Abstract
Accumulating evidence demonstrates the significant influence of weather factors, especially temperature and humidity, on influenza seasonality. However, it is still unclear whether temperature variation within the same day, that is diurnal temperature range (DTR), is related to influenza seasonality. In addition, the different effects of weather factors on influenza seasonality across age groups have not been well documented in previous studies. Our study aims to explore the effects of DTR and humidity on influenza seasonality, and the differences in the association between weather factors and influenza seasonality among different age groups in Hong Kong, China. Generalized additive models were conducted to flexibly assess the impact of DTR, absolute humidity (vapor pressure, VP), and relative humidity on influenza seasonality in Hong Kong, China, from January 2012 to December 2016. Stratified analyses were performed to determine if the effects of weather factors differ across age groups (< 5, 5–9, 10–64, and > 64 years). The results suggested that DTR, absolute humidity, and relative humidity were significantly related to influenza seasonality in dry period (when VP is less than 20 mb), while no significant association was found in humid period (when VP is greater than 20 mb). The percentage changes of hospitalization rates due to influenza associated with per unit increase of weather factors in the very young children (age 0–4) and the elderly (age 65+) were higher than that in the adults (age 10–64). Diurnal temperature range is significantly associated with influenza seasonality in dry period, and the effects of weather factors differ across age groups in Hong Kong, China.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The annual influenza epidemic leads to increased mortality and hospital admissions, especially in high-risk populations (Thompson et al. 2003, 2004). It is estimated that influenza infection is related to 250,000 to 500,000 deaths around the world each year (World Health Organization 2009). Influenza epidemics typically occur every cold winter in temperature regions. However, influenza seasonality is more diverse, and multiple peaks tend to arise at various times within a year in the warm tropical and subtropical regions (Tamerius et al. 2013).
Previous studies have found that weather factors are closely correlated with the transmission and disease burden of influenza, and temperature and humidity are considered to be remarkably significant factors in the spread of influenza (Lowen et al. 2007; Tamerius et al. 2013). Cold and dry weather conditions were found to enhance the activity of influenza in guinea pig models (Lowen et al. 2007). Low-temperature can increase contact rates, suppress immunity, and facilitate the transmission of influenza disease (Tamerius et al. 2011). On the other hand, absolute humidity can constrain both transmission and survival of influenza viruses, and has been recognized as a better predictor than relative humidity (Shaman and Kohn 2009). In general, weather factors lead to a change of susceptibility to influenza infections indirectly by changing individual behavior and health status (Dowell 2001). In addition, diurnal temperature range (DTR) describes the variation between the maximal and minimal temperatures that occurs in the same day (Braganza et al. 2004). Although the influence of temperature has been well established, it is still unclear whether DTR is related to influenza seasonality.
The description and comparison of influenza incidence among different age groups have been widely conducted (Ruf and Knuf 2014; Simonsen 1998). Nevertheless, there are few studies on the different effects of weather factors on influenza across age groups (Huang et al. 2017). High-risk groups, including the very young children and the elderly, are vulnerable to influenza virus and tend to suffer from influenza-related complications (Ruf and Knuf 2014; World Health Organization 2009). Accordingly, it is essential to explore if the impact of meteorological factors on the occurrence of influenza varies across different age groups.
This study is designed to examine the impact of DTR, absolute humidity, and relative humidity on influenza seasonality in Hong Kong, a subtropical city in the Asian Pacific rim. The different effects of weather factors on various age groups were also explored in our study. We constructed a generalized additive model to flexibly assess the impact of DTR, absolute humidity, and relative humidity on influenza seasonality after controlling the confounding effects of other environmental factors and time trend.
Methods
Data source
The Hong Kong Centre for Health Protection conducted routine laboratory surveillance for influenza. Weekly respiratory samples in laboratory surveillance system were collected from patients with influenza like illness (defined as fever ≥ 38 °C and sore throat or cough) in general practitioners (GPs) and general out-patient clinics (GOPCs), and inpatients with acute respiratory diseases (Yang et al. 2008). With the development of the sentinel surveillance program for influenza in Hong Kong, 50 general practitioners and 64 general out-patient clinics selected throughout Hong Kong were included in the sentinel surveillance system. Weekly influenza-positive rate from laboratory confirmation was collected from the Center for Health Protection (http://www.chp.gov.hk/). The laboratory surveillance data indicates the activity of influenza viruses in the entire region of Hong Kong (Hong Kong Centre for Health Protection 2017). However, we have no access to weekly laboratory-confirmed influenza rates by age groups. Hospitalizations for influenza calculated from principal discharge diagnosis of influenza may be expected to be a minimum estimate of influenza disease but can inform policy-makers on influenza immunization in many settings (Beard et al. 2006). Hospitalization for influenza across various age groups is an alternative approach to estimate the activity of influenza among age groups. We obtained weekly rates in hospitals with a principal discharge diagnosis of influenza infection (ICD-9-CM 487) across four age groups (0–4, 5–9, 10–64, and 65+ years of age) from the Center for Health Protection. In cases of hospitalization, the discharge code ICD-9-CM 487 was used in the principle diagnosis at discharge to identify influenza-related hospitalization cases. All the hospitalized patients in our study were predominantly due to influenza infection.
Meteorological parameters including daily maximal, mean, and minimum temperature, relative humidity, wind speed, and rainfall were obtained from the Hong Kong observatory. The daily maximum temperature minus the daily minimum temperature was calculated as the DTR. The mean of each daily meteorological factor was aggregated over influenza surveillance weeks. Data on laboratory-confirmed influenza, hospitalizations for influenza, and meteorological parameters were available from 2012 to 2017.
According to previous research, vapor pressure could be used as the measure of absolute humidity in our study (Shaman and Kohn 2009). We used the following equations to calculate vapor pressure (e) from temperature (K) and relative humidity:
and
where es(T0) is the saturation vapor pressure = 6.11 mb at temperature T0 = 273.15 K, L is the latent heat of evaporation for water = 2.27 MJ/kg, RV is the gas constant for water vapor = 461.5 J/(kg/K), T is the temperature in K, and RH is the relative humidity (Tang et al. 2010).
Statistical analyses
We conducted descriptive statistical analyses to describe the summary statistics of weekly influenza-positive rate from laboratory confirmation (LAB%), weekly rates of hospitalizations for influenza (per 10,000 population), and meteorological data. The coefficients of Pearson correlation, tolerance, and variation inflation factors (VIF) among meteorological parameters were examined to determine the possible effects of collinearity.
First, we used a generalized additive regression model (GAM) to analyze the effects of DTR and humidity on influenza seasonality. The nonparametric smoothing functions were adopted in GAM to explore the association between response variable and independent variables. In this study, the weekly-confirmed rates of positive specimens of influenza in Hong Kong were considered as the response variable. The independent variables consisted of the weekly-averaged DTR, relative humidity (RH), vapor pressure (VP), rainfall, and wind speed (WS). Time trend and meteorological parameters, including wind speed and rainfall, were considered in all models as the adjustment for seasonal factors, unmeasured long-term time trend, and other meteorological parameters. The model used for analysis was
where t is the number of the week, μt is the expected rate of laboratory-confirmed influenza-positive specimens at week t, α0 is the model intercept, and s(x) denotes the penalized smoothing spline functions of weather factors and time trend. The confounding of seasonal factors and unmeasured long-term were adjusted by the smoothing function of time trend. The combination of degree of freedom for this model was applied to minimize the generalized cross validation scores. To explore the delayed effect of weather factors on influenza activity, we lagged meteorological parameters by i weeks. For single-week lag, a lag of zero week (i = 0, lag 0) corresponded to the current week weather factors, while a lag of 1 week (i = 1, lag 1) was corresponding to weather factors in previous week. For multiple-week average lag, the moving average lag (lag 01) was the 2-week moving average of the values of the current and previous weeks. We selected the lag time by the Akaike information criterion (AIC). Concurvity, the nonparametric analogue of multicollinearity, was assessed using GAM concurvity measures in our study (Ramsay et al. 2003).
Second, we plotted the exposure-response curve between laboratory-confirmed influenza and weather factors based on the above GAM with a selected lag time. If the association were linear or almost linear, weather effects were directly indicated as percentage change of laboratory-confirmed influenza infection rates per unit increase of weather factors. If the associations were non-linear, we chose a breakpoint and used a linear-threshold model to explore quantitatively the effect of weather factors (Liu et al. 2011; Zhang et al. 2014). The percentage changes of LAB% for per unit increase in weather factors below the threshold and per unit increase above the threshold were estimated to evaluate the effects of weather factors. The estimation of 95% confidence interval in our study was based on the assumption of asymptotic normality and a Bayesian approach for confidence interval calculation with good coverage probabilities (Wood and Wood 2007).
To examine the different impacts of weather factors on influenza hospitalization among various age groups, stratified analyses of four age groups (< 5, 5–9, 10–64, ≥ 65 years) were performed by the same procedure. All statistical analyses in this study were performed using the MGCV packages in software R (version 3.2.0.).
Data availability
The meteorological datasets are available from the Hong Kong Observatory (http://www.hko.gov.hk/wxinfo/pastwx/extract.htm), and the data on laboratory-confirmed influenza and hospitalizations for influenza across age groups are available from the Hong Kong Center for Health Protection (http://www.chp.gov.hk/).
Results
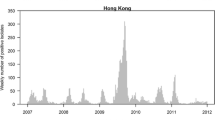
The descriptive statistics for the weekly percentages of laboratory-confirmed positive specimens of influenza (LAB%), rates of hospitalizations for influenza, and meteorological data are summarized in Table 1. The average rate of weekly influenza from the 1st of January 2012 to the 31st of December 2016 was 10.28%. The average rate of hospitalizations for influenza (per 10,000 population) in Hong Kong was 0.994 (range 0–6.710), 0.379 (range 0–2.550), 0.053 (range 0–0.260), and 0.560 (range 0–5.330) for the age groups 0–4, 5–9, 10–64, and 65+ years, respectively. The weekly time series of meteorology data and influenza surveillance data, including LAB% and hospitalizations for influenza by age groups over the 5-year period, are depicted in Fig. 1. Seasonal patterns of hospitalizations for influenza rates were similar among the four age groups with two peaks observed in summer and winter annually (Fig. 1). As shown in Table 2, the collinearity statistics in our study indicated that the Pearson’s correlation coefficients among weather factors ranged from − 0.028 to − 0.469, and the variance inflation factor (VIF) ranged between 1.367 and 2.058 (tolerance 0.486 to 0.732). A variance inflation factor above 10 (or, tolerance values less than 0.10) indicates high multicollinearity among independent variables and is thought to signal harmful collinearity (Marquaridt 1970), while a variance inflation factors of less than 10 (or, tolerance values above 0.10) is indicative of inconsequential collinearity (Hair et al. 1995). The collinearity analysis indicates that multicollinearity would not pose a serious threat in our study (O’brien 2007). The model with moving average of 2 weeks (lag 01) had the smallest AIC values (− 710.95) among all these models and yielded the best fit (Table 3). Therefore, the model with moving average of 2 weeks was used in the subsequent analyses. The estimated indices of concurvity among nonparametric smoothing terms ranged from 0.08 to 0.32, which is prone to support that the current degree of concurvity would not result in serious inflated variance of the estimate.
The exposure-response relationships for weather factors and influenza activity (Fig. 2) suggested that influenza infections had strong positive relationship with DTR and RH. The approximate linear association of DTR and RH with laboratory-confirmed influenza was obtained (Fig. 2). The estimated effect (slope) of VP on influenza activity sharply decreased as VP increased up until around 20 mb and then plateaued, which indicated the almost linear association between influenza risks and VP in the range of less than 20 mb. The exposure-response curves were shown as a similar linear-threshold pattern between weather factors and hospitalizations for influenza by different age groups (Fig. 3). In fact, Wang et al. estimated a U-shaped correlation between influenza activity and VP with through at around 20 mb in two subtropical regions of southern China (Wang et al. 2017). Such association between weather factors and influenza risk was partially consistent with previous studies (Shaman and Kohn 2009; Tamerius et al. 2013). Consequently, 20 mb was considered as a breakpoint (commonly called the “threshold”), and a linear-threshold model was conducted to explore quantitatively the effect of weather factors in vapor pressure above (humid period) or below (dry period) the threshold.
Exposure-response curves for the effects of meteorological factors on rates of hospitalizations for influenza across four age groups. The X-axis is the meteorological factors (moving average of 2 weeks). The solid lines state the mean estimates, and the dashed lines indicate the corresponding 95% CI
In dry period (when VP is less than 20 mb), positive correlations were observed between DTR, RH, and laboratory-confirmed influenza, while a negative correlation was observed between VP and influenza (Table 4). The impacts of DTR and humidity on hospitalizations for influenza by different age groups in the dry period were also detected (Table 5). DTR and relative humidity had positive effects on hospitalization for influenza across all age groups, except for the association between DTR and the elderly (65+ years). The increase in the weekly hospitalizations for influenza were 26.69% (95% CI 19.11 to 34.27), 11.52% (95% CI 7.93 to 15.11), 1.53% (95% CI 1.10 to 1.95), and 17.49% (95% CI 11.26 to 23.71) for per unit decrease in weekly VP for the 0–4, 5–9, 10–64, and 65+ years age groups, respectively. The corresponding average increases in the weekly rates of hospitalizations for influenza were 71.35% (95% CI 44.49 to 98.21), 22.61% (95% CI 9.80 to 35.42), 3.10% (95% CI 1.60 to 4.60), and 17.43% (95% CI − 4.85 to 39.70) for per unit increase in weekly DTR, and 11.63% (95% CI 7.71 to 15.55), 4.40% (95% CI 2.57 to 6.24), 0.66% (95% CI 0.44 to 0.88), and 6.46% (95% CI 3.31 to 9.62) for per unit increase in RH. However, the effect of DTR on hospitalizations for influenza at the elderly (age 65+) was not significant. Additionally, we found the impacts of weather factors on hospitalizations for influenza varied by age groups. The percentage changes of hospitalization rates due to influenza associated with per unit increase of weather factors in the very young children (age 0–4) and the elderly (age 65+) were higher than that in the adults (age 10–64).
In humid environmental surroundings (when VP is greater than 20 mb), the associations between weather factors and influenza infections were completely different from those in dry environments. Laboratory-confirmed influenza (Table 4) and hospitalizations for influenza across four age groups (Table 5) were not significantly related to weather factors except for VP, which was positively related to hospitalization for influenza in group of the elderly (age 65+).
Discussion
Our study found that diurnal temperature range and humidity had significant impacts on influenza infections in dry period. The association between weather variables, especially temperature and humidity, and seasonal influenza has been widely reported (Shaman and Kohn 2009; Wang et al. 2017). However, few studies have investigated the association between DTR and influenza seasonality. The GAM models suggested that DTR had positive impact on influenza infections in dry period, after adjusting for other meteorological factors, seasonal variability, and unmeasured long-term. It is biologically plausible because DTR can contribute to the spread of influenza and infections, though the underlying mechanism is unclear. Previous studies found that temperature change could increase cardiovascular workload and had negative effects on the health of human beings (Imai et al. 1998; Luurila 1980). Another study suggested that the temperature change of inhaled air could lead to the release of inflammatory mediators associated with mast cells (Togias et al. 1985). DTR may bring about pathophysiological responses of the respiratory epithelium, such as inflammatory changes and bronchospasms (Graudenz et al. 2006). All the adverse effects on human health caused by DTR may lower the resistance and enhance the susceptibility to airborne pathogens, which lead to an increased rate of influenza infections.
Influenza seasonality has been shown to be closely related with humidity (Tamerius et al. 2013). We found that the incidence of influenza infections increased with the relative humidity, which was consistent with previous studies in Hong Kong (Chan et al. 2009; Tang et al. 2010), Buenos Aires (Viegas et al. 2004), and Shanghai (Wang et al. 2017). In fact, influenza viruses tend to loss infectivity under low relative humidity due to unstable nature of their structures as enveloped viruses (Hambling 1964; Hammond et al. 1989; Rechsteiner and Winkler 1969). Aerosolized influenza virions remain relatively stable at a high relative humidity (60–80%) (Schaffer et al. 1976). The influenza activity may fluctuate in Hong Kong with relative humidity ranging from 59 to 93% (Chan et al. 2009). The correlation between temperature and VP indicates that low temperature can be more common in dry environment and is favorable for the spread and transmission of influenza. Furthermore, colder air is easier to be saturated with water vapor, and thus a high RH occurred (Tang et al. 2010). Consequently, relative humidity was sustained to have a positive relation with influenza infections. A recent study suggested that absolute humidity is a very important factor to explain the seasonality of influenza and correlates more closely with influenza seasonality than relative humidity. Experimental studies indicated the survival and transmission of influenza virus increased as the absolute humidity decreased (Shaman and Kohn 2009). The estimated effect of VP on influenza infection sharply decreased as VP increased up until around 20 mb and then plateaued in our study. Similar to our results, previous studies also demonstrated a negative correlation between influenza seasonality and VP within the range of 5 to 20 mb (Shaman and Kohn 2009; Wang et al. 2017). In all, absolute humidity is believed to constrain both transmission and survival of influenza virus significantly and reduce the spread of influenza within a certain range (McDevitt et al. 2010).
Accumulating evidence has demonstrated that temperature plays an important role in the transmission of influenza. However, we avoid building a model including both VP and temperature because of the collinearity problem between VP and temperature (Pearson correlation coefficient 0.95, P < 0.01). Alternatively, we can develop another model including the covariate temperature by replacing s(DTRt − i) and s(VPt − i) with s(Temperaturet − i) in model (1) and the conducted model selection. Akaike information criterion (AIC) was used to compare the fitness of models with various weather factors. The AIC values of these models clearly revealed that the models including the effect of diurnal temperature range (with minimum AIC values) provided a better fit to the data than the other models including the effect of temperature (see Supplementary Information, Table S1). Therefore, the model (1) including the effect of diurnal temperature range was mainly explored in our study.
Another novel contribution of this study is that we explored the impact of meteorological factors on influenza hospitalization by different age groups. Our results indicated that DTR, VP, and RH had the greatest effect on the young children (age 0–4), followed by the elderly (age 65+) and older children (age 5–9), and had relatively less effect on adults (age 10–64). The differences in the extent of impact among different age groups may be attributable to the differences of environment exposure, immunity, social behavior, and other related factors. The young children (age 0–4) are susceptible to influenza viruses for the reason that their lungs have little ability to fight off virus infections (Feng et al. 2016). Influenza virus infections are also important risk factors of the complications (Izurieta et al. 2000), which causes a massive number of influenza infections and hospitalizations in children. Children, especially infants, are greatly susceptible to influenza infection during the epidemic period (Neuzil et al. 2000). On the other hand, the elderly are susceptible to influenza infection despite being vaccinated due to the weakened immune system (Kang et al. 2004). Influenza infections are usually complicated by secondary virus or bacterial infection, and the elderly are especially vulnerable to complications caused by influenza infections (Fleming and Elliot 2005). Additionally, the elderly tend to require hospitalization because influenza infections usually cause serious diseases (Fleming et al. 2003; Mullooly et al. 1994). Those older children (age 5–9) attend school or day care, which would lead to crowding and increase the spread and infections of influenza (Huang et al. 2017). Compared to adults, older children tend to spend more time playing outdoors and have greater exposure to adverse meteorological factors. Therefore, children (aged 0–9 years) and the elderly group (aged > 64 years) have substantially higher hospitalization rates due to influenza than adults (aged 10–64 years). Our results support the current influenza immunization policies recommended by the Hong Kong government and WHO, which suggest that young children, the elderly, pregnant women, and those in clinical risk groups should be vaccinated (WHO 2012). Interestingly, the only exception in dry period was that DTR had no significant influence on hospitalization for influenza at the elderly (age 65+). The living and exercise habits of elderly people are different from the adults and children, and the outdoor DTR data in our study cannot completely represent the temperature differences that the elderly experienced. It is possible that indoor diurnal temperature range is more related to the influenza infection and hospitalization for the elderly than outdoor DTR data in practice. Therefore, the elderly may be less susceptible to the outdoor DTR. Future studies are in need to understand the associations between indoor environmental factors and influenza activities.
Not surprisingly, the association between weather factors and influenza seasonality in humid environmental surroundings is significantly different from those in dry environments. VP was positively related to hospitalization for influenza at the elderly (age 65+), but other weather factors had no significant effect on influenza seasonality and hospitalizations for influenza across four age groups. In hot days, air-conditioning is widely used in homes, shopping malls, and other indoor area where people live in high density in many subtropical/tropical countries. The effect of air-conditioning on influenza survival and transmission is still unclear. Air-conditioning can lower humidity, which makes environments more favorable for the survival and transmission of influenza virus. The enhancement of influenza survival and transmissibility increases the potential for influenza infections and other respiratory disease. On the contrary, virus-bearing aerosols can also be trapped by the condensation process within the unit itself. Because the indoor climate conditions are different from those of outdoor in summer in Hong Kong, current meteorological parameters in our study may be an imperfect indicator of personal exposure because they spend a majority of time indoors (Chan et al. 2009). The positive correlation between VP and hospitalizations for influenza at the elderly in humid surroundings may be because the elderly is greatly susceptible to influenza infection and VP is positively associated with precipitation. Precipitation induces social behavior and promotes contact transmission, which greatly contribute to the summer influenza peak in Hong Kong (Lowen et al. 2008; Soebiyanto et al. 2010).
In practice, wind could speed the air circulation and change the virus concentration in the air. Ambient temperatures, including mean, maximum, and minimum temperatures, are usually used to assess influenza seasonality. Additionally, wind could make people feel cold by drawing heat away from the exposed body and influence people’s perception of temperature (Lin et al. 2013; Siple and Passel 1999). Concentrations of air pollutants, which have significant impact on spread of influenza, are closely related with wind speed (Demirci and Cuhadaroglu 2000; Rigby and Toumi 2008). Therefore, wind speed was considered as confounding effects in our study to better examine the impact of meteorological factors on influenza seasonality.
We also conducted another model to explore whether there was an interaction effect between DTR and VP on influenza activity with dry and humid periods defined using the VP threshold of 20 mb. We found that there was no significant interaction effect of DTR and VP on influenza activity with dry and humid periods in our study (see Supplementary Information, Table S2). However, the underlying mechanism of the association between weather factors and influenza activity still needs to be further investigated.
To our knowledge, this is the first study which has found that DTR is statistically related to influenza activities in a subtropical city of China. An additional finding of our study is the different effects of environmental factors on influenza hospitalization across age groups. Weekly influenza-positive rate from laboratory confirmation and hospitalizations for influenza calculated from principal discharge diagnosis of influenza can be used to indicate the activity of influenza viruses and inform policy-makers on influenza immunization, though they reflect different degrees of severity of influenza infection (Beard et al. 2006; Hong Kong Centre for Health Protection 2017). Several weaknesses should be acknowledged. This is an ecological study, and the bias caused by exposure misclassification may be inevitable. Only one city was taken into consideration, and extensive studies are in need to verify the generalizability of our results to other regions. In addition, hospitalizations for influenza calculated from principal discharge diagnosis of influenza are expected to be a minimum estimate of influenza disease burden but cannot fully reflect the disease and social economic burden caused by influenza (Beard et al. 2006).
Conclusions
Our findings suggested that weather factors of DTR, VP, and RH played significant roles in the spread and transmission of influenza virus under dry condition. We focused on DTR, which rarely has been studied in previous studies on influenza, was found to have statistically significant effect on influenza infections, and could be important predictor of influenza. Furthermore, the effects of climatic conditions were significantly related to hospitalizations for influenza across all ages in dry period. On the contrast, influenza seasonality and hospitalizations for influenza across four age groups had no relation to weather factors in humid environment except for VP, which was positively related to hospitalizations for influenza at the elderly (age 65+). Our results provide an improved understanding of the associations between weather factors and influenza activities within different age groups. These findings are of great importance to provide evidences for precise vaccination strategies and public health polices in different age groups.
Abbreviations
- AIC:
-
Akaike information criterion
- DTR:
-
diurnal temperature range
- GAM:
-
generalized additive regression model
- LAB%:
-
laboratory-confirmed influenza-positive rate
- RH:
-
relative humidity
- VP:
-
vapor pressure
- WS:
-
wind speed.
References
Beard F, Mcintyre P, Gidding H, Watson M (2006) Influenza related hospitalisations in Sydney, New South Wales, Australia. Arch Dis Child 91:20–25
Braganza K, Karoly DJ, Arblaster JM (2004) Diurnal temperature range as an index of global climate change during the twentieth century. Geophys Res Lett 31:405–407
Chan PK, Mok HY, Lee TC, Chu IM, Lam WY, Sung JJ (2009) Seasonal influenza activity in Hong Kong and its association with meteorological variations. J Med Virol 81:1797–1806
Demirci E, Cuhadaroglu B (2000) Statistical analysis of wind circulation and air pollution in urban Trabzon. Energy Build 31:49–53. https://doi.org/10.1016/S0378-7788(99)00002-X
Dowell SF (2001) Seasonal variation in host susceptibility and cycles of certain infectious diseases. Emerg Infect Dis 7:369–374
Feng C, Li J, Sun W, Zhang Y, Wang Q (2016) Impact of ambient fine particulate matter (PM 2.5) exposure on the risk of influenza-like-illness: a time-series analysis in Beijing, China. Environ Health 15:17
Fleming D, Harcourt S, Smith G (2003) Influenza and adult hospital admissions for respiratory conditions in England 1989-2001. Commun Dis Public Health 6:231
Fleming DM, Elliot AJ (2005) The impact of influenza on the health and health care utilisation of elderly people. Vaccine 23(Suppl 1):S1
Graudenz GS, Landgraf RG, Jancar S, Tribess A, Fonseca SG, Faé KC, Kalil J (2006) The role of allergic rhinitis in nasal responses to sudden temperature changes. J Allergy Clin Immunol 118:1126–1132
Hair JF Jr, Anderson RE, Tatham RL, Black WC (1995) Multivariate data analysis, 3rd edn. Macmillan Publishing Company, New York
Hambling MH (1964) Survival of the respiratory syncytial virus during storage under various conditions. Br J Exp Pathol 45:647
Hammond GW, Raddatz RL, Gelskey DE (1989) Impact of atmospheric dispersion and transport of viral aerosols on the epidemiology of influenza. Rev Infect Dis 11:494–497
Hong Kong Centre for Health Protection (2017) Flu Express. http://www.chp.gov.hk/en/guideline1_year/29/134/441/304.html. Accessed 12 Feb 2017
Huang X, Mengersen K, Milinovich G, Hu W (2017) Effect of weather variability on seasonal influenza among different age groups in Queensland, Australia: a Bayesian spatiotemporal analysis. J Infect Dis 215:1695–1701. https://doi.org/10.1093/infdis/jix181
Imai Y, Nobuoka S, Nagashima J, Awaya T, Aono J, Miyake F, Murayma M (1998) Acute myocardial infarction induced by alternating exposure to heat in a sauna and rapid cooling in cold water. Cardiology 90:299–301
Izurieta HS, Thompson WW, Kramarz P, Shay DK, Davis RL, DeStefano F, Black S, Shinefield H, Fukuda K (2000) Influenza and the rates of hospitalization for respiratory disease among infants and young children. N Engl J Med 342:232–239
Kang I, Hong MS, Nolasco H, Park SH, Dan JM, Choi JY, Craft J (2004) Age-associated change in the frequency of memory CD4+ T cells impairs long term CD4+ T cell responses to influenza vaccine. J Immunol (Baltimore MD 1950) 173:673–681
Lin YK, Wang YC, Lin PL, Li MH, Ho TJ (2013) Relationships between cold-temperature indices and all causes and cardiopulmonary morbidity and mortality in a subtropical island. Sci Total Environ 461-462:627–635. https://doi.org/10.1016/j.scitotenv.2013.05.030
Liu L, Breitner S, Pan X, Franck U, Leitte AM, Wiedensohler A, von Klot S, Wichmann HE, Peters A, Schneider A (2011) Associations between air temperature and cardio-respiratory mortality in the urban area of Beijing, China: a time-series analysis. Environ Health 10:51
Lowen A, Steel J, Mubareka S, Palese P (2008) High temperature (30 degrees C) blocks aerosol but not contact transmission of influenza virus. J Virol 82:5650–5652
Lowen AC, Samira M, John S, Peter P (2007) Influenza virus transmission is dependent on relative humidity and temperature. PLoS Pathog 3:1470–1476
Luurila OJ (1980) Arrhythmias and other cardiovascular responses during Finnish sauna and exercise testing in healthy men and post-myocardial infarction patients. Acta Medica Scand Suppl 641:1–60
Marquaridt DW (1970) Generalized inverses, ridge regression, biased linear estimation, and nonlinear estimation. Technometrics 12:591–612
McDevitt J, Rudnick S, First M, Spengler J (2010) Role of absolute humidity in the inactivation of influenza viruses on stainless steel surfaces at elevated temperatures. Appl Environ Microbiol 76:3943–3947. https://doi.org/10.1128/aem.02674-09
Mullooly JP, Bennett MD, Hornbrook MC, Barker WH, Williams WW, Patriarca PA, Rhodes PH (1994) Influenza vaccination programs for elderly persons: cost-effectiveness in a health maintenance organization. Ann Intern Med 121:947–952
Neuzil KM, Mellen BG, Wright PF, Jr MEF, Griffin MR (2000) The effect of influenza on hospitalizations, outpatient visits, and courses of antibiotics in children. N Engl J Med 342:225–231
O’brien RM (2007) A caution regarding rules of thumb for variance inflation factors. Quality & Quantity 41:673–690. https://doi.org/10.1007/s11135-006-9018-6
Ramsay TO, Burnett RT, Krewski D (2003) The effect of concurvity in generalized additive models linking mortality to ambient particulate. Matter Epidemiol 14:18–23
Rechsteiner J, Winkler K (1969) Inactivation of respiratory syncytial virus in aerosol. J Gen Virol 5:405–410
Rigby M, Toumi R (2008) London air pollution climatology: indirect evidence for urban boundary layer height and wind speed enhancement. Atmos Environ 42:4932–4947
Ruf BR, Knuf M (2014) The burden of seasonal and pandemic influenza in infants and children. Eur J Pediatr 173:265–276
Schaffer F, Soergel M, Straube D (1976) Survival of airborne influenza virus: effects of propagating host, relative humidity, and composition of spray fluids. Arch Virol 51:263–273
Shaman J, Kohn M (2009) Absolute humidity modulates influenza survival, transmission, and seasonality. Proc Natl Acad Sci U S A 106:3243–3248. https://doi.org/10.1073/pnas.0806852106
Simonsen L (1998) Pandemic versus epidemic influenza mortality: a pattern of changing age distribution. J Infect Dis 178:53–60
Siple PA, Passel CF (1999) Measurements of dry atmospheric cooling in subfreezing temperatures. Wilderness Environ Med 10:176–182
Soebiyanto RP, Farida A, Kiang RK (2010) Modeling and predicting seasonal influenza transmission in warm regions using climatological parameters. PLoS One 5:e9450
Tamerius J, Nelson MI, Zhou SZ, Viboud C, Miller MA, Alonso WJ (2011) Global influenza seasonality: reconciling patterns across temperate and tropical regions. Environ Health Perspect 119:439–445. https://doi.org/10.1289/ehp.1002383
Tamerius JD, Shaman J, Alonso WJ, Bloom-Feshbach K, Uejio CK, Comrie A, Viboud C (2013) Environmental predictors of seasonal influenza epidemics across temperate and tropical climates. PLoS Pathog 9:e1003194
Tang JW, Lai FY, Wong F, Hon KL (2010) Incidence of common respiratory viral infections related to climate factors in hospitalized children in Hong Kong. Epidemiol Infect 138:226–235. https://doi.org/10.1017/s0950268809990410
Thompson WW, Shay DK, Weintraub E, Brammer L, Bridges CB, Cox NJ, Fukuda K (2004) Influenza-associated hospitalizations in the United States. JAMA 292:1333–1340. https://doi.org/10.1001/jama.292.11.1333
Thompson WW, Shay DK, Weintraub E, Brammer L, Cox N, Anderson LJ, Fukuda K (2003) Mortality associated with influenza and respiratory syncytial virus in the United States. JAMA 289:179–186
Togias AG, Naclerio RM, Proud D, Fish JE, Adkinson NF Jr, Kagey-Sobotka A, Norman PS, Lichtenstein LM (1985) Nasal challenge with cold, dry air results in release of inflammatory mediators. Possible mast cell involvement. J Clin Investig 76:1375–1381
Viegas M, Barrero PR, Maffey AF, Mistchenko AS (2004) Respiratory viruses seasonality in children under five years of age in Buenos Aires, Argentina: a five-year analysis. J Infect 49:222–228
Wang XL, Yang L, He DH, Chiu APY, Chan KH, Chan KP, Zhou M, Wong CM, Guo Q, Hu W (2017) Different responses of influenza epidemic to weather factors among Shanghai, Hong Kong, and British Columbia. Int J Biometeorol 61:1043–1053. https://doi.org/10.1007/s00484-016-1284-y
WHO (2012) Vaccines against influenza. WHO position paper–November 2012 Wkly Epidemiol Rec 87:461–476
Wood S, Wood MS (2007) The mgcv package www r-project org
World Health Organization (2009) Influenza (seasonal). http://www.who.int/mediacentre/factsheets/fs211/en/. Accessed 15 Feb 2014
Yang L, Wong CM, Lau EH, Chan KP, Ou CQ, Peiris JS (2008) Synchrony of clinical and laboratory surveillance for influenza in Hong Kong, e1399. PLoS One 3. https://doi.org/10.1371/journal.pone.0001399
Zhang Y, Yan C, Kan H, Cao J, Peng L, Xu J, Wang W (2014) Effect of ambient temperature on emergency department visits in Shanghai, China: a time series study. Environ Health 13:100. https://doi.org/10.1186/1476-069x-13-100
Funding
This work was funded by the National Science Foundation of China (No. 11501124; 81602936).
Author information
Authors and Affiliations
Contributions
All authors contributed to the conception and/or design of this study, data interpretation, writing, and critical revision of the manuscript; and approved the final version to be published. YL contributed to the collection and analysis of the data.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interest.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Electronic supplementary material
ESM 1
(DOCX 22 kb)
Rights and permissions
About this article
Cite this article
Li, Y., Wang, XL. & Zheng, X. Impact of weather factors on influenza hospitalization across different age groups in subtropical Hong Kong. Int J Biometeorol 62, 1615–1624 (2018). https://doi.org/10.1007/s00484-018-1561-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00484-018-1561-z