Abstract
Renal histological features of focal segmental glomerulosclerosis (FSGS) are found in 75% of pediatric patients with steroid-resistant nephrotic syndrome. In order to evaluate the predictive factors of chronic kidney disease (CKD), we retrospectively reviewed the records of 110 children with biopsy-proven FSGS admitted between 1972 and 2004. Renal survival was analyzed by the Kaplan–Meier method and Cox’s regression model. Two multivariate models were developed: (1) from the onset of symptoms to the occurrence of CKD and (2) from the time of renal biopsy to CKD. Mean follow-up time was 10 years [standard deviation ((SD) 5.5], and 24 patients (21.8%) progressed to CKD. At baseline, after adjustment three variables remained as independent predictors of CKD: age >6.5 years (RR=3.3, 95% CI=1.3–7.8), creatinine >1 mg/dl (RR=2.5, 95% CI=0.97–6.5), and non-response to steroids (RR=7.3, 95% CI=2.7–19.7). In a model with continuous variables only age and non-response to steroids were associated with CKD. At the time of renal biopsy, after adjustment two variables remained as independent predictors of CKD: hematuria (RR=3.0, 95% CI=1.2–7.3) and creatinine >0.8 mg/dl (RR=4.3, 95% CI=1.7–10.6). In a model with continuous variables four factors predicted CKD: age, creatinine, hematuria, and percentage of global sclerosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The International Study of Kidney Disease in Children (ISKDC) reported primary focal segmental glomerulosclerosis (FSGS) as a relatively rare cause of nephrotic syndrome in children, observed in only 5% to 7% of biopsies [1–3]. However, 75% of steroid-resistant patients exhibit renal histological features of FSGS [4], although a recent study reported 32.9% [5]. In addition, recent studies have demonstrated an increased incidence of FSGS in adults and children [6–8]. The clinical course and prognosis of FSGS is heterogeneous in children. The reported frequency of end stage renal disease (ESRD) ranges widely from 13% to 78% in studies with up to 20 years of follow-up [9].
A number of studies have shown that some clinical, laboratory, and pathologic features are predictors of outcome, such as the degree of proteinuria at presentation, presenting serum creatinine concentration, race, age at diagnosis, extent of interstitial fibrosis, and morphologic type of lesion (cellular or collapsing) [9–12]. However, most of these studies with larger samples enrolled only adult patients. In the pediatric setting, many cohort studies have involved small numbers of patients and a relatively short follow-up period.
This retrospective cohort study was undertaken with the aim to identify variables that are possible predictors of progression to chronic kidney disease (CKD) by using data available at the time of onset of nephrotic symptoms and at the time of renal biopsy.
Patients and methods
Patients
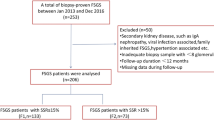
The data were collected retrospectively from the records of the Pediatric Nephrology Unit (PNU), Federal University of Minas Gerais. The PNU is situated in Belo Horizonte (State of Minas Gerais, Brazil). The center is associated with Hospital das Clínicas, a tertiary teaching hospital belonging to the Brazilian Public Health System, which provides clinical, laboratory and treatment support to all patients at no charge. The Belo Horizonte region has a total population of approximately 8 million. In the past decade 30 new cases of nephrotic syndrome per year (approximately 10% of FSGS) have been referred to the PNU. The study included all children and adolescents admitted from March 1972 to February 2004 with biopsy-proven primary FSGS and a minimal follow-up period of 12 months. The diagnosis of primary FSGS was established if there was no clinical evidence of a systemic disease or if there was any pathologic evidence of primary glomerular disease. The medical records were reviewed, and patients with clinical evidence of systemic disease associated with glomerulopathy, vesicoureteral reflux, or solitary kidney (or nephrectomy) were excluded from analysis. In addition, at entry to our Unit all patients with nephrotic syndrome were submitted to serological tests for hepatitis, syphilis, systemic lupus erythematosus, and, more recently, HIV [13, 14]. The data reviewed were obtained (1) at admission: gender, race, age at the onset of nephrotic syndrome symptoms, age at admission, height, weight, blood pressure, response to steroid therapy, laboratory data (serum creatinine, serum urea, glomerular filtration rate, 24-h urinary protein excretion, hematuria); (2) at the time of renal biopsy: age, height, weight, blood pressure, laboratory data (serum creatinine, serum urea, glomerular filtration rate, 24-h urinary protein excretion, hematuria). Ethnicity (variable race in analysis) was established by clinical examination according to skin color, hair color and texture. According to the Brazilian Institute of Geography and Statistics (IBGE), 98.3% of the Brazilian population has been categorized into three “races”: white (53.7%), black (6.2%), and intermediate color (38.4%) (https://doi.org/www.ibge.gov.br/home/estatistica/populacao/censo2000/populacao/cor_raca_Censo2000.pdf). For analysis purposes, the categories black and intermediate color were merged under the “non-white” label. Glomerular filtration rate (GFR) was estimated by the method of Schwartz et al. [15]. Proteinuria (in grams per 24 hours) was adjusted by body surface area (BSA) because of the wide amplitude of age at entry in the study. Blood pressure was measured according to the recommendations of the Task Force on Blood Pressure in Children. Blood pressure was standardized for age and gender using the Task Force tables, and the 95th percentile was used as the cut-off point [16, 17].
Treatment protocol
Prednisone was started at a dose of 2 mg/kg per day (maximum daily dose 60 mg) administered orally in a single morning dose for 4 weeks, followed by 4 weeks of the same daily dose given every other day. After week 8, prednisone was progressively tapered off at the rate of 25% a week until complete discontinuation had been achieved by week 12. Steroid-resistant or steroid-dependent patients received cyclophosphamide at the dose of 2 mg/kg for 12 weeks or 3 mg/kg for 8 weeks concurrently with low-dose prednisone. Since this was a retrospective study there was inevitable heterogeneity in the treatment of steroid-resistant and cyclophosphamide non-responder patients. Patients who did not respond to this initial regime were given high-dose methylprednisolone, intravenously, plus oral administration of an alkylating agent as proposed by Mendoza et al. [18] or, more recently, cyclosporine at an initial dose of 5 mg/kg per day. Patients classified as steroid-dependent were given a low dose of alternate-day prednisone for a long-term period. The definitions of steroid-dependent, steroid-resistant and frequent-relapser nephrotic syndrome were made according to the International Study of Kidney Disease in Children [19]. Patients were also classified according to their response to the initial course of prednisone at our Unit (by week 8): (1) a complete response was defined as a proteinuria <0.3 g/day and clinical remission of nephrotic syndrome; (2) a partial response was defined as urinary protein excretion of <1 g/day and >0.3 g/day, and (3) no response was defined as urinary protein excretion of >1 g/day. For analysis purposes, the categories “complete response” and “partial response” were merged into a single category.
Histopathological analysis
All biopsies were stained with hematoxylin–eosin, periodic acid-Schiff (PAS), and Masson’s trichrome for light microscopy evaluation, and with fluorescent antibodies against IgG, IgM, IgA, and C3 for immunofluorescence analysis. The diagnosis of FSGS was established on morphologic grounds from the kidney biopsy according to the criteria of the International Study of Kidney Diseases in Childhood [2]. All specimens were reviewed for the present study by the same pathologist who was blind to the clinical outcome. The severity of glomerular changes was assessed by calculating the percentage of glomeruli with segmental and total sclerosis. The localization (vascular/tuft) and morphology (collapsing/cellular) of the changes were also determined. Other histological changes (mesangial cellularity, interstitial fibrosis, interstitial infiltration, tubular atrophy and blood vessel involvement) were scored according to a semiquantitative scoring system as follows: 0=no change, 1=focal changes, 2=mild involvement, 3=moderate changes, and 4=severe changes [20].
Predictive factors
Two models were developed: (1) from the onset of symptoms of nephrotic syndrome to the occurrence of CKD; (2) from the time of renal biopsy to CKD (see below). For the first model the following variables were recorded: age at admission, gender, race, hypertension, serum creatinine concentration, GFR, serum urea level, hematuria (more than five red blood cells per cubic millimeter), proteinuria (in grams per 24 hours per BSA), and initial response to prednisone. For the second model the same variables were recorded at the time of renal biopsy. In addition, pathologic variables were also included in the analysis: global sclerosis (percentage), segmental sclerosis (percentage), localization (vascular/tuft), and morphology (collapsing/cellular). Three histological variables were dichotomized (absent/present): mesangial hypercellularity, vascular involvement, and tubulointerstitial fibrosis.
Moreover, two different strategies were used for each model. First, models were developed with all categorized variables as presented in Tables 1 and 2. The code used for dichotomous variables was 1 (presence) and 0 (absence). Continuous variables were categorized using either traditional cut-off levels or the third quartile for continuous variables. Second, models were developed with all variables included in the model as they were initially recorded (i.e., continuous variables without dichotomization).
Outcome
CKD, defined as estimated glomerular filtration rate <60 ml/min per 1.73 m2 BSA in two consecutive examinations, was considered as the outcome variable in the analysis. Renal survival was measured from the date of onset of nephrotic symptoms to the date of CKD. Chronic kidney disease stage 5 was defined as a GFR <15 ml/min per 1.73 m2 BSA or the need for renal replacement therapy.
Statistical analysis
Data are reported as the mean and standard deviation (SD). For both models the analysis was conducted in two steps. In the first, we performed univariate analysis to identify variables that were significantly associated with adverse outcome. Univariate analyses were performed by the Kaplan–Meier method [21]. Differences between patient subgroups were assessed by the two-sided log rank test. Cox’s regression model was applied to identify variables that were independently associated with adverse outcome [22]. Only those variables that were found to be associated with adverse outcome by univariate analysis (P<0.25) were included in Cox’s regression model. Then, in a backward elimination strategy, those variables that retained a significant independent association with adverse outcome (P<0.05) were included in the final model [23]. Model assumptions were checked graphically by log-minus-log versus time plots for each variable.
Ethical aspects: the study was approved by the Ethics Committee of UFMG.
Results
Baseline findings (n=110)
A total of 110 patients was included in the analysis; 71 were male (64.5%), and 55 (50%) were white. The median age at admission was 5 years (range 1 year–15 years). Mean follow-up time was 10 years (SD 5.5, range 12 months to 26 years). A total of 87 (79%) patients was followed up for more than 5 years and 61 (55.4%) for more than 10 years. Twenty-four patients (21.8%) progressed to CKD in a median time of 85 months (range 15–212 months) after the onset of nephrotic syndrome and in a median time of 48 months (range 6–194 months) after the renal biopsy. Twenty-two patients progressed to CKD stage 5. The probability of CKD was estimated to be 8% at 5 years, 17% at 10 years, 32% at 15 years, and 43% at 20 years after the onset of nephrotic syndrome. The main clinical and biochemical characteristics and unadjusted renal survival analysis of the 110 patients included in the study are shown in Table 1.
In the renal survival analysis four variables recorded at admission were found to be significantly associated with the development of CKD during follow-up: age >6.5 years, non-response to steroids, creatinine >1.0 mg/dl, and hematuria. The estimate of renal survival at 10 years after the onset of nephrotic syndrome was of 89% for patients <6.5 years, as opposed to 59% for patients above this age. Figure 1 illustrates the influence of age at onset of symptoms on the development of CKD. Response to therapy with prednisone at admission was complete in 42 children (38.8%) and partial in 34 (31.4%), and 32 (29.6%) patients presented resistance to the initial course of prednisone. Two patients who developed CKD were not classified according to initial response to prednisone due to non-adherence to the treatment protocol. Renal survival was estimated at 10 years after diagnosis in 96% for patients who presented a complete or partial response to the initial course of steroids, whereas the estimate for patients without a response was 54% (Fig. 2). The median renal survival time for patients who did not respond to prednisone was 12 years (95% CI=5.3–18.6). Survival was estimated at 89% 10 years after the onset of symptoms in patients with creatinine <1.0 mg/dl at admission and at 43% for patients with creatinine >1.0 mg/dl (Fig. 3). According to our criteria, two other variables were included in multivariate analysis: white race and decade of admission before 1980. In multivariate analysis, after adjustment three variables remained as independent predictors of chronic renal failure (CRF) in children and adolescents with FSGS: age >6.5 years (RR=3.3, 95% CI=1.3–7.8, P=0.007), creatinine >1 mg/dl (RR=2.5, 95% CI=0.97–6.5, P=0.056), and non-response to steroids (RR=7.3, 95% CI=2.7–19.7, P<0.001). The median renal survival time was 2.9 years (95% CI=0.9–4.9) for patients who presented the three predictive factors and 6.2 years for patients with two factors (95% CI=3.2–9.3) (Fig. 4). All four patients who presented the three factors developed CKD, whereas only 8.5% (five out of 59) of patients without any predictive factors presented deterioration of renal function. In multivariate analysis including continuous variables, only two variables remained as independent predictors of CKD at baseline: age (RR=1.014, 95% CI=1.004–1.0023, P=0.004) and non-response to steroids (RR=7.7, 95% CI=2.7–19.5, P<0.001).
Data at the time of renal biopsy (n=104)
All patients were submitted to a renal biopsy at a median age of 6.9 years (range 1 year–19 years). The median time span between onset of symptoms and renal biopsy was 2 years (range 1 month–13 years). Six patients were excluded from this analysis: two children had already presented a GFR <60 ml/min per 1.73 m2 BSA at the time of the renal biopsy, and laboratory data could not be retrieved for four other patients. The probability of CKD was estimated to be 15% at 5 years, 25% at 10 years, and 33% at 15 years after the renal biopsy. The main clinical, biochemical, and pathologic characteristics at the time of renal biopsy and the unadjusted renal survival analysis are shown in Table 2.
In the renal survival analysis two variables recorded close to the time of renal biopsy were found to be significantly associated with the development of CKD during follow-up: hematuria and creatinine >0.8 mg/dl. The estimate of renal survival at 10 years after the renal biopsy was 68% for patients with hematuria at the time of biopsy and 78% for patients without hematuria. Renal survival 10 years after the renal biopsy was estimated at 84% in patients with creatinine <0.8 mg/dl and at 49% in patients with creatinine >0.8 mg/dl recorded soon after the renal biopsy. Age >11 years at the time of renal biopsy was marginally associated with CKD. Renal survival 10 years after the renal biopsy was estimated at 81% and 55% in patients younger and older than 11 years, respectively. GFR at the time of renal biopsy was also marginally associated with CKD. Renal survival 10 years after the renal biopsy was estimated at 83% and 66% in patients with GFR >95 ml/min per 1.73 m2 BSA and <95 ml/min per 1.73 m2 BSA, respectively. Among the pathologic features, only two variables presented a marginal association with CKD: global sclerosis and localization of the scar (Table 2). According to our criteria, two other variables were included in multivariate analysis: race and blood pressure >95th percentile. In multivariate analysis, after adjustment two variables remained as independent predictors of CKD at the time of renal biopsy: hematuria (RR=3.0, 95% CI=1.2–7.3, P=0.015) and creatinine >0.8 mg/dl (RR=4.3, 95% CI=1.7–10.6, P=0.001). The median renal survival time was 2.6 years (95% CI=1.1–4.0) for patients who presented the two predictive factors and 16 years (95% CI=9.5–22.8) for patients with one risk factor at the time of renal biopsy (Fig. 5). In multivariate analysis including continuous variables, four variables remained as independent predictors of CKD at the time of renal biopsy: age (RR=1.15, 95% CI=1.041–1.268, P=0.006), percent global sclerosis (RR=1.041, 95% CI=1.002–1.080), P=0.037), serum creatinine concentration (RR=8.8, 95% CI=1.4–55.1, P=0.02), and presence of hematuria (RR=4, 95% CI=1.4–10.4, P=0.004).
Discussion
In this retrospective cohort study we investigated possible predictive factors of CKD in children and adolescents with primary FSGS. We developed two models of prediction of renal survival. In the first multivariate model, based on categorized variables recorded at onset of nephrotic syndrome, three independent factors were identified by the Cox regression model: age >6.5 years, creatinine >1.0 mg/dl, and non-response to a standard 8-week prednisone protocol. On the other hand, when variables were inserted as originally recorded, only two were found to be predictive of CKD: age and non-response to prednisone. In the model based on time of renal biopsy, two variables were predictors of CKD: creatinine >0.8 mg/dl and presence of hematuria. Of note, in the model with continuous variables at the time of renal biopsy, four variables were found to be associated with CKD: age, percent global sclerosis, serum creatinine level, and presence of hematuria.
It is important to point out the limitations associated with the retrospective design of our study. The possible main weakness is the limited control over patient treatment through the decades, because of the large span of time of patient enrollment in our cohort. For example, four patients had to be excluded from the second model because laboratory data were not appropriately collected at the time of renal biopsy. Nevertheless, some features of the study may increase the strength of our findings, such as the size of our sample, management by the same medical team, and length of follow-up.
In our series 24 patients (21.8%) presented deterioration of renal function, and the probability of CKD was estimated at 17% at 10 years and at 32% at 15 years after the onset of initial symptoms of nephrotic syndrome. A number of cohort studies of FSGS in children [9, 12, 24–30] and in adults [11, 31–36] has been reported in literature. Other studies have included both children and adults in the analysis [20, 37–39]. Nevertheless, few studies in the pediatric setting have investigated predictive factors of outcome. In addition, a small number of studies has applied survival analysis and estimated the probability of impairment of renal function over time, with adjustment for possible confounders. In adults with FSGS the degree of proteinuria at presentation has been the clinical feature most often used to predict the clinical course [40]. The presence of nephrotic-range proteinuria has been associated with a poor prognosis in primary FSGS, with 50% of patients reaching CKD over 6 to 8 years [10, 31, 37, 41]. However, a recent study applying multivariate analysis did not demonstrate the degree of proteinuria as an independent predictor of renal survival [32]. Yoshikawa et al. [28] have demonstrated a similar prognosis in pediatric patients with FSGS with and without nephrotic syndrome. In our series all patients presented with nephrotic syndrome, and we investigated the degree of proteinuria as a predictor of renal survival. Our findings suggest that the degree of proteinuria at baseline as well as at time of renal biopsy was not a predictor of CKD in children and adolescents with nephrotic syndrome and primary FSGS.
In the present study, age >6.5 years at onset of nephrotic syndrome was a strong predictor of CKD in univariate analysis as well as in multivariate analysis. In addition, age as a continuous variable was also found to be associated with CKD at the onset of nephrotic syndrome and at the time of renal biopsy. In the Cox regression model with continuous variables the interpretation of the risk of CKD is different. For example, the relative risk estimated for age at the time of renal biopsy was 1.15 (95% CI=1.041–1.268, P=0.006). Thus, according to our analysis, for each increase in age by 1 year the risk of CKD increased by approximately 15%. To our knowledge no studies in the pediatric setting have specifically investigated the age at onset of nephrotic syndrome as a predictive factor of renal survival in FSGS. Ellis et al. [24] reported a mean age at onset of disease of 5.3 years (SD 4.5) in 20 children with FSGS who retained normal renal function and of 7.6 (SD 4.4) in 12 patients with renal failure. Sorof et al. [9] reported that the probability of FSGS increases with age in pediatric patients with proteinuria, especially in African-American patients, although the authors did not examine the implication of this fact in prognosis.
Serum creatinine concentration at onset of disease has been regarded as a predictor of renal failure by many studies on adult patients. Wehrmann et al. [38] investigated 250 patients with FSGS with a mean age of 32 years and reported that creatinine levels higher than 1.3 mg/dl at the time of renal biopsy were predictive of renal failure, in univariate analysis. However, in multivariate analysis, creatinine level did not remain as an independent prognostic marker. Other studies have also demonstrated that patients with creatinine >1.3 mg/dl at presentation had a significantly poorer renal survival [36, 41, 42]. Chitalia et al. [32] investigated 111 patients (16 to 70 years at the time of renal biopsy) and showed that plasma creatinine >0.14 mmol/l was a predictor of renal failure, in both univariate and multivariate analysis. In our series, serum creatinine at baseline as well as at the time of renal biopsy was a predictor of renal survival. The estimated probability of renal survival at 10 years after the onset of nephrotic syndrome for patients with serum creatinine <1.0 mg/dl at admission (89%) was twice that for children with creatinine >1.0 mg/dl (43%). Interestingly, at the time of renal biopsy, creatinine at a slightly lower cut-off point (0.8 mg/dl) was an even stronger predictor of CKD, in either univariate or multivariate analysis. However, these results should be interpreted with caution in the pediatric setting, because a creatinine cut-off point of 1 mg/dl has a different significance for children of distinct ages. In is important to notice that creatinine concentration as a continuous variable remained as a predictor of CKD only at time of renal biopsy.
The initial response to corticosteroids in patients with idiopathic FSGS has been considered poor, and only about 20% to 25% of them achieve complete remission of proteinuria [43]. Recently, we described the response of our patients after the first course of 8 weeks of prednisone [44]. The response to prednisone was complete in 42 children (38.8%) and partial in 34 (31.4%), and 32 (29.6%) patients were resistant to the initial course of prednisone. Two patients were not classified according to initial response to prednisone due to non-adherence to the treatment protocol. The initial response to the standard steroid protocol has been regarded as a powerful predictor of renal failure by many studies of children and adult patients [45]. In our series, at baseline the stronger predictor of renal survival was the total or partial response to the initial 8-week course of prednisone. The median renal survival time for patients who did not respond to prednisone was 12 years (95% CI=5.3–18.6), whereas only 4% of patients who had a total or partial response to prednisone presented CKD 10 years after the onset of nephrotic syndrome. Arbus et al. [25] demonstrated a 10-year renal survival rate of 100% for patients who achieved consistent remission and only of 38% for those who did not respond. Cattran and Rao [39] reported long-term renal survival of 100% in children with complete remission of proteinuria after a prednisone course, as opposed to a 73%, 58%, and 51% rate over 5 years, 10 years, and 15 years, respectively, for children without remission. Recently, Chun et al. [11] have shown in a series of adult patients an overall renal survival rate of 92% and 33% at 10 years for those patients who, respectively, attained or did not attain remission. Of note, some studies have shown that patients with steroid-resistant nephrotic syndrome with homozygous or compound heterozygous mutations in NPHS2 do not respond to standard steroid treatment and have a reduced risk of recurrence of FSGS in a renal transplant [46, 47].
In the present study we did not confirm some variables, such as race and degree of proteinuria, as predictors of renal survival. In the study by Ingulli and Tejani [48] of 70 nephrotic children with FSGS, 78% of black patients had progressed to ESRD over 8.5 years of follow-up as compared with only 33% of white patients. In the study by Sorof et al. the estimated 5-year renal survival was only 8% in African-American (AA) children compared with 31% in non-AA patients. However, Rydel et al. [42] did not find any significant racial difference in the rate of renal survival in nephrotic adults with FSGS. The 10-year renal survival rate was 64% for black patients and 55% for white patients. Race, as a prognostic marker in FSGS, is a complex issue to ascertain, since patients labeled as “black” or “white” may have quite different genetic backgrounds, especially in regions with a high rate of miscegenation. Brazilians form one of the most heterogeneous populations in the world, which is the result of five centuries of interethnic crosses of peoples from three continents: the European colonizers, mainly represented by the Portuguese, the African slaves, and the autochthonous Amerindians. Recently, in an elegant study, Parra et al. [49] have shown that in Brazil, at the individual level, color, as determined by physical evaluation, is a poor predictor of genomic African ancestry, estimated by molecular markers. Thus, the absence of significance of the variable “race” in our analysis was somewhat expected, because the physical characteristics of the Brazilian population are not reliable markers of genetic ancestry.
The prognostic significance of histologic features has been extensively assessed in adult patients [11, 32–34, 36, 38, 50, 51]. Only the extent of interstitial fibrosis has been shown to consistently predict a poor prognosis [32, 40]. In our pediatric population we found only the proportion of glomeruli with global sclerosis to be a continuous variable predictive of CKD. The estimated relative risk was 1.041 (95% CI=1.002–1.080), meaning that, for each increase in 10% of glomeruli with global sclerosis, the risk of CKD increased by approximately 40%. Ibels et al. [52] reported on a series of 68 patients (mean age 44 years, range 8 to 78 years) with primary FSGS and also showed that the percentage of glomeruli with global and segmental sclerosis was a predictor of adverse outcome, in a multivariate analysis. However, the percentage of global sclerosis has not been found to be a predictor of renal survival in the adult population [11, 34]. A less severe histopathological involvement found in younger patients may account for the scarce significance of histological features as predictor of renal outcome. For example, Gulati et al. [20] have shown that the histological features of renal specimens from children older than 12 years and adults are more extensively affected than those of specimens from younger children. In our series there was a preponderance of mild/moderate glomerular involvement, tubular atrophy, and interstitial fibrosis. These findings are concordant with those of other pediatric series [24, 25, 30]. Therefore, probably in children and adolescents with FSGS, clinical variables are more powerful predictors of renal survival than histopathological features. In addition, Ichikawa and Fogo [53] pointed out that the lack of correlation between renal outcome and structural involvement in FSGS is expected, because the heterogeneous histological involvement at the whole kidney level is deducted by random sampling and single-section analysis of the material obtained by biopsy. Even in the adult population, Chun et al. [11] have demonstrated that patients who attained remission had excellent prognosis, regardless of the histologic lesion.
The possible main clinical implication of our study of predictive factors of CKD in pediatric patients with FSGS is that there is a subgroup of patients with a patently worse prognosis. The mean renal survival time for patients older than 6.5 years, with serum creatinine >1.0 mg/dl and no response to the initial course of prednisone, was only 2.9 years (95% CI=0.9–4.9) after the onset of nephrotic syndrome. An accurate estimate of the prognosis of chronic diseases is particularly important for several reasons. First, prognostic information is useful to advise patients and parents about the likely outcome of the disease. Second, knowledge about the prognosis for an individual patient or subgroups of patients can be used as a guide for selecting therapeutic options. Third, the identification of the variables with most influence on the rate of progression to CKD may lead to important etiologic and pathogenic insights and allow the characterization of relevant therapeutic targets [32]. Therefore, for this subgroup of children and adolescents, alternative treatment protocols must be developed and assessed in appropriate, randomized, clinical trials.
In conclusion, the clinical course of primary FSGS in children and adolescents is heterogeneous. In the present study various potential clinical or histological features were assessed by the proportional hazard model, and some variables were identified as significant predictors of renal survival. At presentation, three factors were predictive of CKD: age, creatinine level, and non-response to prednisone. At the time of renal biopsy, four factors were predictive of CKD: age, percentage of global sclerosis, creatinine level , and presence of hematuria.
References
White RH, Glasgow EF, Mills RJ (1970) Clinicopathological study of nephrotic syndrome in childhood. Lancet 1:1353–1359
Churg J, Habib R, White RH (1970) Pathology of the nephrotic syndrome in children: a report for the International Study of Kidney Disease in Children. Lancet 760:1299–1302
No authors listed (1978) Nephrotic syndrome in children: prediction of histopathology from clinical and laboratory characteristics at time of diagnosis. A report of the International Study of Kidney Disease in Children. Kidney Int 13:159–165
Fuchshuber A, Gribouval O, Ronner V, Kroiss S, Karle S, Brandis M, Hildebrandt F (2001) Clinical and genetic evaluation of familial steroid-responsive nephrotic syndrome in childhood. J Am Soc Nephrol 12:374–378
Nammalwar BR, Vijayakumar M, Prahlad N (2006) Experience of renal biopsy in children with nephrotic syndrome. Pediatr Nephrol 21:286–288
D’Agati V (1994) The many masks of focal segmental glomerulosclerosis. Kidney Int 46:1223–1241
Haas M, Spargo BH, Coventry S (1995) Increasing incidence of focal-segmental glomerulosclerosis among adult nephropathies: a 20-year renal biopsy study. Am J Kidney Dis 26:740–750
Bonilla-Felix M, Parra C, Dajani T, Ferris M, Swinford RD, Portman RJ, Verani R (1999) Changing patterns in the histopathology of idiopathic nephrotic syndrome in children. Kidney Int 55:1885–1890
Sorof JM, Hawkins EP, Brewer ED, Boydstun, II, Kale AS, Powell DR (1998) Age and ethnicity affect the risk and outcome of focal segmental glomerulosclerosis. Pediatr Nephrol 12:764–768
Korbet SM, Schwartz MM, Lewis EJ (1994) Primary focal segmental glomerulosclerosis: clinical course and response to therapy. Am J Kidney Dis 23:773–783
Chun MJ, Korbet SM, Schwartz MM, Lewis EJ (2004) Focal segmental glomerulosclerosis in nephrotic adults: presentation, prognosis, and response to therapy of the histologic variants. J Am Soc Nephrol 15:2169–2177
Martinelli R, Okumura AS, Pereira LJ, Rocha H (2001) Primary focal segmental glomerulosclerosis in children: prognostic factors. Pediatr Nephrol 16:658–661
Ray PE, Xu L, Rakusan T, Liu XH (2004) A 20-year history of childhood HIV-associated nephropathy. Pediatr Nephrol 19:1075–1092
Ahuja TS, Abbott KC, Pack L, Kuo YF (2004) HIV-associated nephropathy and end-stage renal disease in children in the United States. Pediatr Nephrol 19:808–811
Schwartz GJ, Brion LP, Spitzer A (1987) The use of plasma creatinine concentration for estimating glomerular filtration rate in infants, children, and adolescents. Pediatr Clin North Am 34:571–590
No authors listed (1987) Report of the second task force on blood pressure control in children. Task force on blood pressure control in children. National Heart, Lung, and Blood Institute, Bethesda, Maryland. Pediatrics 79:1–25
No authors listed (1996) Update on the 1987 Task Force Report on high blood pressure in children and adolescents: a working group report from the National High Blood Pressure Education Program. National High Blood Pressure Education Program Working Group on Hypertension Control in Children and Adolescents. Pediatrics 98:649–657
Mendoza SA, Reznik VM, Griswold WR, Krensky AM, Yorgin PD, Tune BM (1990) Treatment of steroid-resistant focal segmental glomerulosclerosis with pulse methylprednisolone and alkylating agents. Pediatr Nephrol 4:303–307
No authors listed (1981) The primary nephrotic syndrome in children. Identification of patients with minimal change nephrotic syndrome from initial response to prednisone. A report of the International Study of Kidney Disease in Children. J Pediatr 98:561–564
Gulati S, Elhence R, Kher V, Sharma RK, Jain M, Gupta A, Gupta RK (2000) Early versus late-onset idiopathic focal segmental glomerulosclerosis. Pediatr Nephrol 14:960–964
Kaplan EL, Meier P (1958) Nonparametric estimation from incomplete observation. J Am Stat Assoc 53:457–481
Cox DR (1972) Regression models and life-tables. J R Stat Soc 34:184–220
Greenland S (1989) Modeling and variable selection in epidemiologic analysis. Am J Public Health 79:340–349
Ellis D, Kapur S, Antonovych TT, Salcedo JR, Yunis EJ (1978) Focal glomerulosclerosis in children: correlation of histology with prognosis. J Pediatr 93:762–768
Arbus GS, Poucell S, Bacheyie GS, Baumal R (1982) Focal segmental glomerulosclerosis with idiopathic nephrotic syndrome: three types of clinical response. J Pediatr 101:40–45
Tejani A, Nicastri AD, Sen D, Chen CK, Phadke K, Adamson O, Butt KM (1983) Long-term evaluation of children with nephrotic syndrome and focal segmental glomerular sclerosis. Nephron 35:225–231
No authors listed (1985) Focal segmental glomerulosclerosis in children with idiopathic nephrotic syndrome. A report of the Southwest Pediatric Nephrology Study Group. Kidney Int 27:442–449
Yoshikawa N, Ito H, Akamatsu R, Matsuyama S, Hasegawa O, Nakahara C, Matsuo T (1986) Focal segmental glomerulosclerosis with and without nephrotic syndrome in children. J Pediatr 109:65–70
Tufro-McReddie A, Alvarez E, Arrizurieta E, Repetto H (1992) Focal glomerulosclerosis in children: an Argentinian experience. Pediatr Nephrol 6:158–161
Mongeau JG, Robitaille PO, Clermont MJ, Merouani A, Russo P (1993) Focal segmental glomerulosclerosis (FSG) 20 years later. From toddler to grown up. Clin Nephrol 40:1–6
Beaufils H, Alphonse JC, Guedon J, Legrain M (1978) Focal glomerulosclerosis: natural history and treatment. A report of 70 cases. Nephron 21:75–85
Chitalia VC, Wells JE, Robson RA, Searle M, Lynn KL (1999) Predicting renal survival in primary focal glomerulosclerosis from the time of presentation. Kidney Int 56:2236–2242
Schwartz MM, Korbet SM, Rydell J, Borok R, Genchi R (1995) Primary focal segmental glomerular sclerosis in adults: prognostic value of histologic variants. Am J Kidney Dis 25:845–852
Schwartz MM, Evans J, Bain R, Korbet SM (1999) Focal segmental glomerulosclerosis: prognostic implications of the cellular lesion. J Am Soc Nephrol 10:1900–1907
Korbet SM (1999) Clinical picture and outcome of primary focal segmental glomerulosclerosis. Nephrol Dial Transplant 14 [Suppl 3]:68–73
Alexopoulos E, Stangou M, Papagianni A, Pantzaki A, Papadimitriou M (2000) Factors influencing the course and the response to treatment in primary focal segmental glomerulosclerosis. Nephrol Dial Transplant 15:1348–1356
Cameron JS, Turner DR, Ogg CS, Chantler C, Williams DG (1978) The long-term prognosis of patients with focal segmental glomerulosclerosis. Clin Nephrol 10:213–218
Wehrmann M, Bohle A, Held H, Schumm G, Kendziorra H, Pressler H (1990) Long-term prognosis of focal sclerosing glomerulonephritis. An analysis of 250 cases with particular regard to tubulointerstitial changes. Clin Nephrol 33:115–122
Cattran DC, Rao P (1998) Long-term outcome in children and adults with classic focal segmental glomerulosclerosis. Am J Kidney Dis 32:72–79
Korbet SM (1998) Primary focal segmental glomerulosclerosis. J Am Soc Nephrol 9:1333–1340
Velosa JA, Holley KE, Torres VE, Offord KP (1983) Significance of proteinuria on the outcome of renal function in patients with focal segmental glomerulosclerosis. Mayo Clin Proc 58:568–577
Rydel JJ, Korbet SM, Borok RZ, Schwartz MM (1995) Focal segmental glomerular sclerosis in adults: presentation, course, and response to treatment. Am J Kidney Dis 25:534–542
Eddy AA, Symons JM (2003) Nephrotic syndrome in childhood. Lancet 362:629–639
Abrantes MM, Cardoso LS, Lima EM, Silva JM, Diniz JS, Bambirra EA, Oliveira EA (2006) Clinical course of 110 children and adolescents with primary focal segmental glomerulosclerosis. Pediatr Nephrol 21:482–489
Gipson DS, Chin H, Presler TP, Jennette C, Ferris ME, Massengill S, Gibson K, Thomas DB (2006) Differential risk of remission and ESRD in childhood FSGS. Pediatr Nephrol 21:344–349
Niaudet P (2004) Genetic forms of nephrotic syndrome. Pediatr Nephrol 19:1313–1318
Ruf RG, Lichtenberger A, Karle SM, Haas JP, Anacleto FE, Schultheiss M, Zalewski I, Imm A, Ruf EM, Mucha B, Bagga A, Neuhaus T, Fuchshuber A, Bakkaloglu A, Hildebrandt F (2004) Patients with mutations in NPHS2 (podocin) do not respond to standard steroid treatment of nephrotic syndrome. J Am Soc Nephrol 15:722–732
Ingulli E, Tejani A (1991) Racial differences in the incidence and renal outcome of idiopathic focal segmental glomerulosclerosis in children. Pediatr Nephrol 5:393–397
Parra FC, Amado RC, Lambertucci JR, Rocha J, Antunes CM, Pena SD (2003) Color and genomic ancestry in Brazilians. Proc Natl Acad Sci USA 100:177–182
Schwartz MM, Korbet SM (1993) Primary focal segmental glomerulosclerosis: pathology, histological variants, and pathogenesis. Am J Kidney Dis 22:874–883
Stokes MB, Markowitz GS, Lin J, Valeri AM, D’Agati VD (2004) Glomerular tip lesion: a distinct entity within the minimal change disease/focal segmental glomerulosclerosis spectrum. Kidney Int 65:1690–1702
Ibels LS, Gyory AZ, Mahony JF, Caterson RJ, Pollock CA, Waugh DA, Coulshe S (1998) Primary focal sclerosing glomerulonephritis: a clinicopathological analysis. Nephrology (Carlton) 4:9–17
Ichikawa I, Fogo A (1996) Focal segmental glomerulosclerosis. Pediatr Nephrol 10:374–391
Acknowledgments
This study was partially supported by CNPq (Brazilian National Research Council), Pró-Reitoria de Pesquisa (UFMG), and FAPEMIG.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Abrantes, M.M., Cardoso, L.S.B., Lima, E.M. et al. Predictive factors of chronic kidney disease in primary focal segmental glomerulosclerosis. Pediatr Nephrol 21, 1003–1012 (2006). https://doi.org/10.1007/s00467-006-0138-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-006-0138-y