Summary
On 11 March 2020 the World Health Organization (WHO) declared a status of global pandemic caused by the new severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (coronavirus disease 2019, COVID-19). The pandemic is currently underway, and to date has caused approximately 2.42 million deaths worldwide. The first vaccines have recently been licensed; however, research continues to identify therapeutic agents to prevent serious complications, such as anti-inflammatory, immunomodulatory, anticoagulant or antiviral agents authorized for other therapeutic indications. Epidemiological evidence shows that advanced age and comorbidities, such as diabetes, heart disease, and dyslipidemia may represent COVID-19 risk factors. In particular, in patients with hypercholesterolemia treated with statins, it is recommended that treatment should not be discontinued if COVID-19 infection occurs. The pleiotropic effects of statins are well known. In this brief review, we propose that the use of statins can potentially protect against SARS-CoV-2-induced tissue damage and improve lung function in COVID-19 patients through several pleiotropic effects. Pleiotropic effects of statins that may be a significant benefit in patients with hypercholesterolemia treated with statins and COVID-19 positive. Recent evidence shows promising results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
SARS-CoV-2 (COVID-19)
In November 2019 a new coronavirus was identified as the cause of a number of severe pneumonia cases in Wuhan, China. The virus designated as coronavirus‑2 is responsible for severe acute respiratory syndrome, SARS-CoV‑2 (coronavirus disease 2019, COVID-19). The virus has rapidly spread worldwide. In March 2020, the World Health Organization (WHO) proclaimed the status of a global pandemic by COVID-19, to date there are about 2.42 million deaths and 109 million infected persons [1]. The SARS-CoV‑2 is an RNA (ribossinucleid acid) virus similar to SARS-CoV (responsible for the 2003 outbreak) for about 80% of the viral genome [2]. In vitro studies confirmed that the virus penetrates human cells by binding to the protein angiotensin conversion enzyme 2 (ACE-2), which is part of the renin-angiotensin system (RAS) [3] and is considered a possible receptor of the protein. It is also known that patients infected with this virus have changes and variations in the concentrations of the enzyme components of RAS [4, 5] during illness days. A SARS-CoV‑2 infection may have an asymptomatic or symptomatic course. In a percentage of cases, however, the infection has a course consisting of an initial asymptomatic or slightly symptomatic phase and subsequent phases characterized by a generalized inflammatory state that causes multiorgan tissue lesions and respiratory distress syndrome [6]. The generalized inflammatory state responsible for severe lesions is caused by an overactivation of the components of the host inflammatory/immune system characterized by a sudden and high release of cytokines, an event called a cytokine storm that leads to severe and sometimes fatal tissue damage. Since a few months the first vaccines have been authorized, in the case of a positive COVID-19 case ongoing treatments for other diseases should be continued to avoid serious complications [7,8,9,10,11].
Clinical manifestations
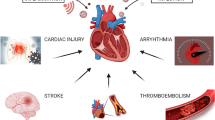
The SARS-CoV‑2 is transmitted from person to person. In most cases the incubation period is about 5 days after exposure and in some cases it can be as long as 15 days [12]. Bilateral interstitial pneumonia seems to be the most frequent serious manifestation of infection characterized by coughing and dyspnea [13]. The infection may also have a totally asymptomatic or slightly asymptomatic course; however, the manifestation of upper respiratory tract symptoms, myalgia and fatigue, diarrhea, and disturbances of the sense of smell are common [14]. Epidemiological evidence shows that fever is present in about 90% of hospitalized COVID-19 patients [13]. In some studies, smell and taste disorders have been reported in about 50% of COVID-19 positive patients [14, 15]. A smaller percentage of COVID-19 positive patients experience gastrointestinal symptoms, such as nausea and diarrhea [16]. Cases of dermatological reactions such as rashes and hives have also been reported [17]. A SARS-CoV‑2 infection can cause several serious complications: acute respiratory distress syndrome (ARDS) is the major complication in COVID-19 positive patients [16]; however, in addition to the respiratory system, other organs may also be affected, particularly the cardiovascular system. Epidemiological data report cases of acute cardiac lesions from COVID-19 [18]. Thromboembolic complications including pulmonary embolism have also been reported [19]. Some cases reported liver lesions caused by COVID-19 [20]. The presence of lesions of the lungs and other organs such as the heart or liver appears to be caused by direct or indirect damage of the virus. As described above SARS-CoV‑2 uses the entry receptor ACE‑2, a protein expressed in several tissues, in type II pneumocytes, heart cells, liver cholangiocytes [21], which may be responsible for direct tissue damage caused by the virus; however, in the most severe stages of COVID-19 infection, a cytokine storm [22] can be generated that is responsible for organ lesions, in particular the formation of fibrotic tissue, such as pulmonary fibrosis, myocardial fibrosis, or liver fibrosis observed in some cases of COVID-19. [23, 24].
Risk factors in COVID-19 patients
Epidemiological evidence has shown that the severity of viral infection can vary greatly from subject to subject depending on various factors. As described in fact, some individuals may be totally asymptomatic, others may represent cases with a severe course, and in some cases fatal. The risk of serious complications from COVID-19 is increased in older people and/or with pre-existing diseases, in particular pulmonary, cardiac, metabolic diseases and weakening of the immune system may represent an important risk factor. Pulmonary diseases such as COPD (chronic obstructive pulmonary disease), asthma, cystic fibrosis can make the respiratory tract vulnerable to serious injuries from COVID-19 [25]. Diseases such as diabetes and obesity may reduce the efficiency of the immune system, heart diseases such as ischemic heart disease or heart failure may make the heart susceptible to serious injury from COVID-19, considering that SARS-CoV‑2 itself may cause damage to cardiac tissue. The presence of hypercholesterolemia can also be a risk factor. The development of atherosclerosis may predispose to acute coronary syndrome, a COVID-19 infection may further complicate the scenario and increase the risk of myocardial ischemia [26,27,28].
Statins
The inhibitors of hydroxy-methylglutaryl-coenzyme A (HMG-CoA) reductase, the statins, have been used for many years with undoubted therapeutic efficacy in the management of hyperlipidemia and in the prevention of atherosclerotic vascular diseases, in particular acute coronary syndromes [29, 30]; however, the therapeutic benefits of statin treatment are not only related to lowering endogenous cholesterol, suggesting that other effects and mechanisms come into play. Numerous experimental and clinical trials in recent years have led to the widely accepted scientific concept of pleiotropic effects of statin treatment independent of HMG-CoA inhibition, including restoration of endothelial dysfunction, stabilization of atherosclerotic plaques, regulation of angiogenesis, antifibrotic, antithrombotic and antifibrotic effects [31]. The pleiotropic effects of statins may result in potential therapeutic benefits in the patient under treatment and COVID-19 positive, particularly for properties in thrombotic manifestations that may occur in the more severe stages of SARS-CoV‑2 infections. (Fig. 1).
Pleiotropic effects of statins and COVID-19
Reducing LDL (Low Density Lipoprotein) and cardiovascular protective effects
The therapeutic efficacy of statin treatment and associated pleiotropic effects can indirectly preserve or reduce cardiac damage that can occur in severe COVID-19 patients [18]. Well-known epidemiological evidence indicating the protective effect of statin treatment on the cardiovascular system is also potentially useful in cases of severe COVID-19 infection; however, the clinical significance of the pleiotropic effects of statins in the cardiovascular system remains controversial and has yet to be fully clarified, given the enormous benefits of cholesterol reduction in the prevention of cardiovascular events. As described above, cardiac lesions can occur in severe COVID-19 positive patients, in particular cases of acute coronary syndrome (SCA), arrhythmia, edema, pericarditis, acute heart failure have been reported. An SCA can be a serious complication caused by COVID-19 infection in patients without or with pre-existing cardiovascular risk factors. The basic mechanism by which COVID-19 causes these effects remains questionable. It has been proposed that COVID-19 may induce a prothrombotic state, as supported by high levels of factor VIII, fibrinogen and d‑dimer [32, 33]. Some interesting evidence associates antithrombotic properties to the statins. In addition, statins can have a reducing effect on cardiac fibrosis, hypertrophy, and pathologic remodeling in response to angiotensin II (Ang II) in a Rho/ROCK dependent manner [34,35,36]. Increased ROCK (Rho-associated protein kinase) activity is observed in patients with hypertension, pulmonary hypertension, metabolic syndrome, dyslipidemia, acute coronary syndrome (CAD), coronary vasospasm, left ventricular hypertrophy (LVH), and in heart failure with reduced systolic function [37,38,39]. The ROCK inhibition is a candidate for mediating pleiotropy of statins. The effect of statins on the myocardium mediated by RhoA and ROCK is of paramount importance because both lead to increased apoptosis and increased fibrosis, which could lead to development of LVH and heart failure. Endothelial dysfunction can be caused by hypercholesterolemia and is characterized by reduced bioavailability of endothelial nitric oxide (NO). Endothelial NO is important for vasodilation, platelet aggregation, vascular smooth muscle proliferation and leukocytic endothelial interactions. Statins increase endothelial NO production, in part by increasing endothelial NO synthase (eNOS) [40, 41]. Statins increase the bioavailability of NO, which increases myocardial blood flow under hypoxic conditions and inhibits interleukin 6 (IL-6), IL‑8 and the adhesion molecule of vascular cell‑1 (VCAM-1). In vitro studies show that statins reduce mitochondrial dysfunction and death of cardiomyocytes [42]. Several studies have described a protective effect of 3‑hydroxy-3-methylglutaryl-coenzyme A reductase inhibitors (statins) against ventricular arrhythmia and sudden cardiac death. Statins reduce inflammation, a known risk factor for sudden death and ventricular arrhythmia [43, 44]. An overactive inflammatory state, as may occur in severe COVID-19 phases, alters the autonomic tone measured by heart rate variability, which may partly explain these associations of inflammation and arrhythmic outcomes. Statins have documented effects on autonomic activation, improving heart rate variability and desensitizing myocytes to beta-adrenergic stimulation [45].
Anti-inflammatory and immunomodulatory effects
Recently numerous in vitro and in vivo evidence has associated direct anti-inflammatory effects that are not mediated by their hypocholesterolemic activity. The evidence is further supported by observations that statin treatment lowers the C‑reactive protein (CRP), a marker of inflammation, regardless of the lipid-lowering effect [46, 47]; however, there are still many aspects to be clarified on the anti-inflammatory effect of statins. Some studies showed that statins inhibit leukocyte recruitment. The activity on leukocyte migration is probably related to the reduction of chemokines and IL‑6 cytokine [48]. In addition, statin treatment can improve NO release from the endothelium and downregulatee endothelial P‑selectin [49]. An increasing amount of in vitro and in vivo evidence associates the antispasmodic effects of statins with the key concept of modulation of the leukocyte adhesion cascade. Based on these considerations, statins inhibit both acute and chronic cholesterol-inhibiting inflammation independently by exerting their anti-inflammatory effect by interfering with the adhesion and transendothelial migration of leukocytes to sites of inflammation. In addition, it seems that the inhibition of the activation of the integrins is related to the reduced geranylgeranylation of Rho [50]. By blocking the activity of Rho GTPase the statins prevent ICAM‑1 expression in endothelial cells [51]. Other evidence shows that by inhibiting the geranylgeranylation of Rho GTPase the statins induce the expression of eNOS[52,53,54,55]. Finally statins are associated with cytokine and chemokine release inhibition effects by regulating nuclear receptors, proliferator of the activated peroxisome receptor α (PPAR-α) and PPAR‑γ. Other studies indicated that statins could modulate the adhesion of leukocytes by interfering with the path of nuclear factor κB (NF-κB) [56, 57]. In the most severe stages of COVID-19 infection a hyperactive and generalized inflammatory state may be responsible for the most severe complications, in this direction the pleiotropic anti-inflammatory effects, particularly in endotheliitis by statins, could prove to be therapeutically effective [58,59,60,61].
Antiviral effects
Some studies have attributed direct cholesterol-dependent or non-cholesterol-dependent antiviral effects to statin treatment. In fact, in this direction, many studies suggested that statins, due to their pleiotropic properties, may be beneficial for the treatment of viral infections and their complications. Some evidence has shown that statins can exert direct antiviral effects, blocking the intracellular production of cholesterol and intervening directly on the infectious cycle of viruses [62]. Moreover, as described above statins reduce geranylgeranyl pyrophosphate (GGP) and farnesyl pyrophosphate isoprenoids, which are necessary for the prenylation of proteins such as Rho and Ras GTPase; in particular the latter proteins are associated to the regulation of the life cycle of viruses. This evidence has been supported by some studies that have shown that statins may have some antiviral potential against HCV (hepatitis C virus). In fact, statins have been shown to block viral replication against HCV when used in association with interferon [62,63,64]. By reducing the availability of cholesterol, statins may represent possible candidates to interfere with virus fusion and entry into host cells. How much this evidence can also be associated with an anti-SARS-CoV‑2 activity is to be demonstrated. A suggested mechanism could be that membrane cholesterol reduction prevents normal ACE2-spike interactions.
Antifibrotic effects
Many studies have suggested that statins have antifibrotic effects on liver and lung tissue and decrease portal hypertension. One of the antifibrotic mechanisms of statins is the reduction of proinflammatory mediators, as described above, which can induce tissue fibrosis; however, it seems that other pathways are involved. In particular, the reduction and decrease in activity of profibrotic factors such as TGFβ1 (Transforming growth factor β1), CTGF (Connective tissue growth factor) and PDGFβ (platelet-derived growth factor-β) are associated with statins. Moreover, by decreasing the RhoA pathway and its downstream Rho-kinase effector, collagen synthesis and liver fibrosis are reduced. Finally, a greater availability of statin-mediated NO causes a decrease in intrahepatic resistance and portal pressure [65, 66]. The hyperactive inflammatory state caused by COVID-19 infection may also be responsible for the formation of fibrotic tissue, in particular pulmonary fibrosis that could cause serious complications. Characteristics of pulmonary fibrosis pathogenesis are cell proliferation, collagen deposition and differentiation of fibroblasts into the profibrogenic phenotype of myofibroblasts, these processes are mainly mediated by connective tissue growth factor (CTGF), an autocrine growth factor induced by TGF-b1. Some evidence suggests that statins could modify the critical determinants of profibrogenic mechanisms and potentially prevent pulmonary parenchymal remodeling associated with the formation of myofibroblasts by inhibiting the expression of the CTGF gene after TGF-b1 induction [67, 68].
Antithrombotic effects
Treatment with statins has been associated with antiplatelet and anticoagulant effects, independent of cholesterol lowering. A decrease in platelet activity is through an increase in NO, which is a powerful inhibitor of platelet aggregation. In addition, the administration of statins has been shown to decrease the expression and activity of tissue factor (TF) in monocytes and macrophages [69]. Thrombomodulin acts as a cofactor of thrombin in the process of activation of protein C (APC), which proteolytically inactivating the activated factors V and VIII plays an anticoagulant role. The statins have been shown to increase the expression of anticoagulants TM (thrombomodulin), APC (activated protein C) [70].
Increasing ACE-2
The intracellular input receptor used by SARS-CoV‑2 is the angiotensin-conversion of enzyme 2 (ACE-2), expressed in pulmonary, hepatic and cardiac tissue. The ACE‑2 is an important regulatory enzyme in the renin-angiotensin system (RAS), catalyzing the conversion of angiotensin II (AT-II) to angiotensin 1–7 (AT 1‑7). The AT 1–7 oppose the effects induced by AT-II, with antioxidant, anti-inflammatory, antifibrotic and vasodilator action. It is also known that SARS-CoV‑2 infection in the most severe stages causes a reduction in ACE‑2. This effect can increase the likelihood of lung injury, which can be fatal in some cases. Ultimately, ACE‑2 plays a dual role in COVID-19 infection, the first as a protector against the damaging effects of hyperinflammatory response, the second as an input receptor for SARS-CoV. Statins have been the first choice in the treatment of hypercholesterolemia for years. Studies have shown an increase in ACE‑2 expression after statin treatment. Important questions arise. If statins increase ACE‑2, can they be a risk factor for SARS-CoV‑2 infection? Or, in severe stages of infection, can the increase in ACE‑2 be an additional protection value? To date, it is not clear how clinical results in patients with COVID-19 are affected by the use of statins, alone or in combination with ACE inhibitors and ARBs (angiotensin receptor blocker). Well-structured clinical studies are needed [71,72,73].
Clinical evidence and COVID-19 patients
Several studies have compared the outcomes of COVID-19 infections in patients who take statins with those who do not. The results have been encouraging, generally suggesting that statin use does not cause worsening health outcomes. Notably, in some studies, statin use was associated with fewer deaths. One retrospective observational study showed that statin use in hospitalized subjects with COVID-19 was associated with a lower risk of all-cause mortality and a favorable recovery profile. Because of the nature of such retrospective studies, these findings should be interpreted and considered with due caution; however, these data also provide evidence supporting the safety of statins as monotherapy or in combination with ACEi/ARBs in patients with COVID-19 [74]. Another retrospective observational study showed slower progression to death associated with atorvastatin in patients with COVID-19 [75]. The current preliminary results suggested a 30% reduction in fatal or severe disease and discredited the suggestion of harm with statin use in patients with COVID-19. Much remains to be determined about the statin regimen for the treatment of COVID-19, although available evidence suggests that moderate to high intensity statin treatment may be effective [76]. Another retrospective study showed that statin use during the 30 days before hospitalization for COVID-19 was associated with a lower risk of developing severe COVID-19 and a faster recovery time among patients without severe disease [77]. Another retrospective study showed that in patients with hyperlipidemia, statin use was independently associated with fewer ICU admissions. This supports the current practice of continuing statin prescribing in patients with COVID-19 [78] but although the results of these studies are interesting and important, they cannot answer the question of whether statins can treat COVID-19 [79]. Recent evidence has also associated novel PCSK‑9 (Proprotein convertase subtilisin/kexin type 9) inhibitors with cardiovascular pleiotropic effects; one might speculate that their long-term use before infection may also play a protective role.
Interactions of statins and COVID-19
Statins are drugs well tolerated at the common doses used in the treatment of hypercholesterolemia; however, like any drug, they are not free from potential adverse reactions. The patient with severe COVID-19 is a complex patient, who may have organ lesions, in particular liver and kidney with modified statin metabolization and excretion, increased circulating concentrations, and increased risk of inducing adverse reactions, such as myotoxicity and rhabdomyolysis. Rhabdomyolysis may further create kidney damage [80].
In addition, old COVID-19 patients may have further decreased liver and kidney clearance, making the scenario more complicated. In addition, as described above, a potential increase in ACE‑2 concentration caused by statin treatment could represent a COVID-19 risk factor, as the virus would find a higher amount of transmembrane cellular input receptor. In this direction, however, there is no certain epidemiological evidence and studies are necessary. Moreover, most of the available statins are substrate for the cytochrome P450 (CYP) system, in particular 3A isoenzymes and P‑glycoproteins (P-gp). Antivirals used in the COVID-19 positive patient (e.g. lopinavir, darunavir) are potent inhibitors of CYP3A and P‑gp, and their concomitant administration can cause a marked increase in statin exposure with potential toxic effects [81]. The patient with COVID-19 infection, is a complex patient, the benefit/risk ratio of the pharmacological agents used must be carefully monitored avoiding any adverse reactions that may complicate the scenario [82,83,84,85,86].
Conclusion and perspectives
Statins are drugs of undoubted therapeutic efficacy and with a good tolerability profile. Current guidelines recommend not to stop treatment in cases of COVID-19 positivity. The pleiotropic effects of statins can represent an added value in patients on statin treatment of hypercholesterolemia and COVID-19 positive. Well-structured epidemiological studies are necessary to generate further evidence on this topic.
These effects include combating SARS-CoV-2-induced inflammation and cytokine storm, inhibition of cellular trafficking through the autophagy pathway, mediation of ACE‑2 expression, and decreased extracellular matrix biosynthesis and scar formation in COVID-19 patients. Our current work may have some different results from those reported in the study in China, probably because of differences in the number (limitation of our current study) and genetic background of patients involved. Although we could not demonstrate a significant association between statin use and a reduction in COVID-19 mortality, our results are promising and clinically relevant and warrant the need for prospective randomized controlled trials and large retrospective studies in large and diverse patient populations to further evaluate the potential beneficial therapeutic effects of statin treatment on clinical symptoms and mortality rates associated with COVID-19. We hypothesize that long-term statin use prior to infection could represent a strong adjuvant therapeutic strategy but clinical studies are needed.
References
World health organization (WHO). Situation Reports September 2020.. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports. Accessed 10 February 2021.
Wu Y. Compensation of ACE2 function for possible clinical management of 2019—nCoV-Induced acute lung injury. Virol Sin. 2020; https://doi.org/10.1007/s12250-020-00205-6.
Guoping L, Xiang H, Lei Z, Qin R, Junyi W, Anying X, et al. Assessing ACE2 expression patterns in lung tissues in the pathogenesis of COVID-19. J Autoimmun. 2020;13:102463. https://doi.org/10.1016/j.jaut.2020.102463.
Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel Coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199.
Vitiello A, Ferrara F. Correlation between renin-angiotensin system and severe acute respiratory syndrome Coronavirus 2 infection: what do we know? Eur J Pharmacol. 2020;883:173373. https://doi.org/10.1016/j.ejphar.2020.173373.
Chen N, Zhou M, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–13.
Ferrara F, Porta R, D’Aiuto V, Vitiello A. Remdesivir and COVID-19. Ir J Med Sci. 2020;17:1–2. https://doi.org/10.1007/s11845-020-02401-5.
Vitiello A, Ferrara F. Therapeutic strategies for SARS-coV‑2 acting on ACE‑2. Eur J Pharm Sci. 2021;156:105579. https://doi.org/10.1016/j.ejps.2020.105579.
Vitiello A, La Porta R, Ferrara F. Sacubitril, valsartan and SARS-CoV‑2. BMJ Evid Based Med. 2020; https://doi.org/10.1136/bmjebm-2020-111497.
Vitiello A, Ferrara F. Remdesivir versus ritonavir/lopinavir in COVID-19 patients. Ir J Med Sci. 2020; https://doi.org/10.1007/s11845-020-02440-y.
Vitiello A, La Porta R, Ferrara F. Scientific hypothesis and rational pharmacological for the use of sacubitril/valsartan in cardiac damage caused by COVID-19. Med Hypotheses. 2021; https://doi.org/10.1016/j.mehy.2021.110486.
Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of Coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708.
Struyf T, Deeks JJ, Dinnes J, et al. Signs and symptoms to determine if a patient presenting in primary care or hospital outpatient settings has COVID-19 disease. Cochrane Database Syst Rev. 2020; https://doi.org/10.1002/14651858.CD013665.
Chung TW, Sridhar S, Zhang AJ, et al. Olfactory dysfunction in Coronavirus disease 2019 patients: observational cohort study and systematic review. Open Forum Infect Dis. 2020;7:ofaa199.
Tong JY, Wong A, Zhu D, et al. The prevalence of olfactory and gustatory dysfunction in COVID-19 patients: a systematic review and meta-analysis. Otolaryngol Head Neck Surg. 2020;163:3.
Wang D, Hu B, Hu C, et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020;323:1061.
Recalcati S. Cutaneous manifestations in COVID-19: a first perspective. J Eur Acad Dermatol Venereol. 2020;34:e212.
Arentz M, Yim E, Klaff L, et al. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington state. JAMA. 2020;323:1612.
Xie Y, Wang X, Yang P, Zhang S. COVID-19 complicated by acute pulmonary embolism. Radiol Cardiothorac Imaging. 2020;2(2):e200067. https://doi.org/10.1148/ryct.2020200067.
Fan Z, Chen L, Li J, Tian C, Zhang Y, Huang S, et al. Clinical features of COVID-19 related liver damage. medRxiv. 2020. https://doi.org/10.1101/2020.02.26.20026971.
Chai X, Hu L, Zhang Y, Han W, Lu Z, Ke A. Specific ACE2 expression in cholangiocytes may cause liver damage after 2019-nCoV infection. BioRxiv. 2020; https://doi.org/10.1101/2020.02.03.931766.
Vitiello A, Ferrara F, Pelliccia C, Granata G, La Porta R. Cytokine storm and colchicine potential role in fighting SARS-CoV‑2 pneumonia. Ital J Med. 2020;14(2):88–94. https://doi.org/10.4081/itjm.2020.1284.
Yang Z, Xu M, Yi JQ, Jia WD. Clinical characteristics and mechanism of liver damage in patients with severe acute respiratory syndrome. Hepatobiliary Pancreat Dis Int. 2005;4:60–3.
Ferrara F, Granata G, Pelliccia C, et al. The added value of pirfenidone to fight inflammation and fibrotic state induced by SARS-CoV‑2. Eur J Clin Pharmacol. 2020; https://doi.org/10.1007/s00228-020-02947-4.
American Lung Association. Lung Health & COVID-19.. https://www.lung.org/lung-health-diseases/lung-disease-lookup/covid-19/faq. Accessed 3 Apr 2020.
Vitiello A, Pelliccia C, Ferrara F. Drugs acting on the renin-angiotensin system and SARS-CoV‑2. Drug Discov Today. 2021;21:1359–6446. https://doi.org/10.1016/j.drudis.2021.01.010.
Gupta R, et al. Clinical considerations for patients with diabetes in times of COVID-19 epidemic. Diabetes Metab Syndr Clin Res Rev. 2020; https://doi.org/10.1016/j.dsx.2020.03.002.
Vitiello A, Ferrara F. Pharmacological agents to therapeutic treatment of cardiac injury caused by Covid-19. Proc Natl Sci Counc Repub China B. 2020; https://doi.org/10.1016/j.lfs.2020.118510.
LaRosa JC, He J, Vupputuri S. Effects of statins on risk of coronary artery disease: a meta-analysis of randomized controlled trials. JAMA. 1999;282:2340–6.
Law MR, Wald NJ, Rudnicka AR. Quantifying effect of statins on low density lipoprotein cholesterol, ischaemic heart disease, and stroke: systemic review and meta-analysis. BMJ. 2003;326:1423.
Takemoto M, Liao JK. Pleiotropic effects of 3‑hydroxy-3-methylglutaryl coenzyme A reductase inhibitors. Arterioscler Thromb Vasc Biol. 2001;21:1712–9.
Sacks FM, Pfeffer MA, Moye LA, Rouleau JL, Rutherford JD, Cole TG, et al. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. N Engl J Med. 1996;335:1001–9.
Group TL-TIwPi. Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. N Engl J Med. 1998;339:1349–57.
Noma K, Oyama N, Liao JK. Physiological role of ROCKs in the cardiovascular system. Am J Physiol, Cell Physiol. 2006;290(16469861):C661–C8.
Kataoka C, Egashira K, Inoue S, Takemoto M, Ni W, Koyanagi M, et al. Important role of Rho-kinase in the pathogenesis of cardiovascular inflammation and remodeling induced by long-term blockade of nitric oxide synthesis in rats. Hypertension. 2002;39:245–50.
Higashi M, Shimokawa H, Hattori T, Hiroki J, Mukai Y, Morikawa K, et al. Long-term inhibition of Rho-kinase suppresses angiotensin II-induced cardiovascular hypertrophy in rats in vivo: effect on endothelial NAD(P)H oxidase system. Circ Res. 2003;93:767–75.
Do EZ, Fukumoto Y, Sugimura K, et al. Rho-kinase activation in patients with heart failure. Circ J. 2013;77:2542–50.
Ohnaka K, Shimoda S, Nawata H, Shimokawa H, Kaibuchi K, Iwamoto Y, et al. Pitavastatin enhanced BMP‑2 and osteocalcin expression by inhibition of Rho-associated kinase in human osteoblasts. Biochem Biophys Res Commun. 2001;287:337–42.
Ma MM, Li SY, Wang M, Guan YY. Simvastatin attenuated cerebrovascular cell proliferation in the development of hypertension through Rho/Rho-kinase pathway. J Cardiovasc Pharmacol. 2012;59:576–82.
Satoh M, Ogita H, Takeshita K, Mukai Y, Kwiatkowski DJ, Liao JK. Requirement of Rac1 in the development of cardiac hypertrophy. Proc Natl Acad Sci U S A. 2006;103:7432–7.
Tanaka S, Fukumoto Y, Nochioka K, Minami T, Kudo S, Shiba N, et al. Statins exert the pleiotropic effects through small GTP-binding protein dissociation stimulator upregulation with a resultant Rac1 degradation. Arterioscler Thromb Vasc Biol. 2013;33:1591–600.
Jones SP, Teshima Y, Akao M, Marban E. Simvastatin attenuates oxidant-induced mitochondrial dysfunction in cardiac myocytes. Circ Res. 2003;93:697–9.
Node K, Fujita M, Kitakaze M, Hori M, Liao JK. Short-term statin therapy improves cardiac function and symptoms in patients with idiopathic dilated cardiomyopathy. Circulation. 2003;108:839–43.
Buber J, Goldenberg I, Moss AJ, Wang PJ, McNitt S, Hall WJ et al. Reduction in Life-Threatening Ventricular Tachyarrhythmias in Statin-Treated Patients With Nonischemic Cardiomyopathy Enrolled in the MADIT-CRT (Multicenter Automatic Defibrillator Implantation Trial with Cardiac Resynchronization Therapy). J Am Coll Cardiol. 2012;60:749–55.
Muhlhauser U, Zolk O, Rau T, Munzel F, Wieland T, Eschenhagen T. Atorvastatin desensitizes beta-adrenergic signaling in cardiac myocytes via reduced isoprenylation of G‑protein gamma-subunits. FASEB J. 2006;20:785–7.
Ridker PM, et al. Measurement of C‑reactive protein for the targeting of statin therapy in the primary prevention of acute coronary events. N Engl J Med. 2001;344:1959–65.
Taubes G. Does inflammation cut to the heart of the matter? Science. 2002;296:242–5.
Diomede L, et al. In vivo anti-inflammatory effect of statins is mediated by nonsterol mevalonate products. Arterioscler Thromb Vasc Biol. 2001;21:1327–32.
Stalker TJ, et al. A new HMG-CoA reductase inhibitor, rosuvastatin, exerts anti-inflammatory effects on the microvascular endothelium: the role of mevalonic acid. Br J Pharmacol. 2001;133:406–12.
Liu L, et al. Integrin-dependent leukocyte adhesion involves geranylgeranylated protein(s). J Biol Chem. 1999;274:33334–40.
Takeuchi S, et al. Cerivastatin suppresses lipopolysaccharide-induced ICAM‑1 expression through inhibition of the rho GTPase in BAEC. Biochem Biophys Res Commun. 2000;269:97–102.
Inoue I, et al. Lipophilic HMG-CoA reductase inhibitor has an anti-inflammatory effect: Reduction of mRNAlevels for interleukin-1β, interleukin‑6, cyclooxygenase‑2, and p22phlox by regulation of peroxisome proliferator-activated receptor α(PPARα) in primary endothelial cells. Life Sci. 2000;67:863–76.
Ikeda U, Shimada K. Statins and monocytes. Lancet. 1999;353:2070.
Grip O, et al. Atorvastatin activates PPAR-γand attenuates the inflammatory response in human monocytes. Inflamm Res. 2002;51:58–62.
Zelvyte I, et al. Modulation of inflammatory mediators and PPARγand NFκB expression by pravastatin in response to lipoproteins in human monocytes in vitro. Pharmacol Res. 2002;45:147–54.
Laufs U, et al. Upregulation of endothelial nitric oxide synthase by HMG CoA reductase inhibitors. Circulation. 1998;97:1129–35.
Ortego M, et al. Atorvastatin reduces NF-κB activation and chemokine expression in vascular smooth muscle cells and mononuclear cells. Atherosclerosis. 1999;147:253–61.
Vitiello A, La Porta R, D’Aiuto V, Ferrara F. Pharmacological approach for the reduction of inflammatory and prothrombotic hyperactive state in COVID-19 positive patients by acting on complement cascade. Hum Immunol. 2021; https://doi.org/10.1016/j.humimm.2021.01.007.
Vitiello V, Ferrara F. Colchicine and SARS-CoV-2: management of the hyperinflammatory state. Respir Med. 2021; https://doi.org/10.1016/j.rmed.2021.106322.
Campioni M, Severino A, Manente L, De Luca A, La Porta R, Vitiello A, et al. Identification of protein-protein interactions of human HtrA1. Front Biosci. 2011;3:1493–9. https://doi.org/10.2741/e350.
Ferrara F, Vitiello A. Efficacy of synthetic glucocorticoids in COVID-19 endothelites. Naunyn Schmiedebergs Arch Pharmacol. 2021; https://doi.org/10.1007/s00210-021-02049-7.
Verpaalen B, Neyts J, Delang L. Are statins a viable option for the treatment of infections with the hepatitis C virus? Antiviral Res. 2014;105:92–9. https://doi.org/10.1016/j.antiviral.2014.02.020.
Zhu Q, Han Q, Liu Z. Potenzial role for statins in the treatment of chronic HCV infection. Future Virol. 2013;8:727–9. https://doi.org/10.2217/fvl.13.70.
Ikeda M, Abe K, Yamada M, Dansako H, Naka K, Kato N. Different anti-HCV profiles of statins and their potential for combination therapy with interferon. Hepatology. 2006;44:117–25. https://doi.org/10.1002/hep.21232.
Trebicka J, Hennenberg M, Laleman W. et alAtorvastatin lowers portal pressure in cirrhotic rats byinhibition of RhoA/Rho-kinase and activation ofendothelial nitric oxide synthase. Hepatology. 2007;46:242–5.
Marrone G, Maeso-Diaz R, Garcia-Cardena G, et al. KLF2 exerts antifibrotic and vasoprotective effects in cirrhotic rat livers: behind the molecular mechanismsof statins. Gut. 2014; https://doi.org/10.1136/gutjnl-2014-308338.
Watts KL, Sampson EM, Schultz GS, et al. Simvastatin inhibits growth factor expression and modulates profibrogenic markers in lung fibroblasts. Am J Respir Cell Mol Biol. 2005;32:290–300.
Nadrous HF, Ryu JH, Douglas WW, et al. Impact of angiotensin-converting enzyme inhibitors and statins on survival in idiopathic pulmonary fibrosis. Chest. 2004;126:438–46.
Meisel SR, Xu XP, Edgington TS, et al. Dose-dependent modulation of tissue factor protein andprocoagulantactivity in humanmonocyte-derived macrophagesbyoxidizedlowdensitylipoprotein. J Atheroscler Thromb. 2011;18(7):596–603.
Owens AP 3rd, Mackman N. The antithrombotic effects of statins. Annu Rev Med. 2014;65:433–45. https://doi.org/10.1146/annurev-med-051812-145304.
Liao JK, Laufs U. Pleiotropic effects of statins. Annu Rev Pharmacol Toxicol. 2005;45:89–118. https://doi.org/10.1146/annurev.pharmtox.45.120403.095748.
Yildirim M, Kayalar O, Atahan E, Oztay F. Anti-fibrotic effect of atorvastatin on the lung fibroblasts and myofibroblasts. Eur Respir J. 2018;52(Suppl 62):PA991. https://doi.org/10.1183/13993003.congress.
Ferrara F, Vitiello A. Potenzial pharmacological approach in the regulation of ACE‑2 and DPP-IV in diabetic COVID-19 patient. Ital J Med. 2020; https://doi.org/10.4081/itjm.2020.1435.
Zhang XJ, Qin JJ, Cheng X, et al. In-hospital use of Statins is associated with a reduced risk of mortality among individuals with COVID-19. Cell Metab. 2020;32(2):176–187.e4. https://doi.org/10.1016/j.cmet.2020.06.015.
Rodriguez-Nava G, Trelles-Garcia DP, Yanez-Bello MA, Chung CW, Trelles-Garcia VP, Friedman HJ. Atorvastatin associated with decreased hazard for death in COVID-19 patients admitted to an ICU: a retrospective cohort study. Crit Care. 2020;24:429.
Siang Kow C, Syed Shahzad H. meta-analysis of effect of Statins in patients with COVID-19. Am J Cardiol. 2020; https://doi.org/10.1016/j.amjcard.2020.08.004.
Daniels LB, Sitapati AM, Zhang J, Zou J, Bui QM, Ren J, Longhurst CA, Criqui MH, Messer K. Relation of Statin Use Prior to Admission to Severity and Recovery Among COVID-19 Inpatients. Am J Cardiol. 2020;136:149–155. https://doi.org/10.1016/j.amjcard.2020.09.012.
Tan WYT, Young BE, Lye DC, et al. Statin use is associated with lower disease severity in COVID-19 infection. Sci Rep. 2020;10:17458. https://doi.org/10.1038/s41598-020-74492-0.
Vitiello A, La Porta R, Ferrara F. Correlation between the use of statins and COVID-19: what do we know? BMJ Evid Based Med. 2020; https://doi.org/10.1136/bmjebm-2020-111589.
Turner RM, Pirmohamed M. Statin-related myotoxicity: a comprehensive review of pharmacokinetic, pharmacogenomics and muscle components. J Clin Med. 2020; https://doi.org/10.3390/jcm9010022.
Liverpool COVID-19 drug interactions.. http://www.covid19-druginteractions.org/. Accessed 20 Mar 2020.
Ferrara F. Antirheumatic in SARS-CoV-2: benefit or risk? Ital J Med. 2020;14(2):114–5. https://doi.org/10.4081/itjm.2020.1290.
Ferrara F, Porta R, Santilli P, D’Aiuto V, Vitiello A. Are multiple sclerosis therapies safe in severe acute respiratory syndrome coronavirus 2 times? Indian J Pharmacol. 2020;52(5):441–2. https://doi.org/10.4103/ijp.IJP_417_20.
Lombardi N, Crescioli G, Bettiol A, Marconi E, Vitiello A, Bonaiuti R, et al. Characterization of serious adverse drug reactions as cause of emergency department visit in children: a 5-years active pharmacovigilance study. BMC Pharmacol Toxicol. 2018;19(1):16. https://doi.org/10.1186/s40360-018-0207-4.
Vitiello R, Ferrara F, La Porta R. Remdesivir and COVID-19 infection, therapeutic benefitsor unnecessary risks? Ir J Med Sci. 2020; https://doi.org/10.1007/s11845-020-02482-2.
Vitiello A, La Porta R, D’Aiuto V, Ferrara F. The risks of liver injury in COVID-19 patients and pharmacological management to reduce or prevent the damage induced. Egypt Liver J. 2021;11:11. https://doi.org/10.1186/s43066-021-00082-y.
Author contribution
Antonio Vitiello: conceptualization, writing original draft, methodology. Francesco Ferrara: writing, review and editing, supervision, validation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
F. Ferrara and A. Vitiello declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Copyright
The authors certify that the manuscript is original, never submitted to another journal for publication before. All authors contributed equally to the manuscript and had the opportunity to revise and approve the final text.
Rights and permissions
About this article
Cite this article
Ferrara, F., Vitiello, A. The advantages of drug treatment with statins in patients with SARS-CoV-2 infection. Wien Klin Wochenschr 133, 958–965 (2021). https://doi.org/10.1007/s00508-021-01845-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-021-01845-8