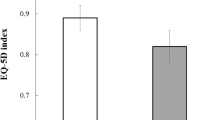
Unadjusted mean SED from baseline through follow-ups (3M, 6M, and 12M) is presented in Fig. 1. Mean objectively measured SED was 1641.65 (SD = 480.56) minutes/monitoring period (3-day monitoring period) and 1791.78 (SD = 342.21) minutes/monitoring period (3-day monitoring period) at baseline and 12M follow-up respectively. Results suggest there were no significant changes in mean SED from baseline to 3M, 3M to 6M or 6M to 12M (p’s > .05) between or within randomized groups.
Data supported a 4-class model of SED over time, with 22% of participants having high and sustained min/monitoring period of SED (class 1), 24% low and sustained SED (class 2), 33% with increasing SED over time (class 3), and 22% with high SED through 6M followed by a marked decrease from 6M to 12M (class 4). These trajectories are illustrated in Fig. 2. With respect to demographics, there were significant between-class differences in gender with female participants more likely to be in classes 2 through 4 compared to class 1 (p < .05). This differs for male participants for whom 90% had high and sustained SED over time (class 1).
Furthermore, there were significant between-class differences in baseline mood, fitness, body fat, and cognitive processes (p’s < .05). Total mood disturbance (TMD) was significantly lower at baseline among those with low and sustained SED over time (class 2). Baseline cognitive processes were significantly higher and fitness and body fat significantly worse at baseline among participants with increasing SED over time (class 3). Mean comparisons for each of the psychosocial, fitness, and demographic variables are presented in Table 2. There were no additional significant between-class differences at baseline.
Discussion
CRC survivors spend the majority of their day in SED [7], even though SED has been associated with poorer quality of life outcomes among cancer survivors [8]. As the number of cancer survivors continues to increase within the USA [21], examining longitudinal predictors associated with SED is a necessary step to identify those individual survivors at a greater risk. The purpose of this study was to identify predictors associated with SED among male and female CRC survivors over a 12-month duration. By identifying these characteristics, health providers can be proactive with their individual approach to reduce SED among this population.
The majority (90%) of male CRC participants fell into class 1 (high and sustained SED), while females were more likely to be in classes 2–4 with a majority (80%) in class 3 (increasing SED over 12M). This difference in SED with gender is consistent within the literature. Previous studies have found being male as a characteristic significantly associated with increased SED (approximately 42 min/day) as compared to female CRC survivors [7]. The difference in time spent in SED between male and female survivors may be partially due to participation in light-intensity activities. Lynch and colleagues showed that greater light-intensity activity was significantly associated with being female among CRC survivors [7]. Higher levels of light-intensity activity (e.g., gardening, cooking) among female survivors may replace time spent in SED as compared to males.
Physical characteristics at baseline such as fitness and body fat were significantly worse among class 3 participants (increasing SED over 12-months) compared to the other classes. Previous research using NHANES 2003–2004 data examined the potential association between low cardiorespiratory fitness and SED among young (mean age = 22.4 ± 10.3 years) adults. Results suggested that low fitness may mediate the risk of SED among adults [22]. Specifically, males with low fitness spent approximately 36 more minutes in SED compared to more fit males; similar trends were seen among women [22]. Our findings (low fitness is associated with high SED over 1 year) is consistent with those of healthy, young adults. While the association with low fitness and SED exists among young adults, more research is necessary to further understand this relationship among CRC survivors who tend to be older (mean age in this sample was 57.3 years).
Secondly, higher body fat has been associated with high SED among older [23] and healthy [24, 25] adults. Specifically, among cancer survivors, SED was significantly associated with adiposity among breast cancer survivors [26]. Conversely, no significant relationship was seen between SED and adiposity among prostate cancer survivors [27]. Our data show members of class 3 (increasing SED) had significantly higher body fat at baseline compared to the other classes. Interestingly, class 3 participants had the lowest SED at baseline (but did increase over time) among the other classes. Due to the small sample size and differing results from prior research based on gender (SED was associated with fat mass among female survivors [breast] and not male survivors [prostate]), this result should be considered with caution. However, we can speculate that the high body fat in addition to low fitness played a key role in causing an increase in SED over time.
Among class 2 (low, sustained SED), a significantly better mood was reported at baseline as compared to the other classes. Overall, among CRC survivors, no association has been seen between psychosocial health outcomes (i.e., depression, anxiety, and satisfaction with life) and SED (including overall SED or SED accumulated in 30-min bouts) [28]. To the best of our knowledge, mood and SED have not been examined among CRC survivors. However, among young adults, worsened mood was reported with high levels of SED following a 1-week sedentary induced environment [29]. Members of class 2 (low, sustained SED) had low levels of SED at baseline; therefore, they most likely participated in higher levels of light-or moderate-intensity PA, thus improving their mood. Overall, more longitudinal research is necessary to further understand the relationship of mood and SED over time among CRC survivors.
Class 3 (increased SED over time) reported greater use of cognitive processes at baseline. To the best of our knowledge, limited research exists to help explain the relationship between higher cognitive processes as a predictor of SED over time among CRC survivors. Due to the small sample size in addition to the fact that this study did not assess cognitive processes for SED, these results should be taken with caution. More research is necessary to understand the possible association of cognitive processes and SED among cancer survivors and healthy adults.
There are several limitations to this research. The small sample size (n = 46) limits the generalizability of the study sample. Additionally, majority of participants were well-educated and Non-Hispanic White. Although an objective assessment, the CSA monitor was only worn for 3 days (including at least one-weekend day). Data collection from additional days (e.g., 7 days) can improve the assessment of SED. Furthermore, the authors recognize the limitation of using the assessments of self-efficacy and processes of change which have been developed for PA, not SED. Transtheoretical model constructs for SED have been validated among college students [30]; however, these measures were not validated prior to the study’s inception. This study has several strengths that should be highlighted. Firstly, a longitudinal study design is an advantage as a majority of the prior work has been cross-sectional [10]. Previous work has examined the association of SED with characteristics such as gender among cancer survivors. Participants also completed submaximal fitness testing and body fat measures; the use of these measures can add to the literature to further describe characteristics associated with SED among CRC survivors.
In conclusion, among CRC survivors, four classes were identified based on objectively measured SED over a 12-month duration. A variety of characteristics arose within each class such as being male was associated with high, sustained SED over a 12-month duration. In addition, having a better mood at baseline were associated with low, sustained SED, while poor fitness and increased body fat were associated with increasing SED over time. Recommendations for future research include obtaining objective SED data for at least 1 week to increase accuracy of SED measurement and using validated questionnaires exploring motivational variables relevant to SED (e.g., SED-specific self-efficacy and processes of change). While more research is necessary, these predictors of SED may help healthcare providers predict future sedentary lifestyles among CRC survivors. Finally, consistent with the literature [9, 31, 32], there were no intervention (group assignment) effects on SED suggesting that interventions targeting SED are needed.
References
Ekelund U, Steene-Johannessen J, Brown WJ, Fagerland MW, Owen N, Powell KE, Bauman A, Lee IM, Lancet Physical Activity series 2 Executive C, Lancet Sedentary Behaviour Working G (2016) Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet 388(10051):1302–1310. https://doi.org/10.1016/S0140-6736(16)30370-1
Biswas A, Oh PI, Faulkner GE, Bajaj RR, Silver MA, Mitchell MS, Alter DA (2015) Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis. Ann Intern Med 162(2):123–132. https://doi.org/10.7326/M14-1651
Chau JY, Grunseit AC, Chey T, Stamatakis E, Brown WJ, Matthews CE, Bauman AE, van der Ploeg HP (2013) Daily sitting time and all-cause mortality: a meta-analysis. PLoS One 8(11):e80000. https://doi.org/10.1371/journal.pone.0080000
Grontved A, Hu FB (2011) Television viewing and risk of type 2 diabetes, cardiovascular disease, and all-cause mortality: a meta-analysis. JAMA 305(23):2448–2455. https://doi.org/10.1001/jama.2011.812
Kushi LH, Doyle C, McCullough M, Rock CL, Demark-Wahnefried W, Bandera EV, Gapstur S, Patel AV, Andrews K, Gansler T, American Cancer Society N, Physical Activity Guidelines Advisory C (2012) American Cancer Society guidelines on nutrition and physical activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity. CA Cancer J Clin 62(1):30–67. https://doi.org/10.3322/caac.20140
Lynch BM (2010) Sedentary behavior and cancer: a systematic review of the literature and proposed biological mechanisms. Cancer Epidemiol Biomark Prev 19(11):2691–2709. https://doi.org/10.1158/1055-9965.EPI-10-0815
Lynch BM, Boyle T, Winkler E, Occleston J, Courneya KS, Vallance JK (2016) Patterns and correlates of accelerometer-assessed physical activity and sedentary time among colon cancer survivors. Cancer Causes Control 27(1):59–68. https://doi.org/10.1007/s10552-015-0683-4
Lynch BM, Dunstan DW, Vallance JK, Owen N (2013) Don’t take cancer sitting down: a new survivorship research agenda. Cancer 119(11):1928–1935. https://doi.org/10.1002/cncr.28028
Lynch BM, Courneya KS, Sethi P, Patrao TA, Hawkes AL (2014) A randomized controlled trial of a multiple health behavior change intervention delivered to colorectal cancer survivors: effects on sedentary behavior. Cancer 120(17):2665–2672. https://doi.org/10.1002/cncr.28773
Prince SA, Reed JL, McFetridge C, Tremblay MS, Reid RD (2017) Correlates of sedentary behaviour in adults: a systematic review. Obes Rev 18(8):915–935. https://doi.org/10.1111/obr.12529
Pinto BM, Papandonatos GD, Goldstein MG, Marcus BH, Farrell N (2013) Home-based physical activity intervention for colorectal cancer survivors. Psychooncology 22(1):54–64. https://doi.org/10.1002/pon.2047
Winningham M (1993) Developing the symptom activity 27: an instrument to evaluate perception of symptom effects on activity. Oncol Nurs Forum 20:330
Freedson PS, Melanson E, Sirard J (1998) Calibration of the computer science and applications, Inc. accelerometer. Med Sci Sports Exerc 30(5):777–781
Melanson EL Jr, Freedson PS (1995) Validity of the computer science and applications, Inc. (CSA) activity monitor. Med Sci Sports Exerc 27(6):934–940
Pober DM, Freedson PS, Kline GM, McInnis KJ, Rippe JM (2002) Development and validation of a one-mile treadmill walk test to predict peak oxygen uptake in healthy adults ages 40 to 79 years. Can J Appl Physiol 27(6):575–589
Widrick J, Ward A, Ebbeling C, Clemente E, Rippe JM (1992) Treadmill validation of an over-ground walking test to predict peak oxygen consumption. Eur J Appl Physiol Occup Physiol 64(4):304–308
Roubenoff R, Baumgartner RN, Harris TB, Dallal GE, Hannan MT, Economos CD, Stauber PM, Wilson PW, Kiel DP (1997) Application of bioelectrical impedance analysis to elderly populations. J Gerontol A Biol Sci Med Sci 52(3):M129–M136
McNair DM, Lorr M, Droppleman LF (1971) Manual for the profile of mood states. Educational and Industrial Testing Services, San Diego
Marcus BH, Selby VC, Niaura RS, Rossi JS (1992) Self-efficacy and the stages of exercise behavior change. Res Q Exerc Sport 63(1):60–66. https://doi.org/10.1080/02701367.1992.10607557
Marcus BH, Rossi JS, Selby VC, Niaura RS, Abrams DB (1992) The stages and processes of exercise adoption and maintenance in a worksite sample. Health Psychol 11(6):386–395
Parry C, Kent EE, Mariotto AB, Alfano CM, Rowland JH (2011) Cancer survivors: a booming population. Cancer Epidemiol Biomark Prev 20(10):1996–2005. https://doi.org/10.1158/1055-9965.EPI-11-0729
Kulinski JP, Khera A, Ayers CR, Das SR, de Lemos JA, Blair SN, Berry JD (2014) Association between cardiorespiratory fitness and accelerometer-derived physical activity and sedentary time in the general population. Mayo Clin Proc 89(8):1063–1071. https://doi.org/10.1016/j.mayocp.2014.04.019
Swartz AM, Tarima S, Miller NE, Hart TL, Grimm EK, Rote AE, Strath SJ (2012) Prediction of body fat in older adults by time spent in sedentary behavior. J Aging Phys Act 20(3):332–344
Mun J, Kim Y, Farnsworth JL, Suh S, Kang M (2017) Association between objectively measured sedentary behavior and a criterion measure of obesity among adults. Am J Hum Biol 30. https://doi.org/10.1002/ajhb.23080
Myers A, Gibbons C, Finlayson G, Blundell J (2017) Associations among sedentary and active behaviours, body fat and appetite dysregulation: investigating the myth of physical inactivity and obesity. Br J Sports Med 51(21):1540–1544. https://doi.org/10.1136/bjsports-2015-095640
Lynch BM, Dunstan DW, Healy GN, Winkler E, Eakin E, Owen N (2010) Objectively measured physical activity and sedentary time of breast cancer survivors, and associations with adiposity: findings from NHANES (2003-2006). Cancer Causes Control 21(2):283–288. https://doi.org/10.1007/s10552-009-9460-6
Lynch BM, Dunstan DW, Winkler E, Healy GN, Eakin E, Owen N (2011) Objectively assessed physical activity, sedentary time and waist circumference among prostate cancer survivors: findings from the National Health and nutrition examination survey (2003-2006). Eur J Cancer Care (Engl) 20(4):514–519. https://doi.org/10.1111/j.1365-2354.2010.01205.x. ECC1205 [pii]
Vallance JK, Boyle T, Courneya KS, Lynch BM (2015) Accelerometer-assessed physical activity and sedentary time among colon cancer survivors: associations with psychological health outcomes. J Cancer Surviv 9(3):404–411. https://doi.org/10.1007/s11764-014-0409-8
Edwards MK, Loprinzi PD (2016) Effects of a sedentary behavior-inducing randomized controlled intervention on depression and mood profile in active young adults. Mayo Clin Proc 91(8):984–998. https://doi.org/10.1016/j.mayocp.2016.03.021
Han H, Gabriel KP, Kohl HW (2015) Evaluations of validity and reliability of a transtheoretical model for sedentary behavior among college students. Am J Health Behav 39(5):601–609. https://doi.org/10.5993/AJHB.39.5.2
Pinto B, Dunsiger S, Stein K (2017) Does a peer-led exercise intervention affect sedentary behavior among breast cancer survivors? Psychooncology 26(11):1907–1913. https://doi.org/10.1002/pon.4255
Chau JY, der Ploeg HP, van Uffelen JG, Wong J, Riphagen I, Healy GN, Gilson ND, Dunstan DW, Bauman AE, Owen N, Brown WJ (2010) Are workplace interventions to reduce sitting effective? A systematic review. Prev Med 51(5):352–356. https://doi.org/10.1016/j.ypmed.2010.08.012
Acknowledgments
The study was supported by the National Cancer Institute (CA 101770).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Kindred, M.M., Pinto, B.M. & Dunsiger, S.I. Predictors of sedentary behavior among colorectal survivors. Support Care Cancer 27, 2049–2056 (2019). https://doi.org/10.1007/s00520-018-4452-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-018-4452-2