Abstract
An important aspect of positron emission tomography (PET) imaging in a clinical application is the localization and detection of tumors and lesions by administering a predetermined amount of radiotracer. This allows detailed 3D imaging of a wide range of molecular processes in the human body. The quality of the PET image is dependent on the amount of radiotracer administrated and the patient’s body parameters. As the amount of injected radiotracer increases, an overall improvement in the quality of the reconstructed PET images and lesion detectability is expected, but it is accepted that any radiotracer doses are associated with the risk of radiation and it could be harmful to the patient if essential PET imaging is not performed because of the fear of radiation risk. To ensure the highest-quality diagnosis and the smallest radiation risk, the patient should receive the smallest amount of radiotracer that provides an image of sufficient quality. Our study proposed a PET simulation tool to predict the smallest amount of radiotracer that allows for a reliable diagnosis based on patients’ significant body parameters (weight, age) within a fixed total scan time to improve diagnostic processes for detecting and localizing tumors. We built a model of a particular PET scanner and patient, based on real MRI images and a digital anthropomorphic phantom of the brain. We performed Monte Carlo simulations of PET data acquisitions. A dataset of 60 patients was used, and 11 independent dose prediction simulations were performed for each patient. We concluded that our simulator estimated injected radiotracer doses 28% smaller than the standard clinical doses that yielded PET images of clinically acceptable quality. We also found that the total injected radiotracer dose for adult patients was affected by considering the patient’s weight rather than age.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Medical imaging is becoming an increasingly important component of clinical applications and research oncology for diagnosis, treatment planning, and tumor monitoring. Over the years, multiple imaging technologies have been developed, using the rapid advances in computer and imaging approaches, such as X-ray radiography, computed tomography (CT), ultrasound (US), magnetic resonance imaging (MRI), and nuclear medicine imaging: PET and single-photon emission computed tomography (SPECT) (Cherry 2009; Mawlawi 2009).
Nuclear medicine imaging is an independent field within medical imaging, designed to observe the biological functions of the body. It is widely applied in cardiology, oncology, and neuroscience. This method integrates two main components in order to work effectively: radiotracer synthesis and administration to the patient followed by in vivo data acquisition using an appropriate scanner detector system.
The radiotracer is a material composed of a pharmaceutical substance and a radioactive isotope compound which labels the substance. The radio-labeled pharmaceutical substance is then administered to the human body in trace amounts and is associated with a specific molecular in vivo process, such as metabolism, inflammation, proliferation, and calcification. It is usually introduced to the body by injection, swallowing, or even by inhalation, while the scanner is represented by a camera able to detect the presence of the radiotracer and thus generate images.
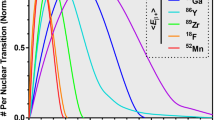
PET is one of the main applications of nuclear medicine imaging that estimates the spatial distribution of the injected radiotracer based on annihilation of the photons emitted by positron emitting isotopes, e.g., C-11, N-13, O-15, and F-18. The information provided by PET differs from other medical imaging modalities such as X-ray, CT, or MRI. These modalities provide anatomical information about the structural changes, while PET provides information about biological activities.
Because the biological changes often precede structural changes, PET may determine the presence of abnormalities much earlier than the other approaches (de SEOB Silva 2010; Gillam and Rafecas 2016; Turco 2012).
In PET imaging, a small amount of radiotracer can be injected into the patient in order to examine a specific molecular process targeted by the pharmaceutical component of the radiotracer. The field of nuclear medicine recognizes that any dose of radiotracer used in this procedure is associated with some possible risks of radiation. Radiation doses for PET imaging should be minimized, so the patient receives the smallest amount of radiotracer that provides images of sufficient quality. Suppose that essential PET imaging sessions—PET imaging sessions that provide the clinician with important data about the patient’s treatment and diagnosis—are not carried out because of the fear of radiation risk: What would happen? Radiation could harm the patient.
The aim in clinic is to maximize diagnostic image quality with the minimum exposure to radiation, and for that purpose the injected dosage should be optimized.
Because the advantages of PET examination outweigh the potential risks, the goal of this paper is to propose a tool to simulate the PET examination, based on significant body parameters (weight, age) at the set scanning time. This tool predicts the optimal radiotracer dose for individual patients, to reduce the cost of PET imaging and avoid potential radiation exposure risks.
To achieve our goal, we will describe in the following sections the details of the PET imaging simulation, the PET scanner model, and the patient model as well as explain the PET image quality measurement. Finally, we will predict the smallest possible amount of administered radiotracer that provides the appropriate diagnostic information to improve the clinical diagnostic process in terms of tumor detection and localization.
1.1 PET and Monte Carlo simulation
PET imaging deals with radiotracer decay, positron emission, photon transportation, and particle detection, and the use of simulation is extremely popular in PET research and clinical practice. The Monte Carlo simulation technique plays an essential role in this field and covers a wide range of problems that could not be solved using experimental or analytical methods. Monte Carlo simulations are widely used for PET imaging simulations because they consider all the random processes affecting PET imaging. PET simulation tools using Monte Carlo are useful for quantifying the radiotracer amount and planning the radiotracer dose, as well as studying the factors that affect the quality of PET reconstructed images. Furthermore, the Monte Carlo simulation can create data remarkably close to those obtained from real measurement. The simulation tools currently available are not easy to understand and use by beginners or short-term users without a background in programming and physics. These software applications are also extremely time-consuming, require considerable space on a hard disk, and are, generally, consumers of high computational resources. For example, to simulate a scan of the whole body, more than 17,000 h of CPU time is required (Zaidi 1999; Zaidi and Koral 2006).
Augusto et al. presented their work (Augusto et al. 2018) which results in the estimation of irradiation with RI that led to better accuracy of signals’ peak position with factor of two. They explained that their work was through projectile fragmentation. The authors claim that this was due to the signal acquisition with PET scanner. In their work (Kang et al. 2015), the authors managed to evaluate the accuracy of their algorithm on the dataset that has images of 11 patients. The image was evaluated using the low dose of PET that was calculated using their algorithm. The images were clear and gave a great result. The authors suggest that low dosage could be used for high-quality PET image of the brain. The images that are presented in their paper where they compared the low-dose PET with the standard dose show great results. A very promising result was presented (Junshen et al. 2017), showing that using deep learning results in enhanced images with low dose compared to the standard dose. The authors claimed that they managed to reconstruct the image with as low as 0.5% of the low dose that supposed to be used. Although low dose usually results in very low image quality that does not help for a better diagnosis, the experiment utilizes the high-quality deep learning and gave an excellent result. The study has a promising result for future utilization of image quality with low dose.
1.2 Injection dose prediction
This section provides an overview of previous studies relevant to the current study. Recently, Boldys et al. in their paper (Boldyš et al. 2013) employed a Monte Carlo simulation to calculate the amount of injection radiotracer needed to achieve a statistically constant quality of PET images, even with patients with differing body parameters (weight). The experiment was done on a simple patient model; they used a cylindrical geometric shape to approximate the body’s trunk–this method is not representative (Dvořák et al. 2013).
Also, in their paper (Karakatsanis et al. 2014) Karakatsanis et al. employed a Monte Carlo simulation to model a direct relation between administered activity and statistical quality measurement noise equivalent count rate (NECR) for a wide range of scanner parameters. They used a digital voxelized phantom and resized it to large-, small-, and medium-sized phantoms. The resulting total amounts of injected radiotracer represented by this work are smaller than the minimum amount that would be administrated to the real patient (Karakatsanis et al. 2014).
1.3 The proposed PET simulation methodology
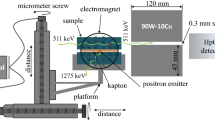
This section describes the significant steps performed to build the proposed PET simulation tool and how the PET-related physical effects were included. Figure 1 presents the computerized PET imaging system which is composed of phantom specifications (patient model) and scanner specifications, processed by simulation software in order to reconstruct the desired PET images. Phantoms are seen as a collection of digital volume arrays or 2D images that are used to approximate the locations and dimensions of the patient’s body structures and organs. The scanner model has been designed to reflect the specifications common to PET scanners currently used in clinics. The process of PET imaging is then simulated based on techniques such as the Monte Carlo method by following the basic algorithm provided in Yu (2010) and PET processes like radiotracer activity uptake, acquisition time, positron range, positron annihilation, photon transportation, and photon detection. The information that comes from the simulation is organized in a matrix called a sinogram. A sinogram is a simple ordered way to store the events registered by each detector into sets of parallel projections. Finally, using a reconstruction method, the PET image of the injected radiotracer activity distribution within the targeted part of the patient’s body is produced.
1.4 Patient model
Generating a realistic model of the patient’s anatomical and biological functions from imaging data is an important aspect of simulation (Ljungberg 2004; Zaidi and Koral 2006; Peter et al. 2000). Theoretically, the computerized model of a patient represents a set of tissues, organs, or body regions, visualizing the distributions of the radiotracer emission, scattering, and absorption points in a patient as similar to those in a real patient. By using a computerized model of a patient, we were able to test different or completely innovative cases by simply altering that model to reflect different situations. As shown in Fig. 2, two digital volumes were used for the Monte Carlo simulation performed: a matrix generated from reading real clinical data (clinical CT or MRI image for the patient) and a matrix of a digital anthropomorphic phantom (mathematical model designed to accurately represent the tissue and organ system in the whole body). Clinical data provide accurate experimental results, while the digital phantom provides the simulation data to make an evaluation of detecting abnormal lesions and tumors.
1.5 Radiotracer injection dose calculation
The radiotracer used in PET imaging can affect the quality of the resulting images. All radiotracers used in PET have to satisfy some requirements: They have to be nontoxic or not harmful for the patient, and they have to be chemically incorporated into the biological process being examined without modifying it. In addition, they should be specific for the physiological process under study. The most common radiotracer used in PET examination is fluorodeoxyglucose (FDG). As FDG is analogous to glucose and tumors can absorb significantly more glucose than the surrounding healthy tissue, FDG has been used to detect end-stage cancer (de SEOB Silva 2010; Turco 2012).
The amount of radiotracer that should be injected into a patient’s body injection administration (IA) is an important issue in PET examination. There are standards for the doses of radiotracer administered, and the European Association of Nuclear Medicine (EANM) has published clinical guidelines with recommendations for the administered amounts of specific radiotracers for specific applications (1) (Boellaard et al. 2010). Equation (1) shows the formula to calculate the IA, and it can be found from the patient weight in Kg and the min. scanning time.
By following the principle of as low as reasonable achievable (ALARA) (Waterstram-Rich and Christian 2013), each patient should receive the minimum amount of IA that is necessary to produce a good diagnostic image. For this purpose, and along with the variation in patient body parameters, we proposed a method to scale the IA dose according to a patient’s age, based on the EANM guideline recommendation and Young’s formula for nuclear medicine dosage calculations (Piepsz et al. 1990; Treves et al. 2011; Accorsi et al. 2010). Equation (2) shows the modified IA’ based on the patient age and its original IA:
1.6 Scanner model
When defining the model of a tomographic scanner, specific guidelines with respect to the hierarchy of the scanner components must be followed in order to track the particle’s physical interactions. Most PET scanners are built from single or multiple rings, each ring having several blocks divided into crystal detectors. The number of crystal detectors in blocks for single ring (No. Detectors) is calculated according to Eq. (3), using the ring radius and the total surface area, and it is computed is as follows:
According to (Saha 2010), the ring radius setting is usually between 300 and 600 mm and the surface area setting of each crystal detector is usually between 2 and 5 mm.
After setting up the scanner model, we defined the PET physical processes that occur during the simulation. The four processes we implemented are summarized in Fig. 3, and a detailed description of each process can be found in (Alsanea 2016).
1.7 Image quality measurement tools
There are many image quality assessment tools available in the field of PET imaging. For the purpose of our work, we employed the well-established statistical tools signal-to-noise ratio (SNR) and noise equivalent count (NEC). From a medical point of view, for a given diagnostic task, such as tumor or lesion detection, the significant measure for PET image quality is observing and detecting small foci (Boldyš et al. 2013; Dvořák et al. 2013). Thus, we provide a particularly attractive performance measurement of the reconstructed image precision and recall.
Signal-to-noise ratio (SNR) is a statistical measurement representing the relation between an acquired signal and the background image noise. We get its value by calculating the ratio between the mean of total detected photons \({\text{DP}}\mu \) and the standard deviation of the signal \({\text{DP}}\sigma\).
NEC is a statistical measurement describing the number of detected photons needed to produce an equivalent image with an ideal PET detection system that accounts only for true coincidences, and discards the random and scatter coincidences which contribute only to data noise.
The ability to detect the presence of possible tumors and lesions is a measure of PET image quality. In certain situations, the diagnostic task of classifying significant changes in the pixel values of the reconstructed image of a given region can be regarded as a problem for tumor detection and location. There are several measures of performance metrics for classifying tumor detectability, such as precision and recall. In order to calculate precision and recall, the classifier confusion matrix is computed, as shown in Fig. 4.
Precision measures the percentage of pixels detected as tumors that are truly tumors. Recall measures the percentage of tumor pixels that are truly detected from all pixels in the reconstructed image. The following equations represent the precision and recall, computed based on the confusion matrix:
1.8 PET simulation experiments
In this section, different simulations are performed on a set of patients chosen from clinical data. We used 60 patients’ MRI images and metadata that were available from the Digital Imaging and Communications in Medicine (DICOM) library. The main purpose of these simulations is to evaluate the simulated PET system discussed in previous sections and then predict the optimal injected radiotracer dose used to detect abnormal lesions and tumors.
To perform our simulations, the patient model was built from a digital phantom and a corresponding clinical MRI image. By following the algorithm illustrated in Fig. 5, each patient model was injected with 11 independent and different 18F-FDG doses calculated using Eq. (2). The scanner model was also built according to the technical specifications of a real clinical scanner used in a PET imaging system. After that, the PET imaging simulation was performed for all patient models. Furthermore, according to the scope of the experiment, the patient models were divided into four different groups based on their age and weight. Finally, the resulting images and statistical values for those groups were used in system evaluation comparisons, image quality assessments, and performance measurements.
In this simulation, we chose the brain as our main region of interest because it is an important region in clinical PET imaging. The brain has been associated with tumor lesions as well as a wide range of other diseases, such as Parkinson’s and Alzheimer’s diseases. In addition, the brain can have frequent lesion and tumor occurrence beside other abnormality diseases including Parkinson’s disease and Alzheimer’s disease.
2 PET simulation results and discussion
We simulated a set of 60 patients provided by the DICOM dataset, with weights ranging from 40 to 150 kg, and adult age distribution from 20 to 95 years. From the given weight range and for a constant age, we can divide the patients dataset into four groups: slim patients (the group of patients with very low weight; weight ≤ 45 kg), medium-weight patients (the group of patients with moderate weight; 45 < weight < 70 kg), overweight patients (the group of patients with a heavy weight; 70 < weight < 90 kg) , and obese patients (the group of patients with weight > 90 kg). The PET image simulations are classified as follows:
-
1.
Computing the NEC for default patient parameters weight = 63 kg and age 35 years (Fig. 6).
-
2.
Calculating the optimal radiotracer injection amount for patient parameters weight = 63 kg and age 35 years (Table 1, Fig. 7).
-
3.
Calculating the optimal radiotracer injection amount for patients with different weights in kg and constant age in years (Table 2, Fig. 8).
-
4.
Calculating the optimal radiotracer injection amount for patients with fixed weights in kg and different ages in years (Table 3, Fig. 9).
In Fig. 6, the quality of the reconstructed PET image increases with the injected radiotracer dose but only for doses smaller than a certain value. After the peak of NEC values is reached, then as the injected amount of radiotracer increases the acquired NEC data and the corresponding PET image quality remain constant. For the same patient, Fig. 7 illustrates the effect of the total injected dosage on the optimal radiotracer dose, the latter having been calculated from a lesion or tumor precision or recall score. The optimal radiotracer amount according to our simulation is 355 MBq, that is a reduction of 5% compared to the clinical injection dosage of 370 MBq. There is also a discrepancy of 5% from the calculated initial dosage value of 338 MBq.
Figure 8 illustrates the optimal radiotracer dosage in terms of lesion and tumor detection based on precision and recall values for a set of randomly selected patients from the available dataset of 60 patients.
Theoretically calculated doses for the classified patients are as follows:
-
For the group of slim patients, the minimal injected radiotracer amount by the simulator is 4% greater than the recommended dose.
-
For the group of medium-weight patients, the simulator doses are less than the clinical recommendations by approximately 5% to 7%.
-
For the group of overweight patients, the simulator reduced the clinical recommendation dosage by 17% to 24%.
-
For the group of obese patients, the simulator dosage reduced the clinical recommendation dose by up to 28%.
Finally, Fig. 9 illustrates the evaluation of the result of calculating the optimal radiotracer injection amounts in terms of lesion and tumor detection based on precision and recall values for a set of randomly selected patients. The comparative evaluation between simulator, clinical recommendation, and the theoretically calculated dosage shows a discrepancy in the values for the theoretical dosage for patients. Also, the simulator dosage provides a 4% to 5% downward optimization of the clinically recommended dose of injected radioactive substance.
3 Conclusion
The main purpose of this study is to predict the optimal dose of injected radiotracer for adult patients. To achieve our goal, we performed a set of simulations to assess the relationship between the quality of simulated PET images, the amount of radiotracer injected into the patient, and the patient’s physical parameters (age, weight). Each simulation was done using the PET scanner model and the patient model for a diagnostic task (tumor/lesion detection), and it calculates the PET image quality assessment variables NEC and SNR. From the results of those simulations, we concluded that our simulator can produce a desirable and efficient prediction of injected radiotracer amount that optimizes the current clinical amount downward by up to 28%. In addition, we can conclude that the total injected radiotracer dose for adult patients is mostly affected by the patient’s weight rather than the patient’s age.
References
Accorsi R, Karp JS, Surti S (2010) Improved dose regimen in pediatric PET. J Nucl Med 51(2):293–300
Alsanea E (2016) Prediction of radioactive injection dosage for PET image. King Abdul Aziz university
Augusto RS, Mohammadi A, Tashima H, Yoshida E, Yamaya T, Ferrari A, Parodi K (2018) Experimental validation of the FLUKA Monte Carlo code for dose and β2 -emitter predictions of radioactive ion beams. Phys Med Biol 63(21):215014
Boellaard R, O’Doherty MJ, Weber WA, Mottaghy FM, Lonsdale MN, Stroobants SG, Oyen WJ, Kotzerke J, Hoekstra OS, Pruim J (2010) FDG PET and PET/CT: EANM procedure guidelines for tumour PET imaging: version 1.0. Eur J Nucl Med Mol Imaging 37(1):181–200
Boldyš J, Dvořák J, Skopalová M, Bělohlávek O (2013) Monte Carlo simulation of PET images for injection dose optimization. Int J Numer Methods Biomed Eng 29(9):988–999
Cherry SR (2009) Multimodality imaging: beyond pet/ct and spect/ct. Semin Nucl Med 39:348–353
de SEOB Silva (2010) Small animal PET imaging using GATE Monte Carlo simulations: implementation of physiological and metabolic information
Dvořák J, Boldyš J, Skopalová M, Bělohlávek O (2013) Application of the random field theory in PET imaging-injection dose optimization. Kybernetika 49(2):280–300
Gillam JE, Rafecas M (2016) Monte-Carlo simulations and image reconstruction for novel imaging scenarios in emission tomography. Nucl Instrum Methods Phys Res Sect Accel Spectrometers Detect Assoc Equip 809:76–88
Kang J, Gao Y, Shi F, Lalush DS, Lin W, Shen D (2015) Prediction of standard-dose brain PET image by using MRI and low-dose brain [18F]FDG PET images. Med Phys 42:5301–5309
Karakatsanis NA, Loudos G, Rahmim A, Nikita KS (2014) Monte-Carlo based characterization of the counting rate (NECR) response for personalized optimization of the administered activity in clinical PET imaging. Front Biomed Technol 1(1):14–34
Ljungberg M (2004) Simulation techniques and phantoms. In: Emission tomography, the fundamentals of PET and SPECT, Elsevier Inc., pp 551–563
Mawlawi O (2009) DW Townsend (2009) Multimodality imaging: an update on PET/CT technology. Eur J Nucl Med Mol Imaging 36(1):15–29
Peter J, Tornia M, Jaszczek R (2000) Analytical versus voxelized phantom representation for Monte Carlo simulation in radiological imaging. Med Imaging IEEE Trans 19(5):556–564
Piepsz A, Hahn K, Roca I, Ciofetta G, Toth G, Gordon I, Kolinska J, Gwidlet J (1990) A radiopharmaceuticals schedule for imaging in paediatrics. Eur J Nucl Med 17(3–4):127–129
Saha GB (2010) Basics of PET imaging: physics, chemistry, and regulations. Springer, Berlin
Treves ST, Baker A, Fahey FH, Cao X, Davis RT, Drubach LA, Grant FD, Zukotynski K (2011) Nuclear medicine in the first year of life. J Nucl Med 52(6):905–925
Turco A (2012) Monte Carlo simulations of a small-animal PET scanner. Analysis of performances and comparison between camera designs
Waterstram-Rich KM, Christian PE (2013) Nuclear medicine and PET/CT: technology and techniques. Elsevier, Amsterdam
Xu J, Gong E, Pauly P, Zaharchuk G (2017) 200x low-dose PET reconstruction using deep learning
Yu S (2010) Simulation of PET brain images using Monte Carlo method. Master Thesis in Medical Imaging, School of Technology and Health Royal Institute of Technology, Stockholm, Sweden
Zaidi H (1999) Relevance of accurate Monte Carlo modeling in nuclear medical imaging. Med Phys 26(4):574–608
Zaidi H, Koral K (2006) Scatter correction strategies in emission tomography. In: Quantitative analysis in nuclear medicine imaging, Springer, pp 205–235
Acknowledgements
The project was funded by the Deanship of Scientific Research (DSR), King Abdulaziz University, Jeddah, under Grant No. (DF-578-611-1441). The authors, therefore, gratefully acknowledge DSR technical and financial support.
Funding
There was no fund for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Alsanea, E., Alhalabi, W. Prediction of radioactive injection dosage for PET imaging. Soft Comput 25, 5847–5854 (2021). https://doi.org/10.1007/s00500-021-05577-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00500-021-05577-9