Abstract
Purpose
Platelets have multiple functions and they also play an important role in malignancies. Elevated platelet count and thrombocytosis at the time of diagnosis in patients with many solid tumors correlates with prognosis and is associated with poor survival. The aim of the following report is to review the literature concerning elevated platelet count and thrombocytosis in gynecologic malignancies.
Method
A PubMed search of all English literature peer-reviewed publications was performed containing the terms elevated platelet count or thrombocytosis and vulvar cancer, cervical cancer, endometrial cancer, and ovarian cancer. All studies published until December 31, 2015, were included in the following review.
Results
A pretreatment elevated platelet count and thrombocytosis have been shown to be associated with a poor prognosis in many studies of gynecologic malignancies with the exception of vulvar carcinoma.
Conclusion
Since elevated platelet count and thrombocytosis may be prevented by blocking thrombopoietic cytokines, their assessment may, in the future, be of therapeutic significance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The role of platelets in solid tumors
Platelets have multiple functions. They respond to localized injury of vascular integrity preventing hemorrhage, they defend their host against microbial invasion and participate in inflammatory and immune responses. In addition, they also play an important role in malignancies.
Recently, two extensive reviews summarized tumor–platelet interactions [1, 2]. According to these reviews, elevated platelet count and thrombocytosis at the time of diagnosis in patients with many solid tumors correlates with prognosis and is associated with poor survival. Clinically, thrombocytosis may precede the diagnosis of malignancy by a long time period. The increase in platelet counts in these tumors is due to tumor-secreted cytokines that play a role in stimulating megakaryocyte growth and thrombopoiesis. The most frequent of these cytokines are interleukin (IL)-1, IL-3, IL-6, IL-11, leukemia inhibitory factor, granulocyte–macrophage colony-stimulating factor and many others. IL-6 in particular, acting as an autocrine growth factor, is overproduced in a variety of malignancies, including gastrointestinal, renal cell, prostate, lung cancer as well as epithelial ovarian cancer. However, it remains unclear whether the worse prognosis in patients with thrombocytosis is a result of IL-6-induced thrombocytosis or caused by IL-6 itself. Platelets also play a role in intravasation and extravasation of tumor cells in the process of metastasis.
Tumor cells generate thrombin, a potent platelet activator agonist. Activated platelets release multiple proteins that may stimulate angiogenesis including vascular endothelial growth factor, platelet-derived growth factor and others, thus promoting tumor growth and metastasis. Consequently, a vicious cycle is created in which tumors increase platelet counts that augment tumor growth and metastases that, in turn, further increase platelet counts. Furthermore, activated platelets adhere to tumor cells and secrete immunoregulatory molecules that prevent their contact with the host’s immune system. Thereby, they serve as a so called “protective cloak” for circulating tumor cells, protecting them from immune destruction by natural killer cells.
The effect of blocking the various steps of tumorigenesis facilitated by platelets has been investigated in tumor cells and in patients. Inhibition of IL-6 or antiplatelet agents such as heparinoids that interrupt the vicious cycle might prove beneficial for patients with solid tumors and thrombocytosis. It has been shown that platelet inhibition or depletion reduces metastasis rates. Investigations of combined therapy of antiplatelet agents with conventional chemotherapy therapy seem, therefore, to be indicated. The most important concern of using such agents is that it may interfere with normal platelet function, thereby causing bleeding complications.
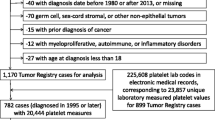
The purpose of the following report is to review the literature concerning elevated platelet count and thrombocytosis in gynecologic malignancies. A PubMed search of all English literature peer-reviewed publications was performed containing the terms elevated platelet count or thrombocytosis and vulvar cancer, cervical cancer, endometrial cancer, and ovarian cancer. All studies published until August 31, 2015, were included in the following review.
Platelet count in gynecological malignancies
Elevated preoperative platelet count (>300,000/mcL) and thrombocytosis (>400,000/mcL) have been assessed in many gynecological tumors and, although the results are occasionally inconsistent, they have usually been shown to be associated with a bad prognosis with the exception of vulvar carcinoma.
Vulvar carcinoma
Two studies found that pretreatment thrombocytosis was not a prognostic indicator. Lavie et al. [3] reviewed the pretreatment platelet counts of 201 women with vulvar cancer and correlated them to the patient’s age, stage of disease, node status, histologic type, and outcome. Thrombocytosis was present in 14.92 % of patients with vulvar malignancies and in 15.46 % of patients with squamous cell carcinoma of the vulva. No correlation was found between thrombocytosis and tumor size, incidence of lymph node metastases, or stage of the disease. The five-year survival rate for patients with thrombocytosis was not significantly different from that of patients with normal platelet counts (89.29 vs. 76.47 %, respectively). When adjusted for age, histological differentiation, number of tumors, stage, presence of nodal metastases, platelet count, hemoglobin, and white blood count, only the staging, number of tumors, and histological differentiation were associated with an unfavorable prognosis. Hefler et al. [4] also found that pretreatment thrombocytosis was not an independent predictor of outcome in patients with vulvar cancer. They assessed 62 patients with squamous cell vulvar cancer. They used a cutoff level of 300,000/mcL for tumor thrombocytosis. Thrombocytosis, according to their definition, was present in 27.4 % of vulvar cancer patients. In a univariate analysis, tumor stage and tumor thrombocytosis were significantly associated with a shortened progression-free survival (PFS) and overall survival (OS). However, a multivariate analysis taking into account stage, anemia, and thrombocytosis showed that pretreatment platelet count did not confer additional prognostic information to that already obtained by stage on PFS and OS.
Cervical cancer
Many studies have evaluated the prognostic significance of a preoperative platelet count in cervical cancer patients occasionally yielding conflicting results.
The preoperative platelet count in 219 women with stage IB cervical cancer treated by radical hysterectomy was assessed by Rodriguez et al. [5]. An elevated thrombocyte count was found in 85 (38.8 %) women. The cumulative five-year survival of women with a preoperative platelet count greater than 300,000/mcL was significantly higher in women with a count equal to or less than 300,000/mcL (65 vs. 84 %; P = 0.004). On multivariate analysis taking into account age, race, the presence of nodal metastases, and lesion size, high platelet count was still found to be an independent prognostic factor for poor survival in patients with early stage cervical cancer (P = 0.04).
Several studies by Hernandez et al. [6–8] also investigated the effect of platelet count on prognosis in patients with cervical cancer. In their first study (1992) of 113 patients treated with radiation therapy, they found that thrombocytosis is an independent indicator of poor prognosis. The five-year cumulative survival rate for the 93 patients with normal platelet counts was 65 % and only 25 % for the 20 patients (17.7 %) with thrombocytosis (P < 0.0001). In a later Gynecologic Oncology Group study [8], they assessed the significance of thrombocytosis in 623 surgically treated patients with stage IB cervical squamous cell carcinoma. Thrombocytosis was found in 59 (9.5 %) patients. In this study, in contrast to the study by Rodriguez et al. [5] of stage IB patients, the five-year survival for patients with thrombocytosis was statistically not different than that of patients with a normal platelet count (82 vs. 83.5 %, respectively; P = 0.4). Pelvic node metastasis was present in 13 (22 %) of 59 patients with thrombocytosis, and 77 (13.7 %) of 564 patients with a normal platelet count (P = 0.1). However, there was a significant correlation between tumor size and platelet count. Patients with thrombocytosis had a mean tumor size of 27.9 mm, while it was 20.4 mm in patients without thrombocytosis (P = 0.002). Other factors found to be associated with thrombocytosis in this population were elevated white blood cell (WBC) count (P = 0.009) and history of chronic obstructive pulmonary disease. (COPD). In a multivariate analysis for thrombocytosis adjusted for COPD, WBC count, and tumor size, tumor size continued to be statistically significant (P = 0.01). The authors concluded that thrombocytosis is a marker of tumor burden and not an independent prognostic factor for PFS or survival. In an additional Gynecologic Oncology Group study (2000) of 291 patients with stages IIB-IVA cervical carcinoma without periaortic node metastasis, thrombocytosis was present in 86 (29.6 %) of them. Thrombocytosis seemed again to be related to tumor burden. It was also found that in these stages, patients with thrombocytosis had a 55 % greater chance of dying than those who had a normal platelet count.
De Jong et al. [9] retrospectively evaluated the value of a platelet count as well as several tumor-related proteins as predictors of lymph node metastasis (LNM) and their prognostic significance in 93 stage IB cervical cancer patients treated by radical hysterectomy. Thrombocytosis was present in 6.7 % of patients and was significantly associated with PFS and OS in univariate analysis (P = 0.04 and P = 0.001, respectively) with a tendency to significance in multivariate analysis (P = 0.08 and P = 0.09, respectively). But thrombocytosis could not predict LNM. They, therefore, postulated that thrombocytosis could be a marker for subclinical tumor burden in early stage cervical cancer.
In contrast, thrombocytosis was not found to be an independent prognostic factor in patients with carcinoma of the cervix by Lopes et al. [10]. They reviewed the pretreatment platelet counts of 643 women with cervical cancer and correlated them to patient’s age, stage of disease, histologic type, node status (when available), and outcome. Squamous cell carcinoma was diagnosed in 491 patients (76.4 %), adenocarcinoma in 106 (16.5 %), mixed carcinoma in 22 (3.4 %) and undifferentiated carcinoma in 24 (3.7 %) patients. Thrombocytosis was present in 109 patients (1 7 %)—106 with adenocarcinoma and 491 with squamous cell carcinoma and was associated with a poorer outcome in both these histological types. In univariate analysis, the five-year survival rate for patients with thrombocytosis was significantly worse than that for those with normal platelet counts (57.1 vs. 76.5 %; P < 0.01). However, when adjusted for stage of disease, thrombocytosis failed to have a significant effect on patient survival. Similar to the study by De Jong et al. [9], there was also no relation between thrombocytosis and the incidence of positive lymph nodes. They concluded that thrombocytosis did not have a significant effect on patient survival when broken down by stage. In this study as well as in the study by Hernandes et al. [6], an increase in the rate of thrombocytosis with advancing stage was found. Recently, Zhao et al. [11] reported that higher platelet levels correlated significantly with advanced tumor stage, large tumor size, and tumor recurrence. They also found that thrombocytosis may be a biomarker for predicting recurrence in patients with early stage cervical cancer.
However, in this study as well, multivariate survival analyses showed that platelet levels were not an independent prognostic factor for poor survival in early stage cervical cancer patients.
Endometrial carcinoma
The frequency of preoperative thrombocytosis varies widely in endometrial carcinoma and ranges between 1.5 and 33.9 % [12–17]. In most studies, preoperative thrombocytosis was found to be an indicator of poor prognosis in this malignancy [13, 15–20]. This was found to be true in univariate as well as in multivariate analysis. Gucer et al. [13] found among 135 endometrial carcinoma cases that thrombocytosis was significantly more frequent in stage II-IV disease, in G2 and G3 tumors, in those with deep myometrial invasion and lymph-vascular space invasion. The five-year survival rate of the 19 (14.0 %) patients with thrombocytosis was significantly worse than that of the patients without thrombocytosis (61 vs. 96 %, P < 0.0001). The recurrence rate was significantly higher in patients with thrombocytosis than in those without thrombocytosis. In multivariate analysis, thrombocytosis continued to be a predictor of worse prognosis. Gorelic et al. [15] reported that patients with stage III-IV disease had a significantly higher mean preoperative platelet count compared to patients with stage I-II disease (359,000 vs. 283/mcL; P = 0.005). The median PFS and OS in patients without thrombocytosis was significantly better than in those with thrombocytosis. The median OS in patients without thrombocytosis (n = 21) was 24.0 ± 4.5 months and, in patients with thrombocytosis (n = 8), was 7.0 ± 3.8 months (P = 0.015). In this study as well, multivariate analysis showed that preoperative thrombocytosis retained independent prognostic significance. However, among patients with localized disease, preoperative thrombocytosis was not associated with worsened OS or PFS. Scholz et al. [19] also found in multivariate analysis of 59 stage III or IV endometrial carcinoma patients that five-year DFS as well as five-year OS were significantly influenced by preoperative thrombocytosis. The effect of thrombocytosis in 68 patients with endometrial serous carcinoma was assessed by Lerner et al. [18]. The eight patients with thrombocytosis had significantly more advanced-stage disease and ascites of more than 1 L. Those with normal preoperative platelet counts demonstrated a greater likelihood of optimal tumor resection to less than 1 cm residual disease. Patients with thrombocytosis had a shorter PFS and OS. On multivariate analysis, after controlling for age and stage, thrombocytosis retained significance as an indicator of poor prognosis.
Other studies assessed the association of thrombocytosis only in univariate analysis. Tamussino et al. [17] found among 212 endometrial carcinoma patients that low pretreatment hemoglobin is a poor prognostic factor in univariate analysis and that it is associated with thrombocytosis. Metindir et al. [20] also evaluated the relationship between preoperative hemoglobin and platelet count and prognostic factors in 61 endometrial cancer patients. In univariate analysis, the presence of cervical involvement and lymphatic metastasis were associated with significantly higher median preoperative platelet counts.
Some studies found that thrombocytosis was a prognostic predictor in univariate analysis but not in multivariate analysis. Heng et al. [16] reported that among 238 endometrial carcinoma patients, those who had advanced stage, adnexal involvement, lymph node metastasis, and positive peritoneal cytology had significantly higher mean preoperative platelet counts when compared with those who had not. They found that patients with thrombocytosis had significant higher rates of advanced stage, cervical involvement, adnexal involvement, positive peritoneal cytology, and lymph node involvement than patients with a normal pretreatment platelet count. The five-year PFS and OS were significantly lower in patients who had thrombocytosis. Thrombocytosis was shown to be a prognostic factor in the univariate but not in multivariate analysis.
Not only thrombocytosis but elevated platelet counts may also be associated with some poor prognostic factors. Menczer et al. [12] reported that among 81 consecutive endometrial carcinoma patients, grades 2 and 3 were found to be significantly more common in those with a platelet count higher than 300,000/mcL. Patients with an elevated count also had a poorer survival rate and higher prevalence of older age, high stage and deep myometrial invasion, but this trend did not reach statistical significance. Ayhan et al. [14] assessed the platelet count in 155 endometrial carcinoma patients. They considered a 325,000/mcL platelet count as a threshold value. Stage III and IV, tumor grade 3, the presence of cervical and adnexal involvements were associated with significantly higher median preoperative platelet counts. Multivariate analysis revealed cervical involvement and presence of high-grade histology to be significantly associated with higher platelet counts. Furthermore, they found that higher preoperative platelet counts, even within the normal range (150,000–400,000/mcL), may reflect poor prognostic factors such as cervical involvement and high grade.
We located only one study comprising 190 endometrial carcinoma patients that found that a preoperative platelet count was not correlated with two factors known to be of prognostic significance namely stage and grade of the tumor. In this study by Kologlu et al. [21], thrombocytosis was defined as a platelet count of >300,000/mcL.
Epithelial ovarian carcinoma
Several studies found that an elevated platelet count and thrombocytosis was a frequent preoperative finding in patients with epithelial ovarian carcinoma ranging from 22.4 to 62.5 % [22–25]. Thrombocytosis was found to be a marker of advanced disease and poor prognosis in this malignancy as well [23–27].
Menczer et al. [23] assessed preoperative thrombocytosis in 82 ovarian cancer patients. No statistically significant correlation was found between thrombocytosis with age, grade and residual disease. A statistically non-significant excess of thrombocytosis was found among patients with advanced disease. However, the survival of patients with thrombocytosis was significantly lower in those with than those without thrombocytosis (P = 0.04). Li et al. [24] reported that among 183 ovarian carcinoma patients, those with preoperative thrombocytosis were found to have statistically significant greater elevations of CA-125, more advanced-stage disease, higher grade tumors, more frequent lymph node metastases and greater volume of ascites. Patients with thrombocytosis demonstrated a greater likelihood of suboptimal tumor resection (residual disease >1). Also, patients with thrombocytosis had a shorter PFS and OS (28 vs. 79 months, P < 0.0001). Thrombocytosis retained significance as a poor prognostic indicator in patients with stage III and IVA disease (P = 0.04) on multivariate analysis. Platelet count was also found to be a predictor of PFS and OS by Gerestein et al. [26] in univariate as well as multivariate analysis. Among 118 patients, the median preoperative serum blood platelet counts were higher in those with progressive disease and of those who died of disease when compared with patients without recurrence and those alive at last follow-up date, 332 ± 124 and 33 ± 127 vs. 251 ± 122 and 267 ± 115·109/L with P = 0.005 and <0.0001, respectively. Studies by Gastl et al. [22, 28] found that serum IL-6 levels and thrombocytosis in ovarian cancer patients were significantly higher than in patients with benign ovarian tumors; that highest platelet counts occurred in patients with undifferentiated ovarian carcinoma or advanced disease; and that IL-6 levels in ascites correlate significantly with the volume of ascites, with ovarian tumor size, with thrombocytosis and with prognosis. Furthermore, Bakkum-Gamez et al. [29] found that preoperative thrombocytosis is independently associated with increased postoperative ileus at primary cytoreductive surgery of epithelial ovarian cancer, fallopian tube cancer, and primary peritoneal cancer. Also, Cohen et al. [30] reported that an elevated platelet count (≥350,000/mcL) is associated with suboptimal resection and shortened overall survival at time of secondary cytoreductive surgery for recurrent disease.
In contrast, one study of epithelial ovarian carcinoma [31] that comprised 130 patients, a relatively large proportion of whom were in stage I (37 %), found that thrombocytosis had no effect on survival although it was associated with advanced-stage disease, higher serum levels of CA125, greater volumes of ascites, and greater incidence of suboptimal cytoreduction.
Also, there are some inconsistencies regarding the association of thrombocytosis and stage of ovarian cancer. Zeimet et al. [31] and Gastl et al. [22, 28] found a significantly higher percentage of patients with thrombocytosis among those with advanced disease, while Chalas et al. [32] reported that patients with thrombocytosis are evenly distributed among stages.
Several studies that assessed the effect of preventing thrombocytosis in ovarian cancer are of great significance. Guo et al. [33] measured, by immunohistochemistry, IL-6 expression in ovarian cancer patient specimens, and evaluated the effects of siltuximab, a monoclonal anti-IL-6 antibody, in ovarian cancer cell lines. They found that siltuximab effectively block the IL-6 signaling pathways, that IL-6-induced gene expression and that siltuximab increased the cytotoxic effects of paclitaxel in a paclitaxel-resistant ovarian cancer cell line in vitro. However, the drug did not have a significant effect on paclitaxel-resistant tumor growth in a xenograft mouse model in vivo. Egan et al. [34] investigated platelet interactions with ovarian cancer cells in ovarian cancer cell lines. Platelets adhered to ovarian cancer cells and these cells induced platelet activation. They found that ovarian cancer-induced platelet activation is mediated by adenosine 5′-diphosphate released from tumor cells and can be blocked by adenosine 5′-diphosphate receptor (P2Y12 and P2Y1) antagonists. Coward et al. [35] found by automated immunohistochemistry of tissue microarrays from 221 ovarian cancer cases, that intensity of IL-6 staining in malignant cells was significantly associated with poor prognosis. Treatment of ovarian IL-6-producing cancer cells with siltuximab reduced cytokine and chemokine production and also inhibited IL-6 signaling, angiogenesis and tumor growth. In a very limited clinical trial of siltuximab, they observed that one of 18 evaluable patients had a partial response, while seven others had periods of disease stabilization. Another noteworthy study was performed by Stone et al. [25]. They investigated the underlying mechanisms of thrombocytosis in 619 human ovarian carcinoma samples and mouse models of epithelial ovarian cancer to assess the effects of platelets on tumor growth and angiogenesis. Their findings indicated that increased production of thrombopoietic cytokines in tumor and host tissue leads to thrombocytosis in ovarian carcinoma and that the use of an antiplatelet antibody in tumor-bearing mice significantly reduced tumor growth and angiogenesis. They, therefore, suggested that targeting these cytokines may have therapeutic potential.
A recent population-based Danish study [36] of primary gynecological cancer diagnosed between July 1, 2003 and January 23, 2010, identified through the Danish Cancer Registry 581 women with a primary diagnosis of gynecological cancer. Of these, 139 (23.9 %) women had cervical cancer, 218 (37.5 %) had endometrial cancer, and 224 (38.6 %) had ovarian cancer. The authors concluded that pre-diagnostic thrombocytosis was associated with advanced stage of gynecological cancer at diagnosis and increased all-cause and cancer-specific mortality.
Conclusions
In cervical cancer pretreatment, thrombocytosis has been shown, in most studies, to be an indicator of poor prognosis in univariate analysis and to be associated with high tumor burden in multivariate analysis. In endometrial carcinoma, an elevated platelet count and thrombocytosis are associated with known prognostic factors such as high grade, deep myometrial invasion, lymph-vascular space involvement, advanced stage and poor outcome. Thrombocytosis is a marker of advanced disease and poor survival in ovarian cancer as well. This was found to be true in univariate analysis as well as in multivariate analysis in most studies of these two malignancies. Only in vulvar cancer, thrombocytosis seems not to be a prognostic indicator.
Studies in cell lines and mouse models of ovarian carcinoma found that platelet activation and thrombocytosis could possibly be prevented by blocking thrombopoietic cytokines. These cytokines may constitute new potential targets for therapeutic intervention.
Although similar studies have not been reported in other gynecologic malignancies, assessment of elevated platelet count and thrombocytosis in patients with any type of gynecologic malignancy, may, in the future, be of therapeutic significance.
References
Buergy D, Wenz F, Groden C, Brockmann MA (2009) Tumor-platelet interaction in solid tumors. Int J Cancer 130:2747–2760
Lin RJ, Afshar-Kharghan V, Schafer AI (2014) Paraneoplastic thrombocytosis: the secrets of tumor self-promotion. Blood 124:184–187
Lavie O, Comerci G, Daras V, Bolger BS, Lopes A, Monaghan JM (1999) Thrombocytosis in women with vulvar carcinoma. Gynecol Oncol 72:82–86
Hefler L, Mayerhofer K, Leibman B, Obermair A, Reinthaller A, Kainz C et al (2000) Tumor anemia and thrombocytosis in patients with vulvar cancer. Tumour Biol 21:309–314
Rodriguez GC, Clarke-Pearson DL, Soper JT, Berchuck A, Synan I, Dodge RK (1994) The negative prognostic implications of thrombocytosis in women with stage IB cervical cancer. Obstet Gynecol 83:445–448
Hernandez E, Lavine M, Dunton CJ, Gracely E, Parker J (1992) Poor prognosis associated with thrombocytosis in patients with cervical cancer. Cancer 69:2975–2977
Hernandez E, Heller PB, Whitney C, Diana K, Delgado G (1994) Thrombocytosis in surgically treated stage IB squamous cell cervical carcinoma (a gynecologic oncology group study). Gynecol Oncol 55:328–332
Hernandez E, Donohue KA, Anderson LL, Heller PB, Stehman FB (2000) The significance of thrombocytosis in patients with locally advanced cervical carcinoma: a gynecologic oncology group study. Gynecol Oncol 78:137–142
De Jonge ET, Viljoen E, Lindeque BG, Amant F, Nesland JM, Holm R (1999) The prognostic significance of p53, mdm2, c-erbB-2, cathepsin D, and thrombocytosis in stage IB cervical cancer treated by primary radical hysterectomy. Int J Gynecol Cancer 9:198–205
Lopes A, Daras V, Cross PA, Robertson G, Beynon G, Monaghan JM (1994) Thrombocytosis as a prognostic factor in women with cervical cancer. Cancer 74:90–92
Zhao K, Deng H, Qin Y, Liao W, Liang W (2015) Prognostic significance of pretreatment plasma fibrinogen and platelet levels in patients with early-stage cervical cancer. Gynecol Obstet Invest 79:25–33
Menczer J, Geva D, Schejter E, Zakut H (1996) Elevated platelet count in patients with endometrial carcinoma: correlation with selected prognostic factors and with survival. Int J Gynecol Cancer 6:463–466
Gücer F, Moser F, Tamussino K, Reich O, Haas J, Arikan G et al (1998) Thrombocytosis as a prognostic factor in endometrial carcinoma. Gynecol Oncol 70:210–214
Ayhan A, Bozdag G, Taskiran C, Gultekin M, Yuce K, Kucukali T (2006) The value of preoperative platelet count in the prediction of cervical involvement and poor prognostic variables in patients with endometrial carcinoma. Gynecol Oncol 103:902–905
Gorelick C, Andikyan V, Mack M, Lee YC, Abulafia O (2009) Prognostic significance of preoperative thrombocytosis in patients with endometrial carcinoma in an inner-city population. Int J Gynecol Cancer 19:1384–1389
Heng S, Benjapibal M (2014) Preoperative thrombocytosis and poor prognostic factors in endometrial cancer. Asian Pac J Cancer Prev 15:10231–10236
Tamussino KF, Gucer F, Reich O, Moser F, Petru E, Scholz HS (2001) Pretreatment hemoglobin, platelet count and prognosis in endometrial carcinoma. Int J Gynecol Cancer 1(11):236–240
Lerner DL, Walsh CS, Cass I, Karlan BY, Li AJ (2007) The prognostic significance of thrombocytosis in uterine papillary serous carcinomas. Gynecol Oncol 104:91–94
Scholz HS, Petru E, Gucer F, Haas J, Tamussino K et al (2000) Preoperative thrombocytosis is an independent prognostic factor in stage III and IV endometrial cancer. Anticancer Res 20:3983–3985
Metindir J, Dilek GB (2009) Preoperatiove hemoglobin and platelet count and poor prognostic factors in patients with endometrial carcinoma. J Cancer Res Clin Oncol 135:125–129
Kaloglu S, Guraslan H, Tekirdag AI, Dagdeviren H, Kaya C (2014) Relation of preoperative thrombocytosis between tumor stage and grade in patients with endometrial carcinoma. Eurasian J Med 46:164–168
Gastl G, Plante M, Finstad CL, Wong GY, Federici MG, Bander NH et al (1993) High IL-6 levels in ascitic fluid correlate with reactive thrombocytosis in patients with epithelial ovarian cancer. Br J Haematol 83:433–441
Menczer J, Schejter E, Geva D, Ginath S, Zakut H (1998) Ovarian carcinoma associated thrombocytosis. Correlation with prognostic factors and with survival. Eur J Gynaecol Oncol 19:82–84
Li AJ, Madden AC, Cass I, Leuchter RS, Lagasse LD, Karlan BY (2004) The prognostic significance of thrombocytosis in epithelial ovarian carcinoma. Gynecol Oncol 92:211–214
Stone RL, Nick AM, McNeish IA, Balkwill F, Han HD, Bottsford-Miller J et al (2012) Paraneoplastic thrombocytosis in ovarian cancer. N Engl J Med 366:610–618
Gerestein CG, Eijkemans MJ, de Jong D, van der Burg ME, Dykgraaf RH, Kooi GS et al (2009) The prediction of progression-free and overall survival in women with an advanced stage of epithelial ovarian carcinoma. BJOG 116:372–380
Kuyumcuoglu U, Guzel AI, Celik Y, Erdemoğlu M (2010) The association of preoperative thrombocytosis with prognostic factors in malignant ovarian tumor. Eur J Gynecol Oncol 31:514–516
Gastl G, Plante M (2001) Bioactive interleukin-6 levels in serum and ascites as a. Methods Mol Med 39:121–123
Bakkum-Gamez JN, Langstraat CL, Martin JR, Lemens MA, Weaver AL, Allensworth S et al (2012) Incidence of and risk factors for postoperative ileus in women undergoing primary staging and debulking for epithelial ovarian carcinoma. Gynecol Oncol 125:614–620
Cohen JG, Tran AQ, Rimel BJ, Cass I, Walsh CS, Karlan BY et al (2014) Thrombocytosis at secondary cytoreduction for recurrent ovarian cancer predicts suboptimal resection and poor survival. Gynecol Oncol 132:556–559
Zeimet AG, Marth C, Müller-Holzner E, Daxenbichler G, Dapunt O (1994) Significance of thrombocytosis in patients with epithelial ovarian cancer. Am J Obstet Gynecol 170:549–554
Chalas E, Welshinger M, Engellener W, Chumas J, Barbieri R, Mann WJ (1992) The clinical significance of thrombocytosis in women presenting with a pelvic mass. Am J Obstet Gynecol 166:974–977
Guo Y, Nemeth J, O’Brien C, Susa M, Liu X, Zhang Z et al (2010) Effects of siltuximab on the IL-6-induced signaling pathway in ovarian cancer. Clin Cancer Res 6:5759–5769
Egan K, Crowley D, Smyth P, O’Toole S, Spillane C, Martin C et al (2011) Platelet adhesion and degranulation induce pro-survival and pro-angiogenic signalling in ovarian cancer cells. PLoS ONE 6:e26125
Coward J, Kulbe H, Chakravarty P, Leader D, Vassileva V, Leinste DA et al (2011) Interleukin-6 as a therapeutic target in human ovarian cancer. Clin Cancer Res 17:6083–6096
Andersen CL, Eskelund CW, Siersma VD, Felding P, Lind B, Palmblad J et al (2015) Is thrombocytosis a valid indicator of advanced stage and high mortality of gynecological cancer? Gynecol Oncol 139:312–318
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
I (the only author) declare that I received no grants and that I have no conflicts of interests.
My paper needs no ethical approval since it is a review of previously published articles.
Rights and permissions
About this article
Cite this article
Menczer, J. Preoperative elevated platelet count and thrombocytosis in gynecologic malignancies. Arch Gynecol Obstet 295, 9–15 (2017). https://doi.org/10.1007/s00404-016-4212-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-016-4212-9