Abstract
Influenza is an acute respiratory disease that seriously threatens public health. The occurrence of influenza has been proved to be related to a variety of meteorological factors. However, less attention has been paid to the effect of relative humidity (RH) on different types of influenza, especially in subtropical regions. Daily data on laboratory-confirmed influenza cases, weather variables, and air pollutants in Hefei covering the 2014–2019 period were collected. The seasonality and trend of daily influenza cases were explored by the time series seasonal decomposition method. Generalized linear model was fitted in conjunction with distributed lag nonlinear model to quantify the associations of RH with influenza A and influenza B. Subgroup analyses were conducted by sex, age (0–4, 5–17, and ≥18 years), and season (cold and warm seasons). A total of 5238 influenza cases including 2847 influenza A cases and 2391 influenza B cases were recorded. The epidemic of influenza presented a distinct seasonal pattern, and the number of daily influenza cases increased steadily since 2016. High RH was related to an increased risk of influenza A (maximum RR = 1.683, 95%CI: 1.365–2.076), especially among males, females, and school-age children. Low RH was associated with an increased risk of influenza B (maximum RR = 1.252, 95%CI: 1.169–1.340). The contrasting relationships of RH with influenza A and B remained significant in cold seasons. High RH and low RH were significantly associated with the increased risk of influenza A and B, respectively. The findings of our study may provide clues for proposing new effective interventions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Influenza is an acute viral respiratory infection that annually affects 3–5 million people and contributes to 500,000 deaths worldwide, thus generating serious threats to human health and the economy (World Health Organization 2018). There are three types of influenza viruses, namely A, B, and C. In general, type A is more common and is associated with a higher risk of death than type B (Finkelman et al. 2007). People of all ages, especially infants and pre-school children, can be attacked by influenza (Izurieta et al. 2000). The infection usually lasts within a week and is mainly accompanied by fever, myalgia, headache, and cough. These clinical features of influenza are often indistinguishable from the symptoms caused by other respiratory viruses that may also spread in the community (Wiselka 1994). Therefore, laboratory confirmation of influenza infection provides important information for investigating influenza outbreaks. The peak periods of influenza A and influenza B are not consistent, which may be caused by different modes of transmission (Goldstein et al. 2011). Amid the background of rapid global climate change, interest in assessing the impact of weather conditions on the emergence of infectious diseases has surged. In the last decades, a variety of studies have assessed the effects of meteorological parameters such as humidity, temperature, and wind speed (WS) on influenza transmission in tropics and temperate areas (Azziz Baumgartner et al. 2012; Peci et al. 2019; Shaman et al. 2010; Soebiyanto et al. 2014; Xu et al. 2013; Zhang et al. 2015). So far, the applicability of existing findings from subtropics remains uncertain. For example, a recent study elucidated that relative humidity (RH) as low as 51.5% exerted the peaking risk of both influenza A and B (Zhang et al. 2020). However, a 7-year surveillance conducted in Japan suggested that influenza A infection was negatively related to RH, while influenza B infection was positively related to RH (Iha et al. 2016). Guo et al. (2019) described the relationship between RH and influenza cases with a U-shaped curve, showing an increased risk of infection when RH was below 50% or above 80%. In addition, a few studies failed to find a significant association between RH and influenza (Monamele et al. 2017; Tsuchihashi et al. 2011; Zhang et al. 2015).
The present study aimed to address the following objectives: (1) to examine the seasonal variation and long-term trend in the number of influenza cases in Hefei, a subtropical city, from 2014 to 2019; (2) to understand the associations between RH and laboratory-confirmed influenza A and B based on the daily influenza surveillance data; and (3) to explore the vulnerable populations by grouping cases according to sex and age, and further to determine whether the association between RH and influenza differs by season.
Material and methods
Study site
Hefei is the capital city of Anhui Province with a resident population of 8,189,000 by the end of 2019. It is located in eastern China, at latitude 31° 52′ N and longitude 117° 17′ E. The city now has 4 districts (Baohe, Luyang, Yaohai, and Shushan), 4 counties (Lujiang, Feidong, Feixi, and Changfeng), and one county-level city (Chaohu) under its jurisdiction (Fig. 1).
Influenza data
As influenza is a notifiable infectious disease, information on each sampled case should be collected by physicians in sentinel hospitals and reported to the Chinese Influenza Surveillance Information System (CISIS). Based on the diagnostic criteria for influenza (WS 285–2008) (http://www.nhc.gov.cn), influenza cases were confirmed by the following criteria: (1) fever ≥38 °C; (2) acute onset of respiratory symptoms without other diagnoses; and (3) nasopharyngeal/throat swab specimens tested positive for influenza viruses. The daily reported data including age, sex, types of influenza viruses, and date of onset in Hefei between 1 January 2014 and 31 December 2019 were derived from the CISIS. The annual population size data in Hefei was retrieved from Anhui Provincial Bureau of Statistics (http://tjj.ah.gov.cn/).
Meteorological and air pollution data
Data on daily RH (%), mean temperature (MT, °C), and WS (m/s) between 1 January 2014 and 31 December 2019 were provided by the China Meteorological Data Service Center (http://data.cma.cn/). We also obtained data on ambient air pollutants from the Hefei Municipal Ecology and Environment Bureau (http://sthjj.hefei.gov.cn/), including daily average concentrations of PM2.5 (μg/m3), NO2 (μg/m3), and SO2 (μg/m3) and daily maximum 8-h average concentrations of O3 (μg/m3).
Statistical analysis
To examine the seasonal variation and long-term trend of the number of influenza cases in Hefei from 2014 to 2019, a seasonal-trend decomposition analysis which decomposes the time series into seasonality, trend, and remainder components was performed (Willis et al. 2012).
Spearman correlation tests were firstly applied to understand the correlations between meteorological parameters and air pollutants to avoid any multi-collinearity issue. When the correlation coefficient was less than 0.7, it was considered that there was no multi-collinearity issue. Since daily influenza count typically followed an over-dispersed Poisson distribution, a generalized linear model linked by a quasi-Poisson distribution was employed. The distributed lag nonlinear model was developed to quantify the lag relationship between RH and influenza. MT, WS, and four air pollutants were all controlled for in the regression model. The optimal degrees of freedom (dfs) were selected based on the quasi-Poisson Akaike Information Criterion (Q-AIC) (Gasparrini et al. 2010). The equation for the final model can be expressed as follows: 
where Yt and μt refer to the observed and expected counts of influenza on the day t, respectively; α is the intercept; RHt,l means the cross-basis for RH and β denotes vector of coefficients for RHt,l; l represents the number of lag days; ns() represents the natural cubic spline function; MT was controlled with 4 dfs; WS was controlled with 5 dfs; air pollutants (AP) including PM2.5, NO2, SO2, and O3 were controlled with 3 dfs; 8 dfs per year was selected to adjust for the seasonality and long-term trends; DOWt and Holidayt were modeled as dummy variables to adjust for the possible impacts of the day of week and public holidays, respectively; population was also taken into account in the regression model. Referring to the previous studies (Liu et al. 2019; Park et al. 2020; Roussel et al. 2016), a lag of 1 week was chosen to fully capture the overall effect of RH on daily count of influenza. The risk estimates were calculated using the RH corresponding to the minimum infection risk as a reference value, expressed as relative risk (RR) and its 95% confidence intervals (CIs). In the same way, we also explored the association between RH and different types of influenza (A and B).
In order to determine the vulnerable subgroups, the stratified analysis was performed by age (0–4 years, 5–17 years, and ≥18 years) and sex. In addition, the lag relationship between RH and influenza in cold seasons (from October to March) and warm seasons (from April to September) was evaluated separately. Finally, to assess the robustness of the models, we performed sensitivity analyses by applying different dfs for time per year (dfs = 6–8), MT (dfs = 3–5), WS (dfs = 3–5), and the four air pollutants (dfs = 3–5). All data analyses were implemented using the packages “dlnm” and “splines” in R environment (Version 3.6.1). The statistical tests were two-sided with a significant level set at p < 0.05.
Results
Data description
The descriptive statistics of the daily laboratory-confirmed influenza cases, meteorological variables, and air pollutants in Hefei from 2014 to 2019 are summarized in Table 1. A total of 5238 influenza cases (2847 influenza A cases and 2391 influenza B cases) were recorded during the study period. The daily count of influenza cases ranged from 0 to 48, with an average of 2.39. There were 2856 males (54.52%) and 2382 females (45.48%). The vast majority of the influenza cases were children aged 5–17 years (63.84%), followed by adults (20.85%) and pre-school children aged 0–4 years (15.31%). There were more cases in cold seasons (77.82%) than in warm seasons (22.18%). The median of RH was 77% (range: 33 to 100%). As presented in Figure S1, the Spearman correlation coefficients (r) among all parameters were less than 0.7.
Seasonal decomposition analysis
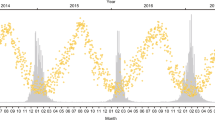
Figure 2 depicts the results of seasonal decomposition analysis of influenza epidemics, revealing a distinct seasonal pattern each year. Specifically, the epidemic of influenza A presented a semiannual seasonal peak, with the primary peak occurring in winter (December to February) and the second peak happening in summer (July to August) (Figure S2). The epidemic of influenza B only showed a peak occurring in winter (December to February) (Figure S3). Overall, there was a steadily increasing trend in the number of influenza cases, especially since the year 2016.
Effects of RH on influenza A and B
The contour plots for RR of different types of influenza along RH and lag days qualitatively revealed that there was a nonlinear lag relationship between RH and influenza A and B (Figure S4). Additionally, the overall exposure-response curve indicated an increased risk of influenza when exposed to RH higher than 57% (Fig. 3). Of note, we observed that the exposure-response curves for influenza A and B displayed almost opposite trends. Accordingly, the present study sought to determine the impact of high RH (90th percentile; 92%) on the risk of influenza A and the impact of low RH (10th percentile; 59%) on the risk of influenza B, respectively.
Table 2 presents the single-day and cumulative effect estimates of high RH on the risk of influenza A by different sex, age, and season, using the RH corresponding to the minimum infection risk (33%) as a reference value. Overall, the single-day effect on influenza A firstly appeared at lag 0 with the highest RR of 1.683 (95%CI: 1.365–2.076) and then decreased to lag 4 with the lowest RR of 1.124 (95%CI: 1.011–1.250). The cumulative risk effects peaked at lag 0–5 with the RR of 5.009 (95%CI: 2.449–10.245). We found that both female and male were susceptible to the adverse effect of high RH, with maximum single-day effects appeared at lag 0 (female: 1.646, 95%CI: 1.209–2.241; male: 1.716, 95%CI: 1.288–2.285). With respect to different age groups, high RH only showed adverse effects on children aged 5–17 years (maximum RR = 2.024, 95%CI: 1.454–2.817, at lag 0). When stratified by different seasons, there was a strong and significant relationship between high RH in cold seasons and influenza A, with the maximum RR (1.886, 95%CI: 1.512–2.353) appearing at lag 0. However, high RH in warm seasons was not statistically associated with influenza A.
Table 3 displays the single-day and cumulative effect estimates of low RH on the risk of influenza B stratified by sex, age, and season, using the RH corresponding to the minimum infection risk (86%) as a reference value. Overall, the single-day effect on influenza B firstly appeared at lag 0 with the highest RR of 1.252 (95%CI: 1.169–1.340) and then dropped to lag 5 with the lowest RR of 1.073 (95%CI: 1.036–1.111). The cumulative risk effects peaked at lag 0–7 with the RR of 2.541 (95%CI: 2.011–3.212). Both female and male were susceptible to the adverse impacts of exposure to low RH, with maximum single-day effects occurred at lag 0 (female: 1.206, 95%CI: 1.090–1.335; male: 1.292, 95%CI: 1.178–1.416). Low RH showed adverse effect both on children aged 0–4 years with the maximum RR of 1.354 (95%CI: 1.113–1.648, lag 0) and 5–17 years with the maximum RR of 1.255 (95%CI: 1.159–1.359, lag 0). In addition, we only observed a strong and significant association between low RH in cold seasons and influenza B, with the maximum RR of 1.273 (95%CI: 1.172–1.383) appearing at lag 0.
Sensitivity analysis
The results from the sensitivity analysis showed that the effect estimates of RH on influenza (including influenza A and B) remained stable when varying the dfs for MT (dfs = 3–5), WS (dfs = 3–5), four air pollutants (dfs = 3–5), and time per year (dfs = 6–8) in the three regression models, respectively (Figures S5–S7).
Discussion
Understanding and predicting the seasonal variation in influenza are critical to optimize public health decisions regarding vaccination strategies and healthcare resource allocation. We observed that the influenza epidemic in Hefei revealed a distinct seasonal pattern, and the number of influenza cases increased steadily since 2016. A study conducted by monitoring influenza reports in 30 provinces in China identified three epidemic areas with obvious seasonal characteristics: epidemic peaked in winter in northern provinces and in spring in southernmost provinces, while mid-latitude provinces experienced semiannual influenza periodicity (Yu et al. 2013). There may be kinds of factors that influence the epidemic pattern of influenza, such as virus evolution, host susceptibility, and external environment. Consistent with a previous report in mainland China (Zou et al. 2013), we have identified complex seasonal patterns of influenza. To be specific, the epidemic of influenza A presented a semiannual periodicity with peaks in winter and summer, whereas the epidemic of influenza B only peaked unimodally in winter. To date, the underlying mechanisms leading to different seasonal patterns of influenza in specific climate regions remain poorly defined.
In this study, we found significant relationships of extreme RH with increased risk of influenza A and B, which were partly consistent with previous studies conducted in subtropical and tropical regions (Chan et al. 2009; Munshili Njifon et al. 2019; Pan et al. 2019; Tang et al. 2010). Marr et al. (2019) concluded that the final equilibrium size of respiratory droplet which exerts important impact on the physics and chemistry of the droplet depends on the ambient humidity. It is plausible that droplet nuclei formed when patients cough or sneeze would swell into hygroscopic particles when exposed to outdoor humid air, which is more conducive to the spread of the influenza virus (Tellier 2006). However, prior studies have yielded controversial findings regarding RH on influenza epidemics. For instance, a multi-region modelling analysis indicated that the activities of influenza A and B viruses were generally favored by higher RH in the temperate regions, whereas this connection was not consistent in subtropical and tropical regions (Chong et al. 2020). Chan et al. (2009) pointed out that the activity of influenza A tended to be higher in humid weather regardless of temperature, which was different from influenza B. By contrast, several studies identified that low humid conditions can preserve the viability of influenza virus and promote the transmission of influenza (Lowen et al. 2007; Yang and Marr 2011), echoing the high incidence of influenza A and B under dry conditions (Shaman et al. 2010; Soebiyanto et al. 2010; Tang et al. 2010). It can be inferred that the occurrence of influenza during the “cold-dry” and “humid-rainy” climates may be due to the U-shaped relationship between influenza activity and RH (Schaffer et al. 1976; Tamerius et al. 2013; Yang et al. 2012). In addition, the contrasting relationships of RH with influenza A and B may be related to the difference in their virological characteristics. For instance, the membrane ion channel in influenza A viruses is the M2 protein, while the membrane ion channel in influenza B viruses is the NB protein (Cox and Subbarao 1999). The changes in positive rates of influenza subtypes may be associated with the complicated interaction between RH, virulence variation of viruses and host susceptibility (Pan et al. 2019).
Subgroup analyses suggested that the effects of high RH varied by the different age groups. Compared with prior research reporting that pre-school children are the vulnerable people (Feng et al. 2016; Li et al. 2018), we found more significant risk of influenza A and B among children aged 5–17 years. Two possible reasons may explain this finding. First, school-age children spend more time outdoors, while the pre-school children have limited opportunities for outdoor activities on rainy days (Huang et al. 2017). Second, it is possible that school-age children are more frequently in close contact with others in schools, which increased the risk of influenza transmission (Kawaguchi et al. 2009). When stratified by season, we only found significant associations between RH in cold seasons and increased risk of influenza A and B. Our results corroborate with a prior review concluded that RH and ambient temperature may interact to affect the airborne survival of aerosolized influenza virus (Tang 2009). It seems reasonable that cold conditions favor the survival of the influenza virus, and increase the chance of catching influenza by causing indoor crowding (Cheng et al. 2016).
The present study had several limitations. First of all, this was ecological research which can only provide clues to etiology and propose hypotheses for future research, but may be restricted in causal inference. Second, data on RH used in the present study were measured outdoors, whereas some people may spend most of their time indoors. Third, the surveillance data for influenza were only retrieved from a city in subtropical region. Accordingly, caution should be taken when generalizing our findings to other regions, especially those with different climate zones. Moreover, large-scale studies covering different climatic zones are still warranted in the future. Fourth, there may be other potential confounding factors that have not been controlled in our study, such as vaccination, medical conditions and misclassification.
Despite the aforementioned limitations, our study has some strengths. Compared with the commonly used weekly or monthly influenza-like illness (ILI) counts as the outcome, the daily laboratory-confirmed data enable minimization of residual confounding and provide more precise assessment. Considering the seasonality of influenza, we examined the associations of influenza A and B with RH in cold seasons and warm seasons separately. Furthermore, confounding factors including MT, WS, and air pollutants have been controlled in the regression models.
Conclusion
The epidemic of influenza presented a distinct seasonal pattern, and there was a steadily increasing trend in the number of influenza cases since 2016. High RH was related to an increased risk of influenza A, especially among males, females, and school-age children. Low RH was associated with an increased risk of influenza B. Additionally, the associations of RH with influenza A and B were only observed in cold seasons, respectively. These findings might provide guidance for the development of an early warning system based on RH in order to timely response to the epidemic of influenza.
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- RH:
-
relative humidity
- WS:
-
wind speed
- CISIS:
-
the Chinese Influenza Surveillance Information System
- MT:
-
mean temperature
- CIs:
-
confidence intervals
- AP:
-
air pollutants
- Dfs:
-
degrees of freedom
- DOW:
-
day of week
References
Azziz Baumgartner E, Dao CN, Nasreen S, Bhuiyan MU, Mah EMS, Al Mamun A, Sharker MA, Zaman RU, Cheng PY, Klimov AI, Widdowson MA, Uyeki TM, Luby SP, Mounts A, Bresee J (2012) Seasonality, timing, and climate drivers of influenza activity worldwide. J Infect Dis 206:838–846
Chan PK, Mok HY, Lee TC, Chu IM, Lam WY, Sung JJ (2009) Seasonal influenza activity in Hong Kong and its association with meteorological variations. J Med Virol 81:1797–1806
Cheng YH, Wang CH, You SH, Hsieh NH, Chen WY, Chio CP, Liao CM (2016) Assessing coughing-induced influenza droplet transmission and implications for infection risk control. Epidemiol Infect 144:333–345
Chong KC, Lee TC, Bialasiewicz S, Chen J, Smith DW, Choy WSC, Krajden M, Jalal H, Jennings L, Alexander B, Lee HK, Fraaij P, Levy A, Yeung ACM, Tozer S, Lau SYF, Jia KM, Tang JWT, Hui DSC, Chan PKS (2020) Association between meteorological variations and activities of influenza A and B across different climate zones: a multi-region modelling analysis across the globe. J Inf Secur 80:84–98
Cox NJ, Subbarao K (1999) Influenza. Lancet 354:1277–1282
Feng C, Li J, Sun W, Zhang Y, Wang Q (2016) Impact of ambient fine particulate matter (PM2.5) exposure on the risk of influenza-like-illness: a time-series analysis in Beijing, China. Environ Health 15:17
Finkelman BS, Viboud C, Koelle K, Ferrari MJ, Bharti N, Grenfell BT (2007) Global patterns in seasonal activity of influenza A/H3N2, A/H1N1, and B from 1997 to 2005: viral coexistence and latitudinal gradients. PLoS One 2:e1296
Gasparrini A, Armstrong B, Kenward MG (2010) Distributed lag non-linear models. Stat Med 29:2224–2234
Goldstein E, Cobey S, Takahashi S, Miller JC, Lipsitch M (2011) Predicting the epidemic sizes of influenza A/H1N1, A/H3N2, and B: a statistical method. PLoS Med 8:e1001051
Guo Q, Dong Z, Zeng W, Ma W, Zhao D, Sun X, Gong S, Xiao J, Li T, Hu W (2019) The effects of meteorological factors on influenza among children in Guangzhou, China. Influenza Other Respir Viruses 13:166–175
Huang X, Mengersen K, Milinovich G, Hu W (2017) Effect of weather variability on seasonal influenza among different age groups in Queensland, Australia: a Bayesian spatiotemporal analysis. J Infect Dis 215:1695–1701
Iha Y, Kinjo T, Parrott G, Higa F, Mori H, Fujita J (2016) Comparative epidemiology of influenza A and B viral infection in a subtropical region: a 7-year surveillance in Okinawa, Japan. BMC Infect Dis 16:650
Izurieta HS, Thompson WW, Kramarz P, Shay DK, Davis RL, DeStefano F, Black S, Shinefield H, Fukuda K (2000) Influenza and the rates of hospitalization for respiratory disease among infants and young children. N Engl J Med 342:232–239
Kawaguchi R, Miyazono M, Noda T, Takayama Y, Sasai Y, Iso H (2009) Influenza (H1N1) 2009 outbreak and school closure, Osaka Prefecture, Japan. Emerg Infect Dis 15:1685
Li Y, Wang XL, Zheng X (2018) Impact of weather factors on influenza hospitalization across different age groups in subtropical Hong Kong. Int J Biometeorol 62:1615–1624
Liu Z, Zhang J, Zhang Y, Lao J, Liu Y, Wang H, Jiang B (2019) Effects and interaction of meteorological factors on influenza: based on the surveillance data in Shaoyang, China. Environ Res 172:326–332
Lowen AC, Mubareka S, Steel J, Palese P (2007) Influenza virus transmission is dependent on relative humidity and temperature. PLoS Pathog 3:1470–1476
Marr LC, Tang JW, Van Mullekom J, Lakdawala SS (2019) Mechanistic insights into the effect of humidity on airborne influenza virus survival, transmission and incidence. J R Soc Interface 16:20180298
Monamele GC, Vernet MA, Nsaibirni RFJ, Bigna JJR, Kenmoe S, Njankouo MR, Njouom R (2017) Associations between meteorological parameters and influenza activity in a subtropical country: case of five sentinel sites in Yaoundé-Cameroon. PLoS One 12:e0186914
Munshili Njifon HL, Monamele CG, Kengne Nde C, Vernet MA, Bouba G, Tchatchouang S, Njankouo MR, Tapondjou R, Deweerdt L, Mbacham W, Njouom R (2019) Influence of meteorological parameters in the seasonality of influenza viruses circulating in Northern Cameroon. Influenza Other Respir Viruses 13:158–165
Pan M, Yang HP, Jian J, Kuang Y, Xu JN, Li TS, Zhou X, Wu WL, Zhao Z, Wang C, Li WY, Li MY, He SS, Zhou LL (2019) Association of meteorological factors with seasonal activity of influenza A subtypes and B lineages in subtropical western China. Epidemiol Infect 147:e72
Park JE, Son WS, Ryu Y, Choi SB, Kwon O, Ahn I (2020) Effects of temperature, humidity, and diurnal temperature range on influenza incidence in a temperate region. Influenza Other Respir Viruses 14:11–18
Peci, A., Winter, A.L., Li, Y., Gnaneshan, S., Liu, J., Mubareka, S., Gubbay, J.B., 2019. Effects of absolute humidity, relative humidity, temperature, and wind speed on influenza activity in Toronto, Ontario, Canada. Appl Environ Microbiol 85.
Roussel M, Pontier D, Cohen JM, Lina B, Fouchet D (2016) Quantifying the role of weather on seasonal influenza. BMC Public Health 16:441
Schaffer FL, Soergel ME, Straube DC (1976) Survival of airborne influenza virus: effects of propagating host, relative humidity, and composition of spray fluids. Arch Virol 51:263–273
Shaman J, Pitzer VE, Viboud C, Grenfell BT, Lipsitch M (2010) Absolute humidity and the seasonal onset of influenza in the continental United States. PLoS Biol 8:e1000316
Soebiyanto RP, Adimi F, Kiang RK (2010) Modeling and predicting seasonal influenza transmission in warm regions using climatological parameters. PLoS One 5:e9450
Soebiyanto RP, Clara W, Jara J, Castillo L, Sorto OR, Marinero S, de Antinori ME, McCracken JP, Widdowson MA, Azziz-Baumgartner E, Kiang RK (2014) The role of temperature and humidity on seasonal influenza in tropical areas: Guatemala, El Salvador and Panama, 2008-2013. PLoS One 9:e100659
Tamerius JD, Shaman J, Alonso WJ, Bloom-Feshbach K, Uejio CK, Comrie A, Viboud C (2013) Environmental predictors of seasonal influenza epidemics across temperate and tropical climates. PLoS Pathog 9:e1003194
Tang JW (2009) The effect of environmental parameters on the survival of airborne infectious agents. J R Soc Interface 6(Suppl 6):S737–S746
Tang JW, Lai FY, Nymadawa P, Deng YM, Ratnamohan M, Petric M, Loh TP, Tee NW, Dwyer DE, Barr IG, Wong FY (2010) Comparison of the incidence of influenza in relation to climate factors during 2000-2007 in five countries. J Med Virol 82:1958–1965
Tellier R (2006) Review of aerosol transmission of influenza A virus. Emerg Infect Dis 12:1657–1662
Tsuchihashi Y, Yorifuji T, Takao S, Suzuki E, Mori S, Doi H, Tsuda T (2011) Environmental factors and seasonal influenza onset in Okayama city, Japan: case-crossover study. Acta Med Okayama 65:97–103
Willis MD, Winston CA, Heilig CM, Cain KP, Walter ND, Mac Kenzie WR (2012) Seasonality of tuberculosis in the United States, 1993-2008. Clin Infect Dis 54:1553–1560
Wiselka M (1994) Influenza: diagnosis, management, and prophylaxis. Bmj 308:1341–1345
World Health Organization (2018) Influenza (Seasonal) [updated 6 November 2018] Available from: http://www.who.int/mediacentre/factsheets/fs211/en/. [cited 14 September 2020].
Xu Z, Hu W, Williams G, Clements AC, Kan H, Tong S (2013) Air pollution, temperature and pediatric influenza in Brisbane, Australia. Environ Int 59:384–388
Yang W, Elankumaran S, Marr LC (2012) Relationship between humidity and influenza A viability in droplets and implications for influenza's seasonality. PLoS One 7:e46789
Yang W, Marr LC (2011) Dynamics of airborne influenza A viruses indoors and dependence on humidity. PLoS One 6:e21481
Yu H, Alonso WJ, Feng L, Tan Y, Shu Y, Yang W, Viboud C (2013) Characterization of regional influenza seasonality patterns in China and implications for vaccination strategies: spatio-temporal modeling of surveillance data. PLoS Med 10:e1001552
Zhang Y, Feng C, Ma C, Yang P, Tang S, Lau A, Sun W, Wang Q (2015) The impact of temperature and humidity measures on influenza A (H7N9) outbreaks-evidence from China. Int J Infect Dis 30:122–124
Zhang Y, Ye C, Yu J, Zhu W, Wang Y, Li Z, Xu Z, Cheng J, Wang N, Hao L, Hu W (2020) The complex associations of climate variability with seasonal influenza A and B virus transmission in subtropical Shanghai, China. Sci Total Environ 701:134607
Zou J, Yang H, Cui H, Shu Y, Xu P, Xu C, Chen T (2013) Geographic divisions and modeling of virological data on seasonal influenza in the Chinese mainland during the 2006-2009 monitoring years. PLoS One 8:e58434
Author information
Authors and Affiliations
Contributions
Qian Wu and Jun He: conceptualization, writing- original draft preparation, visualization. Jun He: methodology. Qian Wu: software and data curation. Wen-Yan Zhang, Ke-Fu Zhao, Jing Jin, Jun-Ling Yu, Qing-Qing Chen, Sai Hou, and Meng Zhu: investigation. Zhiwei Xu and Hai-Feng Pan: supervision, writing- reviewing and editing.
Corresponding authors
Ethics declarations
Ethical approval and consent to participate
This study was approved by the Ethical Committee of Anhui Medical University (Hefei, Anhui, China).
Consent for publication
Not applicable (this study does not contain any individual person’s data in any form).
Competing interests
The authors declare no competing interests.
Additional information
Responsible Editor: Lotfi Aleya
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 1246 kb)
Rights and permissions
About this article
Cite this article
Wu, Q., He, J., Zhang, WY. et al. The contrasting relationships of relative humidity with influenza A and B in a humid subtropical region. Environ Sci Pollut Res 28, 36828–36836 (2021). https://doi.org/10.1007/s11356-021-13107-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-021-13107-1