Abstract
Background
Integration of oncology and palliative care (PC) should be the standard model of care for patients with advanced cancer. An expert panel developed criteria that constitute integration. This study determined whether the PC service within this Health Service, which is considered to be fully “integrated”, could be benchmarked against these criteria.
Methods
A survey was undertaken to determine the perceived level of integration of oncology and palliative care by all health care professionals (HCPs) within our cancer centre. An objective determination of integration was obtained from chart reviews of deceased patients. Integration was defined as >70% of all respondents answered “agree” or “strongly agree” to each indicator and >70% of patient charts supported each criteria.
Results
Thirty-four HCPs participated in the survey (response rate 69%). Over 90% were aware of the outpatient PC clinic, interdisciplinary and consultation team, PC senior leadership, and the acceptance of concurrent anticancer therapy. None of the other criteria met the 70% agreement mark but many respondents lacked the necessary knowledge to respond.
The chart review included 67 patients, 92% of whom were seen by the PC team prior to death. The median time from referral to death was 103 days (range 0–1347). The level of agreement across all criteria was below our predefined definition of integration.
Conclusion
The integration criteria relating to service delivery are medically focused and do not lend themselves to interdisciplinary review. The objective criteria can be audited and serve both as a benchmark and a basis for improvement activities.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Palliative care has been shown to improve quality of life, symptom control, and end-of-life care for patients suffering from advanced cancer [1, 2]. Costs of care are less where oncology and palliative care are integrated and survival may be prolonged [3, 4]. As a result, several professional oncological societies have stated that the integration of palliative and oncology care should be considered as standard care for patients with advanced cancer [5, 6]. A recent guideline by the American Society of Clinical Oncology strongly recommends that palliative and oncology care should be offered to all patients with advanced cancer as standard practice [7].
A clear and defined model of integration of oncology and palliative care does not exist. In an attempt to define relevant indicators of effective integration, Hui and colleagues conducted a systematic review [2]. They concluded that the definition of integration was heterogeneous, but were able to extract 38 relevant indicators from 101 publications. The indicators were classified into four categories—clinical, education, research, and administration—and analysed according to structure, process or outcome measures [8].
Following the documentation of these indicators, an International Consensus Panel (ICP) was formed that determined minor and major indicators for the integration of oncology and palliative care [9]. Forty-seven experts who were experienced and active physicians specializing in oncology or palliative care, who had published in the area, defined 13 major and 30 minor indicators after three rounds of a Delphi process. The international experts reached consensus with 88–100% agreement on the major criteria that include structure, process, outcome and education indicators. The authors emphasize the potential utility of these indicators for benchmarking, prioritization, quality improvements, and research.
The Supportive and Palliative Care service within Mater Health Services in Brisbane, Australia has been an integral part of the oncology department for more than 10 years. The palliative care team is interdisciplinary and includes physicians, nurses, and varied allied health professionals (psychologist, social workers, physiotherapists and occupational therapists, and a pastoral care service). In close collaboration, oncology and palliative care specialists co-manage both in-patients and out-patients with advanced cancer. The medical director of cancer services is an oncology trained palliative care physician. Communication and continuous education in palliative care and oncology is a mainstay of the oncology department.
Given the lack of data on integration at a site specific level, we sought to use the published indicators to assess formally the level of integration of oncology and palliative care at this centre.
The aim of this project was to test both the degree of perceived integration in our department and the appropriateness of the indicators.
Methods
Mater Health Services is a private not-for-profit organization that comprises a network of several hospitals, health centres, and a research institute delivering care to both public and private patients throughout Queensland, Australia. The Mater Cancer Care Centre (MCCC) is an ambulatory cancer centre within Mater Health that provides approximately 13,000 episodes of care (consultations and treatment) each year. It is supported by on-site private and public in-patient wards. A variety of solid and haematological cancers are managed, predominantly breast, gynaecological, lung, and colorectal malignancies. To determine if the MCCC provides an integrated oncology and palliative care service, according to the indicators reported by Hui and colleagues [9], a staff survey was distributed and a chart review undertaken.
The project was approved by the Mater Health Services Human Research Ethics Committee (HREC/15/MHS/86).
Part A. The survey contained 24 questions based on the major and minor indicators of clinical structure, clinical processes, education and research relating to the service as a whole, and included a request for demographic data. Respondents were asked to respond to all indicators on a 5-point Likert scale (strongly disagree to strongly agree). The survey was sent to all health professionals within the MCCC including medical consultants, registrars, residents, and interns, as well as nurses, allied health professionals, pharmacists, and managers. Anonymity was guaranteed. Participants were asked to return the completed survey within 1 month. The medical director of the service was also asked to complete the survey.
Part B. A subset of the indicators of integration of oncology and palliative care are objective outcome measures. These were assessed separately in a retrospective chart review and included all clinical outcome indicators and one objective clinical process outcome. All patients who had attended the oncology clinic and were listed as having died in the first 6 months of 2015 were sourced from the electronic data base system used in the MCCC. The information for each patient was assessed independently by two investigators and any differences were resolved by discussion and agreement.
A total of 37 indicators were assessed: 24 (10 major and 14 minor) in the survey and 15 (5 major, 10 minor) in the chart review. Two indicators (early referral to PC and routine documentation of advance care planning) were included in both the staff survey and the chart review.
In the original article, Hui et al. [9] describe 43 indicators. These included 3 “general” indicators: (1) “the presence of a comprehensive palliative care program”, (2) “improved patient care outcomes such as symptom management, quality of life, and quality of end-of-life care”, and (3) “high level of collaboration between oncology and palliative care in educational activities”. It was considered that components of these broad indicators were assessed within other more specific indicators and as such, were not included.
Three further indicators were not assessed as they were considered specific to the US hospice program model and did not apply to Australia. These were (1) “proportion of outpatients with any hospice enrolment”, (2) “proportion of outpatients with hospice enrolment within 3 days of death”, and (3) “proportion of non-referred patients with PC or hospice discussed within last 2 months of life”.
Descriptive statistics using the mean and standard deviations for normally distributed data and medians and interquartile ranges was used to summarize the data.
As the expert panel did not define an objective measure of ‘integration’, we arbitrarily defined integration as >70% of all respondents answering “agree” or “strongly agree” to each indicator and >70% of patient records supporting each criteria. The Palliative and Supportive Care service was to be considered fully integrated with oncology if >70% of the indicators were positive according to the listed criteria.
Results
Part A. Staff survey
Fifty-seven surveys were distributed to 16 medical staff (including trainees (2 oncology, 1 palliative care)), nursing (22), allied health (11), and pharmacy (8) staff. Of these 34 were returned (69% participation rate). Demographic data of participants are summarized in Table 1. The majority of respondents were female nursing staff working in oncology. Results of the major and minor criteria tested in the survey are shown in Table 2. At least 70% of participants agreed with 3 out of the 10 major indicators and 3 of the 14 minor criteria. There was significant disagreement around several of the education indicators and palliative care referral criteria. According to our pre-determined definition, respondents considered that we met the criteria of an integrated service in only 25% of the criteria. There were a number of indicators in which a significant proportion of those surveyed were unable to give an answer (“don’t know”) (Table 2).
Responses given by the medical director to the survey are also shown in Table 2. Positive responses were given to all but 2 of the indicators (92% agreement). The service does not provide a didactic training program for oncology nor a routine trigger for palliative care referral.
Part B. Chart review
Seventy-two patients known to the MCCC were recorded as having died between the first of January 2015 and the 30th of June 2015. Of these, five patients with haematological diseases and one with non-malignant disease were excluded. Sixty-seven charts were reviewed. Their median age was 68 (range 32–86) years with the preponderance of females reflecting the cancers most commonly treated at this centre (breast (27%), gynaecological (27%), colorectal (14%), prostate and lung (11% each)). Adherence to the major and minor objective indicators are shown in Table 3.
There was documentation that the majority of patients (92%) were seen by the palliative care team prior to death, usually as an out-patient on 2 or more occasions. Thirty percent of this cohort was reviewed only on the ward and not in the out-patient clinic. The median times from referral and last outpatient visit to death were 103 (range 0–1347) and 39 (range 7–653) days, respectively.
Pain assessment was documented commonly (90%) within the last 2 out-patient visits prior to death, but dyspnoea less so (36%). A median of three other symptoms were also addressed during the two visits. Prognostic discussions with the patient, or family, were recorded in the chart in 45 cases (68%). Advanced care planning discussions were documented in 38 charts (58%).
The preferred place of death was noted in 39% of cases. Although 21% of patients stated a wish to die at home, this occurred in only 9% of the cohort in which place of death was known. Similarly although only 15% wished to die in a palliative care unit, this was the place of death for 42%. Four patients (6%) were admitted to the intensive care unit (ICU) within 30 days prior to death, but none died in the ICU. Five patients (8%) received chemotherapy within their last 2 weeks of life. In the 30 days prior to death, only 5 (8%) patients had 2 or more emergency department visits and 12 (18%) 2 or more hospital admissions.
In summary, in the chart review, we met our pre-defined definition of integration in 3 out of 5 major and 6 out of 10 minor indicators (total 9 of 15, 60%).
Discussion
To our knowledge, this is the first study benchmarking the integration of oncology and palliative care at a major cancer centre against published ICP criteria.
The staff survey and chart review met our definition of an integrated service in only 6 out 13 major criteria and 9 of 24 minor criteria. The results did not reach our predefined cut-off of 70%, as there was subjective (survey) or objective (chart review) agreement of more than 70% for only 41% of the indicators.
Does this reflect a true lack of integration, poor documentation in clinical notes or lack of awareness on the part of non-medical health staff as to the role of palliative care within the oncology department?
In the survey of health care professionals (HCP) including physicians, nurses, allied health and pharmacologists, the presence of an interdisciplinary outpatient and inpatient palliative care consultation team was recognized by the majority of respondents (> 94%). They also acknowledged the senior leadership role of a palliative care clinician and the acceptance of concurrent anticancer treatment. However, we did not reach our pre-determined benchmark of 70% agreement for the majority of indicators (18 questions out of the 24), mainly because of a high percentage of “don’t know” answers. This was especially evident for those indicators relating to education, but also to those concerning research and service delivery. Further education is necessary in order to inform all members of our multidisciplinary team of the service provided. Of note, the criteria of integration were developed by physicians with a focus on physician training and education, and consequently a high percentage of the non-medical health care professionals were unable to respond to most of the indicators on education.
Surveys on the level of integration of oncology and palliative care have been conducted in the past [5]. However, all of them have been addressed to the head of either a palliative care or an oncology service, thus reflecting only the opinion of a senior leader. According to the Director of Cancer Services at this site, we would be considered a highly integrated service in that they responded in agreement to 92% of all questions (22/24). However, palliative care is an interdisciplinary approach and we propose that integration is only achieved if it is perceived as such by all health care professionals working with patients with advanced cancer.
Some of the indicators such as “early palliative care” lacked specific definitions. Even the expert panel could not agree, but was split between referral within 3 months, 2 months, or 1 month after diagnosis of advanced cancer. In a tertiary centre, it was often difficult to determine the exact date of diagnosis of advanced cancer for example, in patients treated elsewhere first, or referred from other centres. Therefore, we chose to measure the median time from referral to death, which in this case was between 3 and 4 months. Some palliative care experts suggest that symptom burden rather than time from diagnosis should be used as a trigger for palliative care involvement [10].
The chart review allowed for a more objective benchmarking process as this was not dependent on the knowledge of the respondent but on documentation of practice.
For the outcomes measuring “aggressive” treatment at the end of life (e.g., proportions of patients with ICU admission in last 30 days of life, chemotherapy administered within the last 2 weeks of life, 2 or more emergency room visits or hospital admissions in last 30 days of life and hospital admission or death in the ICU) there is no definition of what should be considered acceptable. We suggest setting a benchmark of less than 10% for each of these indicators with the possible exception of hospital admissions. Using these criteria, very few patients in our sample received aggressive treatment at the end of life.
Pain was documented as being assessed commonly (94%) in either of the last 2 out-patient visits prior to death, but dyspnoea less so (36%). A median of 3 (range 0–7) other symptoms were also addressed. The indicators do not specify assessment of any of the other common symptoms e.g. fatigue, drowsiness, lack of appetite or nausea. Following the audit, symptom scores are now routinely collected from all patients at every clinic review. Documentation of discussions around prognosis and assessment of patients’ preferred place of death were also highlighted as areas for improvement.
Two indicators were included in both the survey and the chart review in order to establish whether there is a difference in the perception by health care professionals and the documentation in the chart. There was reasonable consistency around advance care planning (around 60% in both the survey and chart review). Regarding early referral to palliative care, in the survey 61% of respondents agreed with this whereas the actual time was a median of 103 days before death, which in the absence of an agreed definition, we considered consistent with early referral.
Limitations
It proved difficult to benchmark our service against the current published criteria that include a mixture of indicators. Those relating to service models could only be fully assessed by senior clinicians in the department with an in-depth knowledge of the service. Other more objective criteria could be audited via a formal chart review. Whilst 43 indicators were defined by the expert panel, we chose to assess only 37 (13 major, 24 minor indicators).
With respect to our audit, there were considerable missing data around actual place of death. Many of the patients at this hospital are referred to hospices or community palliative care teams in the terminal phase. Therefore, place of death is not always known. Similarly, it was not possible to benchmark against some of the criteria that lacked definitions, e.g. early referral and aggressive care at the end of life.
As with all retrospective chart reviews, the results depend on the quality of the documentation.
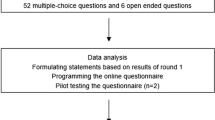
Suggestions for improvements for other departments wishing to undertake a similar bench-marking exercise are shown in Fig. 1.
What we learned from the study
We identified a need to educate all members of the multidisciplinary team about what is offered by our service. Other improvement initiatives have included the implementation of routine symptom screening and assessments during clinic visits with clear documentation of such. An advance care plan document has also been developed for future use.
Conclusions
Contrary to the view of the Medical Director, a survey of the multidisciplinary team at our major cancer centre in conjunction with an objective chart review does not support our pre-determined definition of an integrated service according to published criteria. The putative indicators of integration of oncology and palliative care as developed by the expert panel [9] have been proven to be feasible in clinical application, but are too focused on the medical view of integration and are not always applicable to review by other members of the multidisciplinary team. Clearer definitions around some of the criteria need to be formulated. Similarly, it is not clear whether these criteria would apply to all models of cancer care delivery. The objective criteria can be audited from review of clinical notes. Our results have highlighted areas for improvement in our service and might serve as a benchmark for other cancer services.
References
Yennurajalingam S, Urbauer DL, Casper KL et al (2011) Impact of a palliative care consultation team on cancer-related symptoms in advanced cancer patients referred to an outpatient supportive care clinic. J Pain Symptom Manag 41:49–56
Hui D, Kim YJ, Park JC et al (2015) Integration of oncology and palliative care: a systematic review. Oncologist 20:77–83
Temel JS, Greer JA, Muzikansky A et al (2010) Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med 363:733–742
Zimmermann C, Swami N, Krzyzanowska M et al (2014) Early palliative care for patients with advanced cancer: a cluster-randomised controlled trial. Lancet 383:1721–1730
(ESMO) ESfMO (2003). Designated centres of integrated oncology and palliative care. In
Smith TJ, Temin S, Alesi ER et al (2012) American Society of Clinical Oncology provisional clinical opinion: the integration of palliative care into standard oncology care. J Clin Oncol 30:880–887
Ferrell B, Temel JS, Termin S et al (2016) Integration of Palliative Care Into STandard Oncology Care: American Society of Clinical Oncology Clinical Practice Guideline Update. Journal of Clinical Oncology Epub
Rhee KJ, Donabedian A, Burney RE (1987) Assessing the quality of care in a hospital emergency unit: a framework and its application. QRB Qual Rev Bull 13:4–16
Hui D, Bansal S, Strasser F et al (2015) Indicators of integration of oncology and palliative care programs: an international consensus. Ann Oncol 26:1953–1959
Hui D, Bruera E (2015) Models of integration of oncology and palliative care. Ann Palliat Med 4:89–98
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Prof Janet Hardy declares that she has sat on medical advisory boards of MundiPharma Pty Ltd. and Menarini Australia Pty Ltd. Any honoraria are directed to charity.
All other authors declare no conflict of interest.
Funding
Petra Vayne-Bossert was granted a travel and expense fund by the University Hospital of Geneva for a research fellow year (2015) in Brisbane, Australia.
Rights and permissions
About this article
Cite this article
Vayne-Bossert, P., Richard, E., Good, P. et al. Integration of oncology and palliative care: setting a benchmark. Support Care Cancer 25, 3253–3259 (2017). https://doi.org/10.1007/s00520-017-3736-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-017-3736-2