Summary
Background
Preoperative hyponatremia and thrombocytosis are associated with perioperative morbidity in patients with epithelial ovarian cancer (EOC). The aim of the present study was to evaluate preoperative hyponatremia and thrombocytosis as prognostic parameters in patients with EOC.
Methods
In a retrospective cohort study, serum levels of sodium and thrombocyte counts were evaluated in 498 patients with EOC. Data were extracted from the prospectively maintained database. Results were correlated with clinicopathological parameters and patient survival.
Results
Mean (standard deviation) overall pretherapeutic serum sodium levels and thrombocyte counts in patients with EOC were 138.8 (2.9) mmol/l and 340.1 (122.6) × 103/µl, respectively. Hyponatremia (serum sodium levels ≤ 134 mmol/l) was found in 33 (6.7%) patients and thrombocytosis (thrombocytes ≥ 450/µl) in 88 (17.7%) patients. Serum sodium levels were associated with the presence or absence of residual tumor tissue after primary surgery. Thrombocyte counts were associated with Fédération Internationale de Gynécologie et d’Obstétrique (FIGO) tumor stage, presence/absence of residual tumor, histological grade and histological type. Patients with thrombocytosis presented with advanced tumor stage, a higher rate of postoperative residual tumor mass, higher tumor grade, and a higher rate of serous ovarian cancer. In a multivariate logistic regression analysis, only the established clinicopathological parameters but not serum sodium and thrombocyte count were independent predictors of patient overall survival.
Conclusion
Preoperative hyponatremia and thrombocytosis are not useful as additional independent prognostic parameters in patients with EOC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recently, a published study reported preoperative hyponatremia, elevated serum creatinine levels, hypoalbuminemia, and thrombocytosis to be associated with perioperative morbidity in patients with epithelial ovarian cancer (EOC) [1]. While various studies have also shown a significant prognostic influence of serum albumin levels [2] and thrombocyte counts [3], no data are available in patients with EOC regarding hyponatremia. Hyponatremia is one of the most commonly seen water-electrolyte imbalances defined as a serum sodium level of less than 135 mmol/l and its severe form defined as a serum sodium level of less than 120 mmol/l [4, 5]. It can cause various clinical symptoms including nausea, confusion, seizures and even coma [4, 5]. A total of three different types of hyponatremia have been described according to a patient’s fluid status: low, normal, and high volume hyponatremia. Low volume hyponatremia can be caused by diarrhea, vomiting, or diuretics. Normal volume hyponatremia can be caused by adrenal insufficiency, hypothyroidism, the syndrome of inappropriate antidiuretic hormone secretion or high fluid intake. Lastly, high volume hyponatremia can be caused by heart, liver or kidney failure [4, 5].
Besides its predictive value regarding postoperative morbidity, hyponatremia has also been investigated as a prognostic parameter in various malignancies including colon, renal and lung cancer [6,7,8]. Of note, normalization of hyponatremia was found to improve patients’ prognosis [9].
No data are available regarding the prognostic value of hyponatremia. As serum sodium levels and thrombocyte counts are laboratory parameters evaluated in routine clinical care, these parameters could serve as cheap and readily available prognostic parameters. Therefore, it was the aim of the present study to investigate whether hyponatremia and thrombocytosis are associated with overall survival in patients with EOC undergoing cytoreductive surgery.
Material and methods
Patients
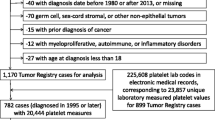
A total of 498 patients with EOC were included in the present retrospective cohort study. All patients were treated between 2000 and 2015 at the Department of General Gynecology and Gynecologic Oncology, Medical University of Vienna, Austria. The institutional review board of the Medical University of Vienna approved the present study (IRB approval number: 247/2009). Individual patient data were extracted from the departmental database. At the time of EOC diagnosis, a physical examination was performed and routine blood tests were carried out including serum levels of sodium and thrombocyte counts. Patients were treated according to local standards with cytoreductive surgery and adjuvant platinum-based chemotherapy with or without bevacizumab. Surgical staging was performed according to the International Federation of Gynecologists and Obstetricians (FIGO) guidelines, including hysterectomy, bilateral salpingo-oophorectomy, pelvic and/or para-aortic lymphadenectomy, appendectomy, omentectomy and additional cytoreductive procedures to resect all gross tumors. All patients with tumor stages FIGO IC-IV and all patients with clear cell carcinoma received an adjuvant platinum-based chemotherapy. All patients were followed upposttreatment four times annually, including pelvic examination, abdominal ultrasound examination, and serum evaluation of CA-125.
Laboratory tests
As part of the institutional clinical routine, blood samples were obtained by peripheral venous puncture 24–72 h prior to surgery. Quantitative determination of sodium in serum was performed with an ion-sensitive electrode (ISE) using the ISE module of the Roche Hitachi Cobas C System (ISE indirect Na-K-Cl for Gen. 2, Cobas, Roche Diagnostics, Mannheim, Germany) with normal values ranging from 135–145 mmol/l. Thrombocyte counts were determined by the Sysmex XE-5000 (Sysmex Austria, Vienna, Austria) test system with normal values ranging from 150–450 × 103/µl.
Statistics
Values are given as number (n) or means (standard deviation [SD]). Variables were compared using χ2-tests, Pearson’s correlation coefficient, t‑test and one-way ANOVA, where appropriate. Survival probabilities were calculated by the product limit method of Kaplan and Meier. Differences between groups were tested using the log-rank test. Univariate and multivariate Cox regression models for overall survival were performed including tumor stage (FIGO I vs. II vs. III vs. IV), presence of postoperative residual tumor mass (present vs. absent), histological grade (G1 vs. G2 vs. G3), histological type (serous vs. all others), patient age, serum sodium levels, and thrombocyte counts. The results were analyzed for the endpoint of overall survival. Only cancer-related death was regarded as an event, patients who died due to other reasons or who were still alive even with tumor present at the time of last follow-up were censored with the date of last follow-up. Survival times of patients who were disease free or still alive or dead as a result of other causes were censored with the last follow-up date. In the study two multivariate models were performed, one with all established clinical prognostic parameters and the experimental parameters as continuous variables (continuous model) and one with all established clinical prognostic parameters and the experimental parameters as dichotomous variables (dichotomous model). Estimated p-values of < 0.05 were considered statistically significant. Hazard ratios (HR) and 95% confidence intervals (CI) are provided.
Based on an assumed frequency of hyponatremia of 9% as reported by Martin et al. [1], it was hypothesized that women with a poor prognosis might differ from those with a good prognosis by a minimum increment of at least 9%. Thus, the sample size calculation was based on an assumed difference of 9% versus 18%. With 498 patients, this study has a power of > 85% to detect this difference with a p-value of 0.05 indicating statistical significance. With respect to the multivariate model, only nine potential confounders were included in order to avoid model overfitting. For statistical analysis, the Statistical Package for the Social Sciences statistical software (SPSS 22.0, SPSS, Chicago, IL, USA) was used.
Results
Patients’ characteristics are shown in Table 1. The mean (SD) overall pretherapeutic serum sodium levels and thrombocyte counts in patients with EOC were 138.8 (2.9) mmol/l, 0.84 (0.40) mg/dl and 340.1 (122.6) × 103/µl, respectively. Hyponatremia (serum sodium levels ≤ 134 mmol/l) and thrombocytosis (thrombocytes ≥ 450 × 103/µl) were found in 33 (6.7%) and 88 (17.7%) patients, respectively. The association between investigated serum parameters and clinicopathological parameters are shown in Table 2. Serum sodium levels were only associated with the presence/absence of residual tumor tissue after primary surgery. Thrombocyte counts were associated with FIGO tumor stage, presence/absence of residual tumor, histological grade, and histological type. Patients’ characteristics broken down by absence/presence of hyponatremia and thrombocytosis are shown in Table 3. Patients with thrombocytosis presented with advanced tumor stage, a higher rate of postoperative residual tumor mass, higher tumor grade, and a higher rate of serous ovarian cancer.
In the univariate survival analysis, experimental parameters, i. e., sodium levels and thrombocyte counts, were considered both as continuous variables and separately as dichotomous variables broken down by the abovementioned, well-established groups. Both parameters reached statistical significance both as continuous and as dichotomous variables (Fig. 1 and 2), as did all established clinical prognostic parameters (Table 4). In the multivariate analysis, both parameters were not associated with overall survival both as continuous variables and dichotomous variables.
Discussion
In the present study, low sodium levels and thrombocytosis were not associated with impaired overall survival in patients with EOC. A number of laboratory parameters have been shown to be associated with impaired prognosis in patients with EOC including markers of inflammation, serum tumor markers, serum levels angiotensin-converting enzyme or cell surface markers expressed by the tumor cells [11,12,13,14,15]. Interestingly enough, recently published studies investigated whether medical interventions such as antihypertensive medication or parenteral nutrition, by altering circulating inflammatory markers or serum albumin, influences the prognosis of cancer patients [10, 16]. Serum levels of sodium could also be changed by medical interventions; however, the results of the present study are contradictory to the aforementioned data, as no independent prognostic effect of serum levels of sodium was ascertained in the study.
The exact underlying pathophysiological processes of hyponatremia in cancer patients have not been fully elucidated to date. The largest body of evidence regarding causes of hyponatremia in cancer patients derives from small-cell lung cancer [8]. Hyponatremia is usually caused by the syndrome of inappropriate antidiuretic hormone, which may be driven by ectopic production of arginine vasopressin by tumors or by effects of anticancer and palliative medications on arginine vasopressin production or action [1]. Other factors may also cause hypovolemic hyponatremia, including diarrhea and vomiting, which are associated with peritoneal carcinomatosis [1]. The present data show that in EOC patients, low serum sodium levels or hyponatremia are not associated with patient survival, although hyponatremia was found to be associated with 30 day postoperative mortality [1]. It can be reasonably argued that the effect of preoperative hyponatremia is likely to be only of short duration and may be outweighed by numerous other clinical parameters, such as tumor stage and residual tumor mass after primary debulking surgery.
Due to the availability of new targeted therapies and the implications for family members, recommendations for genetic testing regarding BRCA1/2 have been recently issued [17]. Due to the retrospective design, this study included patients who were diagnosed with ovarian cancer between 2000 and 2015. Therefore, data regarding BRCA mutation were missing in most of the cases. Another interesting hypothesis which has to be kept in mind when interpreting the results of this study is the fact that hyponatremia might be associated with a decreased tolerance to chemotherapy. As no data are available regarding side effects of chemotherapy regimens, this assumption cannot be supported or refuted. Although a relatively high number of patients were included in the study, another point of criticism might be an insufficient power to detect differences based on the number of events. Based on the sample size analysis and on the number of parameter included in the multivariate analysis, an adequate power and sample size can be assumed. Of note, based on the study design only possible associations could be investigated but by no means any causality.
Conclusion
Despite the previously reported association between hyponatremia with perioperative morbidity [1] and thrombocytosis with perioperative morbidity as well as prognosis [1, 3], the study falls short of showing any association between preoperative serum levels of sodium and thrombocyte counts with overall survival among patients with primary EOC. Preoperative hyponatremia and thrombocytosis are not useful as additional independent prognostic parameters in patients with EOC.
References
Martin JY, Goff BA, Urban RR. Preoperative hyponatremia in women with ovarian cancer: an additional cause for concern? Gynecol Oncol. 2016;142(3):471–6.
Ataseven B, du Bois A, Reinthaller A, Traut A, Heitz F, Aust S, et al. Pre-operative serum albumin is associated with post-operative complication rate and overall survival in patients with epithelial ovarian cancer undergoing cytoreductive surgery. Gynecol Oncol. 2015;138(3):560–5.
Cozzi GD, Samuel JM, Fromal JT, Keene S, Crispens MA, Khabele D, et al. Thresholds and timing of pre-operative thrombocytosis and ovarian cancer survival: analysis of laboratory measures from electronic medical records. BMC Cancer. 2016;16:612.
Hoorn EJ, Zietse R. Diagnosis and treatment of Hyponatremia: compilation of the guidelines. J Am Soc Nephrol. 2017;28:1340–9.
Henry DA. In the clinic: Hyponatremia. Ann Intern Med. 2015;163:ITC1–ITC19.
Choi JS, Bae EH, Ma SK, Kweon SS, Kim SW. Prognostic impact of hyponatraemia in patients with colorectal cancer. Colorectal Dis. 2015;17:409–16.
Schutz FA, Xie W, Donskov F, McDermott DF, Rini BI, Agarwal N, et al. The impact of low serum sodium on treatment outcome of targeted therapy in metastatic renal cell carcinoma: results from the International Metastatic Renal Cell Cancer Database Consortium. Eur Urol. 2014;65(4):723–30.
Kobayashi N, Usui S, Yamaoka M, Suzuki H, Kikuchi S, Goto Y, et al. The influence of serum sodium concentration on prognosis in resected non-small cell lung cancer. Thorac Cardiovasc Surg. 2014;62(4):338–43.
Balachandran K, Okines A, Gunapala R, Morganstein D, Popat S. Resolution of severe hyponatraemia is associated with improved survival in patients with cancer. BMC Cancer. 2015;15:163.
Coulson R, Liew SH, Connelly AA, Yee NS, Deb S, Kumar B, et al. The angiotensin receptor blocker, Losartan, inhibits mammary tumor development and progression to invasive carcinoma. Oncotarget. 2017;8(12):18640–56.
Zwakman N, van de Laar R, Van Gorp T, Zusterzeel PL, Snijders MP, Ferreira I, et al. Perioperative changes in serum CA125 levels: a prognostic factor for disease-specific survival in patients with ovarian cancer. J Gynecol Oncol. 2017;28:e7.
Luo Y, Kim HS, Kim M, Lee M, Song YS. Elevated plasma fibrinogen levels and prognosis of epithelial ovarian cancer: a cohort study and meta-analysis. J Gynecol Oncol. 2017;28:e36.
Huo J, Hu J, Liu G, Cui Y, Ju Y. Elevated serum interleukin-37 level is a predictive biomarker of poor prognosis in epithelial ovarian cancer patients. Arch Gynecol Obstet. 2017;295(2):459–65.
Menczer J. Preoperative elevated platelet count and thrombocytosis in gynecologic malignancies. Arch Gynecol Obstet. 2017;295(1):9–15.
Beyazit F, Ayhan S, Celik HT, Gungor T. Assessment of serum angiotensin-converting enzyme in patients with epithelial ovarian cancer. Arch Gynecol Obstet. 2015;292(2):415–20.
Mendivil AA, Rettenmaier MA, Abaid LN, Brown JV 3rd, Mori KM, Goldstein BH. The impact of total parenteral nutrition on postoperative recovery in patients treated for advanced stage ovarian cancer. Arch Gynecol Obstet. 2017;295(2):439–44.
Vergote I, Banerjee S, Gerdes AM, van Asperen C, Marth C, Vaz F, et al. Current perspectives on recommendations for BRCA genetic testing in ovarian cancer patients. Eur J Cancer. 2016;69:127–34.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
K. Hefler-Frischmuth, C. Grimm, L. Gensthaler, E. Reiser, R. Schwameis, and L.A. Hefler declare that they have no competing interests.
Ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. IRB approval (IRB approval number: 247/2009) was obtained for the present study. Due to the retrospective design of our study informed consent from patients was not necessary.
Rights and permissions
About this article
Cite this article
Hefler-Frischmuth, K., Grimm, C., Gensthaler, L. et al. Prognostic value of preoperative hyponatremia and thrombocytosis in patients with epithelial ovarian cancer. Wien Klin Wochenschr 130, 575–580 (2018). https://doi.org/10.1007/s00508-018-1388-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-018-1388-y