Abstract
Homeostasis between pro-oxidants and anti-oxidants is necessary for aerobic life, which if perturbed and shifted towards pro-oxidants results in oxidative stress. It is generally agreed that reactive oxygen species (ROS) production is accelerated with mountainous elevation, which may play a role in spawning serious health crisis. Exposure to increasing terrestrial altitude leads to a reduction in ambient O2 availability in cells producing a series of hypoxic oxidative stress reactions and altering the redox balance in humans. Enormous literature on redox signaling drove research activity towards understanding the role of oxidative stress under normal and challenging conditions like high-altitude hypoxia which grounds for disturbed redox signaling. Excessive ROS production and accumulation of free radicals in cells and tissues can cause various pulmonary, cardiovascular, and metabolic pathophysiological conditions. In order to counteract this oxidative stress and maintain the balance of pro-oxidants and anti-oxidants, an anti-oxidant system exists in the human body, which, however, gets surpassed by elevated ROS levels, but can be strengthened through the use of anti-oxidant supplements. Such cumulative studies of fundamentals on a global concept like oxidative stress and role of anti-oxidants can act as a foundation to further smoothen for researchers to study over health, disease, and other pathophysiological conditions. This review highlights the interconnection between high altitude and oxidative stress and the role of anti-oxidants to protect cells from oxidative damages and to lower the risk of altitude-associated sickness.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
High altitude (HA), a special ecological environment arbitrarily defined as an elevation of 2500 m above sea level, can foster free radical formation due to resulting low partial pressure of oxygen in the blood and the resultant hypoxia. The hypoxic cells susceptible to oxidative stress, together with severe cold, high wind velocity, low humidity, high ultraviolet rays from the sun, dehydration, and lack of anti-oxidant nutrients in the diet, trigger a constellation of adverse effects, including acute mountain sickness (AMS) that can progress to potentially life-threatening complications such as high-altitude pulmonary edema (HAPE) or high-altitude cerebral edema (HACE) (Hultgren 1997; Askew 1995, 1997; Cymerman 1996; Huey and Eguskitza 2001).
Oxidative stress, a phenomenon commonly known as “Oxygen Paradox” (Goldfarb and Sen 1994) and implicated in various pathological conditions, occurs when reactive oxygen species (ROS) overwhelm the cellular anti-oxidant (AO) defense system, through either an escalation in ROS levels or a reduced capability of the cells to mount an effective anti-oxidant response. Evolutionarily, developed as an important part of the innate immune system (as a defense mechanism against bacteria), the term oxidative stress was used for the deleterious processes caused by ROS to almost all biomolecules in the 1970s and 1980s; however, later, German biochemist Helmut Sies defined it as an imbalance between oxidants and anti-oxidants in favor of the oxidants (Sies 1985, 1997; Rosen et al. 2009). One of the main sites of ROS production during high altitude–associated hypoxia could be the mitochondrial electron transport chain as the low availability of oxygen reduces mitochondrial respiration (Dosek et al. 2007; Mohanraj et al. 1998). At high altitude, ROS-generating systems are activated along with the repression of enzymatic and non-enzymatic anti-oxidant systems (Dosek et al. 2007; Mohanraj et al. 1998; Chang et al. 1989).
Indigenous people inhabiting mountainous high-altitude land are acclimatized to this environment through the evolution of mechanisms to relate oxygen supply and metabolism and subsequent energy generation (Hoppeler and Vogt 2001). However, individuals who travel acutely to altitude for short-to-moderate periods of time or intermittently, too high or too fast, jeopardize their normal physiology and experience reduced muscular function concomitant with hypoxia (Hoppeler and Vogt 2001; Brooks et al. 1999; Schoene 2001; Roach and Hackett 2001). Although it has been shown that performance at altitude can be eventually improved by physical training, it may not suffice to enhance performance upon return to sea level (Bailey and Davies 1997). Roach et al. (2000) have shown that exercise at altitude may aggravate AMS. Hypobaric hypoxia along with the stress generated from exercise may accentuate free radical–mediated oxidative tissue injury, thus exerting both short- and long-term consequences for health and performance (Bailey and Davies 1997; Bailey et al. 2000), and in fact, it has been suggested that the cumulative effects of hypoxic exposure may endure for some time even after return to sea level (Hornbein 2001; Neubauer 2001; Joanny et al. 2001). In the study of Operation Everest III, the level of oxidative stress was found to be parallel with the increase in altitude as the level of lipid peroxidation increased by 23% and 79% at 6000 and 8848 m, respectively (Joanny et al. 2001). In a study of US Marine Corps personnel training by Pfeiffer et al., a significant increase in oxidative stress associated with intense physical exertion, ultraviolet light exposure, and fluctuating temperatures at moderate altitudes was observed at the end of a 14-day field-training period (Pfeiffer et al. 1999). The present review draws upon the mechanisms for the generation of ROS, high altitude and oxidative stress, and the success in utilization of anti-oxidant supplements to ameliorate altitude-induced oxidative stress. Before going into detail, different reactive oxygen species source, formation, and biological significance are summarized in Table 1 along with the ROS generation that is schematically represented in Fig. 1a and b.
a Schematic representation of reactive oxygen species generation. b Reactive oxygen species production: Dismutation of O2•− to H2O2 occurs either non-enzymatically (Eq. 1) or through a reaction catalyzed by superoxide dismutases (SODs) (Eq. 2). H2O2 may be fully reduced to water or partially reduced to hydroxyl radical (Eq. 3), one of the strongest oxidants in nature, break down to HO• in the presence of transition metals like Fe2+ or Cu2+, called Haber-Weiss and Fenton reactions. In the first step, Fe(III) is reduced by O2•− (Eq. 4), followed by oxidation by H2O2 (Eq. 5). The reduced transition metals catalyzing the formation of HO• in turn may be oxidized by O2•−, propagating this process (Eq. 6). The hydroxyl radical is also produced when O2•− itself reacts with H2O2 (Eq. 7) or by single-electron oxidation of water (Eq. 8)
Hypoxia and ROS generation
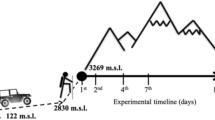
With altitude barometric pressure of the atmosphere reduces and simultaneously reduces the inspired oxygen partial pressure in the environment. Thus, there is reduced partial pressure of inhaled oxygen to the cells and tissues causing hypobaric hypoxia. Acute and prolonged exposure to hypobaric hypoxia causes ROS formation resulting in oxidative stress. This stress generally comes up in any system when the free radicals and active intermediates exceed the system’s ability to curb them disturbing the redox state of any aerobic cell. Normal intracellular metabolism and cytosolic enzyme systems are the source of ROS formation in both normoxic and hypoxic conditions. The only difference lies in low, normal, or higher ROS generation levels during both conditions which affect several body processes and physiological conditions accordingly (Fig. 2).
Mitochondrion-generated hypoxic ROS
The site of constant and major ROS production is mitochondria. Mitochondrial oxygen utilization and reduction through aerobic metabolism generates ROS like superoxide and hydrogen peroxide (Boveris and Cadenas 1982). This generation depends upon the resting or active mitochondrial state. As compared to cytosolic and nuclear, ROS production is about five to ten fold higher in mitochondrial matrix (especially in inner mitochondrial matrix). Furthermore, these ROS form hydroxyl radical generation (though the actual site of hydroxyl generation is not known) which depends upon the metabolic state (Richter et al. 1988; Richter et al. 1995). In mitochondria, oxygen sensing occurs at cytochrome oxidase because oxygen binds there (Bunn and Poyton 1996). Hypoxia elicits changes in the redox state of electron transport proteins of the proximal complexes upstream from the oxidase. This activity decreases the respiration rate due to limitation in ATP utilization and its hydrolysis by mitochondria during prolonged hypoxia. Majorly complex III in particular generates oxidants which stabilize the hypoxia-inducible factor -1 alpha (HIF-1α) during hypoxia (Chandel et al. 1997). Changes induced by hypoxia to redox state of cytochrome oxidase are not the sole mechanism which regulates HIF-1α activation; other mitochondrial complexes are also involved in its regulation. The vectorial transport of the ROS generation from complex III is released in such a way that more oxidants are released into the intermembrane space (IMS) and relatively less to matrix because the strong electric field is the driving force for superoxide anion to move to IMS. During hypoxia, the cytosol and IMS oxidation increases while mitochondrial matrix oxidation decreased due to increased production of ROS on the outer surface of the inner mitochondrial membrane (IMM) (Muller et al. 2004). This release of the ROS to the cytosol leads to further ROS signaling even if the effect of hypoxia has been diminished. Mitochondrial DNA (mtDNA) is more susceptible to oxidative damage as compared to nuclear DNA because of less protective histones, low DNA repair activity, and the constant formation of free radicals in mitochondria contributing to a highly reducing environment (Ames et al. 1995). The 10609 variant is a mitochondrial SNP, and an association between the variant and high-altitude acclimatization was identified that polymorphism in the 10609 variant can affect mitochondrial function. The mtDNA 10609 variant promoted hypoxia-induced increase of intracellular ROS in Han Chinese population. mtDNA 10609T promoted hypoxia-induced increase of intracellular ROS and is a high-altitude polycythemia (HAPC) risk factor (Jiang et al. 2014). Also, there is some kind of activation of complex II of mitochondria. During hypoxia, complex II switches from succinate dehydrogenase to fumarate reductase resulting in ROS generation and succinate accumulation (Paddenberg et al. 2003). Hence, mitochondrial redox changes that track with cellular PO2 cause ROS formation at complex III and trigger several functional responses. ROS release during hypoxia by IMM to the IMS leads to activation of transcription factors, most specifically hypoxia-inducible factors (HIF-1); also, FOXO-mediated transcription factors are activated upon cellular stress which further gets stabilized and impacts on various physiological responses of the body (Guzy and Schumacker 2006; Poyton et al. 2009; Hamanaka and Chandel 2010).
Hypobaric hypoxia activates other ROS-generating systems
During hypoxic conditions, NO• is generated by the mitochondrial respiratory chain. Further, superoxides interact with nitric oxide radical and generate peroxynitrites (which is a strong oxidant). Peroxynitrite concentration consistently increases under hypoxia because of its dependence on oxygen level. These NO-derived free radicals are called as reactive nitrogen species. During hypoxic conditions, NO2− reductase pathway is activated. This pathway works during oxygen-limiting conditions which produces mitochondrial NO and further reduces NO2− to NO via the respiratory chain route and has been proven in rats, mouse brain mitochondria, and human endothelial cells (Zhang and Gutterman 2006).
ROS formation in vascular compartments affects the redox-dependent cell signaling functions and also decreases NO availability by its direct interaction with superoxide. Xanthine oxidoreductase (XOR) is a significant source of cellular ROS and further promotes oxidant-induced cell signaling reactions in hypoxic conditions. When the oxidative phosphorylation declines during low oxygen concentration, anaerobic glycolysis occurs which leads to raised concentration of hypoxanthine and xanthine and they both act as xanthine dehydrogenase enzyme system. Xanthine oxidoreductase exists in two isoforms: XO (xanthine oxidase) and xanthine dehydrogenase (a cytosolic enzyme) (XDH). XDH can be converted to XO by thiol oxidation reactions or phosphorylation. Only XO produces ROS, which causes oxidative phosphorylation of purine substrates with the formation of O2− and H2O2 and under the influence of hypoxia, H2O2 is formed more than O2− (Poss et al. 1996; Lanzillo et al. 1996; Lance et al. 1997; Teradat et al. 1992). Prolonged hypoxia increases XO and its precursor XDH activity in cultured lung endothelial cells. Hypoxia induced increase in both XDH and XO activities but did not convert XDH to XO. This hypoxia-induced increase in activity of XO (present in endothelial cell (EC)) is related to the release of superoxide by EC. Furthermore, superoxide increases intracellular hydroxyl radical in EC. Oxidative damage caused to EC by XO influences albumin passage by depleting intracellular ATP levels by altering calcium homeostasis and cytoskeletal architecture.
NADPH oxidase too leads to the formation of free radicals, given hypoxic conditions for 3 weeks. Also, chronic exposure in rats causes an increase in NOX4 mRNA. NOX enzyme reduces the NO levels by reacting with it and forming peroxynitrite (Liu et al. 2006). Cytochrome P450–dependent microsomal electron transport system in mammals is another major source of ROS generation. CYP enzymes function as a part of NADPH/O2-dependent microsomal electron transport system and one of the most important cellular sources of reactive oxygen species. CYP enzymes localized in the smooth endoplasmic reticulum of the liver contain heme prosthetic group in the form of iron protoporphyrin IX, and this group is essential for enzymatic activity. P450 reaction cycle yields different forms of reactive oxygen like superoxides and peroxides (Liu et al. 2006; Lewis 2002).
Oxidative stress markers and high altitude
Oxidative stress is a mechanism which damages cellular molecules and imposes several toxicological implications. High altitude imposes excessive ROS production by various mechanisms which are capable of damaging proteins, nucleic acids, polysaccharides, and lipids. Several studies have mentioned the existence of markers which can be set as indicators of stress induced by hypoxia-generated ROS in aerobic organisms (Strapazzon et al. 2016). At high altitude under hypobaric hypoxia, ROS production is increased (Irarrázaval et al. 2017). Among damages to aerobic cell, they are most susceptible to membrane oxidation commonly called as lipid peroxidation. High-altitude climbing/trekking/exercise (Debevec et al. 2017) all causes increase in lipid peroxidation during metabolically induced cell damage. Lipid peroxidation in membranes of various cells of humans or animals causes an increase in exhaled pentane gas. Free radicals generated during hypoxia-induced oxidative damage cause changes in membrane lipids and proteins and affect the membrane fluidity (Kappus 1985). Majorly affected by oxidative stress in membranes are the polyunsaturated fatty acids (PUFAs). This attack of ROS on membrane PUFAs causes the normal cell functions to alter (Magalhães et al. 2005). Besides lipid peroxidation of cellular membranes, the red cell membrane fluidity changes and filterability deteriorates at high altitude. A major factor behind this phenomenon is vitamin E deficiency/depletion during stress conditions. Level of vitamin E or extent of its depletion is directly proportional to membrane damage (Simon-Schnass 1994). Red cell membrane enzymatic activity is also affected during exercise at HA. Exercise at HA influences the RBC’s anti-oxidant defense enzymes like superoxide dismutase and catalase (CAT) activity (Güzel et al. 2000). Higher concentration of thiobarbituric acid reactive substances (TBARS) in blood plasma was observed after the training exercise probably due to increase in lipid peroxidation and also oxygen-associated injury to muscle cell membranes (Wozniak et al. 2001; Ramazan et al. 2000; Bernabucci et al. 2002; Vani et al. 2010). Rats and mice exposed to intermittent hypoxia have increased blood pressure and higher ROS generation. Redox stress generated during intermittent hypoxia exposure leads to activation of hypoxia-inducible factors and several consequences like increased levels of endothelin in blood which causes vasoconstriction, production of inflammatory cytokines, and abnormal lipid metabolism (Friedman et al. 2014; Gangwar et al. 2020).
It has been of no contradiction that, during the hypoxic condition, there is decrease in reduced glutathione (GSH) and increase in oxidized glutathione. Glutathione disulfide (GSSG) concentration in plasma is a potent indicator of oxidative stress and is closely related to cellular redox changes in body. GSSG levels increased significantly during high-altitude exposure (Magalhaes et al. 2004). A decrease in GSH and an increase in GSSG were also reported in humans exposed to high altitude (Vats et al. 2008). Decreased activities of glutathione peroxidase, cytochrome c oxidase, and superoxide dismutase in mitochondrial lung are reported during HA exposure and are good indicators of oxidative stress (Lemoine et al. 2018). Oxidative DNA damage can be detected by measuring formamidopyrimidine DNA glycosylase (FPG), 8-oxoguanine DNA glycosylate 1 (OGG1), 4-hydroxynonenal (HNE), F2 isoprostanes, 8-OHDg, and 8-iso-PGF 2 alpha (Moller et al. 2001; Janocha et al. 2017; Jefferson et al. 2004).
Oxygen and oxygen-derived species in cell signaling
ROS are intracellular chemical species which are able to trigger various biological and signaling events (Finkel 2011). ROS plays a role in proliferation, differentiation, and other cellular events in the body. At a low concentration, ROS initiate biological processes, regulate several intracellular signaling, cause cell-to-cell communication, and are a stimulus to pass biological information from the cell surface to nucleus causing a signal transduction or cell signaling. While oxidative stress results in a significant increase in ROS and this accumulation of ROS is more associated with oxidative damage of lipids, proteins, and DNA (Glasauer and Chandel 2013; Schieber and Chandel 2014; Cross et al. 1987). ROS appear to modulate a number of kinases and phosphatases, redox-sensitive transcription factors, and genes associated with it. Thus, for ROS to act as a secondary messenger, its production and utilization must be in a controlled manner. During normal conditions, this activity is controlled tightly but during hypoxic conditions, this activity is imbalanced. Cells when stimulated by ROS undergo the same signaling activation as when experienced during growth factor signaling, but the problem with ROS signaling is that they are a bit small in size and highly reactive. ROS reacts very randomly and rapidly too within very short distances. The first signaling molecules to be considered redox sensitive are transcription factors, NF-κB, AP-1 Sp-1, c-Myc, p53, c-Myc and early growth response factor 1 (EGR-1), metal-responsive transcription factor (MIF-1) and upstream stimulatory factor, glucocorticoid receptor (GR), and cyclic AMP response element-binding protein (CREB). ROS are involved in the receptor signaling propagation and are increased by ligand binding of epidermal growth factor (EGF), platelet-derived growth factor (PDGF), transforming growth factor beta 1 (TGFβ1), etc. (Martindale and Holbrook 2002). Non-receptor tyrosine kinases and serine/threonine phosphorylation are activated by several ROS species like H2O2 and O2−. One electron reduction produces O2− and this is converted to H2O2 by superoxide dismutase. H2O2 is a good signaling molecule as it can easily pass through membranes.
HIF stabilization during ROS signaling in hypoxic conditions
HIF-1 is a heterodimer which consists of two subunits, i.e., HIF-1α (oxygen regulated) and HIF-1β (constitutively expressed and not oxygen regulated). HIF complex is regulated by oxygen-dependent hydroxylation of specific hydroxylases by HIF prolyl hydroxylases (PHDs, member of family 2-oxoglutarate-dependent dioxygenase) like PHD1, PHD2 and PHD3. After hydroxylation, VHL (von Hippel-Lindau, a component of E3 ubiquitin ligase) protein binds and subsequent degradation of α subunit occurs by ubiquitin proteasome pathway. These PHDs cause α subunit to degrade during oxygen conditions, while it cannot degrade in oxygen-deficient conditions, resulting in dimerization and stabilization of HIF-1α with HIF-1β (Schofield and Ratcliffe 2005). When one moves to high altitude, there is attenuated PHD2 hydroxylase activity resulting in increased HIF-1α levels. Thus, it is very much clear that HIFs are key players in cellular responses in relation to limited O2 supply. It is of no conflict that all PHD forms are essential in regulating HIF. It has been observed that PHD2 suppression alone can augment the level of HIF-1α more than HIF-2α and PHD3 suppression alone can increase the level of HIF-2α more than HIF-1α (Appelhoff et al. 2004). Silencing of PHD2 with siRNAs alone is sufficient to stabilize HIF-1α in normoxic human cells while silencing PHD1 and PHD3 in both normoxic and hypoxic conditions has no effect on the stability of HIF-1α (Berra et al. 2003). Thus, PHD2 can be called as a critical oxygen sensor. ROS and HIF-1α are involved in the hypoxic signaling processes. In humans, ROS could be involved in the first phase of regulation of HIF-1α gene expression, as indicated by the positive correlation between both HIF-1α gene expression and DNA oxidation markers (Kietzmann and Görlach 2005). ROS directly inhibit PHDs and thus overall increase in HIF-1α mRNA accumulation (Pialoux et al. 2009).
Heme-containing oxidases control ROS levels and HIF-1α under hypoxia. Heme-containing oxidase like NADPH oxidase converts O2 to O2•− and afterward to H2O2, and it acts as signaling molecules mediating response to hypoxia. Heme-containing enzymes such as NADPH oxidases or cytochrome b-type NAD(P)H oxidoreductase or mitochondria may produce ROS depending on the PO2 (Kietzmann and Görlach 2005). As discussed in the previous section, mitochondria produce ROS and during hypoxia redox potential of mitochondria changes which lead to overproduction of ROS and this may lead to participation in other transcriptional responses. Mitochondrial ROS is required in HIF-1α DNA binding activity (Chandel et al. 1998). It has been observed that in p° cells (deficient in mitochondrial DNA), there is no rise in ROS generation, HIF-1α protein accumulation and HIF-1α-dependent gene expression during hypoxia (Agani et al. 2000). Complex III of mitochondrial electron transport chain is required for the hypoxic stabilization of HIF-1α and HIF-2α and an increase in ROS links this complex to HIF stabilization. Using siRNA to suppress the expression of the Rieske iron-sulfur protein of complex III, hypoxia-induced HIF-1α stabilization is attenuated. Further, ROS production decreased as measured by a novel ROS-sensitive fluorescence resonance energy transfer probe. It is thus clear that mitochondria work as O2 sensors and also signal hypoxic HIF-1α and HIF-2α stabilization by generating and releasing ROS to the cytosol (Guzy et al. 2005; Chandel et al. 2000). Crosstalk among various signaling cascades triggered by high or low ROS levels might influence the stability and further activity of HIF-1α.
Nuclear factor erythroid-related factor 2 as guardian to redox homeostasis during hypoxia
The transcription factor nuclear factor erythroid-related factor 2 (Nrf2) regulates anti-oxidant, anti-inflammatory, and cytoprotective genes during hypobaric hypoxia and is the guardian to redox homeostasis. During stress condition, Nrf2 is released from KEAP1 (Kelch-like erythroid cell–derived protein with CNC homology [ECH]–associated protein 1) (Oh and Jun 2017; Huang et al. 2002). After its release, it is translocated to the nucleus and activates genes which confer resistance to a variety of oxidative stress–related neurodegenerative molecules. All these genes contain this cis-acting ARE. Nrf2-ARE activation is a neuroprotective pathway providing short-term protection against chronic hypobaric hypoxia (Kensler et al. 2007; Rushmore et al. 1991). Other targets downstream to Nrf2, heme oxygenase (HO-1), SOD, thioredoxin (Trx), glutathione S-transferase (GST), and glutamate-cysteine ligases (GCLC and GCLM) are upregulated in response to hypobaric hypoxia (Sethy et al. 2011; Satoh et al. 2006; Innamorato et al. 2008).
Hypoxia and oxidative stress caused due to fluctuations in cellular oxygen affect HIF-1α (involved in the regulation and expression of genes important for cells to hypoxia) and Nrf2 (induced in response to oxidative stress and exert a cytoprotective role). Lung adenocarcinoma cell line (A549) expresses the high levels of NADPH oxidase 1 (NOX1) which is crucial for increased ROS production during intermittent hypoxia and further induces HIF-1α and Nrf2. It also regulates Nrf2 target unit thioredoxin 1 (Trx1). Inhibition of endogenous NOX1 inhibits the targeted expression of Nrf2 and Trx1 while overexpression of NOX1 recombinant protein results in an increase in Nrf2 and Trx1. Dual upregulation of both the factors overall increases HIF-1α signaling during intermittent hypoxia, establishing the fact that Trx1 may probably set a link between Nrf2 and HIF-1α. Nrf2 is considered a transcription factor regulating anti-oxidant and detoxification genes (Malec et al. 2010).
Cells surviving H2O2 treatment showed reduced mitochondrial components like cytochrome c/b. Cells showing Nrf2 overexpression prevented H2O2 from decreasing mitochondrial-related morphological changes and cytochrome b/c. Nrf2 is linked to the outer mitochondrial membrane as it has been proven that mitochondria produced from the myocardium of Nrf2 knockout mice undergo permeability transition, hypersensitive to mitochondrial toxins and has decreased mitochondrial membrane potential. Direct interaction of Nrf2 with mitochondria resulted in decreased oxidative stress in mitochondria (Strom et al. 2016). Also, in cardiomyocytes and mouse embryonic fibroblast culture, Nrf2 gene KO produces high ROS levels. It has been demonstrated that induction of HO-1 and NOX-1 causes removal of damaged mitochondrial units and maintains its function. Thus, Nrf2 has possibly the role in preventing oxidative stress–induced increase in calcium overload and preventing mitochondrial membrane integrity by preventing its membrane transition (Lee et al. 2003; Kovac et al. 2015; Piantadosi et al. 2008).
Peroxisome proliferator–activated receptor-gamma coactivator (PGC)-1alpha and SIRT are associated with HIF-1α activity in hypoxic ROS signaling
Hypoxic signaling increases HIF stabilization in cells and enhances ROS signaling in hypoxic cells. Mitochondria exposed to hypoxia are self-destructed via autophagy which helps in reducing ROS and provides sufficient oxygen supply to the remaining mitochondria. In skeletal muscle cells, PGC-1alpha activity is tightly coupled with HIF-1α activity. Mitochondrial biogenesis increases with rise in PGC-1alpha; this leads to increase oxygen consumption and intracellular hypoxia and thus HIF-1α stabilization. It is important to match the mitochondrial biogenesis and mitochondrial autophagy to match oxygen demand and oxygen supply (Ohagan et al. 2009; Murray 2009). Sirtuins (SIRT, NAD-dependent deacetylases) are regulated in terms of ratio of NAD and NADH. High NAD levels activate sirtuins while high NADH levels suppress its activity. SIRT1 is known to downregulate HIF-1α activity by deacetylating it during hypoxia. This process of deacetylation is dependent on the NAD levels during hypoxia (Lin and Guarente 2003). Another member of the same family, SIRT6, is known to downregulate HIF-1α-mediated transcription by binding to chromatin on hypoxia response element (HRE) (Zhong et al. 2010). SIRT3 is most studied and its overexpression downregulates the ROS production and HIF stabilization. Similarly, if SIRT3 is downregulated, then it stabilizes HIF-1α and starts downstream signaling during exposure to hypoxia. SIRT3 downregulation during hypoxia increased levels of all putative HIF-1 α targets such as VEGF-A, phosphoglycerate kinase 1 (PGK-1), and phosphoinositide-dependent protein kinase-1 (PDK-1) (Bell et al. 2011). Physical exercise–induced ROS generations are important in modulating the several factors of mitochondrial biogenesis like MAP kinases, SIRT1 and PGC-1alpha. All these are modulated by redox state changes in the body. PGC-1alpha decreases ROS generation by activating anti-oxidant enzyme or by increasing the mitochondrial production. ROS-mediated increase in HIF-1α and its stabilization resulted in controlled angiogenesis during exercise. Also, exercise-induced ROS cause methylation in DNA and histone-associated post-translational modification (Radak et al. 2013).
Oxidative stress and inflammation in the brain at high altitude
There are cerebral symptoms like HACE and AMS at high altitude for which subclinical inflammation has been speculated in the brain. Upregulation of aquaporin 4 in astrocytes and water permeability by toll-like receptors has been seen to cause systemic inflammation in the brain by activation of corticotropin-releasing hormone receptor type-1 in central microglia, followed by local secretion of corticotrophin-releasing hormone in the brain (Song et al. 2016). Also, hypoxic stress and associated inflammation cause alteration in the functional integrity of the blood-brain barrier which is essential to maintain the central nervous system homeostasis. The blood-brain barrier disruption by increased paracellular permeability may cause alteration in the tight junctions and further systemic central nervous system drug uptake (Lochhead et al. 2017). It has also been observed that intermittent hypoxia induced injury in the brain and specifically affects cortical, subcortical, and hippocampal regions and causes apoptosis of neurons. This process selectively happens via oxidative stress and inflammatory pathways (Zhang et al. 2012). Thus, hypoxia and oxidative stress have severe pathological and neurological consequences.
Anti-oxidant defense system and its status in body
Detoxification of ROS is paramount to the survival of all aerobic life forms. In order to ameliorate the deleterious effects engendered by oxidants, the human body is equipped with an impressive repertoire of anti-oxidants, which can be classified as enzymatic and non-enzymatic or can be exogenously supplied through foods and supplements (Table 2). They play an effective role as free radical scavengers by donating their own electrons to ROS, thus counteracting the adverse effects of the latter (Fig. 3) (Kunwar and Priyadarsini 2011; Shinde et al. 2012; Birben et al. 2012). Anti-oxidant may work at three different levels in the body: (a) prevention, maintaining ROS formation to a minimum level; (b) interception, scavenging reactive species by using either catalytic or non-catalytic molecules; and (c) repair, removing and repairing damaged biomolecules (Sies 1986). On adaptation to stress conditions, they hold the capability to generate appropriate AO enzymes and transfer these enzymes to the right site at a specific time period and at a right concentration. The activity of anti-oxidants also produces free radicals which sometimes acts as pro-oxidant. Thus, it is necessary that a complete chain reaction occurs so that the generated radical is stabilized by resonance or steric hindrance. This is important in determining the efficacy of anti-oxidants. Supplementation can be given in the form of single vitamin, which sometimes may inhibit the radical load, or as mixture of anti-oxidants which provides a synergistic effect (by interaction between anti-oxidants). It has been observed that the anti-oxidant defense system weakens at high altitude, which, however, can be overcome by anti-oxidant supplementation or by natural anti-oxidant production in the body (Poljsak et al. 2013; Halliwell 2011).
Effective role of anti-oxidants as free radical scavengers: CuZn-SOD dismutation mechanism comprises two stages: (i) reduction of Cu(II) form of the enzyme by superoxide, releasing di-oxygen (Eq. 9), and (ii) oxidation of reduced Cu(I) by another superoxide anion and two protons, generating H2O2 (Eq. 10). (i) Reduction of H2O2 to H2O by heme Fe+3 generating covalent Fe+4 = O species with a porphyrin π-cation radical (compound I) (Eq. 11) and (ii) oxidation of second peroxide molecule to O2 by compound I releasing the ferryl oxygen species as H2O (Eq. 12). Oxidation of selenol gives selenenic acid (E-SeOH) (Eq. 13), which reacts with reduced GSH to form a selenenyl sulfide adduct (E-Se-SG) (Eq. 14). The active form of the enzyme is regenerated by a second GSH via the attack of E-Se-SG forming oxidized glutathione (GSSG) (Eq. 15)
Anti-oxidant supplementation studies to reduce the effect of hypoxic ROS
Free radical load generated at high altitude induces several metabolic and physiological changes. Oxidative stress acts as a pathogenic factor in various respiratory diseases and lungs by activation of several ROS-generating systems like xanthine oxidase. At HA, the effect of oxidative stress can be mitigated by exogenous nutritional supplements like β-carotene, quercetin, resveratrol, vitamin C and vitamin E that quench the singlet oxygen and other free radicals (Stellingwerff et al. 2019; Koivisto et al. 2019). Literature report reveals that the ventilatory threshold (VT) decreases upon ascent to HA, but improves with acclimatization. Subjects exposed to 4300 m of hypoxia with prior AO supplementation were shown to have improved VT upon acute, but not chronic exposure (Subudhi et al. 2006; Masella et al. 2005). In a study by Xu et al., rats supplemented with resveratrol, a natural non-flavonoid polyphenol phytoalexin, were exposed to a high-altitude hypoxia environment. The results revealed that resveratrol ameliorated the enlargement of the lung and spleen mediated by hypobaric hypoxia. Moreover, lowering of serum and liver malondialdehyde, plasma high-density lipoprotein and cholesterol levels, liver CCAAT/enhancer-binding protein alpha (C/EBPa), peroxisome proliferator–activated receptor g (PPARg), and HIF-1α and HIF-2β expression levels were observed. In addition, resveratrol increased liver SOD and fat hormone-sensitive lipase (HSL) activity, and Sirt-1 expression levels, together with the suppression of fat acetyl-CoA carboxylase (ACC), carnitine palmitoyltransferase (CPT-I) and fatty acid synthetase (FAS) activity. Thus, the data demonstrated the effective alleviation of hypoxia-induced oxidative stress by resveratrol along with the modulation of lipid metabolism, which is associated with the HIF signaling pathway (Xu et al. 2016). Sarada et al. evaluated the effect of β-carotene on oxidative stress induced by hypoxia on male albino rats. The increasing trend of malondialdehyde levels in plasma and tissues, and a concurrent decrease in blood glutathione, glutathione peroxidase, and plasma protein on hypoxia exposure were reversed on supplementation with β-carotene, suggesting it to possess potent anti-oxidant activities in reducing the oxidative stress induced by hypobaric hypoxia (Sarada et al. 2002). Quercetin, a flavonol widely present in fruits and vegetables, has been reported to exhibit anti-oxidant effects as free radical scavengers, hydrogen-donating compounds, singlet oxygen quenchers, and metal ion chelators, and lowers oxidative stress and lipid peroxidation. The reduction in hypoxia-induced increase in ROS and MDA production together with the restoration of anti-oxidant enzyme levels, such as GPx, GSH and SOD, by quercetin has been well documented in literature (Patir et al. 2012). A possibility of the use of cobalt for the prevention of oxidative stress induced by hypoxia has also been explored. According to a report by Shrivastava and co-workers, it was found that the administration of cobalt chloride attenuated the generation of ROS, and oxidation of lipids and proteins, while maintaining the GSH/GSSH ratio. The reduction in hypoxic oxidative stress by cobalt supplementation was achieved through the maintenance of higher cellular HO-1 and metallothionein (MT) levels mediated by HIF-1α signaling mechanisms (Shrivastava et al. 2008).
Pfeiffer et al. studied the effect of anti-oxidant supplement consisting of a daily dose of 20,000 IU β-carotene, 400 IU vitamin E, 500 mg vitamin C, 100 μg selenium, and 30 mg zinc in mitigating oxidative stress induced in US Marine Corps personnel training at moderate altitudes along with ultraviolet light exposure and fluctuating temperatures. Some diminution of oxidative stress indicators was brought about by AO supplementation; however, it was not effective in reducing all oxidative stress indicator levels back to baseline values (Pfeiffer et al. 1999; Chao et al. 1999). Furthermore, the efficiency of an anti-oxidant mixture comprising vitamin E, β-carotene, ascorbic acid, selenium, α-lipoic acid, N-acetyl 1-cysteine, catechin, lutein, and lycopene to reduce oxidative stress in US Marines undergoing 24 days of cold-weather field training at a moderate altitude was examined by Schmidt and co-workers. The results concluded that the supplement under investigation was not effective in attenuating the mean levels of oxidative stress in the entire test group; however, few individuals with low initial anti-oxidant status might have derived some benefit from it (Schmidt et al. 2002). In an investigatory study of l-arginine and anti-oxidant vitamins E and C on the cardiovascular performance of broiler chickens grown under chronic hypobaric hypoxia, it was found that arginine supplementation improved the pulmonary vascular performance of hypoxic chickens, with its enhanced effects observed on the addition of vitamins E and C. It was speculated that NO bioavailability increased and oxidative damage decreased as a consequence of synergistic roles of arginine and anti-oxidant vitamins, thus improving cardiopulmonary performance (Bautista-Ortega and Ruiz-Feria 2010). On the other hand, in a study by Hagobian et al., no rise in plasma cytokines, primarily IL-6, TNF-α, and CRP concentrations, was observed for the AO-supplemented group at 4300 m (Hagobian et al. 2006). The effects of anti-oxidant vitamins on new born and placental traits in gestations at high altitude were studied by Parraguez et al., wherein it was concluded that vitamin C and E supplementation during pregnancy prevented hypoxia-induced oxidative stress and, thus, improved pregnancy outcomes (Parraguez et al. 2011). ROS production–associated oxidative stress at high altitude results in memory impairment, with the hippocampus being the most vulnerable towards hypoxic damage. Barhwal et al. investigated the effect of acetyl-l-carnitine on spatial working memory deficits together with oxidative and apoptotic damage in rats exposed to chronic hypobaric hypoxia at a simulated altitude of 6100 m. It was revealed that supplementation with acetyl-l-carnitine ameliorated working memory impairment, reduced oxidative stress, and inhibited hypoxia-induced apoptotic cascade (Barhwal et al. 2007). Alga Spirogyra porticalis inhabiting the Trans-Himalayan Region has immense potential to counter oxidative stress as a nutraceutical supplement (Kumar et al. 2019).
During HA exposure, there is increase in body’s AO defense system such as increase in urate/uric acid (most abundant aqueous AO), which is responsible for contributing to 2/3rd of total anti-oxidant capacity in the human body. The factors which are responsible for increase in urate during hypoxia augment xanthine oxidase–associated increase in free radical load. Breakdown of adenosine by XO also induces increase in urate during hypoxia (Sinha et al. 2009b). There is a significant correlation between urate (present in plasma) and anti-oxidant capacity at HA hypoxia (Baillie et al. 2007). A decrease in GSH and an increase in GSSG were reported in humans exposed to high altitude affecting glutathione metabolism. These changes can be enhanced by supplementation of N-acetyl cysteine and vitamin E (Vats et al. 2008). Lifelong exposure to hypoxia results in a higher GSH/GSSG ratio, higher SOD activity, and overall higher anti-oxidant status in the body for proper acclimatization to HA (Sinha et al. 2009a). Vij et al. (2005) reported that sojourners traveling to HA and acclimatizing there for around 3 months may not show a protective AO defense system. TBARS were higher; non-enzymatic anti-oxidants like ascorbic acid and ceruloplasmin were significantly lower, along with marginal alteration in plasma total anti-oxidant status (TAS), glutathione levels, and SOD activity as compared to their basal values. However, a longer stay for more than a year at altitude led to a reversion of the TBARS levels back to pre-exposure levels. The improvement in TAS, SOD activity, glutathione, ascorbic acid and ceruloplasmin levels was observed, suggesting the activation of anti-oxidant defense system during prolonged high-altitude exposure (Vij et al. 2005). In a recent study, high altitude–induced fatigue was ameliorated using phenylethanoid glycosides from Gansu Maxianhao as they are potential anti-oxidants and regularize energy metabolism by controlling the adverse metabolic products, upsurge energy substances reserve thus help lessen fatigue caused by hypoxia exposure (Yu et al. 2020).
Patterson et al. suggested four possible reasons behind the lack of a measurable effect attributable to anti-oxidant supplementation: (1) vitamin anti-oxidant formulations based upon in vitro studies may be inefficient scavengers in vivo; (2) detrimental ROS may be compartmentalized at sites within the cell that are inaccessible by the administered anti-oxidant; (3) anti-oxidants may possess toxicities that mask their advantageous effect, such as pro-oxidant effects or scavenging free radicals useful for other processes such as cell signaling; and (4) only a group of people may be at a risk of increased oxidative stress (Patterson et al. 2000).
Thus, the determination of appropriate combination and amounts of anti-oxidant nutrients to mitigate oxidative stress yet permitting critical adaptations to hypoxia involving ROS and cell signaling to occur is a challenge that needs to be addressed.
Anti-oxidant supplementation in prevention of altitude-associated sickness
ROS, responsible for alterations in vascular endothelial permeability, results in high altitude–associated pathophysiological conditions like AMS, HAPE and HACE, which can be attenuated by AO supplementation. The treatments of choice include descent and supplementary oxygen; however, in case of severe illness, the combination proves to be an optimal therapy. In fact, de-induction may reduce symptoms of pathophysiological conditions; however, medical therapy comes into play when descent is not possible or supplementary oxygen is not available. Botao and co-workers showed that Ginkgo biloba (GB) extract exhibited a protective effect on HACE in rats, which could be attributed to its anti-oxidant properties and suppression of the caspase-dependent apoptosis pathway. It was observed that GB-treated subjects possessed reduced MDA concentration and active caspase-3 expression along with the increase in SOD activity and GSH concentration (Botao et al. 2013).
Patir et al. elucidated the role of quercetin in reducing hypoxia-induced cerebral edema using male Sprague Dawley rats as an animal model. It was demonstrated that quercetin-administered hypoxia-exposed rats exhibited no edema and inflammation in their brain sections. Moreover, the study revealed that quercetin possessed superior drug in ameliorating high-altitude cerebral edema as compared to dexamethasone by acting as a potent anti-oxidant as well as an anti-inflammatory agent without any side effects (Patir et al. 2012).
Similarly, the general altitude-related sickness called as acute mountain sickness can be lowered by AO supplementation. An anti-oxidant mixture of l-ascorbic acid, α-tocopherol acetate and α-lipoic acid resulted in a reduced Lake Louise AMS score, increased arterial oxygen saturation levels, and calorie intake, suggesting that the attenuation of AMS and improvement in the physiological profile of mountaineers at high altitude could be achieved by exogenous delivery of water- and lipid-soluble anti-oxidant vitamins at the prescribed doses (Bailey and Davies 2001). AMS development with a gradual ascent to an altitude of around 5000 m directly correlated with an increase in serum hydroperoxides. Vascular damage was also observed with increased AMS symptoms. AO supplementation like AO vitamins had a major prophylactic effect, reduced oxidative markers and enhanced total GSH, and overall redox oxidative condition during HA hypoxia (Magalhaes et al. 2004; Araneda et al. 2005).
Supplementation with GB can probably act as a better alternative to acetazolamide, which is also used to curb symptoms of AMS. Prophylactic action of GB leads to hypoxic tissue protection, maintains the AO activity in tissues and prevents AMS with no probable side effects (Gertsch et al. 2004). As a consequence of oxidative damage to the endothelium, there occurs the leakage of cerebrovascular fluid resulting in AMS. In a study by Baillie et al., lowland volunteers ascended to 5200 m were given a dose of ascorbic acid, α-tocopherol acetate, and α-lipoic acid; however, it was observed that 69 and 66% of the anti-oxidant and placebo groups, respectively, had AMS, revealing that there was no benefit from AO supplementation at high altitude (Baillie et al. 2009).
Henceforth, it can be said that there are prophylactic benefits of these pharmacological agents, but the strategies to combat pathophysiological conditions at altitude must intend to define dosage, use, and combination of anti-oxidants which all can help enhance or benefit the near to healthy stay at high altitude for sojourns.
Conclusion
High altitude and free radical production leading to oxidative damage have received considerable attention. Increasing evidence from studies on cell line, rat and human models generate data which implicate the presence of ROS during acute and prolonged high-altitude exposure. ROS overload has a major impact from cell surface to cell signaling downstream to it affecting overall physiological profile of individuals at or exposed to high altitude. Dietary anti-oxidant or vitamin supplementation is evidently safe and a possibly effective intervention that can attenuate the ROS load and can prevent the occurrence of altitude-associated sickness. Thought has to be given to recognize when oxidative damage become possibly damaging enough to provide anti-oxidant therapy. Appropriate blend and quantity of anti-oxidant supplementation essential to provide control of excess ROS and also allow cell to execute cell signaling for critical adaptation to hypoxia is perplexing. Thus, understanding the pharmacological profile of reactive oxygen species, redox-sensitive intracellular signaling pathways, anti-oxidant enzyme family importance and anti-oxidant supplementation to detoxify ROS is imperative.
References
Agani FH, Pichiule P, Chavez JC, LaMann JC (2000) The role of mitochondria in the regulation of hypoxia-inducible factor 1 expression during hypoxia. J Biol Chem 275:35863–35867
Ames BN, Shigenaga MK, Hagen TM (1995) Mitochondrial decay in aging. Biochim Biophys Acta 1271:165–170
Appelhoff RJ, Tian YM, Raval RR, Turley H, Harris AL, Pugh CW, Ratcliffe PJ, Gleadle JM (2004) Differential function of the prolyl hydroxylases PHD1, PHD2, and PHD3 in the regulation of hypoxia inducible factor. J Biol Chem 279:38458–38465
Araneda OF, García C, Lagos N, Quiroga G, Cajigal J, Salazar MP, Behn C (2005) Lung oxidative stress as related to exercise and altitude. Lipid peroxidation evidence in exhaled breath condensate: a possible predictor of acute mountain sickness. Eur J Appl Physiol 95:383–390
Askew EW (1995) Environmental and physical stress and nutrient requirements. Am J Clin Nutr 61:631S–637S
Askew EW (1997) Nutrition and performance in hot, cold, and high altitude environments. In: Wolinsky I (ed) Nutrition in exercise and sport, 3rd edn. CRC Press, Boca Raton, pp 597–619
Bailey DM, Davies B (1997) Physiological implications of altitude training for endurance performance at sea level: a review. Br J Sports Med 31:183–190
Bailey DM, Davies B (2001) Acute mountain sickness; prophylactic benefits of antioxidant vitamin supplementation at high altitude. High Alt Med Biol 2:21–29
Bailey DM, Davies B, Young IS (2000) Evidence for reactive oxidant generation during physical exercise and normobaric hypoxia in man. J Physiol C27:47P
Baillie JK, Bates MG, Thompson AA, Waring WS, Partridge RW, Schnopp MF, Simpson A, Gulliver-Sloan F, Maxwell SR, Webb DJ (2007) Endogenous urate production augments plasma antioxidant capacity in healthy lowland subjects exposed to high altitude. Chest 131:1473–1478
Baillie JK, Thompson AA, Irving JB, Bates MG, Sutherland AI, Macnee W, Maxwell SR, Webb DJ (2009) Oral antioxidant supplementation does not prevent acute mountain sickness: double blind randomized placebo-controlled trial. QJM 102:341–348
Barhwal K, Singh SB, Hota SK, Jayalakshmi K, Ilavazhagan G (2007) Acetyl-L-Carnitine ameliorates hypobaric hypoxic impairment and spatial memory deficits in rats. Eur J Pharmacol 570:97–107
Bautista-Ortega J, Ruiz-Feria CA (2010) L-arginine and antioxidant vitamins E and C improve the cardiovascular performance of broiler chickens grown under chronic hypobaric hypoxia. Poult Sci 89:2141–2146
Bell EL, Emerling BM, Ricoult SJ, Guarente L (2011) SirT3 suppresses hypoxia inducible factor 1α and tumor growth by inhibiting mitochondrial ROS production. Oncogene 30:2986–2996
Bernabucci U, Ronchi B, Lacetera N, Nardone A (2002) Markers of oxidative status in plasma and erythrocytes of transition dairy cows during hot season. J Dairy Sci 85:2173–2179
Berra E, Benizri E, Ginouvès A, Volmat V, Roux D, Pouysségur J (2003) HIF prolyl-hydroxylase 2 is the key oxygen sensor setting low steady-state levels of HIF-1a in normoxia. EMBO J 22:4082–4090
Birben E, Sahiner UM, Sackesen C, Erzurum S, Kalayci O (2012) Oxidative stress and antioxidant defense. World Allergy Organ J 5:9–19
Botao Y, Ma J, Xiao W, Xiang Q, Fan K, Hou J, Wu J, Jing W (2013) Protective effect of ginkgolide B on high altitude cerebral edema of rats. High Alt Med Biol 14:61–64
Boveris A, Cadenas E (1982) Production of superoxide radicals and hydrogen peroxide in mitochondria. In: Oberley LW (ed) Superoxide dismutase. CRC Press, Boca Raton, pp 15–30
Brooks GA, Fahey TD, White TP, Baldwin K (1999) Exercise, atmospheric pressure, air pollution, and travel. In: Exercise Physiology. Mayfield, Mountain View, CA ; pp 504–536
Bunn HF, Poyton RO (1996) Oxygen sensing and molecular adaptation to hypoxia. Physiol Rev 76:839–885
Chandel NS, Budinger GRS, Choe SH, Schumacker PT (1997) Cellular respiration during hypoxia: role of cytochrome oxidase as the oxygen sensor in hepatocytes. J Biol Chem 272:111–112
Chandel NS, Maltepe E, Goldwasser E, Mathieu CE, Simon MC, Schumacker PT (1998) Mitochondrial reactive oxygen species trigger hypoxia-induced transcription. Proc Natl Acad Sci 95:11715–11720
Chandel NS, McClintock DS, Feliciano CE, Wood TM, Melendez JA, Rodriguez AM, Schumacker PT (2000) Reactive oxygen species generated at mitochondrial complex III stabilize hypoxia-inducible factor-1a during hypoxia: a mechanism of O2 sensing. J Biol Chem 275:25130–25138
Chang SW, Stelzner TJ, Weil JV, Voelkel NF (1989) Hypoxia increases plasma glutathione disulfide in rats. Lung 167:269–276
Chao W, Askew EW, Roberts DE, Wood SM, Perkins JB (1999) Oxidative stress in human during work at moderate altitude. J Nutr 129:2009–2012
Cross CE, Halliwell B, Borish ET, Pryor WA, Ames BN, Saul RL, McCord JM, Harman D (1987) Oxygen radicals and human disease. Ann Int Med 107:526–545
Cymerman A (1996) The physiology of high-altitude exposure. In: Marriott BM, Carlson SJ (eds) Nutritional needs in cold and high-altitude environments. National Academy Press, Washington, DC, pp 295–317
Debevec T, Millet GP, Pialoux V (2017) Hypoxia-induced oxidative stress modulation with physical activity. Front Physiol 8:84
Dosek A, Ohno H, Acs Z, Taylor AW, Radak Z (2007) High altitude and oxidative stress. Respir Physiol Neurobiol 158:128–131
Finkel T (2011) Signal transduction by reactive oxygen species. J Cell Biol 194:7–15
Friedman JK, Nitta CH, Henderson KM, Codianni SJ, Sanchez L, Ramiro-Diaz JM, Howard TA, Giermakowska W, Kanagy NL, Gonzalez Bosc LV (2014) Intermittent hypoxia-induced increases in reactive oxygen species activate NFATc3 increasing endothelin-1 vasoconstrictor reactivity. Vasc Pharmacol 60(1):17–24
Gangwar A, Paul S, Ahmad Y, Bhargava K (2020) Intermittent hypoxia modulates redox homeostasis, lipid metabolism associated inflammatory processes and redox post-translational modifications: benefits at high altitude. Sci Rep 10:7899
Gertsch JH, Basnyat B, Johnson EW, Onopa J, Holck PS (2004) Randomised, double blind, placebo controlled comparison of Ginkgo Biloba and acetazolamide for prevention of acute mountain sickness among Himalayan trekkers: the prevention of high altitude illness trial (PHAIT). BMJ 328:797
Glasauer A, Chandel NS (2013) ROS. Curr Biol 23:R100–R102
Goldfarb AH, Sen CK (1994) Antioxidant-supplementation and control of oxygen. In: Sen CK, Packer L, Osmo H (eds) Exercise and oxygen toxicity. Elsevier, New York, pp 163–190
Güzel NA, Sayan H, Erbas D (2000) Effects of moderate altitude on exhaled nitric oxide, erythrocytes lipid peroxidation and superoxide dismutase levels. Med Sci Sports Exerc Jpn J Physiol 50:187–190
Guzy RD, Schumacker PT (2006) Oxygen sensing by mitochondria at complex III: the paradox of increased reactive oxygen species during hypoxia. Exp Physiol 91:807–819
Guzy RD, Hoyos B, Robin E, Chen H, Liu L, Mansfield KD, Simon MC, Hammerling U, Schumacker PT (2005) Mitochondrial complex III is required for hypoxia-induced ROS production and cellular oxygen sensing. Cell Metab 1:401–408
Hagobian TA, Jacobs KA, Subudhi AW, Fattor JA, Rock PB, Muza SR, Fulco CS, Braun B, Grediagin A, Mazzeo RS, Cymerman A, Friedlander AL (2006) Cytokine responses at high altitude: effects of exercise and antioxidants at 4300 m. Med Sci Sports Exerc 38:276–285
Halliwell B (2011) Free radicals and antioxidants-quo vadis? Trends Pharmacol Sci 32:125–130
Hamanaka RB, Chandel NS (2010) Mitochondrial reactive oxygen species regulate cellular signaling and dictate biological outcomes. Trends Biochem Sci 35(9):505–513
Hoppeler H, Vogt M (2001) Muscle tissue adaptations to hypoxia. J Exp Biol 204:3133–3139
Hornbein TF (2001) The high-altitude brain. J Exp Biol 204:3129–3132
Huang HC, Nguyen T, Pickett CB (2002) Phosphorylation of Nrf2 at Ser-40 by protein kinase C regulates antioxidant response element-mediated transcription. J Biol Chem 277:42769–42774
Huey RB, Eguskitza X (2001) Limits to human performance: elevated risks on high mountains. J Exp Biol 204:3115–3119
Hultgren H (1997) High altitude medicine. Hultgren Publications, Stanford
Innamorato NG, Rojo AI, Garcıa-Yague AJ, Yamamoto M, De Ceballos ML, Cuadrado A (2008) The transcription factor Nrf2 is a therapeutic target against brain inflammation. J Immunol 181:680–689
Irarrázaval S, Allard C, Campodónico J, Pérez D, Strobel P, Vásquez L, Urquiaga I, Echeverría G, Leighton F (2017) Oxidative stress in acute hypobaric hypoxia. High Alt Med Biol 18(2):128-134
Janocha AJ, Comhair SAA, Basnyat B, Neupane M, Gebremedhin A, Khan A, Ricci KS, Zhang R, Erzurum SC, Beall CM (2017) Antioxidant defense and oxidative damage vary widely among high- altitude residents. Am J Hum Biol 29(6):1–10
Jefferson JA, Simoni J, Escudero E, Hurtado ME, Swenson ER, Wesson DE, Schreiner GF, Schoene RB, Johnson RJ, Hurtado A (2004) Increased oxidative stress following acute and chronic high altitude exposure. High Alt Med Biol 5:61–69
Jiang C, Cui J, Liu F, Gao L, Luo Y, Li P, Guan L, Gao Y (2014) Mitochondrial DNA 10609t promotes hypoxia-induced increase of intracellular ROS and is a risk factor of high altitude polycythemia. PLoS One 9:e87775
Joanny P, Steinberg J, Robach P, Richalet JP, Gortan C, Gradette B, Jammes Y (2001) Operation Everest III (Comex’97): the effect of simulated severe hypobaric hypoxia on blood lipid peroxidation and antioxidant defence systems in human blood at rest and after maximal exercise. Resuscitation 49:307–314
Kappus H (1985) Lipid peroxidation mechanism, analysis, enzymology and biological relevance. In: Sies H (ed) Oxidative stress. Academic Press, London, pp 273–310
Kensler TW, Wakabayashi N, Biswal S (2007) Cell survival responses to environmental stresses via the Keap1-Nrf2-ARE pathway. Annu Rev Pharmacol Toxicol 47:89–116
Kietzmann T, Görlach A (2005) Reactive oxygen species in the control of hypoxia inducible factor-mediated gene expression. Semin Cell Dev Biol 16:474–486
Koivisto AE, Olsen T, Paur I, Paulsen G, Bastani NE, Garthe I, Raastad T, Matthews J, Blomhoff R, Bøhn SK (2019) Effects of antioxidant-rich foods on altitude-induced oxidative stress and inflammation in elite endurance athletes: a randomized controlled trial. PLoS One 14(6):e0217895. https://doi.org/10.1371/journal.pone.0217895
Kovac S, Angelova PR, Holmstrom KM, Zhang Y, Dinkova-Kostova AT, Abramov AY (2015) Nrf2 regulates ROS production by mitochondria and NADPH oxidase. Biochim Biophys Acta 1850:794–801
Kumar J, Khan S, Mandotra SK, Dhar P, Tayade AB, Verma S et al (2019) Nutraceutical profile and evidence of alleviation of oxidative stress by Spirogyra porticalis (Muell.) Cleve inhabiting the high altitude Trans-Himalayan Region. Sci Rep 9:4091. https://doi.org/10.1038/s41598-018-35595-x
Kunwar A, Priyadarsini KI (2011) Free radicals, oxidative stress and importance of antioxidants in human health. J Med Allied Sci 1:53–60
Lance S, Piermattei TD, Shibao GN, McManaman JL, Wright RM (1997) Hypoxia regulates xanthine dehydrogenase activity at pre- and posttranslational levels. Arch Biochem Biophy 348:163–168
Lanzillo JJ, Yu FS, Stevens J, Hassoun PM (1996) Determination of xanthine dehydrogenase mRNA by a reverse transcription-coupled competitive quantitative polymerase chain reaction assay: regulation in rat endothelial cells by hypoxia and hyperoxia. Arch Biochem Biophy 335:377–380
Lee JM, Shih AY, Murphy TH, Johnson JA (2003) NF-E2-related factor-2 mediates neuroprotection against mitochondrial complex I inhibitors and increased concentrations of intracellular calcium in primary cortical neurons. J Biol Chem 278:37948–37956
Lemoine AJ, Revollo S, Villalpando G, Valverde I, Gonzales M, Laouafa S, Soliz J, Joseph V (2018) Divergent mitochondrial antioxidant activities and lung alveolar architecture in the lungs of rats and mice at high altitude. Front Physiol 9:311
Lewis DFV (2002) Oxidative stress: the role of cytochromes P450 in oxygen activation. J Chem Technol Biotechnol 77:1095–1100
Lin SJ, Guarente L (2003) Nicotinamide adenine dinucleotide, a metabolic regulator of transcription, longevity and disease. Curr Opin Cell Biol 15:241–246
Liu JQ, Zelko IN, Erbynn EM, Sham JSK, Folz RJ (2006) Hypoxic pulmonary hypertension: role of superoxide and NADPH oxidase (gp91phox). Am J Phys 290:L2–L10
Lochhead JJ, Ronaldson PT, Davis TP (2017) Hypoxic stress and inflammatory pain disrupt blood-brain barrier tight junctions: implications for drug delivery to the central nervous system. AAPS J 19(4):910–920
Magalhaes J, Ascensao A, Viscor G, Soares J, Oliveira J, Marques F, Duarte J (2004) Oxidative stress in humans during and after 4 hours of hypoxia at a simulated altitude of 5500 m. Aviat Space Environ Med 75:16–22
Magalhães J, Ascensão A, Marques F, Soares JM, Ferreira R, Neuparth MJ, Duarte JA (2005) Effect of a high-altitude expedition to a Himalayan peak (Pumori, 7,161 m) on plasma and erythrocyte antioxidant profile. Eur J Appl Physiol 93:726–732
Malec V, Gottschald OR, Li S, Rose F, Seeger W, Hänze J (2010) HIF1 alpha signaling is augmented during intermittent hypoxia by induction of the Nrf2 pathway in NOX1-expressing adenocarcinoma A549 cells. Free Radic Biol Med 48:1626–1635
Martindale JL, Holbrook NJ (2002) Cellular response to oxidative stress: signaling for suicide and survival. J Cell Physiol 192:1–15
Masella R, Di Benedetto R, Vari R, Filesi C, Giovannini C (2005) Novel mechanisms of natural antioxidant compounds in biological systems: involvement of glutathione and glutathione-related enzymes. J Nutr Biochem 16:577–586
Mohanraj P, Merola AJ, Wright VP, Clanton TL (1998) Antioxidants protect rat diaphragmatic muscle function under hypoxic conditions. J Appl Physiol 84:1960–1966
Moller P, Loft S, Lundby C, Olsen NV (2001) Acute hypoxia and hypoxic exercise induce DNA strand breaks and oxidative DNA damage in humans. FASEB J 15:1181–1186
Muller FL, Liu Y, VanRemmen H (2004) Complex III releases superoxide to both sides of the inner mitochondrial membrane. J Biol Chem 279:49064–49073
Murray AJ (2009) Metabolic adaptation of skeletal muscle to high altitude hypoxia: how new technologies could resolve the controversies. Genome Med 1:117
Neubauer J (2001) Invited review: physiological and pathological responses to intermittent hypoxia. Am J Phys 90:1593–1599
Oh YS, Jun HS (2017) Effects of glucagon-like peptide-1 on oxidative stress and Nrf2 signaling. Int J Mol Sci 19:E26
OHagan KA, Cocchiglia S, Zhdanov AV, Tambuwala MM, Cummins EP, Monfared M, Agbor TA, Garvey JF, Papkovsky DB, Taylor CT, Allan BB (2009) PGC-1alpha is coupled to HIF-1alpha-dependent gene expression by increasing mitochondrial oxygen consumption in skeletal muscle cells. Proc Natl Acad Sci 106:2188–2193
Paddenberg R, Ishaq B, Goldenberg A, Faulhammer P, Rose F, Weissmann N, Braun-Dullaeus RC, Kummer W (2003) Essential role of complex II of the respiratory chain in hypoxia-induced ROS generation in the pulmonary vasculature. Am J Physiol Lung Cell Mol Physiol 284:L710–L719
Parraguez VH, Atlagich M, Araneda O, García C, Muñoz A, De Los Reyes M, Urquieta B (2011) Effects of antioxidant vitamins on newborn and placental traits in gestations at high altitude: comparative study in high and low altitude native sheep. Reprod Fertil Dev 23:285–296
Patir H, Sarada SKS, Singh S, Mathew T, Singh B, Bansal A (2012) Quercetin as a prophylactic measure against high altitude cerebral edema. Free Radic Biol Med 53:659–668
Patterson C, Nageswara NR, Runge MS (2000) The oxidative paradox: another piece in the puzzle. Circ Res 87:1074–1076
Pfeiffer JM, Askew EW, Roberts DE, Wood SM, Benson JE, Johnson SC, Freedman MS (1999) Effect of antioxidant supplementation on urine and blood markers of oxidative stress during extended moderate-altitude training. Wilderness Environ Med 10:66–74
Pialoux V, Mounier R, Brown AD, Steinback CD, Rawling JM, Poulin MJ (2009) Relationship between oxidative stress and HIF-1 alpha mRNA during sustained hypoxia in humans. Free Radic Biol Med 46:321–326
Piantadosi CA, Carraway MS, Babiker A, Suliman HB (2008) Heme oxygenase-1 regulates cardiac mitochondrial biogenesis via Nrf2-mediated transcriptional control of nuclear respiratory factor-1. Circ Res 103:1232–1240
Poljsak B, Suput D, Milisav I (2013) Achieving the balance between ROS and antioxidants: when to use the synthetic antioxidants. Oxidative Med Cell Longev 2013:1–11. https://doi.org/10.1155/2013/956792
Poss WB, Huecksteadt TP, Panus PC, Freeman BA, Hoidal JR (1996) Regulation of xanthine dehydrogenase and xanthine oxidase activity by hypoxia. Am J Phys 270:L941–L946
Poyton RO, Ball KA, Castello PR (2009) Mitochondrial generation of free radicals and hypoxic signalling. Trends Endocrinol Metabol 20:332–340
Radak Z, Zhao Z, Koltai E, Ohno H, Atalay M (2013) Oxygen consumption and usage during physical exercise: the balance between oxidative stress and ROS-dependent adaptive signaling. Antioxid Redox Signal 18:1208–1246
Ramazan MS, Ekeroglu SH, Dulger H, Algun E (2000) The effect of dietary treatment on erythrocyte lipid peroxidation, superoxide dismutase, glutathione peroxidase, and serum lipid peroxidation in patients with type 2 diabetes mellitus. Clin Biochem 33:669–674
Richter C, Park JW, Ames BN (1988) Normal oxidative damage to mitochondrial and nuclear DNA is extensive. Proc Natl Acad Sci 85:6465–6467
Richter C, Gogvadze V, Laffranchi R, Schlapbach R, Schweizer M, Suter M, Walter P, Yaffee M (1995) Oxidants in mitochondria: from physiology to diseases. Biochim Biophys Acta 1271:67–74
Roach RC, Hackett PH (2001) Frontiers of hypoxia research: acute mountain sickness. J Exp Biol 204:3161–3170
Roach RC, Maes D, Sandoval D, Robergs RA, Icenogle M, Hinghofer-Szalky HH, Lium D, Loeppky JA (2000) Exercise exacerbates acute mountain sickness at simulated high altitude. J Appl Physiol 88:581–585
Rosen H, Klebanoff SJ, Wang Y, Brot N, Heinecke JW, Fu X (2009) Methionine oxidation contributes to bacterial killing by the myeloperoxidase system of neutrophils. Proc Natl Acad Sci 106:18686–18691
Rushmore TH, Morton MR, Pickett CB (1991) The antioxidant responsive element: activation by oxidative stress and identification of the DNA consensus sequence required for functional activity. J Biol Chem 266:11632–11639
Sarada SKS, Dipti P, Anju B, Pauline T, Kain AK, Sairam M, Sharma SK, Ilavazhagan G, Kumar D, Selvamurthy W (2002) Antioxidant effect of beta-carotene on hypoxia induced oxidative stress in male albino rats. J Ethnopharmacol 79:149–153
Satoh T, Okamoto SI, Cui J, Watanabe Y, Furuta K, Suzuki M, Tohyama K, Lipton SA (2006) Activation of the Keap1/Nrf2 pathway for neuroprotection by electrophilic phase II inducers. Proc Natl Acad Sci 103:768–773
Schieber M, Chandel NS (2014) ROS function in redox signalling and review oxidative stress. Curr Biol 24:R453–R462
Schmidt MC, Askew EW, Roberts DE, Prior RL, Ensign WY Jr, Hesslink RE (2002) Oxidative stress in humans training in a cold, moderate altitude environment and their response to a phytochemical antioxidant supplement. Wilderness Environ Med 13:94–105
Schoene RB (2001) Limits of human lung function at high altitude. J Exp Biol 204:3121–3127
Schofield CJ, Ratcliffe PJ (2005) Signalling hypoxia by HIF hydroxylases. Biochem Biophys Res Commun 338:617–626
Sethy NK, Singh M, Kumar R, Ilavazhagan G, Bhargava K (2011) Upregulation of transcription factor NRF2-mediated oxidative stress response pathway in rat brain under short-term chronic hypobaric hypoxia. Funct Integr Genomics 11:119–137
Shinde A, Ganu J, Naik P (2012) Effect of free radicals & antioxidants on oxidative stress: a review. J Dent Allied Sci 1:63–66
Shrivastava K, Shukla D, Bansal A, Sairam M, Banerjee PK, Ilavazhagan G (2008) Neuroprotective effect of cobalt chloride on hypobaric hypoxia-induced oxidative stress. Neurochem Int 52:368–375
Sies H (1985) Oxidative stress: introductory remarks. In: Sies H (ed) Oxidative stress. Academic Press, London, pp 1–8
Sies H (1986) Biochemistry of oxidative stress. Angew Chem Int Ed Engl 25:1058–1071
Sies H (1997) Oxidative stress: oxidants and antioxidants. Exp Physiol 82:291–295
Simon-Schnass I (1994) Risk of oxidative stress during exercise at high altitude. In: Sen CK, Packer L, Hanninen O (eds) Exercise and oxygen toxicity. Elsevier, Amsterdam, pp 191–210
Sinha S, Ray US, Tomar OS, Singh SN (2009a) Different adaptation patterns of antioxidant system in natives and sojourners at high altitude. Respir Physiol Neurobiol 167:255–260
Sinha S, Nath S, Singh, Ray US (2009b) Total Antioxidant Status at High Altitude in Lowlanders and Native Highlanders: Role of Uric Acid. High Altitude Medicine & Biology 10 (3):269-274
Song TT, Bi YH, Gao YQ, Huang R, Hao K, Xu G, Tang JW, Ma ZQ, Kong FP, Coote JH, Chen XQ, Du JZ (2016) Systemic pro-inflammatory response facilitates the development of cerebral edema during short hypoxia. J Neuroinflammation 13(1):63
Stellingwerff T, Peeling P, Garvican-Lewis LA, Hall R, Koivisto AE, Heikura IA, Burke LM (2019) Nutrition and altitude: strategies to enhance adaptation, improve performance and maintain health: a narrative review. Sports Med 49(2):169–184
Strapazzon G, Malacrida S, Vezzoli A, Dal Cappello T, Falla M, Lochner P, Moretti S, Procter E, Brugger H, Mrakic-Sposta S (2016) Oxidative stress response to acute hypobaric hypoxia and its association with indirect measurement of increased intracranial pressure: a field study. Sci Rep 6:32426. https://doi.org/10.1038/srep32426
Strom J, Xu B, Tian X, Chen QM, Strom J, Xu B, Tian X, Chen QM (2016) Nrf2 protects mitochondrial decay by oxidative stress. FASEB J 30:66–80
Subudhi AW, Jacobs KA, Hagobian TA, Fattor JA, Muza SR, Fulco CS, Cymerman A, Friedlander AL (2006) Changes in ventilatory threshold at high altitude: effect of antioxidants. Med Sci Sports Exerc 38:1425–1431
Teradat LS, Guidot DM, Leff JA, Willingham IR, Hanley ME, Piermattei D, Repine JE (1992) Hypoxia injures endothelial cells by increasing endogenous xanthine oxidase activity. Proc Natl Acad Sci 89:3362–3366
Vani R, Reddy CS, Asha Devi S (2010) Oxidative stress in erythrocytes: a study on the effect of antioxidant mixtures during intermittent exposures to high altitude. Int J Biometeorol 54:553–562
Vats P, Singh VK, Singh SN, Singh SB (2008) Glutathione metabolism under high-altitude stress and effect of antioxidant supplementation. Aviat Space Environ Med 79:1106–1111
Vij AG, Dutta R, Satija NK (2005) Acclimatization to oxidative stress at high altitude. High Alt Med Biol 6:301–310
Wozniak A, Drewa G, Chesy G, Rakowski A, Rozwodowska M, Olszewska D (2001) Effect of altitude training on the peroxidation and antioxidant enzymes in sportsmen. Med Sci Sports Exerc 33:1109–1113
Xu C, Qiao X, Zhao Y, Sun R, Shang X, Niu W (2016) Resveratrol ameliorates chronic high altitude exposure-induced oxidative stress and suppresses lipid metabolism alteration in rats. Eur J Lipid Sci Technol 118:612–621
Yu L, Cao X, Tao W, Li M, Chen L (2020) Antioxidant activity and potential ameliorating effective ingredients for high altitude-induced fatigue from Gansu Maxianhao (Pedicularis Kansuensis Maxim.). J Tradit Chin Med 40(1):83–93
Zhang DX, Gutterman DD (2006) Mitochondrial reactive oxygen species-mediated signaling in endothelial cells. Am J Physiol Heart Circ Physiol 292:H2023–H2031
Zhang SXL, Wang Y, Gozal D (2012) Pathological consequences of intermittent hypoxia in the central nervous system. Compr Physiol 2:1767–1777
Zhong L, D’Urso A, Toiber D, Sebastian C, Henry RE, Vadysirisack DD, Guimaraes A, Marinelli B, Wikstrom JD, Nir T, Clish CB, Vaitheesvaran B, Iliopoulos O, Kurland I, Dor Y, Weissleder R, Shirihai OS, Ellisen LW, Espinosa JM, Mostoslavsky R (2010) The histone deacetylase Sirt6 regulates glucose homeostasis via Hif1alpha. Cell 140:280–293
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Gaur, P., Prasad, S., Kumar, B. et al. High-altitude hypoxia induced reactive oxygen species generation, signaling, and mitigation approaches. Int J Biometeorol 65, 601–615 (2021). https://doi.org/10.1007/s00484-020-02037-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00484-020-02037-1