Abstract
Introduction
Continuous palliative sedation (PS) is currently titrated based on clinical observation; however, it is often unclear if patients are still aware of their suffering. The aim of this prospective study is to characterize the level of consciousness in patients undergoing PS using Bispectral Index (BIS) monitoring.
Patients and methods
We enrolled consecutive patients with refractory symptoms requiring PS. We documented the level of sedation using Ramsay Sedation Scale (RSS) and BIS at 0, 2, 4, 6, 12, and 24 h during the first day of PS and examined their degree of association. Intravenous midazolam or propofol was titrated according to the sedation level.
Results
Twenty patients on PS were recruited and had BIS continuous monitoring. Delirium was the most frequent reason for PS (n = 15, 75%). The median time of sedation was 24.5 h (interquartile range 6–46). The average time to achieve the desired sedation level was 6 h, and dose titration was required in 80% of the cases. At baseline, 14 (70%) patients were considered to be awake according to RSS (i.e., 1–3) and 19 (95%) were awake according to BIS (i.e., >60%). This proportion decreased to 31 and 56% at 4 h, 27% and 53 at 6 h, and 22 and 33% at 24 h. RS and BIS had moderate correlation (rho = −0.58 to −0.65); however, a small proportion of patients were found to be awake by BIS (i.e., ≥60%) despite clinical observation (i.e., RSS 4–6) indicating otherwise.
Conclusions
The BIS is a noninvasive, bedside, real-time continuous monitoring method that may facilitate the objective assessment of level of consciousness and dose titration in patients undergoing PS.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Palliative sedation is an important and necessary intervention in the management of patients in whom the intentional reduction of a state of consciousness is required to relieve one or more refractory symptoms at the end of life [1, 2]. However, there is currently no consensus on the optimal level of sedation necessary for the relief of suffering, nor the ideal method to assess a patient’s level of consciousness/awareness [3,4,5]. In practice, palliative care clinicians often rely on a number of observational scales based on the patient’s ability to react to different stimuli; the Ramsay Sedation Scale (RSS) is one of the most frequently used assessments [6,7,8].
One strategy that has been used to objectively assess the level of consciousness is Bispectral Index (BIS) monitor, which collects and processes cerebral electrical activity thru electroencephalogram. Its main output is a number ranging from 0 to 100, with higher level indicating a greater level of consciousness. It has been extensively used in the intensive care and perioperative settings to monitor patients under anesthesia to reduce the risk of intraoperative awareness during surgical procedures [9, 10] and has proven useful to monitor the level of sedation during diagnosis procedures [11, 12] and in the context of the intensive care unit (ICU) [13,14,15]. Increases in the BIS values in sedated patient have been demonstrated due to nociceptive stimuli during routine procedures (endotracheal suctioning and mobilization) in unconscious patients in the ICU [16], and it has been suggested as maybe an additional instrument for pain evaluation in patients undergoing mechanical ventilation and sedation [17, 18]. To date, only a handful of case reports and case series have been published on the use of BIS in the palliative care setting [19,20,21,22].
The Palliative Care Service at the Instituto Nacional de Cancerologia (INCan) has established a palliative sedation protocol based on international guidelines—the Intensive Management of Pain, Anxiety and Distress (MIDAS) program—incorporating the use of BIS to assist with monitoring of the level of consciousness during palliative sedation [7]. This paper reports our preliminary experience of the use of BIS during palliative sedation.
Patients and methods
In this prospective observational study, patients were eligible if they had a diagnosis of advanced cancer with no further disease-modifying treatment options, required admission to the INCan palliative care unit, had refractory symptoms requiring the MIDAS palliative sedation protocol after discussion between the family and at least three attending physicians, and had do-not-resuscitate orders in place. Written consent was obtained from the legal representative before palliative sedation and BIS monitoring were initiated. This study was reviewed and approved by the Institutional Review Board of the INCan (Ref. CEI/1006).
Palliative sedation procedure
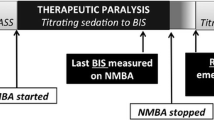
The MIDAS palliative sedation protocol provides continuous IV infusion that combines the hypnotic effect of propofol with the anxiolytic action of midazolam [23, 24], with the purpose of decreasing the level of consciousness in patients with refractory symptoms. Palliative sedation (PS) was initiated by one attending physician and a palliative care fellow together. Initial propofol doses of 0.16 mg/kg/h and midazolam 0.08 mg/kg were adjusted according to the individual patient response. We increased these medications if either RSS remained at 1–3 or BIS >60.
Opioids, antipsychotics, and any other drugs required for symptom control were continued during sedation according with the patient’s needs. Heart rate, blood pressure, and temperature were recorded according to the hospital policy.
Evaluation of sedation
The level of sedation was assessed with both RSS and BIS. The RSS scores sedation at six different levels according to how rousable the patient is: awake states range from 1 (agitated and restless) to 3 (response to commands only), and the asleep states range from 4 (exhibits brisk response to light glabellar tap or loud auditory stimulus) to 6 (no response to stimulus) [8]. This score is easy to use in palliative care [25] and has been validated in several settings [26, 27]. In this study, RSS was documented at 0, 2, 4, 6, 12, and 24 h after initiation of palliative sedation by a palliative care fellow.
We used the BIS Vista Bilateral Monitoring System 1.2 (Covidien, Mansfield, UK) with the commercially available adult bilateral sensor placed on the patient’s forehead (Aspect Medical Systems, Inc. Norwood, MA 02062, USA) at bedside. The BIS transmits four-point EEG signals from a sensor placed on the patient’s head to a monitoring system that acquires and processes four channel measures to produce a single number, called the Bispectral Index™, which correlates to the patient’s level of hypnosis [28,29,30]. Level of sedation is expressed as a parameter ranging from 0 (flat line EEG) to 100 (fully awake). A target range between 40 and 60 has been advocated both to prevent awareness and to reduce the dose of anesthetic agent administered [10, 31, 32].
BIS monitoring was performed continuously from initiation of palliative sedation until death. The readings were recorded at predetermined intervals throughout the first 24 h (i.e., 0, 2, 4, 6, 12, and 24 h) at the same time of RSS assessments. Patients who received PS for longer than 24 h continued to have BIS monitoring and RSS assessed; however, this study focused only on the first 24 h.
Statistics
We summarized the data with descriptive statistics, including mean; median; and interquartile range (IQR), frequencies, and proportions. BIS values and RSS grouped all the measures, and Spearman rank correlation coefficient was calculated between Ramsay and Bispectral Index (baseline, time 1, 2, 4, 6, 12, and 24 h). Results were graphically represented using a boxplot and a scatterplot. The statistical software program Stata Version 12 (StataCorp. 2011. Stata Statistical Software: Release 12. College Station, TX: StataCorp LP) was used to analyze the data.
Financing
The sensors and electrodes were purchased by our institution from Covidien. The company provided technical training to physicians of the Palliative Care Service; however, it did not provide any funding to this study, nor participate in the design, interpretation of data, or preparation of the manuscript.
Results
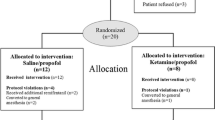
We assessed 254 hospitalized patients for eligibility between April and November 2015. Twenty-seven (13%) were fully eligible. Among these individuals, we obtained surrogate consent in 20 (74%) patients. The median age was 46 years and 12 (60%) were female (Table 1).
The reasons for palliative sedation were delirium (n = 15, 75%), pain (n = 13, 65%), dyspnea (n = 6, 30%), seizures (n = 5, 25%), malignant obstruction (n = 3, 15%), existential distress (n = 2, 10%), asphyxia (n = 1, 5%), and massive bleeding (n = 1, 5%). Among the patients with refractory pain, the average fentanyl doses were 2000 mcg/24 h (range 1600–4000 mcg/24 h) prior to initiation of palliative sedation. Ninety percent of the patients had two or more symptoms, with the combination of delirium and pain in 9/20 patients (Table 1).
Propofol and midazolam titrations were adjusted based on both RSS and BIS. The continuous infusion rate ranged between 0.16 and 1.3 mg/kg/h for propofol, and between 0.08 and 0.5 mg/kg/h for midazolam. The median time of sedation was 24.5 h (IQR 6–46), and the median survival was 19 h. None of the patients required intubation.
During PS, there was a significant decrease in the level of consciousness over time. At baseline, 14 (70%) of patients were considered to be awake according to RSS (i.e., 1–3) and 19 (95%) were awake according to BIS (i.e., >60%). This proportion decreased to 31.2 and 56.2% at 4 h, 26.7 and 53.3% at 6 h, and 22.2 and 33.3% at 24 h (data not shown). A tendency toward the increase of RSS was observed as the BIS values decreased (Fig. 1).
Notably, BIS values varied from 35 to 85.5, even when the RSS was between 4 and 6. Figure 2 shows the association between RSS and BIS at different time points. The Spearman rank correlation between RSS and BIS was −0.583 at baseline (P = 0.007), −0.658 at hour 2 (P = 0.002), −0.48 at hour 4 (P = 0.059), −0.46 at hour 6 (P = 0.0875), −0.68 at hour 12 (P = 0.014), and −0.65 at hour 24 (P = 0.053). The median BIS index among all the patients alive at 24 h (n = 9/20) was 42 (range 40–62). At each assessment time point, a small proportion of patients with RSS 4–6 had high BIS index of 60% of higher.
Only 4 (20%) patients had RSS 4–6 and BIS below 60 throughout the first 24 h and did not require dose escalation. The remaining 16 (80%) patients required an increase in their propofol and/or midazolam doses based on either RSS or BIS readings.
Discussion
The management of symptoms in patients at the end of life is often complex, and the use of PS requires thoughtful discussions among the clinical team members. One of the most challenging aspects of PS involves determination of whether patients were adequately sedated to minimize their suffering. As highlighted in this study, a sizable proportion of patients with low RSS of 4–6 still had BIS readings, suggesting that they may be conscious. Our study supports that BIS may be a promising tool to augment clinical assessment for patients undergoing palliative sedation.
Consistent with the literature, PS was only provided to a highly selected patient population with refractory symptoms. Delirium and pain were the most common indications and can be extremely distressing to patients, family caregivers, and health care professionals. Currently, there are few effective options for agitated delirium [33] and PS represents an important treatment of last resort.
The goal of PS was to provide continuous deep sedation to alleviate intense refractory suffering from terminal cancer. Monitoring the palliative sedation and active titration of medication is possibly the most important aspect to ensure patient comfort and alleviate symptoms and suffering [1, 7, 34,35,36,37,38,39]. Unfortunately, existing clinical observation tools such as RSS are relatively crude and are not able to differentiate among various levels of hypnotic depth [8, 40]. Since its publication, the RSS has been a common method to assess levels of sedations in different clinical settings, mostly because of its familiarity to staff and simplicity [41, 42]. However, its clinical limitations include the lack of a clear discrimination particularly in deeper levels of sedation and the considerable interrater variability [42, 43].
The level of sedation during anesthesia and in seriously ill patients in ICUs has been extensively studied [39,40,41,42,43,44,45]. Awareness during surgery is a distressing complication that patients report as perception of paralysis, accompanied by feelings of helplessness, fear, and pain [46, 47]. In other states with disturbance of consciousness such as delirium, Bruera et al. [48] reported that most patients with advanced cancer who recovered from their delirium were able to recall their experience, causing moderate to severe distress in both patients and family caregivers. It is thus critical to ensure that patients received adequate sedation.
To date, the use of BIS monitoring for PS has only been reported in few studies. Barbato [19] and Gambarell [49] found that BIS was acceptable for patients, family, and caregivers and could be used to monitor sedation level and the effect of medication. Barbato [20, 22] further suggested that BIS monitoring may add value to assure a deep level of sedation. However, these descriptive studies were not aimed at validation of BIS monitoring in the palliative care setting. Masman et al. [21] have recently published the results in concurrent validity, sensitivity to change, and feasibility of BIS monitoring in 58 end-of-life patients. Consistent with our findings, they found a moderate correlation between BIS and Ramsay scores.
This report provides additional information to the works of Masman and Barbato. To our knowledge, this is the first Latin American study that evaluated BIS monitoring in PS in terminal cancer patients; all the patients included in the study had advanced disease, with one or more refractory symptoms; they all were receiving strong opioids for pain control. In addition, propofol and midazolam IV infusion doses were titrated using the targeted depth of sedation BIS value of 60 or less. Dosages were increased if BIS values were above 60, regardless of the RSS.
In this study, we used BIS to augment clinical observation to adjust medications during PS, resulting in a greater proportion of patients achieving sedation within the first 24 h. Overall, we found moderate correlation between BIS and RSS. Interestingly, we found a sizable proportion of patients with RSS indicating adequate sedation but high BIS values, suggesting that they had significant brain activity and may potentially be awake. As suggested by Barbato [22] using observational scales, our findings raise the question of whether RSS alone is adequate to support clinical decision making surrounding PS and highlight the possibility that patients may not be as sedated as they appeared to be [18, 50]. It was not possible to know if these elevated BIS values were transient in nature and whether these patients had any degree of awareness at those moments, or as has been suggested by Coleman and Gelinas, pain increased the BIS values [16, 51].
Our study shows that BIS was feasible in the palliative care setting. It was easy to apply for continuous monitoring, and family caregivers found its use to be acceptable. The placement of sensor over the forehead was not distressing to caregivers, and many reported the BIS reading to be informative even as death approached (data not shown). Some limitations about this study are a small sample size because only a minority of patients had refractory symptoms. This study was performed in a single institution which may limit its generalizability. Finally, we only documented RSS and BIS for the first 24 h. Longer-term studies may be useful.
Conclusion
BIS is a noninvasive continuous monitoring method in real time which can provide objective graphic measurement of the level of consciousness among patients receiving palliative sedation. The use of this tool may augment clinical assessment and help to identify patients who need further titration of medications. Additionally, BIS may provide reassurance to the family that their loved one was not suffering. Further studies are needed to explore the use of BIS from the family caregivers’ perspective and to further validate its utility in the palliative care setting.
References
Cherny N (2009) The use of sedation to relieve cancer patients’ suffering at the end of life: addressing critical issues. Ann Oncol 20(7):1153–1155. doi:10.1093/annonc/mdp302
Cherny N, Radbruch L (2009) European Association for Palliative Care (EAPC) recommended framework for the use of sedation in palliative care. Palliat Med 23:581–593. doi:10.1177/0269216309107024
Maltoni M, Scarpi E, Rosati M, Derni S, Fabbri L, Martini F et al (2012) Palliative sedation in end-of-life care and survival: a systematic review. J Clin Oncol 30:1378–1383. doi:10.1200/JCO.2011.37.3795 Journal of Clinical Oncology 30, no. 12 (April 2012) 1378-1383
Beller EM, van Driel ML, McGregor L, Truong S, Mitchell G (2015) Palliative pharmacological sedation for terminally ill adults. Cochrane Database Syst Rev (1)CD010206.doi: 10.1002/14651858.CD010206.pub2
Gurschick L, Mayer K, Hanson LC (2015) Palliative sedation: an analysis of international guidelines and position statements. Am J Hosp Palliat Care 32:660–671. doi:10.1177/1049909114533002
Chamorro C, Martínez-Melgar JL, Barrientos R (2008) Sedación, analgesia y bloqueo neuromuscular en el paciente crítico. Recomendaciones del grupo de trabajo de analgesia y sedación de la SEMICYUC. Monitorización de la sedación. Monitoring of sedation. Med Int 32 Supl 1:45–52 Vol. 32
Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, Chalfin DB et al (2002) Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 30:119–141
Ramsay MAE, Savege TM, Simpson BRJ, Goodwin R (1974) Controlled sedation with alphaxalone-alphadolone. Br Med J 2:656–659
Rosow C, Manberg PJ (2001) Bispectral index monitoring. Anesthesiol Clin North Am 19:947–966
Punjasawadwong Y, Phongchiewboon A, Bunchungmongkol N (2014) Bispectral index for improving anaesthetic delivery and postoperative recovery. Cochrane Database Syst Rev (6):CD003843. DOI: 10.1002/14651858.CD003843.pub3
Müller JN, Kreuzer M, García PS, Schneider G, Hautmann H (2017) Monitoring depth of sedation: evaluating the agreement between the Bispectral Index, qCON and the entropy module’s state entropy during flexible bronchoscopy. Minerva Anestesiol. doi:10.23736/S0375-9393.17.11262-9
Sathananthan D, Young E, Nind G, George B, Ashby A, Drummond S et al (2017) Assessing the safety of physician-directed nurse-administered propofol sedation in low-risk patients undergoing endoscopy and colonoscopy. Endosc Int Open 5:E110–E115. doi:10.1055/s-0042-121667
Dou L, Gao HM, Lu L, Chang WX (2014) Bispectral index in predicting the prognosis of patients with coma in intensive care unit. World J Emerg Med 5:53–56. doi:10.5847/wjem.j.1920-8642.2014.01.009
Yaman F, Ozcan N, Ozcan A, Kaymak C, Basar H (2012) Assessment of correlation between bispectral index and four common sedation scales used in mechanically ventilated patients in ICU. Eur Rev Med Pharmacol Sci 16:660–666
Faritous Z, Barzanji A, Azarfarin R, Ghadrdoost B, Ziyaeifard M, Aghdaei N, Alavi M (2016) Comparison of bispectral index monitoring with the critical-care pain observation tool in the pain assessment of intubated adult patients after cardiac surgery. Anesthesiology and Pain Medicine 6:e38334. doi:10.5812/aapm.38334
Gélinas C, Tousignant-Laflamme Y, Tanguay A, Bourgault P (2011) Exploring the validity of the bispectral index, the critical-care pain observation tool and vital signs for the detection of pain in sedated and mechanically ventilated critically ill adults: a pilot study. Intensive Crit Care Nurs 27:46–52. doi:10.1016/j.iccn.2010.11.002
Gélinas C, Johnston C (2007) Pain assessment in the critically III ventilated adult: validation of the critical-care pain observation tool and physiologic indicators. Clin J Pain 23:497–505. doi:10.1097/AJP.0b013e31806a23fb
de Wit M, Epstein SK (2003) Administration of sedatives and level of sedation: comparative evaluation via the Sedation-Agitation Scale and the Bispectral Index. Am J Crit Care 12:343–348 Consulted on line at: http://ajcc.aacnjournals.org/content/12/4/343.full, Feb 16, 2016
Barbato M (2001) Bispectral index monitoring in unconscious palliative care patients. J Palliat Care 17:102–108
Barbato M, Barclay G, Potter J, Yeo W (2015) Sedation and analgesia in unconscious palliative care patients: can Bispectral Index monitoring adds to our understanding? J Palliat Care 31:57–59
Masman AD, van Dijk M, van Rosmalen J, Blussé van Oud-Alblas HJ, Ista E, Baar FP, Tibboel D (2016) Bispectral index (BIS) monitoring in terminally ill patients: a validation study. J Pain Symptom Manag. doi:10.1016/j.jpainsymman.2016.01.011
Barbato M, Barclay G, Potter J, Yeo W, Chung J (2017) Correlation between observational scales of sedation and comfort and Bispectral Index scores (BIS). J Pain Symptom Manag. doi:10.1016/j.jpainsymman.2016.12.335
Mercadante S, De Conno F, Ripamonti C (1995) Propofol in terminal care. J Pain Symptom Manag 10:639–642
Lundströms, Zachrisson U, Fürst CJ (2005) When nothing help: propofol as a sedative and antiemetic in palliative cancer care. J Pain Symptom Manag 30:570–577
Porzio G, Aielli F, Verna L, Micolucci G, Aloisi P, Ficorella C (2010) Efficacy and safety of deep, continuous palliative sedation at home: a retrospective, single-institution study. Support Care Cancer 18:77–81. doi:10.1007/s00520-009-0632-4
van Dishoeck AM, van der Hooft T, Simoons ML, van der Ent M, Scholte op Reimer WJ (2009) Reliable assessment of sedation level in routine clinical practice by adding an instruction to the Ramsay Scale. Eur J Cardiovasc Nurs 8:125–128
Cleeland CS, Gonin R, Hatfield AK, Edmonson JH, Blum RH, Stewart JA et al (1994) Pain and its treatment in outpatients with metastatic cancer. N Engl J Med 330:592–596. doi:10.1056/NEJM199403033300902
Avidan MS, Zhang L, Burnside BA, Finkel KJ, Searleman AC, Selvidge JA et al (2008) Anesthesia awareness and the bispectral index. N Engl J Med 358(11):1097–1108
Kelley SD (2007) Monitoring consciousness. Using the Bispectral Index™ during anesthesia. 2nd ed. Aspect Medical Systems, Inc
American Society of Anesthesiology Task Force on Intraoperative Awareness (2006) Practice advisory for intraoperative awareness and brain function monitoring: a report by the American Society of Anesthesiology Task Force on Intraoperative Awareness. Anesthesiology 104(4):847–864
Jacobsohn E, Glick D, Burnside BA, Zhang L, Villafranca A, Karl L et al (2011) Prevention of intraoperative awareness in a high-risk surgical population Eric. N Engl J Med 365:591–600
Sigl JC, Chamoun NG (1994) An introduction to bispectral analyses for the electroencephalogram. J Clin Monit 10:392–404
Hui D, Dev R, Bruera E (2016) Neuroleptics in the management of delirium in patients with advanced cancer. Curr Opin Support Palliat Care 10:316–323
Dean MM, Cellarius V, Henry B, Oneschuk D, Librach L, Canadian Society Of Palliative Care Physicians Taskforce SL (2012) Framework for continuous palliative sedation therapy in Canada. J Palliat Med 15:870–879. doi:10.1089/jpm.2011.0498
McWilliams K, Keeley PW, Waterhouse ET (2010) Propofol for terminal sedation in palliative care: a systematic review. J Palliat Med 13:73–76. doi:10.1089/jpm.2009.0126
Kirk TW, Mahon MM (2010) Palliative Sedation Task Force of the National Hospice and Palliative Care Organization Ethics Committee. National Hospice and Palliative Care Organization (NHPCO) position statement and commentary on the use of palliative sedation in imminently dying terminally ill patients. J Pain Symptom Manag 39:914–923. doi:10.1016/j.jpainsymman.2010.01.009
Deschepper R, Laureys S, Hachimi-Idrissi S, Poelaert J, Distelmans W, Bilsen JL (2013) Palliative sedation: why we should be more concerned about the risks that patients experience an uncomfortable death. Pain 154:1505e1508. doi:10.1016/j.pain.2013.04.038
Sanders RD, Tononi G, Laureys S, Sleigh JW (2012) Unresponsiveness not equal unconsciousness. Anesthesiology 116:946e959
De Jonghe B, Cook D, Appere-De-Vecchi C, Guyatt G, Meade M, Outin H (2000) Using and understanding sedation scoring systems: a systematic review. Intensive Care Med 26:275. doi:10.1007/s001340051150
Reschreiter H, Maiden M, Kapila A (2008) Sedation practice in the intensive care unit: a UK national survey. Crit Care 12:R1521–R1528. doi:10.1186/cc714
Martin J, Parsch A, Franck M, Wernecke KD, Fischer M, Spies C (2005) Practice of sedation and analgesia in German intensive care units: results of a national survey. Crit Care 9:R117–R123 De
Brinkkemper T, van Norel AM, Szadek KM, Loer SA, Zuurmond WWA, Perez RSGM (2013) The use of observational scales to monitor symptom control and depth of sedation in patients requiring palliative sedation: a systematic review. Palliat Med 27:54–67. doi:10.1177/0269216311425421
Olson D, Lynn M, Thoyre SM, Graffagnino C (2007) The limited reliability of the Ramsay Scale. Neurocrit Care 7:227. doi:10.1007/s12028-007-0069-x
Lennmarken C, Bildfors K, Enlund G, Samuelsson P, Sandin R (2002) Victims of awareness. Acta Anaesthesiol Scand 46:229–231
Tonner PH, Paris A, Scholz J (2006) Monitoring consciousness in intensive care medicine. Best Pract Res Clin Anaesthesiol 20:191–200. doi:10.1016/j.bpa.2005.08.011
Sandin R, Enlund G, Samuelsson P, Lennmarken C (2000) Awareness during anaesthesia: a prospective case study. Lancet 355:707–711
Moerman N, Bonke B, Oosting J (1993) Awareness and recall during general anesthesia. Facts and feelings Anesthesiology 79:454–464
Bruera E, Bush S, Willey J, Paraskevopoulos T, Li Z, Palmer J, Elsayem A (2009) The impact of delirium and recall on the level of distress in patients with advanced cancer and their family caregivers. Cancer 115:2004–2012. doi:10.1002/cncr.24215
Gambrell M (2005) Using the BIS monitor in palliative care: a case study. J Neurosci Nurs 37:140–143
Myles PS, Leslie K, McNeil J, Forbes A, Chan MTV, for the B-Aware trial group Bispectral index monitoring to prevent awareness during anaesthesia (2004) The B-Aware randomised controlled trial. Lancet 363:1757–1763 Consulted on line at: http://www.sciencedirect.com/science/article/pii/S0140673604163009, April 6, 2016
Coleman RM, Tousignant-Laflamme Y, Gélinas C, Choinière M, Atallah M, Parenteau-Goudreault E et al (2013) Changes in the bispectral index in response to experimental noxious stimuli in adults under general anesthesia. ISRN Pain 1:1–8
Acknowledgments
The authors would like to thank Dana Aline Perez-Camargo and Adriana Pena for the support in the statistical analysis of the data, Oscar Rodriguez-Mayoral for the discussion of the manuscript.
Author information
Authors and Affiliations
Contributions
The authors declare that they have full control of all primary data and agree to allow the journal to review their data if requested.
Conception and design: Edith Monreal-Carrillo, Silvia Allende-Pérez, and Emma Verástegui
Data collection: Maria-Fernanda Garcia Salamanca
Analysis and interpretation of data: Edith Monreal-Carrillo, Emma Verástegui, David Hui, and Silvia Allende-Pérez
Manuscript writing: Emma Verástegui, Edith Monreal-Carrillo, David Hui, and Eduardo Bruera
Approval of final article: Emma Verástegui, David Hui, Edith Monreal-Carrillo, Silvia Allende-Pérez, Maria-Fernanda Garcia Salamanca, and Eduardo Bruera
All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Written consent was obtained from the legal representative before palliative sedation and BIS monitoring were initiated. This study was reviewed and approved by the Institutional Review Board of the INCan (Ref. CEI/1006).
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
This work received no financial support.
Additional information
Edith Monreal-Carrillo and Silvia Allende-Pérez contributed to the work equally.
Rights and permissions
About this article
Cite this article
Monreal-Carrillo, E., Allende-Pérez, S., Hui, D. et al. Bispectral Index monitoring in cancer patients undergoing palliative sedation: a preliminary report. Support Care Cancer 25, 3143–3149 (2017). https://doi.org/10.1007/s00520-017-3722-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-017-3722-8