Abstract
Background
The Region of Tuscany Health Department was included as an associated member in WP7 “Healthcare” of the European Partnership for Action Against Cancer (EPAAC), initiated by the EU Commission in 2009.
Aims
The principal aim was to map centres across Europe prioritizing those that provide public health services and operating within the national health system in integrative oncology (IO).
Methods
A cross-sectional descriptive survey design was used to collect data. A questionnaire was elaborated concerning integrative oncology therapies to be administered to all the national health system oncology centres or hospitals in each European country. These institutes were identified by convenience sampling, searching on oncology websites and forums. The official websites of these structures were analysed to obtain more information about their activities and contacts.
Results
Information was received from 123 (52.1 %) out of the 236 centres contacted until 31 December 2013. Forty-seven out of 99 responding centres meeting inclusion criteria (47.5 %) provided integrative oncology treatments, 24 from Italy and 23 from other European countries. The number of patients seen per year was on average 301.2 ± 337. Among the centres providing these kinds of therapies, 33 (70.2 %) use fixed protocols and 35 (74.5 %) use systems for the evaluation of results. Thirty-two centres (68.1 %) had research in progress or carried out until the deadline of the survey. The complementary and alternative medicines (CAMs) more frequently provided to cancer patients were acupuncture 26 (55.3 %), homeopathy 19 (40.4 %), herbal medicine 18 (38.3 %) and traditional Chinese medicine 17 (36.2 %); anthroposophic medicine 10 (21.3 %); homotoxicology 6 (12.8 %); and other therapies 30 (63.8 %). Treatments are mainly directed to reduce adverse reactions to chemo-radiotherapy (23.9 %), in particular nausea and vomiting (13.4 %) and leucopenia (5 %). The CAMs were also used to reduce pain and fatigue (10.9 %), to reduce side effects of iatrogenic menopause (8.8 %) and to improve anxiety and depression (5.9 %), gastrointestinal disorders (5 %), sleep disturbances and neuropathy (3.8 %).
Conclusions
Mapping of the centres across Europe is an essential step in the process of creating a European network of centres, experts and professionals constantly engaged in the field of integrative oncology, in order to increase, share and disseminate the knowledge in this field and provide evidence-based practice.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The National Centre for Complementary and Alternative Medicine (NCCAM) defines complementary and alternative medicine (CAM) as follows: “A group of diverse medical and healthcare interventions, practices, products, or disciplines that are not presently considered to be part of conventional medicine”.
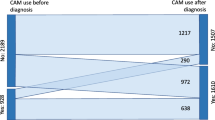
The use of CAM in cancer patients in association with mainstream treatments such as chemotherapy, radiation and surgery is steadily increasing over the past 20 years or so, and it has undoubtedly gained medical, economic and sociological importance [1].
A recent meta-analysis has suggested an increase in CAM use in cancer care from an estimated 25 % in the 1970s and 1980s to more than 32 % in the 1990s and to 49 % after 2000 [2].
The largest survey to date on the use of CAM in cancer patients showed that in Europe, more than one third (35.9 %) of cancer patients reported using some form of complementary and alternative medicine, with little variation across countries [3], but even now, little is still known about the use of CAM in cancer care across European countries and even less about the presence of centres that offer these kinds of services all over Europe.
Integrative oncology
According to Sagar, integrative oncology (IO) can be described as “both a science and a philosophy that recognizes the complexity of care for cancer patients and provides a multitude of evidence-based approaches to accompany conventional therapies and to facilitate health” [4].
According to Cassileth, Deng and Vickers, the introduction of integrative oncology into the consultation would enable the patient to receive a synthesis of the best of cancer treatment and evidence-based, supportive complementary modalities that effectively relieve many of the physical and emotional symptoms that cancer patients experience [5].
The goal of integrative oncology is to increase the efficacy of conventional cancer treatment programmes, reduce symptoms and improve quality of life for cancer patients. In other terms, it is an interdisciplinary blending of both conventional medicine and complementary healthcare that should provide a seamless continuum of decision-making and patient-centred care [6].
We did not use the definition “integrated” instead of “integrative” oncology as in our opinion, this adjective (integrated) should be applied only when any complementary and alternative therapy or practice is directly included in the anticancer therapy protocols as a “standard care”.
Aims of European Partnership on Action Against Cancer
The Joint Action “European Partnership on Action Against Cancer” (EPAAC) is an initiative started in September 2009 by the European Commission with the support of many partners and co-funded by the Programme “Health” of the European Union (EU). This action—which collects the efforts of the European Commission, the member states and the corresponding health ministries, associations of patients, clinicians and researchers and industry and civil society—intends to face the cancer issue within the European Union in an effective and harmonized way. A large number of institutions, scientific societies of Europe, 36 associated partners and more than 90 collaborating members, which were divided into ten work packages, participate in the EPAAC (see http://www.epaac.eu/).
The Region of Tuscany participates in this project as an associated partner in the WP7 “Healthcare” and is responsible for identifying and promoting good practices in oncology. The aim of the Tuscany Region is to collect and review the evidence on the use of CAM in cancer care and to propose criteria for the correct dissemination of information to clinicians, patients and decision-makers, to map the European Cancer Units of Hospitals which provide services of IO, including them in network activating synergies and permanent coordination among the centres.
Although the trend of use of CAM in cancer patients has long been investigated in several European countries, little is known about the presence of centres that offer these types of services in the different European countries.
Aim of the study
The aim of this study is to draw a preliminary mapping of the centres that provide services of integrative oncology to cancer patients across Europe, in order to create a European network of centres, experts and professionals constantly engaged in the field of integrative oncology and increase, share and disseminate knowledge and provide evidence-based healthcare to patients.
Material and methods
Study design and questionnaire
A cross-sectional descriptive survey design was used to collect data through a questionnaire that investigates the provision of IO therapies in cancer centres of 26 European countries.
The questionnaire consisted in 17 items inquiring about the general data of the centre, the year in which the integrative oncology activities were started, the kinds of CAM therapies provided to cancer patients (respondents could choose among acupuncture, traditional Chinese medicine, herbal medicine, homeopathy, homotoxicology, anthroposophic medicine, other specified CAM therapies), number of patients treated with IO therapies yearly, number of IO visits per year, use of therapeutic protocols, use of evaluation systems of results, field of application of the treatments provided (i.e. acupuncture for chemotherapy-induced vomiting), type of service (respondents could choose among public, operating within the national health system, private, other), studies/researches in progress and/or conducted by the centre.
Finally, we asked the respondents to mention any other integrative oncology centres they knew about (Fig. 1).
Identification of recipients
The centres were selected by convenience sampling: all the national health system oncology care centres in each European country identified were possible recipients of the questionnaire.
A search was conducted on websites and cancer- or CAM-related forums, visiting the website of each national conventional cancer centre or hospital with an oncology department. Moreover, some centres were identified through the analysis of international literature and contacts with CAM experts such as technical groups, working groups and CAM health professionals.
Finally, we requested the cooperation of associated partners of EPAAC WP7 and of relevant European cancer institutions such as the European Society for Medical Oncology (ESMO), eCancer, Organization of the European Cancer Institute (OECI) and European Cancer Organization (EcCO).
Inclusion criteria
Only the national health systems or those operating within the National Health System (covered by social insurance) and the European centres providing therapies of integrative oncology (in various forms, depending on the organisation of the national health system of each country) were included in the survey.
Exclusion criteria were as follows: individual doctors or small private medical clinics (even if offering IO therapies); centres like research institutes, which do not provide clinical activities; and extra-European centres.
Questionnaire management
The questionnaire was sent by email and was accompanied by an explanatory letter. It was sent to the person responsible for the clinical activity, usually the medical director of the centre. When it was not possible to identify the person by website or other information, the letter was sent to the general email address of the centre. In case of no reply after the first sending, the letter was sent a second time after 2 months and finally a third time in July, asking for an answer, even if negative.
Finally, the centres that did not answer were contacted by telephone twice at different times of the day; their websites were also analysed in order to find out if they were including a section on CAM.
Response management
The responses were archived either in paper or in electronic form; an electronic database was implemented containing the most relevant data of each integrative oncology cancer centre. A letter of appreciation was sent to the respondents. A separate list was also created of individual doctors, small private medical clinics and research institutes providing integrative oncology therapies, which had been excluded from the main survey.
Ethical approval
The survey did not include human information or material and therefore did not require any ethical approval.
Data analysis
The survey collects information from cancer centres of 26 European countries in a specified year. As it is inappropriate to perform formal statistical testing of the results, we applied a descriptive analysis of data.
Results
Survey achievement
Until 31 December 2013, the answers to the survey have been 123 (52.1 %) out of 236 centres contacted: 81.3 % filled questionnaires and 18.7 % answered by phone.
Ninety-nine out of 123 (80.5 %) responding centres met the inclusion criteria of the survey. Forty-seven out of 99 (47.5 %) responding centres meeting the inclusion criteria provide therapies in the field of integrative oncology. They correspond to 19.9 % of all the contacted centres (32.4 % of Italian centres and 14.1 % of European centres) (Table 1).
Furthermore, we point out that 12 centres which did not answer to the questionnaire, and for this reason not included in the sample, reported an offer of complementary medicine services in their website. However, they have not been included in our survey due to the lack of direct and verified information.
The completed questionnaires returned by the associated and collaborating partners of EPAAC were 16 (13.8 %); 14 of these meet the inclusion criteria and 3 provide IO therapies (6.4 % of the centres included in the survey).
Distribution of integrative oncology centres in Europe
A total of 23 out of 27 EU countries were contacted at the beginning of the survey. Switzerland, Norway and the Ukraine were also added, for a total of 26 countries. Of the EU countries, Bulgaria, Latvia, Luxembourg and Malta were not contacted because we could not identify any of the centres in these countries.
The countries more frequently contacted were Italy (31.4 % of the total), Germany (18.6 %), the UK (8.1 %), Spain (6.8 %), Switzerland (5.9 %) and France (5.1 %). The highest response rate was not only from Cyprus, Estonia, Hungary, Lithuania, Poland and Slovenia (100 % of contacted centres) but also Denmark, Finland, France, Ireland, Italy, Lithuania, the Netherlands, Norway, Portugal, Romania, Spain and Sweden which reported a response rate of at least 50 %.
A hundred percent of the respondent centres provide IO therapies in Austria, France and Lithuania, while 83.3 % in Switzerland, 70 % in Germany, 50 % in the UK and Sweden and 45.3 % in Italy.
No centre provides this type of therapy in Belgium, Cyprus, Denmark, Estonia, Finland, Hungary, Ireland, the Netherlands, Norway, Poland, Portugal, Romania, Slovenia and Spain.
We were unable to gather information about the non-respondent countries (Czech Republic, Greece, Ireland, Slovakia, Slovenia and Ukraine).
We can observe that most of the surveyed centres are located in central Europe (Fig. 2).
Characteristics of integrative oncology centres
The patients treated per year were on average 301.2, and the mean of visits provided per year was 1,335.6; this data is characterized by a very large variability expressed by the standard deviation in Table 2.
This variability is reflected in both the Italian and European data.
The number of public centres was 32 (68.1 %), private was 10 (21.3 %), those operating within the national health system were 2 (4.3 %) and other types of centres were 3 (6.4 %).
In Italy, public centres are prevalent (58.3 %), followed by private centres (29.2 %), other types of centres and centres operating within the national health system (respectively 8.3 and 4.2 %).
In the other European countries, the number of public centres is prevalent (78.3 %), followed by three private centres (13.0 %) and one of both operating within the national health system and other kinds of centres (4.3 %).
Among the centres providing IO therapies, 33 (70.2 %) reported to be using fixed protocols; this data is quite uniform in Italy (70.8 %) and Europe (69.6 %).
Thirty-five centres (74.5 %) reported to have systems for evaluation of the results. The number of centres that had studies/researches in progress or carried out until the deadline of the survey was 32 (68.1 %). The Italian centres reporting to have a system of evaluation of the results were 20 (83.3 %); this data is quite high compared to the other European countries (65.2 %). On the other hand, the centres of the other European countries demonstrated to be more active than Italy in the field of research as conducting more studies (19 centres of other European countries, 82.6 % and 13 Italian centres, 54.2 %) (Table 2).
Among the centres belonging to the group of other European countries, three of those included in the survey provide integrative oncology in more than one place. Another centre reported to have provided this service only in the past.
Complementary and alternative medicines offered to cancer patients
The CAMs more frequently provided in cancer care were acupuncture (55.3 %), followed by homeopathy (40.4 %), herbal medicine (38.3 %) and traditional Chinese medicine (36.2 %); anthroposophic medicine was provided by ten centres (21.3 %) and homotoxicology by six centres (12.8 %). In addition to the above-mentioned therapies, 30 centres (63.8 %) also offer other kinds of therapies.
Table 3 shows the different frequencies of CAMs used in Italy and in the other European countries. The most frequently provided CAM in Italy was acupuncture (70.8 %) followed by therapies classified as “others” (54.2 %), traditional Chinese medicine and herbal medicine provided with the same frequency (50 %), homeopathy (41.7 %) and homotoxicology (20.8 %). The least frequently offered CAM was anthroposophic medicine (8.3 %).
Among the centres belonging to the group of other European countries, the most frequent therapies offered were those classified as “others” (73.9 %) followed by acupuncture and homeopathy, which were provided with the same frequency (39.1 %); the fourth most frequently provided therapy was anthroposophic medicine (34.8 %), followed by herbal medicine (26.1 %) and traditional Chinese medicine (21.7 %). Unlike Italy, in this group, the less frequently offered CAM in the other European countries was homotoxicology, provided by only one centre (4.3 %).
We also report that five centres (10.6 %) offer only therapies classified as “other”.
As the number of centres providing this type of therapy is high, the data were stored in a separate file, although the findings were not initially interesting for the survey. The data were divided into five groups: biologically based methods, mind-body techniques, energy therapies, manipulation and body-based practices and health promotion according to the classification proposed by the Society of Integrative Oncology (SIO) [7]. Any attempt to classify a group of therapies and practices that are very heterogeneous and different among them is quite complicated; however, due to methodological reasons, we had to choose one classification.
Our purpose was mainly to assess the use of acupuncture, anthroposophic medicine, herbal medicine, homeopathy, homotoxicology and other techniques of traditional Chinese medicine in cancer care across European countries.
Among the above-mentioned groups, the most frequent therapies provided were mind-body techniques (42.5 %), followed by energy therapies (20.7 %) and biologically based methods (13.8 %); manipulation and mind-body practices are offered with the same frequency as health promotion (11.5 %).
Table 3 also shows the frequency of centres providing the therapies classified in the five above-mentioned groups. The most frequent category of therapies provided was that of mind-body techniques (33.3 %), the second of biologically based methods and energy therapies offered with the same frequency (19.3 %), health promotion (15.8 %) and manipulation and body-based practices (12.3 %).
The distribution of these therapies varied strongly in Italy and in the other European countries: in Italy, the two most frequent classes were the biologically based methods and energy therapies with the same frequency (26.9 %), followed by mind-body techniques (19.2 %), health promotion (15.4 %) and manipulation and body-based practices (11.5 %); among the group of other European countries, the most frequent class was that of mind-body techniques (45.2 %), followed by health promotion (16.1 %) and, with the same frequency, biologically based methods, manipulation and body-based practices and energy therapies (12.9 %). In this group, a clear difference can be observed between the mind-body techniques and the other classes. This does not happen in the group of Italian centres, where the mind-body techniques are only the third most frequent class.
Different complementary and alternative medicine associations offered by surveyed centres
The most frequent associations offering CAMs in the surveyed centres were acupuncture and traditional Chinese medicine (34.0 %), acupuncture and other therapies (31.9 %), acupuncture and herbal medicine (27.7 %), acupuncture and homeopathy, herbal medicine and homeopathy, herbal medicine and other therapies (25.5 %), anthroposophic medicine and other therapies (21.3 %), traditional Chinese medicine and other therapies, traditional Chinese medicine and homeopathy, traditional Chinese medicine and herbal medicine, homeopathy and other therapies (19.1 %).
The association between acupuncture and traditional Chinese medicine is mutually the most common. The most frequent association of anthroposophic medicine is with other therapies (21.3 %), of herbal medicine with acupuncture (27.7 %), of homeopathy with acupuncture and herbal medicine (25.5 %) and of homotoxicology with herbal medicine (12.8 %).
Use of complementary and alternative medicines in oncology
Table 4 shows all the fields of application of CAMs in the surveyed centres subdivided according to symptoms (of the cancer or the adverse reactions of anticancer therapy) and therapeutic aims, as reported in the questionnaires.
Treatments are mainly directed to reduce adverse reactions to chemo-radiotherapy (23.9 %), in particular nausea and vomiting (13.4 %) and leucopenia (5.0 %); medicines are also used to reduce pain and fatigue with the same frequency (10.9 %), to reduce side effects of iatrogenic menopause (8.8 %) and to improve anxiety and depression (5.9 %), gastrointestinal disturbances and leucopenia (5 %), sleep disturbances and neuropathy (3.8 %). A small percentage also reported the use of CAMs to reduce secondary infections and muscle disorders (0.4 %).
The most frequent aims of complementary treatments are as follows: improvement of quality of life (29.1 %), support during chemo-radiotherapy (24.1 %), reduction of perioperative disturbances (16.5 %), self-empowerment (10.1 %), psychological support (7.6 %), relapse prevention and palliative care (6.3 %).
Among the Italian centres, the most frequent use of CAMs is to reduce the adverse effects of chemo-radiotherapy (24.2 %), in particular nausea and vomiting (9.7 %) and xerostomia (1.6 %) were reported; to reduce pain (14.5 %); to reduce symptoms of iatrogenic menopause (12.9 %); to alleviate fatigue (11.3 %); to improve anxiety and depression (9.7 %); to reduce sleep disturbances and gastrointestinal symptoms (with the same rate of 6.5 %); and finally to improve neuropathy and muscle disorders (1.6 %). In Italy, no centre reported the use of CAMs for lymphedema, leucopenia, mucositis, diarrhoea, constipation and secondary infections.
As concerns the aims of the treatments, the most frequent were support during chemo-radiotherapy, improvement of quality of life and reduction of perioperative disturbs (all with the same rate 24 %), self-empowerment (16 %), relapse prevention (8 %) and palliative care (4 %). No Italian centre reported the use of such treatments for psychological support.
Among the centres of the other European countries, CAMs are mostly used to reduce the adverse reactions of chemo-radiotherapy (22.2 %), as in Italy, in particular nausea and vomiting (14.3 %), leucopenia (6.3 %), xerostomia (2.1 %), lymphedema and mucositis (with the same rate of 1.1 %); CAM treatments are also used to reduce pain (11.1 %) and fatigue (10.6 %), to relieve symptoms of iatrogenic menopause (6.9 %), neuropathy, gastrointestinal symptoms and anxiety and depression (with the same rate of 4.2 %) and to reduce sleep disturbances (2.6 %) and finally secondary infections (0.5 %). Muscle disorders are not reported by any centre.
The most frequently identified aims of CAM treatments were to improve quality of life (27.5 %), provide support during chemo-radiotherapy (25.5 %), alleviate perioperative disturbances (13.7 %), offer psychological support (11.8 %), provide palliative care and develop self-empowerment (7.8 %) and relapse prevention (5.9 %).
Limitations and strengths
Selection bias
The main bias of this study is probably represented by the modalities of the survey, especially designed to identify the healthcare structures where to send the questionnaire, and the centres that could host integrative oncology services or provide CAMs in cancer care and, connected to this, the relatively low response rate of the questionnaire originally delivered by postal mail.
In the first phase of the study, we tried to identify the largest possible number of oncology care centres across Europe. Unfortunately, we were unable to find a complete list of the centres. To this list we added the most important cancer hospitals and oncology care centres already known to provide CAMs, since tools available did not allow to identify cancer units in European hospitals. For this reason, the survey is not exhaustive, as confirmed by other surveys conducted at a national level [9]. However, according to the authors also, this data could be underestimated.
Another problem was the prevalence in the final results of Italian centres compared to those of other European countries. There is in fact a substantial parity in the number of integrative oncology care centres in Italy and in the all other European countries. These outcomes could in part be considered as a consequence of the sample bias of the survey, due to a better knowledge of the Italian situation and also to the primary commitment of Tuscany in the integration of CAMs in the regional health system.
Information bias
The response rate depends, in part, on the completeness of the website of each centre for which the information was found; it was not very simple to identify a responsible person for each centre to whom the questionnaire was to be addressed. Moreover, we cannot be sure that each questionnaire was filled adequately since this survey was based on the answers concerning the use of CAMs in cancer care, as provided by the responders of each centre. When we could not directly contact the person responsible for the CAM centre, the questionnaire was sent to a general info-mail of the centre. This implied that the contacted person could be unaware of the availability of CAM in their centre. For this reason, we suppose that the offer of CAMs in some centres may not have been fully reported and as a consequence that the general data may have been underestimated.
Finally, the situation is likely to be constantly changing with obvious consequences also on data updating.
Strengths
The main value of this study was that it was the first time a European survey had been conducted on the centres providing CAM in cancer care. So far, this issue had always been investigated either from the patients’ point of view [3, 8–10] or by contacting the cancer units or CAM centres in each European country [11].
Despite the above-mentioned limitations, this perspective could offer a more objective picture of CAM use across Europe. This kind of study has permitted to collect data not only on the use of CAM among cancer patients in the various countries but also on the therapeutic aims and symptoms most frequently treated by CAM therapies. Other information includes some organisational characteristics of the centres, such as temporal growth of integrative oncology centres over the years, as well as possible use of therapeutic protocols and evaluation systems of the results.
Discussion
The results of this survey can provide a very general idea on the offer of CAMs in cancer care (“integrative oncology”) in oncology care centres and CAM centres across Europe.
According to the results of our survey (filled questionnaires received and identification of a section on CAM in the websites of non-responding centres), it is possible to assume that a relatively high proportion (around 20 %) of the European oncological centres in our list provide some form of complementary therapy in cancer care.
Furthermore, the offer of integrative oncology services in European countries is very heterogeneous and can be considered proportionally lower than expected, taking into account the widespread use of CAMs among European patients and therapists. Unfortunately, this data can hardly be matched with other studies investigating the European situation. As a matter of fact, also the data and studies about CAM prevalence in Europe are very heterogeneous in terms of prevalence rate, sample sizes, definitions and time periods over which CAM use has been measured, as pointed out by a recent systematic literature review on CAM offer in European countries [12].
Therefore, our research has discovered that in most cases, the countries for which we collected the largest number of integrative oncology centres are the same for which a high prevalence in the use of CAM has been reported, such as Germany, Italy, Switzerland, Sweden and the UK. However, we received no positive responses from Denmark, Finland, Norway and Spain, for which a relatively high prevalence in the use of CAM has also been reported [12].
In any case, our map of the countries where IO centres are more numerous can be overlapped, with some differences, with the most recent maps of the European countries where the regulation of CAMs is more advanced and their historical tradition is stronger. However, the areas of Eastern and Northern Europe are underrepresented in our survey, considering that CAMs have been regulated in many of those countries, as reported by the above-mentioned research [13].
By comparing this data with the results of the only European-wide survey on the use of CAMs in cancer patients published so far [7], it shows that the most frequent CAM users in cancer care are the Italians. Our data partly seems to confirm this trend, but it should be emphasized that other authors have reported a lower percentage in Italy [14].
The fragmented and inhomogeneous distribution of IO centres across European countries observed in our survey could be explained not only with the selection and information bias already explained but also with the high heterogeneity in the field of legislation and regulation of CAMs [13]. This regulatory diversity can influence the offer of IO and also the demand of these therapies by the patients. However, the relatively low number of centres included in the survey could also reflect problems of communication between oncologists and CAM practitioners. This seems particularly true for cancer departments in which the integration of CAMs may also be limited, owing to the fear of oncologists to give unreasonable hopes and false promises to their patients.
In agreement with the increase in the studies on CAM in general [15], there has also been an increase in IO centres since 2000. Many centres included in our research have started their activity in the last 10 years, with a relevant increase in the use of CAMs in Europe, as reported in literature [16]. In the same period also, orthodox medicine has shown a greater interest in the contribution of CAMs, also due to the development of scientific research and evidence in this field.
Among the surveyed centres, there is also a great difference in the number of patients visited and number of visits provided yearly. This could depend not only on the different size of the oncology care centres in which the activity is located but also on the level of integration of complementary medicine in mainstream medicine. The more the IO structure is connected to the oncology department (i.e. whether or not it is located nearby and/or whether the patients are sent by conventional oncologists to an integrative oncology unit), the larger could be the number of CAM users.
According to the above-mentioned study about CAM use in Europe [12], the most popular CAMs are medicinal herbs; the same data is reported by Molassiotis et al. for cancer patients [3].
Instead, in our study, the most frequently provided CAMs in cancer care were acupuncture, followed by homeopathy and herbal medicine. However, this difference can be explained by the fact that the CAMbrella project data resulted from a systematic review of studies published in literature, where CAMs are variously categorized. Moreover, the use of CAM among the general population could be different from that of cancer patients, and finally, it is also possible that herbal preparations are less used due to the fear of potential adverse interactions with anticancer drugs.
Furthermore, the offer of CAMs in the surveyed oncological care centres seems to be more connected to the evidence of these therapies in cancer care as published in literature. Our data about the most frequently provided CAMs to cancer patients showing that acupuncture is the most common among the various integrative medicines seems to confirm the literature. As a matter of fact in these studies, acupuncture and the other traditional Chinese medicine techniques are generally considered to have the highest number of clinical studies, RTCs, reviews, meta-analyses and the most significant results.
According to the results of this survey, CAM in cancer care is mainly used in treatments to reduce adverse reactions to chemo-radiotherapy and side effects of hormonal treatments and to improve the quality of life of cancer patients. According to Molassiotis et al. [3], only 24.8 % of patients use CAM to counteract the adverse effects of cancer or medical treatments, whereas most patients use them to increase body’s ability to fight the disease (50.7 %) and improve physical (40.6 %) or emotional well-being (35.2 %).
The aim of reducing the adverse reactions to anticancer therapies can be the immediate and common purpose of both cancer department oncologists and complementary medicine practitioners. CAMs are known to have a very limited toxicity, and if they can be used successfully to reduce the adverse effects of anticancer therapy without causing additional drug toxicity, then the dose of anticancer therapy could be increased, together with the compliance of patients to conventional treatments.
More than 50 % of the surveyed centres are committed to research. This commitment could increase knowledge in the field of IO in the next future and therefore provide more evidence-based therapies to cancer patients filling the gap of knowledge of the medical community about the possibility to include effective CAM treatments in cancer care.
Finally, our study allowed us to obtain essentially “quantitative” data. We can say nothing, or very little, about the modes of integration adopted in the different centres, in other words which of the different models of integration proposed by Boon and colleagues [17] have been adopted.
Therefore, it is necessary in the future to make a comparison and a higher quality investigation into the various integrative approaches that have been censed, taking into account the key elements identified by Ben-Arye et al. as essential for integrative programme design within oncological supportive care: location of the integrative physician (IP) room within the oncology department area; required oncologist referral to CM consultation; allocated time to IP-oncologist communication; research-based integrative practice; and inclusion of paid professional CM practitioners and institutional cost-covered service [18].
Recently, another comparison has been made between Germany and the USA [19, 20]. Both countries identify themselves with the general principles of integrated oncology, in an attempt to provide the patient with the “best of both worlds” in oncology and integrative medicine, focusing on research and safety, evidence-based treatments and a patient-centred approach.
Moreover, we agree on the need that these authors have expressed to educate promptly physicians expert in integrative oncology in order to facilitate the communication between oncologists and CAMs as it already happens in some healthcare centres. In fact, complementary therapies are now even included worldwide in the curricula of many medical schools, including such prestigious schools as for instance Stanford University Medical School, the Harvard Medical School in the USA and the Charité University Medical Centre in Berlin, Germany, to name a few.
Conclusions
The results of this survey have led to a first preliminary map of the integrative oncology centres in Europe. They show that these kinds of services are spread in various European countries. The offer is quite heterogeneous in terms of presence in territories and offer of services and organisational modalities but still seems largely insufficient considering the use of CAMs among cancer patients.
The current study provides a baseline on which future research might be built: further research is needed to obtain more information on the CAM services provided to cancer patients.
In the perspective of the forthcoming European Programme on cancer: “Con CAN 2014-16”, the next step of this work could be extending the mapping of the European centres of integrative oncology to the main hospitals with cancer departments of the national healthcare system in each country.
The purpose for the future is to foster EU collaboration in integrative oncology and to create a “European Network of Integrative Oncology” to connect permanently the European centres providing CAMs and IO to cancer patients, starting from those surveyed for EPAAC. The common aim could be to conduct multicentre clinical trials and activities of research and to draft and disseminate the recommendations on the use of complementary medicines in cancer care.
References
Ernst E, Cassileth BR (1998) The prevalence of complementary/alternative medicine in cancer. A systematic review. Cancer 83:777–782
Horneber M, Bueschel G, Dennert G et al (2012) How many cancer patients use complementary and alternative medicine: a systematic review and meta-analysis. Integr Cancer Ther 11:187–203
Molassiotis A, Fernadez-Ortega P, Pud D et al (2005) Use of complementary and alternative medicine in cancer patients: a European survey. Ann Oncol 16:655–6
Sagar SM (2008) The integrative oncology supplement—a paradigm for both patient care and communication. Curr Oncol 15:166–7
Cassileth BR, Deng G, Vickers AJ et al (2005) Integrative oncology: complementary therapies in cancer care. BC Decker, Hamilton Ontario, Canada
Sagar SM (2006) Integrative oncology in North America. J Soc Integr Oncol 4:27–39
Deng GE, Frenkel M, Cohen L, on behalf of the Society for Integrative Oncology et al (2009) Evidence-based clinical practice guidelines for integrative oncology: complementary therapies and botanicals. J Soc Integr Oncol 7:85–120
Gansler T, Kaw C, Crammer C, Smith T (2008) A population-based study of prevalence of complementary methods use by cancer survivors: a report from the American Cancer Society’s studies of cancer survivors. Cancer 113:1048–57
Ernst E, White A (2000) The BBC survey of complementary medicine use in UK. Complement Ther Med 8:32–6
Scott JA, Kearney N, Hummerston S (2005) Use of complementary and alternative medicine in patients with cancer: a UK survey. Eur J Oncol Nurs 9:131–7
Egan B, Gage H, Hood J et al (2012) Availability of complementary and alternative medicine for people with cancer in the British National Health Service: results of a national survey. Complement Ther Clin Pract 18:75–80
CAM use in Europe—the patients’ perspective. Part I: a systematic literature review of CAM prevalence in EU. CAMbrella 2012. https://phaidra.univie.ac.at/detail_object/o:292161 (accessed in August 2014)
Legal status and regulation of CAM in Europe. Part I: CAM regulations in the European countries. CAMbrella 2012. https://phaidra.univie.ac.at/detail_object/o:291583 (accessed in August 2014)
Johannessen H, von Bornemann HJ, Pasquarelli E et al (2008) Prevalence in the use of complementary medicine among cancer patients in Tuscany, Italy. Tumori 94:406–10
Salomonsen LJ, Skovgaard L, La Cour S et al (2011) Use of complementary and alternative medicine at Norwegian and Danish hospitals. BMC Compl Alt Med 11:4
PubMed. Complementary and alternative medicine. Results by year. http://www.ncbi.nlm.nih.gov/pubmed/?term=complementary+and+alternative+medicine (accessed in December 2013)
Boon H, Verhoef M, O’Hara D, Findlay B (2004) From parallel practice to integrative healthcare: a conceptual framework. BMC Health Services Research vol. 4, article 1
Ben-Arye E, Schiff E, Zollman C, Heusser P, Mountford P, Frenkel M, Bar-Sela G, Lavie O (2013) Integrating complementary medicine in supportive cancer care models across four continents. Med Oncol 30(2):511. doi:10.1007/s12032-013-0511-1
Cramer H, Cohen L, Dobos G, Witt CM (2013) Integrative oncology: best of both worlds—theoretical, practical and research issues. Evid Based Complement Alternat Med 2013:383142
Mittring N, Pérard M, Witt CM (2013) Corporate culture assessments in integrative oncology: a qualitative case study of two integrative oncology centres. Evid Based Complement Alternat Med 2013:316950
Acknowledgments
This publication arises from the European Partnership for Action Against Cancer (EPAAC), which has received funding from the European Union through the Executive Agency for Health and Consumers of the European Commission, in the framework of the Health Programme 2008–2013.
The European Commission is not responsible for the content of this publication and has had no role in the elaboration or the writing process of the document.
We would like to acknowledge and thank the following people for their contribution to this work: Emanuela Portalupi and Paolo Fedi; Laura Cignoni for her support in the English translation; and José Maria Borras Andres and Joan Lluís Prades Perez and all the associated and collaborating members of EPAAC for their collaboration.
Conflict of interest
The authors declare that they have no competing interests. All the costs for this study were supported by the European Union and the Tuscany Region.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rossi, E., Vita, A., Baccetti, S. et al. Complementary and alternative medicine for cancer patients: results of the EPAAC survey on integrative oncology centres in Europe. Support Care Cancer 23, 1795–1806 (2015). https://doi.org/10.1007/s00520-014-2517-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-014-2517-4






 one integrative oncology centre
one integrative oncology centre