Abstract
Purpose
Following head and neck cancer (HNC) treatment, individuals experience an array of side effects which can impact on physical, emotional, and practical aspects of their lives. Responsive, supportive rehabilitation services are therefore essential to address ongoing survivorship needs. This study examined the nature of patient-reported goals from acute to long-term post-treatment, to inform design/delivery of future rehabilitation services.
Methods
Using a cross-sectional cohort design, 91 patients between 2 weeks and 5 years of post non-surgical HNC treatment (acute n = 29; sub-acute n = 28; long-term n = 34), provided their top four rehabilitation goals considering any aspect of their lives. Content analysis was used to categorise responses at each time point.
Results
Three core categories of patient goals were identified relating to: (1) treatment side effects (TSE), (2) overall health (OH), and (3) living life (LL). TSE goals were a priority during the acute and sub-acute phases, with less focus long-term. LL goals were prevalent across all time points, though increased in the long-term. Approximately a third of all goals at each time point related to OH.
Conclusions
A variety of rehabilitation goals were identified, and the focus shifted over time. These data highlight the importance of changing the focus of rehabilitation as patients’ priorities vary over time. Early multidisciplinary care from allied health services is crucial to provide support with managing side effects and returning to daily activities. In the long-term, greater input from services to address health, nutrition, leisure, and fitness goals may be more beneficial.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Survival rates following head and neck cancer (HNC) treatment are improving due to a number of factors including new treatment techniques and a demographic profile shift to younger patients with HPV-mediated disease, leading to improved locoregional control [1,2,3]. Unfortunately for these survivors, an extensive body of research confirms that patients with HNC who are treated with (chemo)radiotherapy [(C)RT] may experience significant symptom burden and may have unmet support needs relating to these symptoms [4,5,6,7,8,9], consequently impacting on their quality of life [10]. Quantitative studies have highlighted the prevalence of diverse symptoms, such as mucositis, that resolve during the acute phase [11, 12], whilst others, such as xerostomia and dysgeusia, persist in the long-term and can continually impact on daily functions such as swallowing [7, 13,14,15,16]. Systemic problems, such as fatigue and deconditioning, as well as psychosocial issues including anxiety, depression, and fear of recurrence are also common for this population [6]. Additionally, multiple other challenges exist after HNC treatment, including regaining normality, socialising, interpersonal relationships, and financial distress [17, 18].
Such diverse symptoms and their potential pervasive impact on patients’ lives following (C)RT treatment highlight the importance for HNC services to provide ongoing, holistic support for this patient population. In the general cancer literature, rehabilitation services have been identified as a crucial component to patient care to address common, unmet physical, practical, and psychological needs [19, 20], and improve patients’ quality of life [21].
Although rehabilitation services are comparatively well established for patients with chronic disease conditions (e.g. post stroke), long-term rehabilitation services may not be available to all cancer patients after treatment, despite the known benefits [22, 23]. Recently, to address this clinical gap, cancer centres are implementing models of survivorship care. This care emphasises providing support beyond being disease-free, to include ongoing management with recovery, general health, and wellbeing across all time points after treatment completion. Cancer Australia recently identified ‘consumer involvement in person-centred care’ as a key principle of survivorship, in order to empower patients and support their self-management based on personal priorities, to ultimately live a life they desire [24].
To guide a more patient-centred approach to HNC care, researchers have begun to look beyond the prevalence of side effects and specifically investigate the priority of these concerns or potential rehabilitation goals they wish to target. Collaborative goal setting has been identified as a crucial component of survivorship services [31], in order to increase success with self-management, adherence to clinical recommendations, and rehabilitative outcomes [32]. McEwen et al. recently interviewed a small group of survivors (n = 8), family members (n = 3), and clinicians (n = 29) about the range of rehabilitation needs for patients [23], identifying a diverse range of goals patients wanted to work on, and barriers to accessing HNC rehabilitation services. However, the generalisability of the data was limited by the small number of patients, the multi-modal treatment patients underwent, as well as no clarification of what time post-treatment the patients were interviewed. Other larger studies with diverse cohorts have asked patients to rank their top concerns from concise lists of common issues post-treatment [25,26,27,28]. Whilst the information obtained from such studies is valuable for understanding patients’ priorities, this work employed a restricted list of pre-set issues for patients to choose from, often with a focus on physical symptoms [25,26,27, 29, 30]. Hence, further investigation is required in a large, single-modality treatment group to identify the specific nature of HNC patient goals along the post-treatment continuum of care.
Evidence supports that following (C)RT, a number of acute toxicities persist, which can continue to impact patient experience of survivorship in the long-term [7, 33, 34]. Equally, late-onset issues may develop for which patients require assessment, support, and intervention [6]. Patient adjustment to chronic symptoms may also impact rehabilitation goals as time progresses post-treatment [35, 36]. Ultimately, understanding the nature, timing, and progression of patient-generated goals will contribute to the development of HNC survivorship services that are responsive to patients’ needs and ensure that patients’ priorities are being met. Hence, the aims of the current study were to (a) determine the nature and priority of patients’ rehabilitation goals following non-surgical treatment for HNC and (b) explore the progression of goals across the acute, sub-acute, and long-term phases post-treatment.
Materials and methods
Design
This study uses a cross-sectional cohort design.
Participants
Patients who were 2 weeks to 5 years post completion of (C)RT treatment for HNC were recruited for the current study at two tertiary hospitals in Australia (The Prince of Wales Hospital, Sydney, and The Princess Alexandra Hospital, Brisbane). Patients were excluded if they had received surgery as part of their treatment, were treated for a recurrence, or with palliative intent. As part of standard clinical services at each hospital, all patients were routinely seen by a speech pathologist and dietitian during treatment and advised regarding standard prophylactic swallowing exercises, maintaining oral intake, and focussing on weight maintenance and a high-energy/high-protein diet. Within the first 3 months of treatment completion, all participants were reviewed by speech pathology and dietetic services to assess and manage ongoing concerns regarding swallowing and nutrition, with ongoing support provided as required thereafter. Participants of the current study did not complete structured post-treatment therapy intervention for swallowing or nutrition.
Data collection
Potential participants were approached during their routine outpatient follow-up consultations between September 2016 and August 2017 and informed consent was obtained from all individual participants included in the study (POWH HREC no: 10/131; PAH HREC no: HREC/11/QPAH/367). Once-off, cross-sectional data was collected during in-person discussions with a researcher not otherwise involved in their care. Irrespective of their current or previous exposure to rehabilitation health services, all participants were asked to identify their top four goals that they would like to work on in their rehabilitation following treatment, considering all aspects of their lives (i.e. physical, emotional, social, work/family life, spiritual). The researcher was blinded to whether the patient was currently or had previously received specific support or intervention regarding their rehabilitation. If patients were unable to independently generate goals, participants were provided a list of 31 stimulus items (previously published rehabilitation domains from McEwan et al. 2016 [23]) to promote goal setting and prioritisation. Responses were written verbatim, with participants often summarising their goals into a single sentence. Extra field notes were recorded, when necessary, to add context to the goals and clarify the meaning and intent to assist later analysis.
Analysis
Demographics were collected for all participants. Participants were classified into three groups based on time post-treatment: acute (2 weeks to 3 months post-treatment), sub-acute (4 months to 12 months post-treatment), or long-term (13 months to 5 years post-treatment). All goals with the respective time post-treatment were collated into a single master list.
Content analysis was used to code the goals, as per Graneheim and Lundman (2004). Sentence responses from each goal constituted the ‘meaning units’ for analysis purposes [37]. Two clinical researchers (MB and BC) first read and discussed each meaning unit, along with the field notes, to generate interpretations of the responses. From this discussion, units with common content and words were assigned to preliminary sub-categories (regardless of time post-treatment). Meaning units which pertained to multiple sub-categories were initially multi-coded to all relevant sub-categories so as not to falsely eliminate a meaning unit. An initial consensus meeting with an additional two expert clinical researchers then reviewed the sub-category framework, and a second round of sub-categorisation by MB was completed. A second consensus meeting was then conducted to review the refined sub-categories. Finally, grouping of sub-categories into broad categories to generate overarching commonalities was completed, which were exhaustive and mutually exclusive [37].
Descriptive analysis was completed to investigate the percent of goals reported per category and sub-category for the whole cohort, as well as by percent of goals reported in each category across the three time points. Patients who reported goals as ‘nil’ were also tabulated across time points. A Fisher’s exact test was used to explore differences in the proportion of goals reported at each time point.
Results
Participants
The study recruited 91 participants, and demographics are reported in Table 1. The majority had an oropharyngeal primary site and received adjuvant chemotherapy. Of these, 29 were in the acute phase, 28 were in the sub-acute phase, and 34 were long-term post-treatment. From the 91 patients, 313 goals were generated. Only 28 (31%) patients generated less than four goals, with the majority of these being patients who were in the long-term (n = 13) and sub-acute (n = 11) phases.
Content analysis: three categories
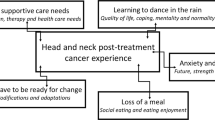
Following content analysis, three broad categories were identified: (1) treatment side effects (TSE), (2) overall health (OH), and (3) live life (LL).
Treatment side effects
Goals which referred to improving or modifying current physical functions or health status which were directly altered as a result of (C)RT treatment effects were categorised within the TSE category (Table 2). This category captured goals referring to direct, localised oropharyngeal side effects from treatment (i.e. dry mouth, pain on swallowing) as well as indirect, systemic effects (i.e. reduced muscle mass leading to deconditioning, fatigue). Participants often referred to the desire to return to a specific physical way of functioning before their treatment, or to eliminate/reduce the impact of the side effect. These goals were further divided into four sub-categories: (1) localised side effects, (2) systemic side effects, (3) pain/inflammation, and (4) communication. Within each of these sub-categories, more specific side effects are described in Table 2.
Overall health
Goals which referred to participants’ physical, emotional, and general health were categorised within the OH category (Table 3). The goals allocated to this category were derived from comments regarding staying healthy or improving general health (including mental health), without specific reference to HNC or its treatment effects. Overall, goals in this category included content which expressed the participants’ desires to live healthier lives or support other people with cancer to be healthy. The OH category was further divided into five sub-categories: (1) general wellbeing; (2) exercise and fitness; (3) emotional wellbeing; (4) other health concerns; and (5) health advocacy.
Live life
Participants which reported goals referring to a desire to improve lifestyle factors, including financial wellbeing, relationship development, and returning to work, were categorised within the LL category (Table 4). Goals within this category referred to wanting to appreciate and enjoy life more, with frequent comments mentioning ‘life may be short’. These goals were further divided into four sub-categories: (1) leisure and recreation; (2) work and financial wellbeing; (3) interpersonal relationships; and (4) social wellbeing.
Analysis
The percent of goals which fell into each category was calculated. Of the total 313 goals, 27% were in the TSE, 35% in the OH, and 38% in the LL categories. Within each category, the number and proportion of goals in each sub-category were also calculated for the entire cohort (regardless of time point; Tables 2–4).
The percent of goals within the three categories at each time point are displayed in Fig. 1. Most of the goals reported within the TSE category were during the acute and sub-acute phases, and reduced considerably in the long-term phase. Goals within the LL category were most often reported during the long-term phase. In contrast, the goals reported in the OH category had fairly even proportions over time. Analysis revealed a significant difference in proportions of goals reported between acute and long-term (p < 0.001), and sub-acute and long-term time points (p < 0.001), identifying that the dominant nature of the rehabilitation goals changed over time. Furthermore, the manner in which patients phrased the goals appeared to change over time. More goals during the acute and sub-acute phase were related to ‘returning to’ function/activities they did prior to the cancer diagnosis, whilst more goals in the long-term were related to ‘improving’ function/activities, but not in comparison to their previous way of life. The top five sub-categories of goals for each time point (distinct from the broad category) were also calculated and are displayed in Table 5.
Discussion
This study investigated the top rehabilitation goals of patients following non-surgical treatment for HNC, and how these goals varied across the acute, sub-acute, and long-term phases post-treatment. In the entire cross-sectional cohort, there was a large diversity in goals discussed, which were ultimately grouped into three categories of ‘treatment side effects’, ‘overall health’, and ‘living life’. The diversity in goals was similar to outcomes reported by McEwen et al. (2016), who found goals in their group of 8 survivors spanned across 17 domains ranging from side effect management (swallowing/eating, dry mouth) to psychosocial or emotional needs (social isolation, psychological trauma, and role functioning) [23]. The largest proportion of the goals across the whole cohort in the current study related to ‘living life’, in which participants described wanting to focus on returning to/maintaining leisure activities, ensuring financial security, and working on personal relationships. When examining specific time points post-treatment, significant differences were observed in the nature of goals, with the largest proportion of goals focused on improving function and/or reducing ‘treatment side effects’ in the short-term, whilst a significant increase in participants focusing on ‘living life’ occurred in the long-term. There was minimal difference in the number of goals within the OH category, indicating staying healthy and being disease-free were maintained as priority goals regardless of the time post-treatment.
It is well-documented that treatment toxicities are most prevalent within the first 6–12 months following (C)RT, with side effects such as odynophagia, xerostomia, and dysgeusia highly prevalent and often impacting on oral intake [7, 34]. Supporting this, qualitative studies have highlighted the considerable symptom burden many patients associate with eating and swallowing, and the impacts on social dining and needing to make practical adjustments during meals [17, 18, 38]. Additionally, the studies which examined patients’ top concerns early post-treatment also found the most important issues included physical functioning such as pain, swallowing, saliva, chewing, dental health, and taste [5, 27, 28]. Hence, it was not unexpected that in the current study the most prevalent rehabilitative goals during the acute and sub-acute phases were related to improving ‘localised side effects’.
However, the finding that was less expected was the proportion (one third) of goals during the acute/sub-acute phases in the LL category, specifically related to ‘leisure’. This finding highlights that even in the early stages post-treatment, many patients wish to focus beyond treatment side effects by prioritising goals which increase their participation in regular activities and enjoying life. Existing qualitative studies which have adopted an open interview approach have also captured this focus on broader life issues, including returning to work, tiredness, social functioning, improving interpersonal relationships, and regaining normality during the first year after treatment [17, 18, 39]. In contrast, studies which used a set ranking methodology found returning to daily activities and recreation were less prevalent [5, 27]. Most similar to the current study’s methodology, McEwen et al. (2016) also identified 3 of the 17 categories related to the LL category defined in the current data [23]. Unfortunately, as the exact time post-treatment of the participants in that study was not reported, it is difficult to more fully compare findings.
A key finding of the current study was the significant difference in the proportion of goals per category based on the time post-treatment. Significantly less goals related to side effects were found after 12 months, with a greater emphasis on leisure, overall health, financial wellbeing, and interpersonal relationships in the long-term phase. This is not surprising given the anticipated progression of acute side effects resolving within the first year following (C)RT [7]. Although no prior studies have specifically analysed rehabilitative goals across time points, four studies which asked patients to rank their priorities or concerns post-treatment have revealed temporal changes, but with differing findings. These studies found issues with side effects often remained as high priorities that did not significantly change over time [5, 25, 27, 28]. However, large variations were found in the ranking of other issues (i.e. social, emotional, practical issues), including returning to activities/daily tasks was a consistently high or increasing priority over time for two of the studies [5, 25], but decreased or remained a low priority in two studies [27, 28]. Variations were also found with either increasing [5, 25] or decreasing [27, 28] prioritisation of anxiety/emotional issues over time, as well as with minimal [5, 27] versus increasing importance on recreation [25]. The variations found between these studies as well as in comparison to the current study’s findings may be due to the heterogeneous cohorts analysed. In addition, using varied and limited sets of common items assigned to participants to rank could potentially emphasise concerns with side effects and restrict patients’ ability to generate their own concerns. As the current study encouraged generation of open-ended rehabilitation goals at specific time points, and only explored non-surgical patients, the current data may be expected to differ.
The significant difference in rehabilitation goals from acute/sub-acute to long-term phases found in the current study potentially reflects the recovery pattern of short-term side effects following treatment. However, differing rehabilitation priorities may also reflect an adjustment to more permanent life changes. Patients were noted to make anecdotal statements which suggested having less concern for chronic side effects (i.e. ‘I don’t really think about [swallowing] anymore’; ‘My dry mouth won’t get better; there are worse problems to have’). Although not formally analysed, there appeared to be a shift over time in the current data regarding how participants phrased their goals. Acute goals were phrased based on ‘returning to normal’, and comparing targets to their pre-treatment functioning, whilst in the long-term, they were based on ‘improving’ their situation without reference to pre-treatment levels. These phrasing patterns parallel the concept of adjustment, in which new ways of coping with ongoing symptoms can be found, and values redefined and reprioritised over time [40]. Emerging literature specific to the HNC population has hypothesised an adjustment to long-term dysphagia [7, 36], with patients noted to downplay challenges with side effects whilst finding enjoyment in meals [35]. The potential adjustment to side effects over time highlights the importance of looking beyond persisting symptoms and generating patient-centred goals to guide rehabilitative services across all phases of survivorship. A new assessment tool, the Brief Rehabilitation Assessment for Survivors of Head-and-Neck Cancer (BRASH), [41] specifically probes items of potential concern to patients, and subsequently whether patients want to then target this concern during rehabilitation. In the future, utilising tools such as the BRASH to differentiate between patient concerns and goals will be beneficial for supporting goal setting with this population.
The collection of cross-sectional data over a range of time points post-treatment limits exploration of the issue of individual patient adjustment over time. Thus, future studies should examine the changing nature of rehabilitation goals in a longitudinal cohort to fully explore this issue. Furthermore, the recognised pattern of different patient phrasing of rehabilitation goals needs to be explored further using qualitative methodology to determine whether this is a reflection of adjustment to chronicity, or an artefact of data collection in the current study. Additionally, identifying the impact of patient characteristics (i.e. T stage, tube feeding) on goals reported was beyond the scope of this study, however would provide valuable insight for rehabilitation services, and should be included in multivariate analysis in future studies. Although a simple methodology was used in the current paper asking patients to self-generate their top goals, it is recognised that tools such as the BRASH and others, e.g. The Cancer Survivors’ Unmet Needs Measure [42] could also be useful within a clinical setting to help guide rehabilitation goal planning.
The current study found a wide variety of patient-generated rehabilitation goals following treatment for HNC, which shifted over time from a focus on treatment side effects to primarily life and health goals after 12 months post-treatment. These findings highlight the need to give patients the opportunity to self-determine their own rehabilitation priorities at multiple phases after treatment, in order to guide the involvement of relevant multidisciplinary team members across their continuum of care. During the acute and sub-acute phases, patients’ goals reflected the need for early speech pathology, dietetics, and physiotherapy rehabilitation for managing treatment side effects and deconditioning, occupational therapy for resuming daily activities such as returning to work and recreation, and psychology support for adjustment and reconnecting with communities. However, after a 12-month survivorship, specialists who focus on general wellness—such as exercise, nutrition, and mental health staff—may have a greater role to play in supporting patients’ overall health and ability to enjoy life in the long-term. Considering that rehabilitation goals may change over time, routine revision of goals with patients post (C)RT is necessary to ensure rehabilitation services accurately reflect current patient preferences and needs.
References
Dirix P, Nuyts S (2010) Evidence-based organ-sparing radiotherapy in head and neck cancer. Lancet Oncol 11(1):85–91. https://doi.org/10.1016/S1470-2045(09)70231-1
Ang KK, Harris J, Wheeler R, Weber R, Rosenthal DI, Nguyen-Tân PF, Westra WH, Chung CH, Jordan RC, Lu C, Kim H, Axelrod R, Silverman CC, Redmond KP, Gillison ML (2010) Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med 363(1):24–35. https://doi.org/10.1056/NEJMoa0912217
Beadle BM, Liao K-P, Elting LS, Buchholz TA, Ang KK, Garden AS, Guadagnolo BA (2014) Improved survival using intensity-modulated radiation therapy in head and neck cancers: a SEER-Medicare analysis. Cancer 120(5):702–710. https://doi.org/10.1002/cncr.28372
Miller MC, Shuman AG, for the American H, Neck Society’s Committee on S (2016) Survivorship in head and neck cancer: a primer. JAMA Otolaryngo Head Neck Surg 142(10):1002–1008. https://doi.org/10.1001/jamaoto.2016.1615
Ghazali N, Roe B, Lowe D, Rogers SN (2015) Patients concerns inventory highlights perceived needs and concerns in head and neck cancer survivors and its impact on health-related quality of life. Br J Oral Maxillofac Surg 53(4):371–379. https://doi.org/10.1016/j.bjoms.2015.01.022
Cohen EEW, LaMonte SJ, Erb NL, Beckman KL, Sadeghi N, Hutcheson KA, Stubblefield MD, Abbott DM, Fisher PS, Stein KD, Lyman GH, Pratt-Chapman ML (2016) American Cancer Society head and neck cancer survivorship care guideline. CA Cancer J Clin 66(3):203–239. https://doi.org/10.3322/caac.21343
Barnhart MK, Robinson RA, Simms VA, Ward EC, Cartmill B, Chandler SJ, Smee RI (2018) Treatment toxicities and their impact on oral intake following non-surgical management for head and neck cancer: a 3-year longitudinal study. Support Care Cancer 26:2341–2351. https://doi.org/10.1007/s00520-018-4076-6
Ringash J, Bernstein LJ, Devins G, Dunphy C, Giuliani M, Martino R, McEwen S (2018) Head and neck cancer survivorship: learning the needs, meeting the needs. Semin Radiat Oncol 28(1):64–74. https://doi.org/10.1016/j.semradonc.2017.08.008
Giuliani M, McQuestion M, Jones J, Papadakos J, Le LW, Alkazaz N, Cheng T, Waldron J, Catton P, Ringash J (2016) Prevalence and nature of survivorship needs in patients with head and neck cancer. Head Neck 38(7):1097–1103. https://doi.org/10.1002/hed.24411
Bressan V, Bagnasco A, Aleo G, Catania G, Zanini MP, Timmins F, Sasso L (2017) The life experience of nutrition impact symptoms during treatment for head and neck cancer patients: a systematic review and meta-synthesis. Support Care Cancer 25(5):1699–1712. https://doi.org/10.1007/s00520-017-3618-7
Murphy BA, Beaumont JL, Isitt J, Garden AS, Gwede CK, Trotti AM, Meredith RF, Epstein JB, Le QT, Brizel DM, Bellm LA, Wells N, Cella D (2009) Mucositis-related morbidity and resource utilization in head and neck cancer patients receiving radiation therapy with or without chemotherapy. J Pain Symptom Manag 38(4):522–532. https://doi.org/10.1016/j.jpainsymman.2008.12.004
Pauloski, Rademaker AW, Logemann JA, Lundy D, Bernstein M, McBreen C, Santa D, Campanelli A, Kelchner L, Klaben B, Discekici-Harris M (2011) Relation of mucous membrane alterations to oral intake during the first year after treatment for head and neck cancer. Head Neck 33(6):774–779. https://doi.org/10.1002/hed.21542
McLaughlin LRNP (2013) Taste dysfunction in head and neck cancer survivors. Oncol Nurs Forum 40(1):E4–E13
Kraaijenga SC, van der Molen L, Jacobi I, Hamming-Vrieze O, Hilgers FM, van den Brekel MM (2015) Prospective clinical study on long-term swallowing function and voice quality in advanced head and neck cancer patients treated with concurrent chemoradiotherapy and preventive swallowing exercises. Eur Arch Otorhinolaryngol 272(11):3521–3531. https://doi.org/10.1007/s00405-014-3379-6
Vainshtein JM, Samuels S, Tao Y, Lyden T, Haxer M, Spector M, Schipper M, Eisbruch A (2016) Impact of xerostomia on dysphagia after chemotherapy–intensity-modulated radiotherapy for oropharyngeal cancer: prospective longitudinal study. Head Neck 38(S1):E1605–E1612. https://doi.org/10.1002/hed.24286
Bressan V, Stevanin S, Bianchi M, Aleo G, Bagnasco A, Sasso L (2016) The effects of swallowing disorders, dysgeusia, oral mucositis and xerostomia on nutritional status, oral intake and weight loss in head and neck cancer patients: a systematic review. Cancer Treat Rev 45:105–119. https://doi.org/10.1016/j.ctrv.2016.03.006
Molassiotis A, Rogers M (2012) Symptom experience and regaining normality in the first year following a diagnosis of head and neck cancer: a qualitative longitudinal study. Palliat Support Care 10(3):197–204. https://doi.org/10.1017/S147895151200020X 10.1016/j.critrevonc.2006.07.005
Larsson M, Hedelin B, Athlin E (2007) Needing a hand to hold: lived experiences during the trajectory of care for patients with head and neck cancer treated with radiotherapy. Cancer Nurs 30(4):324–334. https://doi.org/10.1097/01.ncc.0000281722.56996.07
Holm LV, Hansen DG, Johansen C, Vedsted P, Larsen PV, Kragstrup J, Søndergaard J (2012) Participation in cancer rehabilitation and unmet needs: a population-based cohort study. Support Care Cancer 20(11):2913–2924. https://doi.org/10.1007/s00520-012-1420-0
Jefford M, Karahalios E, Pollard A, Baravelli C, Carey M, Franklin J, Aranda S, Schofield P (2008) Survivorship issues following treatment completion—results from focus groups with Australian cancer survivors and health professionals. J Cancer Surviv 2(1):20–32. https://doi.org/10.1007/s11764-008-0043-4
Passchier E, Stuiver MM, van der Molen L, Kerkhof SI, van den Brekel MW, Hilgers FJ (2016) Feasibility and impact of a dedicated multidisciplinary rehabilitation program on health-related quality of life in advanced head and neck cancer patients. Eur Arch Otorhinolaryngol 273(6):1577–1587. https://doi.org/10.1007/s00405-015-3648-z
Eades M, Murphy J, Carney S, Amdouni S, Lemoignan J, Jelowicki M (2013) Effect of an interdisciplinary rehabilitation program on quality of life in patients with head and neck cancer: review of clinical experience. Head Neck 35:343–349. https://doi.org/10.1002/hed.22972
McEwen S, Rodriguez AM, Martino R, Poon I, Dunphy C, Rios JN, Ringash J (2016) “I didn’t actually know there was such a thing as rehab”: survivor, family, and clinician perceptions of rehabilitation following treatment for head and neck cancer. Support Care Cancer 24(4):1449–1453. https://doi.org/10.1007/s00520-015-3021-1
Cancer Australia and Cancer Voices Australia (2011) National framework for consumer involvement in cancer control. Cancer Australia. ACT, Canberra
Tschiesner U, Sabariego C, Linseisen E, Becker S, Stier-Jarmer M, Cieza A, Harreus U (2013) Priorities of head and neck cancer patients: a patient survey based on the brief ICF core set for HNC. Eur Arch Otorhinolaryngol 270(12):3133–3142. https://doi.org/10.1007/s00405-013-2446-8
Kanatas A, Ghazali N, Lowe D, Udberg M, Heseltine J, O’Mahony E, Rogers SN (2013) Issues patients would like to discuss at their review consultation: variation by early and late stage oral, oropharyngeal and laryngeal subsites. Eur Arch Otorhinolaryngol 270(3):1067–1074. https://doi.org/10.1007/s00405-012-2092-6
Metcalfe CW, Lowe D, Rogers SN (2014) What patients consider important: temporal variations by early and late stage oral, oropharyngeal and laryngeal subsites. J Cranio-Maxillofac Surg 42(5):641–647. https://doi.org/10.1016/j.jcms.2013.09.008
Rogers SN, El-Sheikha J, Lowe D (2009) The development of a Patients Concerns Inventory (PCI) to help reveal patients concerns in the head and neck clinic. Oral Oncol 45(7):555–561. https://doi.org/10.1016/j.oraloncology.2008.09.004
Sharp HM, List M, MacCracken E, Stenson K, Stocking C, Siegler M (1999) Patients’ priorities among treatment effects in head and neck cancer: evaluation of a new assessment tool. Head Neck 21(6):538–546
Rogers SN, Laher SH, Overend L, Lowe D (2002) Importance-rating using the University of Washington Quality of Life questionnaire in patients treated by primary surgery for oral and oro-pharyngeal cancer. J Cranio-Maxillofac Surg 30(2):125–132. https://doi.org/10.1054/jcms.2001.0273
Clinical Oncology Society of Australia Model of Survivorship Care Working Group (2016) Model of survivorship care: critical components of cancer survivorship care in Australia position statement. Clinical Oncology Society of Australia
Bodenheimer T, Lorig K, Holman H, Grumbach K (2002) Patient self-management of chronic disease in primary care. JAMA 288(19):2469–2475
Cartmill B, Cornwell P, Ward E, Davidson W, Porceddu S (2012) Long-term functional outcomes and patient perspective following altered fractionation radiotherapy with concomitant boost for oropharyngeal cancer. Dysphagia 27(4):481–490. https://doi.org/10.1007/s00455-012-9394-0
Cooperstein E, Gilbert J, Epstein JB, Dietrich MS, Bond SM, Ridner SH, Wells N, Cmelak A, Murphy BA (2012) Vanderbilt head and neck symptom survey version 2.0: report of the development and initial testing of a subscale for assessment of oral health. Head Neck 34(6):797–804. https://doi.org/10.1002/hed.21816
Ganzer H, Rothpletz-Puglia P, Byham-Gray L, Murphy BA, Touger-Decker R (2015) The eating experience in long-term survivors of head and neck cancer: a mixed-methods study. Support Care Cancer 23(11):3257–3268. https://doi.org/10.1007/s00520-015-2730-9
Hutcheson KA, Lewin JS, Holsinger FC, Steinhaus G, Lisec A, Barringer DA, Lin HY, Villalobos S, Garden AS, Papadimitrakopoulou V, Kies MS (2014) Long-term functional and survival outcomes after induction chemotherapy and risk-based definitive therapy for locally advanced squamous cell carcinoma of the head and neck. Head Neck 36(4):474–480. https://doi.org/10.1002/hed.23330
Graneheim UH, Lundman B (2004) Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today 24(2):105–112. https://doi.org/10.1016/j.nedt.2003.10.001
Nund WEC, Scarinci NA, Cartmill B, Kuipers P, Porceddu SV (2014) The lived experience of dysphagia following non-surgical treatment for head and neck cancer. Int J Speech Lang Pathol 16(3):282–289. https://doi.org/10.3109/17549507.2013.861869
Semple CJ, Dunwoody L, George Kernohan W, McCaughan E, Sullivan K (2008) Changes and challenges to patients’ lifestyle patterns following treatment for head and neck cancer. J Adv Nurs 63(1):85–93. https://doi.org/10.1111/j.1365-2648.2008.04698.x
de Ridder D, Geenen R, Kuijer R, van Middendorp H (2008) Psychological adjustment to chronic disease. Lancet 372(9634):246–255. https://doi.org/10.1016/S0140-6736(08)61078-8
McEwen S, Dunphy C, Rios JN, Davis A, Jones J, Lam A, Poon I, Martino R, Ringash J (2017) Development and pre-testing of a rehabilitation planning consultation for head-and-neck cancer. 24(3):8. https://doi.org/10.3747/co.24.3529
Hodgkinson K, Butow P, Hunt GE et al (2007) The development and evaluation of a measure to assess cancer survivors’ unmet supportive care needs: the CaSUN (Cancer Survivors’ Unmet Needs measure). Psychooncology 16:796–804. https://doi.org/10.1002/pon.1137
Acknowledgements
The authors wish to thank the speech pathology department, research team, and multidisciplinary team at Prince of Wales Hospital and Princess Alexandra Hospital for their contributions and continued support to this project.
Funding
This project was funded by the Head and Neck Cancer Research Fund at Prince of Wales Hospital, Sydney, Australia.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author has been funded by the institution (Prince of Wales Hospital, Australia) where the research was conducted. The author has full control of all primary data and agrees to allow the journal to review the data if requested.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Barnhart, M.K., Ward, E.C., Cartmill, B. et al. Content analysis of rehabilitation goals for patients following non-surgical head and neck cancer treatment. Support Care Cancer 27, 639–647 (2019). https://doi.org/10.1007/s00520-018-4364-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-018-4364-1