Abstract
Heatwaves can be a common occurrence in Australia, and the public health impacts can be severe. Heat warnings and interventions are being adopted widely to reduce the preventable health impacts. This study examines the effects of heatwaves on morbidity and mortality in different climatic regions in the state of South Australia, to inform the targeting of heat warnings according to regional needs. Heatwaves were defined using the excess heat factor (EHF), an index based on mean daily temperature indices that quantifies heatwave severity relative to the local climate. In all regions, there were increases in morbidity (daily rates of ambulance call-outs and heat-related emergency presentations and hospital admissions) on heatwave days compared to non-heatwave days, which increased with heatwave severity. This study demonstrates that a consistent measure for heatwave severity, based on EHF, can be used to underpin public health warnings for climatically diverse areas.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over recent decades, there have been thousands of excess deaths attributed to heatwave disasters worldwide, most notably in India (Azhar et al. 2014), Europe (Robine et al. 2008), Russia (Shaposhnikov et al. 2014) and Chicago (Semenza et al. 1996). Heatwave conditions can lead to a range of heat-related illnesses, such as dehydration and heat stroke, and can also exacerbate common chronic diseases (Kenny et al. 2010). Although relatively common in much of Australia, the impacts of heatwaves can still be severe. In 2009, over 400 excess deaths were attributed to an unprecedented event affecting the south-eastern states (Victorian Chief Health Officer 2009; State Coroner 2010; Langlois et al. 2013).
Heat-related morbidity and mortality is associated with a range of physiological, behavioural and social risk factors, with the potential for interactive effects (Kovats and Hajat 2008; World Meteorological Organisation and World Health Organisation 2015; Zhang et al. 2016a, 2016b). For example, thermoregulation can be impaired due to age, illness or the physiological effects of certain medications (Kenny et al. 2010). Adopting appropriate behavioural responses can be challenging for those with declining cognitive function, impaired mobility or the frail elderly (Kenny et al. 2010). Other groups who may have limited ability to reduce their heat exposure include outdoor workers, tourists, disadvantaged or homeless populations (Faunt et al. 1995; Kjellstrom et al. 2009; Harlan et al. 2013). Notwithstanding the diversity of these risk factors, most heat-related illness is preventable (World Meteorological Organisation and World Health Organisation 2015), and heatwave warning systems (HWS) and interventions can be effective in moderating the adverse effects (Ebi et al. 2004; Bassil and Cole 2010; Toloo et al. 2013).
In relation to public health measures, it is also important to understand geographic variations in heat effects, so that warnings and interventions can be targeted appropriately. The level of acclimatisation is a significant factor, and this is particularly relevant in the large and climatically diverse states in Australia, where distinct regional variations in heat impacts have been reported (Loughnan et al. 2010; Jegasothy et al. 2017; Xiao et al. 2017). In general, heatwave impacts are expected to be more severe in metropolitan areas, where the built environment retains more heat (the urban heat island effect) (McGeehin and Mirabelli 2001). However, it has been argued that the socio-demographic and occupational characteristics in regional populations can present alternate risks (Williams et al. 2013; Kovach et al. 2015). For example, regional populations are often older, with lower average incomes, and a lower health status than metropolitan counterparts (National Rural Health Alliance 2010). A higher participation in outdoor work, particularly regional agriculture and mining industries, can result in higher exposure. Variation in regional housing, and in access to health services, may also influence how heatwaves affect different regional populations. There is now growing evidence of significant heat impacts in regional populations from diverse locations (Sheridan and Dolney 2003; Wu et al. 2011; Hattis et al. 2012; Henderson et al. 2013; Lippmann et al. 2013; Kovach et al. 2015).
The purpose of this study was to examine the effects of heatwaves on morbidity and mortality across South Australia (SA), a state with a population of 1.6 million and characterised by dry, warm-to-hot summers. Climatic diversity means the populations in the North and inland regions of the state experience higher average temperatures than those in the coastal areas and lower South East (Griffin and McCaskill 1986). Over the last two decades, the annual mean temperature anomaly for SA has shown a strong upwards trend, reaching a peak of 1.5 °C above the 1961–1990 average in 2013 (Australian Government Bureau of Meteorology 2015). Previous extreme heat events have had significant health impacts in SA, most notably during the 2009 heatwave (Nitschke et al. 2011). A HWS for SA was developed following the 2009 heatwave (Akompab et al. 2013), and a recent study suggests that these measures have been effective in reducing heat attributable morbidity in the state capital, Adelaide (Nitschke et al. 2016). However, one quarter of the SA population resides outside the metropolitan area, in climatically diverse regional areas where the effects of heatwaves have not been closely studied.
In this study, heatwaves have been defined using the excess heat factor (EHF) index (Nairn et al. 2009; Nairn and Fawcett 2015), which quantifies heatwave intensity relative to the local climate. The EHF index has been shown to be associated with excess mortality or morbidity in different locations (Langlois et al. 2013; Scalley et al. 2015; Hatvani-Kovacs et al. 2016; Jegasothy et al. 2017; Xiao et al. 2017), and is recognised by the World Health and World Meteorological Organisations (WMO and WHO 2015). The calculation of the EHF relates 3-day mean daily temperatures for a particular location to both the 95th percentile of long-term average temperatures, and the recent (prior 30-day) temperatures, and the estimate is normalised to generate an index of heatwave severity (Nairn and Fawcett 2015). The incorporation of historical and acclimatisation factors within the EHF severity index makes it useful to identify extreme or unusual heat which is likely to be hazardous to population health. Using the EHF severity index to define heatwaves of increasing severity, we have examined the effects of heatwaves in different regions of SA, to inform the development of heat warnings and interventions for the state.
Methods
Study setting
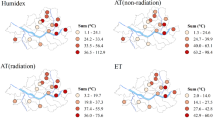
The state of South Australia occupies an area of 984,377 km2 in southern, central Australia, with a Mediterranean climate in the south ranging to hot desert climate in the north. For the purpose of this study, we divided the state into six discrete regions, plus the Adelaide metropolitan area (Fig. 1). These regions were defined with reference to the 12 Australian Bureau of Meteorology (ABM) weather districts and represented areas with broadly similar climate (Australian Government Bureau of Meteorology 2017). Each region is comprised of aggregated postcode areas, and represents a total population of North (64,626), Murray Mallee (62,211), South East and Kangaroo Island (KI) (75,530), Adelaide Hills (112,866), Yorke and Lower Eyre (56,443), and Mid North (59,912). The population of the Adelaide metropolitan area was 1,254,116. The state has a very low population density outside of the metropolitan area, particularly in the northern regions. Approximate population densities (people per square km) for the regions are North (less than 0.1), Murray Mallee (0.1–1.0), South East and KI (1.0–10.0), Adelaide Hills (1.0–10.0), Yorke and Lower Eyre (0.1–10.0), and Mid North (1.0–10.0) (Australian Bureau of Statistics 2016). These populations are largely concentrated within regional centres.
Meteorological data
Meteorological data were provided by the ABM, and included daily indices datasets for the period 2000–2016. For each region, we selected a regional population centre to act as a representative site (latitude and longitude) for extraction of meteorological data (Fig. 1). A second representative site was selected for each region to allow for a sensitivity analysis. Daily mean (average of maximum and minimum) temperatures were acquired using the ABM low-resolution (0.25° × 0.25°, approximately 25 km × 20 km) operational daily temperature analyses (Jones et al. 2009). The EHF intensity and normalised EHF severity metrics were normalised from the temperature data as described by Nairn and Fawcett (2015). The severity levels of events are derived from the ratio of EHF to the historical 85th percentiles of values of all positive EHF at each specific location. The ABM defines a low-severity event occurring when the value of this ratio lies between 0 and 1. In this study, we defined two further severity levels as ‘moderate’ (1 ≤ EHF severity < 2) and ‘high’ (EHF severity ≥ 2). The ABM categorises an extreme heatwave when EHF severity is three times the historical 85th percentile EHF intensity value and greater (EHF severity ≥ 3). However, as there were very few days meeting this criterion within the study period, we chose to combine these days into the high severity category. Non-heatwave days were those with EHF severity ≤ 0.
Health outcome data
Health outcome data included all-cause daily mortality, ambulance call-outs, emergency hospitalisations and emergency department presentations (ED). A direct heat-related hospitalisation and ED category was also extracted, using the ICD-10 codes: T67 (effects of heat and light), E86 (volume depletion) and X30 (exposure to excessive heat). Daily hospital and ambulance call-out data were sourced from the South Australian Department for Health and Wellbeing (SA Health). Hospitalisations were for the period 1 July 2000–30 April 2016, ambulance call-outs for 1 January 2000–31 December 2015, and ED data were from 1 July 2003–30 April 2016. Mortality data (1 January 2000–30 April 2016) were sourced from the SA Registry of Births, Deaths and Marriages. Estimated residential population data were from the ABS. Patient postcodes were used to aggregate and map outcomes to regions.
Statistical analysis
Analysis was undertaken for days within the warmer months, 1 October through 31 March. Poisson regression models were used to estimate the effect of heatwaves of varying severity (low, moderate, high) on specific health outcomes in each region. Negative binomial or zero-inflated Poisson models were used to address issues of over-dispersion or zero counts, where appropriate. Incidence rate ratios (IRRs) and 95% confidence intervals (CI) are reported for heatwave days compared to all non-heatwave days during the same warm season. The EHF is an accumulative index using 3-day mean daily temperatures, and we used a 3-day cumulative count for each health outcome to correspond with the 3-day EHF calculation period. We also analysed 5 and 7-day cumulative outcomes, to capture delayed effects, and these results are shown in Appendix 1. All models were adjusted for year, month, and day of the week, to account for long- and short-term temporal trends. The annual estimated resident population for each region was used as the offset variable to model rates. Population by post code (ABS data) was aggregated to estimate the regional population, with 2014 estimates used for the period 2014–2016. All analyses were conducted using Stata 13 (StataCorp., College Station, TX).
Results
The number of days at each level of heatwave severity and the corresponding average daily maximum temperatures for each region are shown in Table 1. The average maximum temperatures during high severity heatwave days were highest in the North, Murray Mallee and Mid North regions, consistent with the warmer climates in these regions. The mean daily health outcomes by region are shown in Table 2. These descriptive measures are indicative of the total populations in the regional and metropolitan areas.
The analyses of ambulance call-outs in relation to heatwave exposure indicated significant increases during low-severity heatwave days, and across the EHF severity scale, for most regions (Table 3). The highest increase in call-outs was evident for the Mid North region and on high severity heatwave days (35%; CI 24–47%).
The results of analyses of daily all-cause and heat-related hospital admissions are shown in Table 4. There was an increase in all-cause admissions on low-severity heatwave days in all regions, and also at higher severity levels in most regions. The highest increase (18%) was evident for the Mid North region on high severity heatwave days (IRR 1.18; CI 1.11–1.25%). Heat-related admissions increased over 2-fold in all regions on heatwave days, and up to 8.6-fold (IRR 8.57; CI 7.72–9.51) in the Adelaide metropolitan area on high severity days. There was a consistent increase apparent across the heatwave severity scale for heat-related admissions.
All-cause ED presentations showed small increases in most regions during low-severity heatwaves, but, in contrast to the Adelaide metropolitan area, the increase was not consistent at increasing heatwave severity (Table 5). In two regions, there was a significant decrease in presentations during high severity heatwaves, which is difficult to reconcile with the findings for other health services. Heat-related EDs showed a more consistent increase across the EHF severity scale, increasing up to 9.1-fold (IRR 9.06; CI 8.37–9.81) in the Adelaide metropolitan area on high severity heatwave days.
There was a significant increase in mortality on heatwave days at each severity level for the Adelaide population, reaching an estimated 22% (CI 14–31%) increase at high severity (Table 6). This increase was also evident in the North region, with an estimated 50% (CI 18–91%) increase in mortality at highest severity. There was no consistent increase in mortality across the heatwave severity scale for other regions, and evidence of a protective effect of heatwaves in the Yorke and Lower Eyre region.
The effect estimates shown in Tables 3, 4, 5 and 6 were derived from models using 3-day cumulative health outcomes, aligned with the 3-day EHF calculation period, as described in “Methods” section. We also considered the possibility of delayed effects by analysing 5 and 7-day cumulative health outcomes (extending 2 or 4 days beyond the EHF calculation period, respectively), and these results are shown in Appendix 1 (Table 7). In the main, the results indicate that the health effects become apparent in the immediate 3-day heatwave period. In isolated cases there was an apparent increase in effects with longer delays after high severity heatwaves.
The aggregation of outcome data over large areas is likely to result in exposure misclassification, which could affect the estimated associations between heatwave severity and health outcomes. To address this issue, we repeated the analyses using an alternative site for representative meteorological data for each region, and the results are included as Appendix 2 (Tables 8, 9, 10, 11, 12). The alternative sites were chosen on the basis that they represented (i) an alternative population centre within the region, (ii) a site distant from the first site, or (iii) an inland rather than coastal site. In the main, we found that the effect estimates and associated confidence intervals were comparable when using meteorological data from the alternative sites, for all health outcomes and all regions. These results would lead to the same conclusions being drawn, thus providing validation of our results.
Discussion
This study has quantified the effects of heatwaves across diverse regional areas of South Australia, using the normalised EHF intensity index as an indicator of heatwave severity, and considering a range of morbidity and mortality outcomes. At the high severity level (EHF severity ≥ 2), we observed increased daily rates of ambulance call-outs, heat-related hospital admissions and heat-related emergency presentations, in all regions across the state. These findings suggest that, despite differing levels of acclimatisation, populations in all regions experience increased morbidity during periods of extreme or unusual heat. Furthermore, as the EHF severity index was a consistent predictor of morbidity, it appears to provide a suitable index for activating public health warnings and responses across the state.
For some outcomes, (mortality, all-cause hospital admissions and ED presentations), we observed increases on all heatwave days for the Adelaide population, but the effects were less consistent across regional areas. This may be due to limited power when analysing effects in smaller regional populations, combined with fewer days at higher severity levels, and using all-cause outcomes that are less sensitive indicators of heat impacts.
Our results are suggestive of some regional differences in heatwave impacts. The Mid North region showed the highest increases for ambulance call-outs and all-cause hospital admissions during heatwave days, while the North region showed the highest estimate for mortality, when compared with other areas. As noted above, these results must be interpreted with caution because of the limited population sizes in the regions. However, it is of interest to consider any regional characteristics that might explain these results. Regions in the Mid North and North of the state have notably lower socio-economic status than other regions in the state (Australian Bureau of Statistics 2008), and this can be associated with poorer health status, reduced access to air conditioning, and poorer quality of housing (Jones and Tonts 2003). It is highly plausible that these characteristics could lead to a higher risk profile within these populations in relation to severe heatwave exposure.
The range of available health services, and the ease of access to these services, must also be considered when comparing heatwave impacts across different regions. Better access to particular services in some regions, for example hospitals and ED departments, could result in higher levels of use during heatwaves. A study of the usage of services between regional and metropolitan populations in SA found that the self-reported frequency of use of a range of health services was broadly similar across remoteness categories. However, use of primary care services was higher among residents of highly accessible areas and public hospital use increased with increasing remoteness (Eckert et al. 2004). The higher level of all-cause hospital admissions during heatwaves for the Mid North region may be due, in part, to a relatively high access to hospital services in this region (L. Jones, personal communication). In contrast, the more remote North region has relatively low access to hospitals, and it is noteworthy that this region showed the highest increase in mortality during heatwaves. A more detailed investigation is warranted to validate these differences and to explore any specific regional risk factors.
The morbidity outcomes showing the highest increases during heatwaves were specific heat-related hospital admissions and ED presentations. Although the absolute numbers for these admissions are typically low (mean daily admissions of 1–3 in the Adelaide population), the large estimated increases (up to 9-fold at highest severity) could result in a high cumulative burden on services, particularly over the course of an extended heatwave. This would be particularly significant in the context of limited service capacity in regional areas. It is important to note, however, that there is potential for coding bias associated with heat exposure, and this may affect the results for specific heat-related outcomes.
Most states in Australia comprise distinct climatic regions, with varying levels of heat acclimatisation. Establishing the criteria for activating state HWS requires some understanding of these variations in heat susceptibility. This will enable more appropriate targeting of resources and maximise opportunities for prevention, while avoiding the public complacency and fatigue that can result from false positive warnings (Bassil and Cole 2010). The EHF severity index provides an alternative criteria for defining extreme or unusual heatwaves at different locations (Nairn and Fawcett 2015), and, on the basis of our findings, the index could be adopted in the HWS for SA. Over a threshold of EHF severity (≥ 2), the increases in morbidity observed in all regions suggest it would be appropriate to consider public health advisories. Furthermore, the frequency of events meeting this threshold was low (five events in Adelaide for the period 1990–2015) and would not be expected to result in public complacency or fatigue. Our findings for SA are broadly consistent with results from other studies relating the EHF severity index to morbidity or mortality outcomes. For the Adelaide metropolitan population, the EHF severity index has previously been shown to predict excess ambulance call-outs (Hatvani-Kovacs et al. 2016) and mortality (Langlois et al. 2013b). For the state of Western Australia, the EHF severity index was found to be a predictor of health service utilisation for both metropolitan and regional areas, with evidence of geographical variations in effects across the state (Scalley et al. 2015; Xiao et al. 2017). Health service utilisation was also increased on heatwave days (EHF severity > 1) in New South Wales, with some variation across rural, remote and urban areas, and for different outcome measures (Jegasothy et al. 2017). Regional variations in heat effects have also been reported in the relatively smaller state of Victoria, where different maximum temperature thresholds for heat effects have been identified in different regions (Loughnan et al. 2010).
Humidity is considered to be another important factor in heat stress, and how the EHF metric performs as an indicator of hazardous heatwaves in more humid locations is yet to be determined. Although humidity is not directly captured within the EHF metric, Nairn and Fawcett (2015) have argued that the close correlation of humidity with minimum temperature means it is implicitly represented within the EHF calculation.
One of the strengths of our study was the range of different morbidity outcomes examined. This allowed us to identify the most sensitive indicators of heat effects, and revealed some differences between metropolitan and regional populations. For example, while ED presentations are significantly increased during heatwaves in Adelaide, this was not observed in regional populations, which may be explained by differences in access or use of ED services. It is not clear why ED presentations do not increase in parallel with ambulance call-outs in regional areas, but it should be noted that not all call-outs will result in an ED admission. In terms of surveillance of heatwave impacts, it appears that ambulance call-outs would provide the most consistent indicator of emergency health service utilisation across all regions. A further strength of the study was the use of several different categories of heatwave severity, which provided a better indication of the effects in each region. This was possible because the EHF severity categories could be applied consistently across different climatic regions. It should be noted, however, that categorisation of heatwave exposure results in some loss of information, and the use of a continuous EHF severity variable would provide more analytic power.
When using the EHF metric, the exposure relates to a 3-day period, rather than for individual days. Our effect estimates represent overall effects for EHF-defined heat events, with the 3-day cumulative outcomes capturing immediate and short-term effects, while the 5 and 7-day cumulative totals account for delayed effects. A more detailed analysis of daily outcomes, including for lagged days, could provide more information about how the health effects are distributed during and after the 3-day periods. Our results indicate that the health effects can extend beyond the immediate 3-day heatwave period, consistent with findings from other studies (Scalley et al. 2015; Jegasothy et al. 2017; Xiao et al. 2017). Further research could also examine the impact of delayed effects on specific health services.
A particular limitation of our study was the potential for misclassification of exposure, arising because exposure data from a single site was assigned to populations across large regions. For this study, it was not feasible to conduct analyses at smaller scales because of the low population density in most areas of SA. To address this issue, we repeated the analyses using exposure data from a separate site in each region, which provided broad confirmation of the results. We conclude that our effect estimates are indicative of population effects across the broader regions, despite some within-region climatic variations.
It is likely that the relationships between heatwaves and morbidity and mortality will change as populations are exposed (and adapt) to increasing temperatures, and as public health warnings and interventions are more widely implemented. In this context, some ongoing spatial monitoring of heat effects will be important to ensure that warnings and interventions are being targeted for maximum effectiveness.
Conclusions
Morbidity was increased on heatwave days in all regions of South Australia, suggesting that public health warnings and interventions are warranted across the state. Some regional differences in heatwave impacts were evident and may indicate higher levels of susceptibility. The EHF severity index was a consistent predictor of specific morbidity outcomes across regional SA, and could provide uniform threshold criteria for regional heat warnings in the state. These warnings, together with specific interventions, will become more important as the frequency and intensity of heatwaves increases with climate change, and as existing adaptations are challenged.
References
Akompab DA, Bi P, Williams S, Saniotis A, Walker I, Augoustinos M (2013) Engaging stakeholders in an adaptation process: governance and institutional arrangements in heat-health policy development in Adelaide, Australia. Mitig Adapt Strategies Glob Chang 18:1001–1018
Australian Bureau of Statistics. (2008) ABS releases measures of socio-economic advantage and disadvantage. http://wwwabsgovau/AUSSTATS/abs@nsf/Previousproducts/2033055001Media%20Release22006?opendocument&tabname=Summary&prodno=2033055001&issue=2006&num=&view= Accessed 6 May 2013
Australian Bureau of Statistics (2016). Regional population growth, Australia, 2016 http://wwwabsgovau/ausstats/abs@nsf/Latestproducts/32180Main%20Features752016?opendocument&tabname=Summary&prodno=32180&issue=2016&num=&view= Accessed 5 February 2018
Australian Government Bureau of Meteorology (2017) South Australia forecast area map. http://www.bom.gov.au/sa/forecasts/map.shtml Accessed 2 May 2017
Australian Government Bureau of Meteorology. (2015) Climate change and variability. http://wwwbomgovau/climate/change/indexshtml#tabs=Tracker&tracker=timeseries&tQ[graph]=tmean&tQ[area]=sa&tQ[season]=0112&tQ[ave_yr]=10 Accessed 24 May 2017
Azhar GS, Mavalankar D, Nori-Sarma A, Rajiva A, Dutta P, Jaiswal A, Sheffield P, Knowlton K, Hess JJ, on behalf of the Ahmedabad HeatClimate Study Group (2014) Heat-related mortality in India: excess all-cause mortality associated with the 2010 Ahmedabad heat wave. PLoS One 9(3):e91831. https://doi.org/10.1371/journal.pone.0091831
Bassil KL, Cole DC (2010) Effectiveness of public health interventions in reducing morbidity and mortality during heat episodes: a structured review. Int J Environ Res Public Health 7(3):991–1001
Ebi KL, Teisberg TJ, Kalkstein LS, Robinson L, Weiher RF (2004) Heat watch/warning systems save lives: estimated costs and benefits for Philadelphia 1995-98. Bull Am Meteorol Soc 85:1067–1073
Eckert KA, Taylor AW, Wilkinson D (2004) Does health service utilisation vary by remoteness? South Australian population data and the accessibility and remoteness index of Australia. Aust N Z J Public Health 28(5):426–432
Faunt JD, Wilkinson TJ, Aplin P, Henschke P, Webb M, Penhall RK (1995) The effete in the heat: heat-related hospital presentations during a ten day heat wave. Aust NZ J Med 25(2):117–121
Griffin T, McCaskill M. (1986) Atlas of South Australia. http://wwwatlassagovau/resources/atlas-of-south-australia-1986/environment-resources/climate-and-weather Accessed 7 May 2013
Harlan SL, Declet-Barreto JH, Stefanov WL, Petitti DB (2013) Neighborhood effects on heat deaths: social and environmental predictors of vulnerability in Maricopa County, Arizona. Environ Health Perspect 121(2):197–204
Hattis D, Ogneva-Himmelberger Y, Ratick S (2012) The spatial variability of heat-related mortality in Massachusetts. Appl Geogr 33:45–52
Hatvani-Kovacs G, Belusko M, Pockett J, Boland J (2016) Can the excess heat factor indicate heatwave-related morbidity? A case study in Adelaide, South Australia. EcoHealth 13(1):100–110
Henderson SB, Wan V, Kosatsky T (2013) Differences in heat-related mortality across four ecological regions with diverse urban, rural, and remote populations in British Columbia. Canada, Health & Place. https://doi.org/10.1016/j.healthplace.2013.1004.1005
Jegasothy E, McGuire R, Nairn J, Fawcett R, Scalley B (2017) Extreme climatic conditions and health service utilisation across rural and metropolitan New South Wales. Int J Biometeorol 61:1359–1370. https://doi.org/10.1007/s00484-00017-01313-00485
Jones DA, Wang W, Fawcett R (2009) High-quality spatial climate data-sets for Australia. Aust Meteorol Ocean 58(4):233–248
Jones R, Tonts M (2003) Transition and diversity in rural housing provision: the case of Narrogin, Western Australia. Aust Geogr 34(1):47–59
Kenny GP, Yardley J, Brown C, Sigal RJ, Jay O (2010) Heat stress in older individuals and patients with common chronic diseases. CMAJ 182(10):1053–1060
Kjellstrom T, Holmer I, Lemke B (2009) Workplace heat stress, health and productivity—an increasing challenge for low and middle income countries during climate change. Glob Health Action 2:2047. https://doi.org/10.3402/gha.v210.2047
Kovach MM, Konrad CE, Fuhrmann CM (2015) Area-level risk factors for heat-related illness in rural and urban locations across North Carolina, USA. Appl Geogr 60:175–183
Kovats RS, Hajat S (2008) Heat stress and public health: a critical review. Annu Rev Public Health 29:41–55
Langlois N, Herbst J, Mason K, Nairn J, Byard RW (2013) Using the excess heat factor (EHF) to predict the risk of heat related deaths. J Forensic Legal Med 20(5):408–411
Lippmann SJ, Fuhrmann CM, Waller AE, Richardson DB (2013) Ambient temperature and emergency department visits for heat-related illness in North Carolina, 2007–2008. Environ Res 124:35–42. https://doi.org/10.1016/j.envres.2013.1003.1009i
Loughnan M, Nicholls N, Tapper N (2010) Mortality–temperature thresholds for ten major population centres in rural Victoria, Australia. Health & Place 16:1287–1290
McGeehin MA, Mirabelli MC (2001) The potential impacts of climate variability and change on temperature-related morbidity and mortality in the United States. Environ Health Perspect 109(Suppl 2):185–189
Nairn J, Fawcett R, Ray D (2009). Defining and predicting excessive heat events, a national system. Modelling and understanding high impact weather: extended abstracts of the third CAWCR Modelling workshop, Citeseer
Nairn JR, Fawcett RJ (2015) The excess heat factor: a metric for heatwave intensity and its use in classifying heatwave severity. Int J Environ Res Public Health 12(1):227–253
National Rural Health Alliance Inc. Fact Sheet 23: Measuring the metropolitan-rural inequity. 2010. Available online: http://nrha.ruralhealth.org.au/factsheets/?IntContId=14819&IntCatId=41 Accessed on: 5 February 2018
Nitschke M, Tucker G, Hansen A, Williams S, Zhang Y, Bi P (2016) Evaluation of a heat warning system in Adelaide, South Australia, using case-series analysis. BMJ Open 6(7):e012125. https://doi.org/10.1136/bmjopen-2016-012125
Nitschke M, Tucker GR, Hansen AL, Williams S, Zhang Y, Bi P (2011) Impact of two recent extreme heat episodes on morbidity and mortality in Adelaide, South Australia: a case-series analysis. Environ Health 10. https://doi.org/10.1186/1476-1069X-1110-1142
Robine J-M, Cheung SLK, Le Roy S, Van Oyen H, Griffiths C, Michel J-P, Herrmann FR (2008) Death toll exceeded 70,000 in Europe during the summer of 2003. C R Biologies 331:171–178. https://doi.org/10.1016/j.crvi.2007.12.001
Scalley BD, Spicer T, Jian L, Xiao J, Nairn J, Robertson A, Weeramanthri T (2015) Responding to heatwave intensity: excess heat factor is a superior predictor of health service utilisation and a trigger for heatwave plans. Aust N Z J Public Health 39:582–587. https://doi.org/10.1111/1753-6405.12421
Semenza JC, Rubin CH, Falter KH, Selanikio JD, Flanders WD, Howe HL, Wilhelm JL (1996) Heat-related deaths during the July 1995 heat wave in Chicago. N Engl J Med 335(2):84–90
Shaposhnikov D, Revich B, Bellander T, Bedada GB, Bottai M, Kharkova T, Kvasha E, Lezina E, Lind T, Semutnikova E, Pershagen G (2014) Mortality related to air pollution with the Moscow heat wave and wildfire of 2010. Epidemiology 25:359–364. https://doi.org/10.1097/EDE.0000000000000090
Sheridan SC, Dolney TJ (2003) Heat, mortality, and level of urbanization: measuring vulnerability across Ohio. USA Climate Res 24:255–265
State Coroner (2010) Annual report of the state coroner financial year 2009–2010. South Australia
Toloo G, FitzGerald G, Aitken P, Verrall K, Tong S (2013) Evaluating the effectiveness of heat warning systems: systematic review of epidemiological evidence. Int J Public Health 58(5):667–681
Victorian Chief Health Officer (2009). January 2009 Heatwave in Victoria: an assessment of health impacts Melbourne, Victorian Government Department of Human Services
Williams S, Bi P, Newbury J, Robinson G, Pisaniello D, Saniotis A, Hansen A (2013) Extreme heat and health: perspectives from health service providers in rural and remote communities in South Australia. Int J Environ Res Public Health 10(11):5565–5583
World Meteorological Organization and World Health Organization (2015). Heatwaves and health: guidance on warning-system development. WMO-No. 1142. G. R. McGregor
Wu P-C, Lin C-Y, Lung S-C, Guo H-R, Chou C-H, Su H-J (2011) Cardiovascular mortality during heat and cold events: determinants of regional vulnerability in Taiwan. Occup Environ Med 68(7):525–530
Xiao J, Spicer T, Jian L, Yun GY, Shao C, Nairn J, Fawcett RJB, Robertson A, Weeramanthri TS (2017) Variation in population vulnerability to heat wave in Western Australia. Front Public Health 5. https://doi.org/10.3389/fpubh.2017.00064
Zhang Y, Nitschke M, Krackowizer A, Dear K, Pisaniello D, Weinstein P, Tucker G, Shakib S, Bi P (2016a) Risk factors for deaths during the 2009 heat wave in Adelaide, Australia: a matched case-control study. Int J Biometeorol 61:35–47
Zhang Y, Nitschke M, Krackowizer A, Dear K, Pisaniello D, Weinstein P, Tucker G, Shakib S, Bi P (2016b) Risk factors of direct heat-related hospital admissions during the 2009 heatwave in Adelaide, Australia: a matched case-control study. BMJ Open 6(6):e010666. https://doi.org/10.1136/bmjopen-2015-010666
Acknowledgements and funding
The authors would like to acknowledge the contributions of Mr. Graeme Tucker to the design of this study.
This study was supported by the Attorney General’s Department of the Australian Government, under the National Emergency Management Projects Scheme [grant number NP1617-017].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval was obtained from the Human Research Ethics Committees of The University of Adelaide and SA Health.
Conflict of interest
The authors declare that they have no conflict of interest.
Appendices
Appendix 1
Appendix 2
Results from a sensitivity analysis using alternative regional sites for meteorological observations
Rights and permissions
About this article
Cite this article
Williams, S., Venugopal, K., Nitschke, M. et al. Regional morbidity and mortality during heatwaves in South Australia. Int J Biometeorol 62, 1911–1926 (2018). https://doi.org/10.1007/s00484-018-1593-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00484-018-1593-4