Summary
Background
Austria faces increasing numbers of childhood overweight and obesity. Despite increasing numbers of studies, associations between parental body mass index (BMI) and education and the school type on overweight/obesity in students have not been reported. The objective of this study was to evaluate the influence of these parameters on the genesis of overweight/obesity in a large cohort representative of youth in Upper Austrian.
Methods
A cross-sectional analysis of data from 2930 children and adolescents aged 10, 14 or 17 years from 11 different state school types was conducted. Students and their parents completed a questionnaire and heights and weights were measured.
Results
Of the students 16.9% fulfilled the criteria for overweight and 5.6% for obesity, with the highest rates in the 10-year-olds (19.6% and 5.8%, respectively). While no gender differences were present in the youngest age group, the body mass index (BMI) during adolescence remained higher in boys but decreased significantly in girls. Male gender remained a risk factor through all calculations. Boys were overrepresented in schools with lower education levels and more often had BMIs ≥ 85th and ≥95th percentile. Higher parental education levels and lower parental BMIs were associated with lower BMIs of their offspring. Migration was an additional association factor for BMIs ≥ 85th percentile.
Conclusion
Low parental education levels, higher parental BMIs and migration background were associated with overweight and obesity in 10-year-olds. In adolescence, male gender and higher parental BMIs remained risk factors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
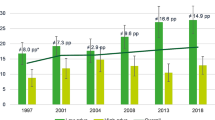
Childhood overweight and obesity have increased dramatically over decades [1]. According to the 2012 Austrian Nutrition Report (Österreichischer Ernährungsbericht) and the 2014 World Health Organization (WHO) Health Behavior in School Children (HBSC) study, this is also reflected by rising numbers of overweight or obese Austrian schoolchildren [2, 3]; however, recent studies have reported evidence of a plateauing and even a decline in the prevalence of obesity but still on a high level [4,5,6,7].
Socioeconomic factors (e.g. education, income), age, gender, heredity and life style factors were studied with conflicting results: a recent cross-sectional survey in seven European countries identified risk factors for overweight as younger age, male gender, watching television (TV) longer and living in the eastern part of Europe [8]. Gender variations of obesity may result from differences in biology and/or cultural habits and with respect to gender, studies have shown results with higher obesity rates among males in some countries and females in others [9, 10]. Contrasting studies reported increasing BMIs with older age in girls but not in boys [11], higher obesity prevalence in males from age 2 through 19 years compared to girls [12] and a decrease of overweight in girls while rates remained stable in boys [5]. Furthermore, higher rates of obesity among low income groups in wealthier countries and conversely in high income groups in poorer countries were published [13]. High maternal education was associated with lower BMIs in males, while overweight/obesity was less frequent in both sexes with higher parental education [14]. Low maternal socioeconomic status (SES) was associated with overweight among boys during childhood, and low paternal SES was associated with higher BMIs in both male and female adolescents. Younger children are more influenced by the socioeconomic position and life style of their families while peer influence plays an increasingly important role in adolescence [15].
The BMIs of children attending state schools were higher than those attending private schools [16]. Students in economically disadvantaged schools were between 1.7–2.4 times more likely to fulfil the criteria for obesity with no distinction between genders [17] and higher parental education correlated significantly with their children’s lower weight, regardless of the school type they attend [18]. Children and adolescents with migration background have an increased prevalence for overweight/obesity [19,20,21]. This risk was higher when both parents were immigrants and less educated [20]. Migration background also correlated significantly with extreme obesity in an earlier Austrian study [21]. Approximately 40–70% of inter-individual variability in BMIs has been attributed to genetic factors [22]. Environments in families with high parental BMIs have an additional negative effect on children and to a lesser extent on adolescents [23, 24]. In girls, body weight was influenced by having one parent with BMI ≥ 85th or ≥95th percentile, while boys’ body weight appeared to be influenced by the father’s BMI [25]. There are countless variables influencing the regulation of body weight and only a selected number can be included in questionnaires and studies. The aim of this study was to examine whether age, gender, environment, school type, parental education level, parental BMIs and migration background can be associated with overweight/obesity.
Participants, materials and methods
Study design
This cross-sectional, single center study was conducted between December 2012 and February 2013 in Upper Austria, an Austrian federal state with 1.5 million inhabitants. A stratified (e.g. school type, region) sample of students was drawn from all schools in Upper Austria: 10-year-olds/grade 4, 14-year-olds/grade 8 and 17-year-olds/grade 11 were recruited from 10 different state school types. Because of similar education levels, the school types were reduced from 10 to 8 for calculations (Table 1). Three questionnaires were adopted for the different age groups (one for the 10-year-olds with 61 questions, one for the 14- and 17-year-olds with 83 questions and one for the parents with 103 questions). The students and their parents were informed that participation was voluntary. Parents provided written informed consent. The study was approved by the local ethics committee and by the Austrian Data Protection Agency.
Measurements
The child’s weight was measured while wearing light clothing, using an electronic weight device with a reading accuracy of 0.1 kg from students of the University of Applied Sciences Steyr (UASS). Height was measured while wearing socks using a manual height board. The BMI was calculated in kg/m2 and BMI percentiles were calculated using gender-specific growth charts [25]. A BMI below the 85th percentile defined normal weight (including underweight), the 85th–95th percentile overweight and ≥95th percentile obesity. Parental body weight and height were self-reported and BMI was categorized as overweight (≥25 kg/m2) and obese (≥30 kg/m2).
Questionnaires
The focus of this study was on the education level of the students, migration status, parent education/BMI and living area. Migration criteria were defined as at least one parent born outside Austria. Students from the UASS assisted the 10-year-old children when answering the questionnaires. The older students could ask questions if needed and completed the questionnaire online. A total of 2930 questionnaires (100%) were obtained from the students, 2209 (75.4%) from the parents (with no information who answered the questions: mother, father, both). Of these 1924 (87.1%) could be matched to the corresponding child so that 65.7% of all student data could be completed with parental data. Parental response rates differed for the age groups (the older the children the less the response rate, 77.7%, 69.9% and 50.9%, respectively for the 10- 14 and 17-year-olds) and for the school types (smallest response rate from vocational schools 36.08%, largest response rate from colleges of education 77.92%), no difference was found for migration yes/no (Table 3).
Schools type and comparable education level
List of school types (schools with similar education level are combined):
-
4th grade: primary school (PS).
-
8th grade, lower education level: secondary school (SS) and secondary modern school (SMS).
-
8th grade, higher education level: junior high school (JHS).
-
11th grade, lower education level: vocational school (VS) and commercial high school (3 years) without final exam (CHSwE).
-
11th grade, higher education level: senior high school (SHS), commercial high school (CHS), technical high school (THS) and college of education (CoE) (kindergarten academy).
To compare parental BMIs and educational influences, indices were created and used for calculations. The parental Education Index (EI) is the sum of points for the highest education level achieved by each parent, i.e. primary school or secondary school 0 points, vocational school, commercial high school (3 years) without final examination 1 point and senior high school, commercial high school, technical high school, and college of education or university degree 2 points. The EI varies from 0 to 4. The parental BMI Index (BMI-I) is the sum of BMI points from each parent: normal weight 0 points, overweight 1 point, obesity 2 points. The BMI-I varies from 0 to 4.
Statistical analysis
Statistical analysis was performed using SAS 9.4 (SAS Institute, Cary, NC). In the univariate description of the data mean and standard deviation were used for continuous data, categorical data were summarized using counts and percentages. The examination of association between two nominal variables was done by χ2-tests, for ordinal variables the Mantel-Haenszel test was used. A p-value of 0.05 was used to determine statistical significance (two-tailed).
To evaluate risk factors for the outcome “overweight or obesity” (yes/no), multivariate logistic step-wise regression models were fitted for each age group. Mother’s BMI, father’s BMI, gender, region, migration status, living area and parental EI were used as influencing variables. As using these models only for explanation, a p-value of 0.1 was assumed to be significant.
Results
The prevalence of overweight/obesity for all students was 22.5%: 16.9% for overweight and 5.6% for obesity, with the highest rates in 10-year-old boys and girls. There was a male predominance of higher BMIs throughout all age groups. While there was no weight change in boys over time, overweight/obesity decreased significantly in 14-year-old and 17-year-old girls (p = 0.002) (Table 3). No BMI differences were found between urban and rural communities (77.2% and 77.6% normal weight, respectively).
In primary schools the distribution between boys and girls was as to be expected (50.9% boys and 49.1% girls). With higher secondary education, the percentage of boys was remarkable lower (Table 2). The prevalence of higher weight paralleled the lower education levels in 14 and 17-year-olds; however, gender-specific evaluations showed that school type had no influence on the BMIs of adolescent girls. Only boys with lower education levels were more often measured with BMI ≥ 85th or ≥95th percentile (Table 2).
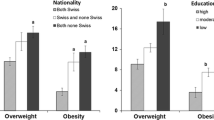
There was an inverse correlation between the parental EI and the prevalence of overweight/obesity (31.1% with EI 0 + 1 and 15.5% with EI 3 + 4, p < 0.001). This influence was significant in 10-year-old boys and girls (p < 0.001). The EI 3 + 4 remained as a positive predictor for lower weight in 14-year-old boys and 14 and 17-year-old girls (p < 0.001) (Table 3).
Parents with the lowest EI and the highest BMI-I were in 76.1% of cases overweight or obese themselves in contrast to 25.2% with the highest EI and the lowest BMI-I. Parents with the lowest EI and the highest BMI-I had 52.6% of their children in the normal weight range, while this rate was 90.4% with the highest EI and the lowest BMI-I. In EI 0 + 1 families, 6.4% of the children attend a school with a higher education level in contrast to 50.9% of EI 3 + 4 families (a ratio of 7.9). In primary schools the ratio EI 3 + 4 to EI 0 + 1 parents was 1.7, supporting the fact that parental education level is a strong predictor for school selection. In students with migration background overweight/obesity was measured in 27.0% of cases in comparison to 20.8% in Austrian students (p = 0.003). This percentage increased to 28.2% when both parents had migration background. Again, boys had higher BMIs than girls. In adolescents there was no association between migration and BMIs (Table 3).
In a stepwise multi-regression analysis for 10-year-olds, a low parental EI negatively correlated with higher student’s BMI, followed by migration, gender and father’s BMI. For 14 and 17-year-old adolescents, male gender predominated, followed by parental BMI (supplementary Table S1).
Discussion
A high percentage (22.5%) of all participating students fulfilled diagnostic criteria for overweight or obesity. The highest prevalence was found in primary school boys and girls (16.9 and 5.6% respectively). Recent data from Austria showed discrepant results (see supplementary Table S2) [2, 3, 26]. Most notably, the 2014 HBSC Study data [27] reported lower overweight and obesity rates. In comparison with the 2010 HBSC study there was no change in weight class over time in girls, while in boys overweight increased from 12.3% to 16.5% and obesity from 2.4% to 3.6%. In the HBSC study weight and height were self-reported. The 2012 Austrian Nutrition Report (Ernährungsbericht) published prevalence rates of obesity and overweight in 387 Austrian students (7–14 years old) [3]. Rates for obesity were higher (9%, 5.5% in boys and girls, respectively) and the ratio of overweight boys to girls was smaller compared to our results (17.1–16.2% compared to 19.8% and 14.2% in our study). In addition to a small sample size, the reported data in the 2012 report are older and might underestimate important gender aspects. Furthermore, different results for age and gender influences were published [5, 7,8,9,10,11,12]. In our study, there was no gender difference in the 10-year-olds. With increasing age BMIs remained high in adolescent boys and decreased in girls. Male gender remained a significant risk factor for the two older age groups throughout all calculations. This suggests that gender specific interventions are needed and these preventive interventions should focus particularly on older male teenagers. The BMIs were higher in primary school children living in rural areas relative to urban areas. After adjusting for parental education level, these differences were greatly attenuated [28]. There were no weight differences found between urban and rural regions, and regional weight distributions based on age and gender were nearly the same.
Other reports published associations between higher parental education and lower BMIs [12, 13]. In our study, a low parental EI was associated with significantly higher BMIs in 10-year-old boys and girls (odds ratio OR 3.6, p < 0.001) and an EI of 3 + 4 remained a positive predictor for lower weight in 14-year-old boys and 14 and 17-year-old girls (p < 0.001).
In addition to genetics, the environment of children and (to a lesser extent) adolescents are important factors for weight regulation [23,24,25]. The parents in our study with the lowest BMI-I and the highest EI reported overweight or obesity in 25.2% of cases compared to 76.1% with the highest BMI-I and lowest EI. Due to missing data, we can only speculate on this association. In families with the lowest EI and the highest BMI-I, 56.6% of children were within the normal weight range, while in families with the highest EI and the lowest BMI-I this number increased to 89.0%.
In our study, the distribution between boys and girls in primary schools was as expected. Schools of higher education levels had up to 25% less boys compared to girls and we found higher percentages of boys in lower education level schools. Interestingly, gender-specific evaluations showed that the school type itself had no influence on BMIs of adolescent girls; however, adolescent boys in schools with a lower education level had higher BMIs than in schools with a higher education level.
What happens with our boys? There was no weight reduction over time in boys. They tend to fall behind in school and drop out more often than girls. The trend is pronounced in higher secondary schools. In European countries, this gap between boys and girls is up to 8% [28]. Does our school system prefer the girls’ learning skills? Is the boys’ underachievement associated with their generally negative attitudes towards schoolwork [29]? Are these negative behaviors also relevant for developing overweight or obesity? In our study, parental EI was a strong predictor for school selection. In families with an EI 0–1 only 6.4% of the children attend a school with a higher education level, compared to 50.9% in EI 3–4 families. We evaluated the influence of the same educational background on boys and girls. Interestingly, a high parental education had less influence on boys. They attended schools with lower education levels more often and were more often measured with higher BMIs. That is why boys from families with lesser education (and higher parental BMI) in compulsory school types with a lower education level, will benefit from interventions the most. It can be assumed that encouraging boys to enrol in higher forms of secondary education, will have a substantial impact on body weight. Results also underline the problematics of less educated and overweight and obese families and regarding childhood weight problems the perspective should remain to address families as a whole system.
From 1961 to 2015, the percentage of foreign nationalities living in Austria increased from 1.4% to 13.3% of our total population (Statistik Austria). In several reports, non-German and non-Austrian children were more often overweight with even higher rates when both parents were immigrants [20]. Our students with a migration background had a significantly higher risk for overweight or obesity (27.0% with 1 and 28.2% with both parents) compared to Austrians (20.8%) and again, boys predominate. The difference was more pronounced for 10-year-old boys and girls. For 14 and 17-year-old boys and girls with a migration background the BMIs were comparable to Austrian students. With a migration background the educational level achieved by girls was higher than that of boys, but lower than that of girls without this background [29, 30]. In our study group, the ratio of low EI and high BMI-I in migration families compared to Austrians was 5.25. In these families 59.0% of their offspring had normal weight and with a high EI and a low BMI-I this value was 83.0%.
As overweight/obesity is highest in the youngest age group, interventional strategies have to be started early. Further prevention strategies must focus on families with lower parental education levels and higher parental BMIs and on gender differences during adolescence. The lower education level of boys might be associated with a higher BMI in adolescence. Further studies on this topic are needed. Due to the large sample size and the analysis of different correlations, even among young people from different types of schools and a different parental status in a more or less representative part of Austria, this study adds unique information on childhood obesity in Austria.
Limitations
A cross-sectional design does not facilitate direct conclusions regarding cause and effect. With questionnaires, overreporting or underreporting cannot be excluded, leading to bias and misclassification. The data are some years old and the situation may have changed. In addition, approximately one third of parental data were missing, reducing the strength of these calculations. On the other hand, the study reports the most recent data for Austria and missing parental questionnaires does not alleviate or alter the study’s main findings. Furthermore, the study was only conducted in one out of nine Austrian federal states. In Austria, existing publications reported higher BMIs in the east and lower ones in the west. Upper Austria is located in the middle of Austria representing a more homogeneous population thus increasing data representativeness. Another limitation is that the study does not include reports on life style variables influencing health behavior but since the overall goal of the study was to answer questions on demographics, gender and education differences regarding overweight and obesity, we chose not to include further variables in this publication. Overall, the strengths of this study are the relatively large sample size, the representativeness and the reliable anthropometric data for the subjects.
References
Wang Y, Lobstein T. Worldwide trends in childhood overweight and obesity. Int J Pediatr Obes. 2006;1(1):11–25.
Felder-Puig R, Ramelow D, Hofmann F, Teutsch F, Maier G. Gesundheit und Gesundheitsverhalten von österreichischen Schülerinnen und Schülern: Ergebnisse des WHO-HBSC-Survey 2014. http://www.bmgf.gv.at/cms/home/attachments/9/7/0/CH1444/CMS1427118828092/gesundheit_und_gesundheitsverhalten_oester_schuelerinnen_who-hbsc-survey_2014.pdf. Accessed 1 Dec 2016, Wien: Bundesministerium für Gesundheit.
Elmadfa I. (editor) Österreichischer Ernährungsbericht. Wien: Bundesministerium für Gesundheit; 2012. http://www.bmgf.gv.at/cms/home/attachments/4/5/3/CH1048/CMS1348749794860/oeb12.pdf. Zugegriffen: 3 Mar 2017.
Aeberli I, Ammann RS, Knabenhans M, Molinari L, Zimmermann MB. A decrease in the prevalence of paediatric adiposity in Switzerland from 2002 to 2007. Public Health Nutr. 2009;13(6):806–11.
Sjoberg A, Lissner L, Albertsson-Wikland K, Marild S. Recent anthropometric trends among Swedish school children: evidence for decreasing prevalence of overweight in girls. Acta Paediatr. 2008;97(1):118–23.
Olds T, Maher C, Zumin S, et al. Evidence that the prevalence of childhood overweight is plateauing: data from nine countries. Int J Pediatr Obes. 2011;6(5–6):342–60.
Skinner A, Skelton JA. Prevalence and trends in obesity and severe obesity among children in the United States, 1999–2012. JAMA Pediatr. 2014;168(6):561–6.
Olaya B, Moneta MV, Pez O, et al. Country-level and individual correlates of overweight and obesity among primary school children: a cross-sectional study in seven European countries. BMC Public Health. 2015;15:475–86.
Sweeting HN. Gendered dimensions of obesity in childhood and adolescence. Nutr J. 2008;7:1. doi:10.1186/1475-2891-7-1.
Lobstein T, Frelut M. Prevalence of overweight among children in Europe. Obes Rev. 2003;4(4):195–200.
Lundeen EA, Norris SA, Adair LS, Richter LM, Stein AD. Sex differences in obesity incidence: 20-year prospective cohort in South Africa. Pediatr Obes. 2016;11(1):75–80.
Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA. 2012;307(5):483–90.
Lobstein T, Baur LA, Uauy R. Obesity in children and young people: a crisis in public health. Obes Rev. 2004;5(Suppl 1):4–85.
Matthiessen J, Stockmarr A, Biltoft-Jensen A, Fagt S, Zhang H, Groth MV. Trends in overweight and obesity in Danish children and adolescents: 2000–2008 – exploring changes according to parental education. Scand J Public Health. 2014;42(4):385–92.
Van Vliet JS, Gustafsson PA, Duchen K, Nelson N. Social inequality and age-specific gender differences in overweight and perception of overweight among Swedish children and adolescents: a cross-sectional study. BMC Public Health. 2015;15:628.
Li J, Hooker NH. Children obesity and schools: evidence from the national survey of children’s health. J Sch Health. 2010;80(2):96–103.
Springer AE, Ranjit N, Delk J, Mehta K, Kelder SH. School-level economic disadvantage and obesity in middle school children in central Texas, USA; a cross.sectional study. Int J Behav Nutr Phys Act. 2015;12(Suppl 1):1–8.
O’Malley PM, Johnston LD, Delva J, Bachman JG, Schulenberg JE. Variation in obesity among American secondary school students by school and school characteristics. Am J Prev Med. 2007;33(4 Suppl):187–94.
Murer SB, Saarsalu S, Zimmermann J, Herter-Aeberli I. Risk factors for overweight and obesity in Swiss primary school children: results from a representative national survey. Eur J Nutr. 2016;55(2):621–9.
Beharat Pour M, Bergström A, Bottai M, et al. Effect of parental migration background on childhood nutrition, physical activity, and body mass index. J Obes. 2014; doi:10.1155/2014/406529.
Segna D, Widhalm H, Pandey MP, Zehetmayer S, Dietrich S, Widhalm K. Impact of mother tongue and gender on overweight, obesity and extreme obesity in 24,989 Viennese children/adolescents (2–16 years). Wien Klin Wochenschr. 2012;124(21–22):782–8.
Visscher PM, Brown MA, McCarthy MI, Yang J. Five years of GWAS discovery. Am J Hum Genet. 2012;90(1):7–24.
Wardle J. Understanding the aetiology of childhood obesity: implications for treatment. Proc Nutr Soc. 2005;64(1):73–9.
Trost SG, Kerr LM, Ward DS. Physical activity and determinants of physical activity in obesity. Int J Obes Relat Metab Disord. 2001;25(6):822–9.
Xu L, Dubois L, Burnier D, Girard M, Prud’homme D. Parental overweight/obesity, social factors, and child overweight/obesity at 7 years of age. Pediatr Int. 2011;53(6):826–31.
Mayer M, Gleiss A, Häusler G, et al. Weight and body mass index (BMI): current data for Austrian boys and girls aged 4 to under 19 years. Ann Hum Biol. 2015;42(1):45–55.
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320(7244):1240–3.
Sjoeberg A, Moraeus L, Yngve A, Poortvliet E, Al-Ansari U, Lissner L. Overweight and obesity in a representative sample of schoolchildren – exploring the urban-rural gradient in Sweden. Obes Rev. 2011;12(5):305–14.
Paseka A, Wroblewski A. Eurydice study: gender differences in educational outcomes: a study on the measures taken and the current situation in Europe: report on Austria 2000. http://eacea.ec.europa.eu/education/. Accessed 1 Dec 2016.
Wroblewski A, Herzog-Punzenberger B. OECD thematic review on migrant education. Country background report AUSTRIA 2009. http://www.oecd.org/dataoecd/8/26/42485003.pdf. Accessed 1 Dec 2016.
Acknowledgements
We thank the students from the University of Applied Sciences for collecting the data and the schools and families for their participation. We thank Mrs. Megan Bittermann for language editing of the manuscript. The study was supported by a grant from the Upper Austrian Government.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
D. Furthner, M. Ehrenmüller, A. Biebl, R. Lanzersdorfer, G. Halmerbauer, L. Auer-Hackenberg, and K. Schmitt declare that they have no competing interests.
Caption Electronic Supplementary Material
508_2017_1247_MOESM1_ESM.docx
S1: Results of the regression models: Odds ratios and confidence intervals for all age groups. S2: Overweight and obesity in Austria
Rights and permissions
About this article
Cite this article
Furthner, D., Ehrenmüller, M., Biebl, A. et al. Gender differences and the role of parental education, school types and migration on the body mass index of 2930 Austrian school children. Wien Klin Wochenschr 129, 786–792 (2017). https://doi.org/10.1007/s00508-017-1247-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-017-1247-2