Abstract
Purpose
Symptomatic adverse events (AEs) are monitored by clinicians as part of all US-based clinical trials in cancer via the U.S. National Cancer Institute’s Common Terminology Criteria for Adverse Events (CTCAE) for the purposes of ensuring patient safety. Recently, there has been a charge toward capturing the patient perspective for those AEs amenable to patient self-reporting via patient-reported outcomes (PRO). The aim of this review was to summarize the empirically reported association between analogous CTCAE and PRO ratings.
Methods
A systematic literature search was conducted using PubMed, EMBASE, Web of Science, and Cochrane databases through July 2015. From a total of 5658 articles retrieved, 28 studies met the inclusion criteria.
Results
Across studies, patients were of mixed cancer types, including anal, breast, cervical, chronic myeloid leukemia, endometrial, hematological, lung, ovarian, pelvic, pharyngeal, prostate, and rectal. Given this mixture, the AEs captured were variable, with many common across studies (e.g., dyspnea, fatigue, nausea, neuropathy, pain, vomiting), as well as several that were disease-specific (e.g., erectile dysfunction, hemoptysis). Overall, the quantified association between CTCAE and PRO ratings fell in the fair to moderate range and had a large variation across the majority of studies (n = 21).
Conclusions
The range of measures used and symptoms captured varied greatly across the reviewed studies. Regardless of concordance metric employed, reported agreement between CTCAE and PRO ratings was moderate at best. To assist with reconciliation and interpretation of these differences toward ultimately improving patient care, an important next step is to explore approaches to integrate PROs with clinician reporting of AEs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Accurate monitoring of symptomatic adverse events (AEs) is essential in clinical trials to assess and ensure patient safety, as well as inform decisions related to treatment and/or continued trial participation [1, 2]. Standard documentation of this information in US-based cancer clinical trials has relied solely on clinician reporting using an AE rating system known as the Common Terminology Criteria for Adverse Events (CTCAE) [3]. This library of descriptive terms was developed and is maintained by the U. S. National Cancer Institute (NCI) and consists of 790 items that capture information on discrete events; each is graded by a clinician on a 5-point scale. Of these, 78 items have been identified as objective, observable AEs [4].
Recently, there has been a charge toward the use of patient-reported outcomes (PROs), defined as the unfiltered direct report of a given symptom toxicity by a patient, and considered to be the “gold standard” for the capture of symptomatic AEs [5, 6]. This charge has been led by the release of the 2009 U. S. Food and Drug Administration (FDA) Guidance for Industry on the Use of PRO Measures in Medical Development to Support Labeling Claims [7], which subsequently led to the NCI initiative to develop a PRO version of the CTCAE (PRO-CTCAE) that will be used in future US-based clinical trials in oncology [4, 8, 9].
As the integration of PRO symptomatic AE ratings into cancer clinical trials becomes commonplace, it is important to understand the degree to which this patient-driven information is complementary to clinician-based CTCAE ratings of observable AEs. The purpose of this review is to summarize the current state of the literature with respect to characterizing the association between clinician-based CTCAE and patient-based PRO ratings.
Methods
Search strategy
A systematic search for articles published in peer-reviewed medical journals was conducted with assistance from health sciences librarians using PubMed, EMBASE, Web of Science, and Cochrane Central Register of Controlled Trials (CENTRAL) databases. In PubMed, Medical Subject Headings (MeSH) were used. In Embase, Emtree terms were exploded. The search terms were: (“Neoplasms”[Mesh] OR cancer OR cancers OR cancerous OR tumor OR tumors OR tumor OR tumors OR neoplasm* OR neoplastic OR malignan* OR metastatic OR metastasis OR metastases) AND (physician* OR doctor OR doctors OR clinician* OR “general practitioner” OR “general practitioners” OR provider* OR specialist* OR nurse* OR staff OR oncologist*) AND (agreement OR disagreement OR reliability OR concordance OR discrepancy OR consistency OR consensus OR “intraclass correlation coefficient” OR “intraclass correlation coefficient” OR “kappa correlation” OR “kappa coefficient” OR “self assessment” OR “physician assessment” OR “provider assessment” OR “self assessed” OR “physician assessed” OR “provider assessed” OR “patient ratings” OR “physician ratings” OR “provider ratings” OR “patients rated” OR “physicians rated” OR “providers rated” OR “Physician’s Role”[Mesh]) AND (“adverse symptom event” OR “adverse symptom events” OR “adverse event” OR “adverse events” OR “adverse effect” OR “adverse effects” OR “patient reported outcome” OR “quality of life” OR “Quality of Life”[Mesh] OR ECOG OR “Eastern Cooperative Oncology Group” OR “functional problems” OR distress OR “performance status” OR depression). There were no date or language restrictions; each database was search in its entirety, through July 2015.
Selection strategy
We deemed studies were eligible for inclusion if they (1) made an original report of a quantitative comparison between analogous CTCAE and PRO ratings and (2) included participants aged 18 or older.
Screening process
For the title screening, abstract review, and full-text review stages, two co-authors were randomly assigned to independently review each article for eligibility, with discrepancies arbitrated by a third co-author who was naïve to the article. At the full-text review stage, each assigned co-author completed standardized coding forms to extract the pre-determined data from the potentially eligible articles. References from the included full-text articles were searched to determine whether they should be also considered for inclusion. Study quality was assessed using a modified version of the Downs and Black Study Quality Checklist [10] (i.e., 16 of the original 27 quality indicators most relevant to the types of studies reviewed).Footnote 1 Based on quality, an article was considered to be fit for inclusion if it met at least 33 % of the modified Downs and Black Study quality indicators.
For the purposes of this review, cutoffs for all agreement metrics reported, including percentage agreement, Kendall-tau rank correlation (τ), Goodman and Kruskal’s gamma statistic (γ), Pearson’s correlation (r) , Cohen’s kappa (κ), weighted Cohen’s kappa (κw) statistics were defined as follows: poor (0.00–0.29), moderate (0.30–0.69), and strong (0.70–1.00). For instances where only specificity/sensitivity was reported, the following cutoffs were used: low (0.00–0.29), moderate (0.30–0.69), and high (0.70–1.00).
Results
A total of 7474 titles were identified through electronic database searching, with 75 additional records found through hand searching. After duplicates were removed, a total of 5658 articles were retrieved. Following title screening, 908 articles were identified for abstract review with 93.6 % agreement between the independent pairs of raters. A total of 251 full-text articles were reviewed. Reasons for article exclusion during the full-text review included the following: CTCAE not used (n = 161), PROs were not assessed (n = 18), the article was a review or did not include original research findings (n = 18), CTCAE and PRO ratings were not explicitly compared (n = 12), and the article described a non-cancer population (n = 5). Twenty-eight articles met the eligibility criteria and were included in this review (Fig. 1). Each of these articles possessed at least 47 % of the relevant quality indicators from a modified version of the Downs and Black Study Quality Checklist [10], with 21 of the included articles having 75 % or more of these quality indicators.
Study characteristics
Table 1 provides a summary of clinical characteristics and findings from each of the 28 included studies. Patients were of mixed cancer types, including anal, breast, cervical, chronic myeloid leukemia, endometrial, hematological, lung, ovarian, pelvic, pharyngeal, prostate, and rectal. Given this, the AEs captured were variable, with many common across studies (e.g., dyspnea, fatigue, nausea, neuropathy, pain, vomiting), as well as several that were disease-specific (e.g., erectile dysfunction, hemoptysis, xerostomia).
Well-validated PRO measures were used to capture patient-based AE ratings in 20 of the included studies. These included disease-specific modules of the European Organization for Research and Treatment of Cancer (EORTC) [12–20] and Functional Assessment of Cancer Therapy (FACT) [21–23] instruments, as well as the dermatology-specific Skindex-16, [24, 25] the EuroQol EQ-5D, [26] the Short-Form 36 Health Survey (SF-36) [27], and two recently developed bowel symptom inventories [28, 29]. Patient-adapted versions of the CTCAE were used in four studies [27, 30–32], with visual analog scales used to capture patient-rated AEs in three studies [11, 33, 34].
Association between CTCAE and PRO ratings
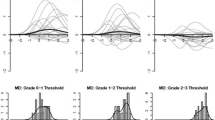
A poor to moderate association between CTCAE and PRO ratings was reported in the majority of included studies (n = 21). Seven such studies reported this as a general finding, with agreement statistics ranging from κ = 0.00 to r = 0.74 [14, 24, 27, 32, 34, 35]. Regardless of how pain was self-reported by patients (i.e., EuroQol EQ-5D or EORTC QLQ-C30), four independent studies reported moderate agreement between PRO and CTCAE ratings (r range = 0.33–0.37; κ range = 0.16–0.29) [16, 17, 20, 26]. Similarly, independent assessments of nausea and vomiting were reported as being poor, as captured by Symptom Tracking and Reporting (STAR) (τ = 0.11 and −0.02) [26] to moderate, as captured by EORTC QLQ-C30 (r range = 0.47–0.48, κ range = 0.41–0.48) [15–17].
Independent studies that made use of the Bowel Problem Scale in cohorts of patients with rectal [28] or anal [29] cancer found poor agreement with clinician ratings for proctitis (κ = 0.22 and 0.11, respectively) and moderate agreement for diarrhea (κ = 0.64 and 0.68, respectively). Additionally, independent studies of neuropathy reported a poor to moderate relationship between PRO and CTCAE reports, as measured by the FACT Gynecologic Oncology Group–Neurotoxicity Module (FACT/GOG-Ntx) (r’s range 0.23–0.69) [23, 36]. A study that made use of the Patient Neurotoxicity Questionnaire found that patients more frequently reported severe neuropathy (30 %) as compared to that identified by CTCAE (10 %) [37].
Several studies (n = 4) reported a mix of poor, moderate, and strong associations between CTCAE and PRO ratings. In a study of 400 patients with lung or genitourinary cancer, Basch and colleagues [30] reported a strong percentage of agreement between CTCAE and a modified CTCAE for nausea and vomiting (96 and 90 %, respectively), but relatively moderate percent agreement for fatigue (55 %) and strong percent agreement for pain (70 %). A study of 82 patients with lung cancer led by Brabo [13] observed a moderate correlation between CTCAE and the sore mouth (r = 0.41, p < 0.01), and alopecia items (r = 0.52, p < 0.01) from EORTC QLQ-C30. However, strong correlations were observed when comparing CTCAE and the EORTC QLQ-C30 dysphagia (r = 0.73, p < 0.01) and neuropathy (r = 0.72, p < 0.01) items. As part of a study of 100 patients with mixed cancer types, Cirillo and colleagues [31] found moderate agreement between CTCAE and a modified patient CTCAE for asthenia (κ = 0.32, 95 % confidence interval (CI) 0.17 to 0.44), but strong agreement between clinicians and patients for nausea (κ = 0.74, 95 % CI 0.64–0.85) and diarrhea (κ = 0.71, 95 % CI 0.43–0.90). A recently completed study of 66 patients with lung cancer by Tang and colleagues [38] found poor agreement between CTCAE and the Thoracic Symptom Self-Assessment Tool (TSSAT) for nausea (κ w = 0.07, 95 % CI −0.16–0.30) and insomnia (κ w = 0.03, 95 % CI −0.34-0.39), but strong agreement for hemoptysis (κ w = 0.71, 95 % CI 0.35–1.00).
Three studies reported a strong agreement between CTCAE and PRO ratings. These included a study of 281 patients with chemotherapy-induced peripheral neuropathy, as captured by the EORTC QLQ-CIPN20 [12]; a study of edema, neuropathy, and pain in 1031 patients with lung cancer, as captured by the FACT-Taxane module [22]; as well as a study of nausea in 30 patients with mixed cancer types, as measured by a visual analog scale (r = 0.88, p < 0.001) [11].
Discussion
As the oncological clinical encounter increasingly incorporates patient-reported data, it is necessary to inform clinicians how this data relates to the standard AE ratings they have been making as part of clinical trials and their routine practice. This review demonstrated that, regardless of which self-report measure was used, the majority of studies that have directly compared CTCAE and PRO ratings report a poor to moderate association between clinician and patient-based AEs, either globally, or by individual symptom (e.g., nausea, neuropathy, pain, vomiting).
This discordance between clinicians and patients provides further evidence that PRO measures provide unique, valuable information that can be complementary to CTCAE ratings. For instance, in a systematic review completed by Gotay and colleagues, it was demonstrated that PRO measures are correlated with survival in cancer clinical trials and provide information above and beyond conventional clinical assessments [39].
Currently, all AEs in clinical trials, including adverse symptoms, are documented by providers at clinic visits to meet federal requirements and facilitate evaluation of new therapies. Patient self-reporting has a relatively minimal role. However, this current practice is problematic, as our previous work has demonstrated that AEs frequently go undetected by clinicians or are reported as less severe than via patient reporting [26, 40]. Additionally, the CTCAE recall period encompasses the entire period since the last clinic visit for a given patient. In many cases, a patient follow-up visit might not occur for 2–4 weeks, which can lead to a loss of information related to AEs that are experienced early in that timeframe.
Recognizing the importance of accurately capturing the patient perspective as complementary information to clinician-based reporting, the NCI has developed a patient language version of the CTCAE (PRO-CTCAE) [4]. PRO-CTCAE is an electronic-based system for patient self-reporting of AEs from the CTCAE that were found to be amenable to patient reporting. This library of 78 symptoms was identified and developed via a process of direct cognitive interviews with patients and extensive quantitative validation in a large multicenter study [8, 9]. PRO-CTCAE utilizes a 7-day recall period and can be completed routinely by patients, and thus may be implemented to systematically capture AEs that may not be apparent at the time of clinician-based CTCAE grading.
The present review is limited by a number of factors. The timing of the respective CTCAE and PRO ratings was not explicitly stated in the majority of included articles, though it was implied that these AEs were proximally assessed. Future studies should clearly indicate the amount of time that occurs between clinician- and patient-based AE reporting to eliminate the possibility that the level of agreement between these rating sources is being influenced by passage of time (e.g., separate visits, between visits versus next or previous clinic visit). Additionally, a meta-analysis would have been optimal to best characterize the relationship between CTCAE and PRO ratings. Unfortunately, given the variety of PRO measures used and numerous instances where study authors did not provide detailed statistical coefficient for each AE captured, a meta-analysis was infeasible.
To better assist clinicians with understanding the relationship between their CTCAE ratings and PRO assessments, future work should seek to systematically equate CTCAE and PRO ratings. Future approaches that aim to integrate PROs with clinician reporting of AEs, especially those of the CTCAE and PRO-CTCAE, would improve our understanding of patient and clinician ratings and assist clinicians and policy makers with the interpretation of clinical trial results.
Notes
Questions 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 16, 17, 18, 19, 20, and 26 from the Downs and Black Study Quality Checklist were used to assess quality.
References
Basch E (2010) The missing voice of patients in drug-safety reporting. N Engl J Med 362:865–869
Basch E (2014) New frontiers in patient-reported outcomes: adverse event reporting, comparative effectiveness, and quality assessment. Annu Rev Med 65:307–317
Vyzula RRS (1996) Lung cancer in patients with HIV-infection. Lung Cancer 15:325–339
Basch E, Reeve BB, Mitchell SA, et al. (2014) Development of the National Cancer Institute’s patient-reported outcomes version of the common terminology criteria for adverse events (PRO-CTCAE). J Natl Cancer Inst 106:dju244
Basch E (2012) Beyond the FDA PRO guidance: steps toward integrating meaningful patient-reported outcomes into regulatory trials and US drug labels. Value Health 15:401–403
Trotti A, Colevas AD, Setser A, Basch E (2007) Patient-reported outcomes and the evolution of adverse event reporting in oncology. J Clin Oncol 25:5121–5127
US Department of Health and Human Services (2009) Guidance for industry. Patient-reported outcome measures: use in medical product development to support labeling claims. Available from: http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM193282.pdf. Accessed 5 Jan 2016
Hay JL, Atkinson TM, Reeve BB, et al. (2014) Cognitive interviewing of the US National Cancer Institute’s patient-reported outcomes version of the common terminology criteria for adverse events (PRO-CTCAE). Qual Life Res 23:257–269
Dueck AC, Mendoza TR, Mitchell SA, et al. (2015) Validity and reliability of the U.S. National Cancer Institute’s patient-reported outcomes version of the common terminology criteria for adverse events (PRO-CTCAE). JAMA Oncol 1:1051–1059
Downs SH, Black N (1998) The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health 52:377–384
Mandala M, Cremonesi M, Rocca A, et al. (2005) Midazolam for acute emesis refractory to dexamethasone and granisetron after highly emetogenic chemotherapy: a phase II study. Support Care Cancer 13:375–380
Alberti P, Rossi E, Cornblath DR, et al. (2014) Physician-assessed and patient-reported outcome measures in chemotherapy-induced sensory peripheral neurotoxicity: two sides of the same coin. Ann Oncol 25:257–264
Brabo EP, Paschoal ME, Biasoli I, et al. (2006) Brazilian version of the QLQ-LC13 lung cancer module of the European Organization for Research and Treatment of Cancer: preliminary reliability and validity report. Qual Life Res 15:1519–1524
Christodoulou M, McCloskey P, Stones N, et al. (2014) Investigation of a patient reported outcome tool to assess radiotherapy-related toxicity prospectively in patients with lung cancer. Radiother Oncol J Eur Soc Ther Radiol Oncol 112:244–249
Di Maio M, Gallo C, Leighl NB, et al. (2015) Symptomatic toxicities experienced during anticancer treatment: agreement between patient and physician reporting in three randomized trials. J Clin Oncol 33:910–915
Fromme EK, Eilers KM, Mori M, Hsieh YC, Beer TM (2004) How accurate is clinician reporting of chemotherapy adverse effects? A comparison with patient-reported symptoms from the quality-of-life questionnaire C30. J Clin Oncol 22:3485–3490
Greimel ER, Bjelic-Radisic V, Pfisterer J, et al. (2011) Toxicity and quality of life outcomes in ovarian cancer patients participating in randomized controlled trials. Support Care Cancer 19:1421–1427
Jensen K, Lambertsen K, Torkov P, et al. (2007) Patient assessed symptoms are poor predictors of objective findings. Results from a cross sectional study in patients treated with radiotherapy for pharyngeal cancer. Acta Oncol 46:1159–1168
Kirchheiner K, Nout R, Lindegaard J, et al. (2012) Do clinicians and patients agree regarding symptoms? A comparison after definitive radiochemotherapy in 223 uterine cervical cancer patients. Strahlenther Onkol: Organ der Deutschen Rontgengesellschaft [et al] 188:933–939
Quinten C, Maringwa J, Gotay CC, et al. (2011) Patient self-reports of symptoms and clinician ratings as predictors of overall cancer survival. J Natl Cancer Inst 103:1851–1858
Cella D, Huang H, Homesley HD, et al. (2010a) Patient-reported peripheral neuropathy of doxorubicin and cisplatin with and without paclitaxel in the treatment of advanced endometrial cancer: results from GOG 184. Gynecol Oncol 119:538–542
Hirsh V, Okamoto I, Hon JK, et al. (2014) Patient-reported neuropathy and taxane-associated symptoms in a phase 3 trial of nab-paclitaxel plus carboplatin versus solvent-based paclitaxel plus carboplatin for advanced non-small-cell lung cancer. J Thoracic Oncol Off Publ int Assoc Study Lung Cancer 9:83–90
Shimozuma K, Ohashi Y, Takeuchi A, et al. (2009) Feasibility and validity of the patient neurotoxicity questionnaire during taxane chemotherapy in a phase III randomized trial in patients with breast cancer: N-SAS BC 02. Support Care Cancer 17:1483–1491
Atherton PJ, Burger KN, Loprinzi CL, et al. (2012) Using the Skindex-16 and common terminology criteria for adverse events to assess rash symptoms: results of a pooled-analysis (N0993). Support Care Cancer 20:1729–1735
Neben-Wittich MA, Atherton PJ, Schwartz DJ, et al. (2011) Comparison of provider-assessed and patient-reported outcome measures of acute skin toxicity during a phase III trial of mometasone cream versus placebo during breast radiotherapy: the North Central Cancer Treatment Group (N06C4). Int J Radiat Oncol Biol Phys 81:397–402
Basch E, Jia X, Heller G, et al. (2009) Adverse symptom event reporting by patients vs clinicians: relationships with clinical outcomes. J Natl Cancer Inst 101:1624–1632
Efficace F, Rosti G, Aaronson N, et al. (2014) Patient- versus physician-reporting of symptoms and health status in chronic myeloid leukemia. Haematologica 99:788–793
Flores LT, Bennett AV, Law EB, et al. (2012) Patient-reported outcomes vs. clinician symptom reporting during chemoradiation for rectal cancer. Gastrointest Cancer Res GCR 5:119–124
Tom A, Bennett A, Rothenstein D, et al. (2013) Prevalence of patient-reported gastrointestinal symptoms and concordance with clinician toxicity assessments in radiation therapy for anal cancer. Int J Radiat Oncol Biol Phys 87:S570–S571
Basch E, Iasonos A, McDonough T, et al. (2006) Patient versus clinician symptom reporting using the National Cancer Institute Common Terminology Criteria for Adverse Events: results of a questionnaire-based study. Lancet Oncol 7:903–909
Cirillo M, Venturini M, Ciccarelli L, et al. (2009) Clinician versus nurse symptom reporting using the National Cancer Institute-Common Terminology Criteria for Adverse Events during chemotherapy: results of a comparison based on patient’s self-reported questionnaire. Ann Oncol 20:1929–1935
Gravis G, Marino P, Joly F, et al. (2014) Patients’ self-assessment versus investigators’ evaluation in a phase III trial in non-castrate metastatic prostate cancer (GETUG-AFU 15). Eur J Cancer 50:953–962
Cella D, Pulliam J, Fuchs H, et al. (2003) Evaluation of pain associated with oral mucositis during the acute period after administration of high-dose chemotherapy. Cancer 98:406–412
Steinsvik EA, Fossa SD, Axcrona K, et al. (2010) Do perceptions of adverse events differ between patients and physicians? Findings from a randomized, controlled trial of radical treatment for prostate cancer. J Urol 184:525–531
Franklin HR, Simonetti GP, Dubbelman AC, et al. (1994) Toxicity grading systems. A comparison between the WHO scoring system and the Common Toxicity Criteria when used for nausea and vomiting. Ann Oncol 5:113–117
Cella D, Riley W, Stone A, et al. (2010b) The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005-2008. J Clin Epidemiol 63:1179–1194
Bennett BK, Park SB, Lin CS, et al. (2012) Impact of oxaliplatin-induced neuropathy: a patient perspective. Support Care Cancer 20:2959–2967
Tang B, Giuliani M, Le LW, et al. (2013) Capturing acute toxicity data during lung radiotherapy by using a patient-reported assessment tool. Clin Lung Cancer 14:108–112
Gotay CC, Kawamoto CT, Bottomley A, Efficace F (2008) The prognostic significance of patient-reported outcomes in cancer clinical trials. J Clin Oncol 26:1355–1363
Atkinson TM, Li Y, Coffey CW, et al. (2012) Reliability of adverse symptom event reporting by clinicians. Qual Life Res 21:1159–1164
Park JH, Kim YS, Park J, et al. (2014) Incidence and dose-volume analysis of acute bladder toxicity following pelvic radiotherapy. Tumori 100:195–200
Acknowledgments
This project was supported by a National Institutes of Health Research Training Grant (T32 CA009461-25), as well as a National Institutes of Health Support Grant (P30 CA08748-48), which provides partial support for the Behavioral Research Methods Core Facility used in conducting this investigation. The authors wish to thank Jan-Samuel Wagner for his early contributions to the project, as well as Dr. Jamie Ostroff for her support of this work. A portion of these results were presented at the 2013 Conference of the International Society for Quality of Life Research in Miami, FL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Atkinson, T.M., Ryan, S.J., Bennett, A.V. et al. The association between clinician-based common terminology criteria for adverse events (CTCAE) and patient-reported outcomes (PRO): a systematic review. Support Care Cancer 24, 3669–3676 (2016). https://doi.org/10.1007/s00520-016-3297-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-016-3297-9