Abstract
Background
Infants and toddlers with kidney failure are susceptible to neurodevelopmental delays due to medical comorbidities and rapid brain development in early childhood. However, research on the neuropsychological development of this patient population has been limited over the past 10 years.
Methods
We performed a retrospective study to evaluate the neurodevelopmental functioning of infants/toddlers with kidney failure who completed the Bayley Scales of Infant and Toddler Development (3rd and 4th Edition) as part of a pretransplant evaluation between 2010 and 2022 (n = 23; Mage = 18 months, SD = 8.53; 16 males) using t-tests, linear model, and Pearson correlations.
Results
Mean Bayley scores of participants were below normative means for cognition (M = 86.74, 95% CI = 80.53–92.94, p < 0.001), language (M = 79.20, 95% CI = 73.32–85.08, p < 0.001), and motor (M = 78.00, 95% CI = 70.15–85.85, p < 0.001) domains. After adjusting for prematurity and epilepsy, patients on dialysis had significantly lower cognitive (78.7 vs. 93.8; p = 0.001) and motor scores (67.1 vs. 85.5; p = 0.01) compared to no dialysis. Pretransplant cognitive scores were positively correlated with posttransplant Full-Scale IQ (r(8) = 0.65 p = 0.04), verbal comprehension (r(8) = 0.75 p = 0.02), and fluid reasoning (r(7) = 0.68 p = 0.045). Similarly, pretransplant language scores were positively correlated with posttransplant Full-Scale IQ (r(7) = 0.74 p = 0.03) and verbal comprehension (r(7) = 0.73 p = 0.03). Of the 16 participants who reached age > 5 years during the study period, seven were diagnosed with a neurodevelopmental disorder, including three with autism spectrum disorder.
Conclusions
Infants and toddlers with kidney failure are at risk of developmental delays and later neurodevelopmental disorders. Dialysis is associated with cognitive and motor delays independent of prematurity and epilepsy.
Graphical abstract
A higher resolution version of the Graphical abstract is available as Supplementary information

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Infants have the highest incidence of kidney failure in the USA, with 27 cases per million. This is in contrast to 8 cases per million for children 1–12 years of age and 16 cases per million people for those 13–17 years of age [1]. Despite substantial improvements in kidney failure outcomes due to advances in kidney transplantation [2], there remain unique neurodevelopmental challenges for infants and toddlers due to their higher medical comorbidities and rapidly developing brains. The rapid formation and pruning of neural synapses during these early years make infants and toddlers particularly vulnerable to early experiences and medical insults [3]. Since infant brains reach 70% of adult volume by 1 year of age and 80% by 2 years [4], kidney failure in infancy and toddlerhood poses a significant threat to the typical neurodevelopmental trajectory.
Infancy and toddlerhood are dynamic periods of motor, language, and cognitive development [5], and early insults may hinder progress in these developmental domains. Recognizing the importance of early assessment, the Kidney Disease Improving Global Outcomes (KDIGO) guidelines recommend neurocognitive assessment for pediatric kidney transplant candidates who develop kidney failure before 5 years of age [6]. However, the available literature delineating neurodevelopmental characteristics of children with kidney disease is limited and largely outdated [7,8,9,10,11,12]. Furthermore, existing studies vary in study design and neurodevelopment assessment methodology, limiting comparisons and specific conclusions. A recent study by Popel et al. (2019), including 15 children with kidney transplants before 5 years of age, and a study by Lullmann et al. (2023), involving 10 kidney transplant recipients assessed at a mean age of ~ 10 years, suggest that neurodevelopmental profiles of children with kidney failure today may differ from those observed 20–30 years ago [13, 14]. The studies by Popel and Lullmann underscore the necessity of current studies to characterize the neurodevelopmental profiles of children in the modern era.
The primary objective of the current study was to characterize the developmental functioning domains of infants and toddlers awaiting a kidney transplant using widely recognized and validated neurodevelopmental assessment tools, as there are no recent studies within this age group, which is most susceptible to neurocognitive deficits. We aimed to include the domains of language and motor functioning in our evaluation, given that previous research has focused on describing cognitive functioning deficits. This study also aimed to contextualize neurodevelopmental functioning in the population by investigating the effects of medical comorbidities and exploring the predictability of future functioning. Considering the effects of early medical insults on neurodevelopment, we hypothesized that infants and toddlers awaiting a kidney transplant would have lower cognitive, language, and motor-standardized scores compared to the normative means. We also hypothesized that medical comorbidities such as epilepsy, prematurity, and dialysis would negatively affect cognitive, language, and motor performances. In addition, we hypothesized that these early cognitive performances would predict future intellectual testing performance after the kidney transplant. Understanding the neurodevelopmental profiles of infants and toddlers and the context in which they occur would inform neurodevelopmental surveillance guidelines, enabling early interventions to optimize outcomes. This is vital as early neurocognitive insults may exert profound and lasting effects on overall neurocognitive trajectories, resulting in significant financial burdens for both patients and the healthcare system.
Methods
Procedures
The Institutional Review Board (IRB) at the University of Minnesota approved this retrospective study.
Data source
We conducted an electronic medical record review to obtain data on infants and toddlers who were referred for neuropsychological evaluations within the MHealth Fairview Health Care System in Minneapolis, MN, USA, between January 2010 and October 2022, as part of their kidney transplant evaluation.
Study participants
Twenty-five infants and toddlers with kidney failure between ages 0 and 2 years (Mage = 17.44 months, SD = 8.44) were referred for a pre-transplant neuropsychological evaluation as part of their pre-transplant workup per the institutional protocol. However, two patients completed parent interviews and parent report measures only and did not complete performance-based assessments resulting in their exclusion from the analyses. Eight (Mage-pre = 20 months, SD = 9.49) of the 23 patients included in the study had a post-transplant neuropsychological evaluation (Mage-post = 80.75 months (i.e., 6.73 years), SD = 30.65).
Study variables
The neuropsychological measures used for this investigation (described below) were guided by clinical indications or determined by pediatric neuropsychologists or pediatric psychologists with specialty training in neuropsychological assessment. In addition to the neuropsychological variables, we retrieved information on demographic variables, dialysis, history of prematurity, and history of epilepsy. Given that neurodevelopmental diagnoses are usually not assigned to infants and toddlers, neurodevelopmental diagnoses later in life (i.e., age older than five years) were also retrieved from the medical chart.
Measures
The primary neuropsychological outcome of interest was infant and toddler development, which was assessed using The Bayley Scales of Infant and Toddler Development – 3rd Edition (Bayley-3) [15] and Bayley Scales of Infant and Toddler Development – 4th Edition (Bayley-4) [16], depending on which measure was current at the time of testing. Measures were administered by experienced pediatric psychologists, pediatric neuropsychologists, psychometrists with training and experience administering these measures to clinical populations, or post-doctoral fellows in pediatric psychology and pediatric neuropsychology under the supervision of a licensed clinical psychologist.
The Bayley Scales of Infant and Toddler Development are standardized tests designed to assess the developmental functioning of infants and toddlers aged 1 month to 42 months. They include three composite index scores in the areas of cognitive, language, and motor functioning, which are provided as standard scores (M = 100, SD = 15). Subtest performances are provided as scaled scores (M = 10, SD = 3) and age-equivalents. The cognitive composite index is based on one subtest and assesses a child’s ability to perceive, process, and respond to environmental stimuli. The language composite index consists of two subtests evaluating a child’s receptive and expressive language skills. The motor composite index also consists of two subtests assessing a child’s gross and fine motor skills. The Bayley-3 and Bayley-4 are widely used in clinical and research settings to evaluate infants’ and toddlers’ developmental abilities, to monitor developmental progress, and to inform age-appropriate interventions. These measures have shown high reliability and validity (Bayley-3: test–retest reliability coefficients range from 0.55 to 0.92; internal consistency coefficients range from 0.67 to 0.98; concurrent validity coefficients range from 0.35 to 0.80; predictive validity coefficients range from 0.21 to 0.82 [15]; Bayley-4: test–retest reliability coefficients range from 0.69 to 0.93; internal consistency coefficients range from 0.70 to 0.98; concurrent validity coefficients range from 0.30 to 0.80; predictive validity coefficients range from 0.26 to 0.82 [16]).
For the subset of study population who underwent post-transplant neuropsychological testing, age-appropriate measures of intellectual functioning were administered per clinical standards (The Wechsler Preschool and Primary Scale of Intelligence (WPPSI) and the Wechsler Intelligence Scale for Children (WISC)). Both are widely used psychological assessment tools for measuring cognitive abilities in children and demonstrate high reliability and strong validity [17, 18].
Data analysis
Patient characteristics were summarized using means and standard deviations or frequencies and percentages. One-sample t-tests compared the sample mean Bayley standard scores for each of the composite indexes (i.e., cognitive, language, and motor) to the normative mean, while paired samples t-tests compared scores across composite indexes. The frequency of patients who had delays and impairments in the development of skill areas was also calculated. A delay was defined as a score of > 1 standard deviation below the normative mean (i.e., a standard score of less than 85) and an impairment was defined as > 2 standard deviations below the normative mean (i.e., a standard score of less than 70). The relationships between Bayley standard scores and cause of kidney disease and age at start of dialysis were examined using linear models. The relationships between Bayley standard scores and medical comorbidities (history of epilepsy, gestational age at birth, and current dialysis treatment) were examined using linear models, including dialysis, epilepsy, and gestational age at birth as covariates. Model results are reported using estimated marginal means with 95% confidence intervals by the dialysis group and adjusted for epilepsy and gestational age at birth. Pearson correlation coefficients were computed in a subgroup of 8 participants with post-transplant testing to assess the relations between developmental skills as an infant/toddler and cognitive performance after receiving a kidney transplant. For participants who were at least five years of age at the time of this study (n = 16), neurodevelopmental diagnoses were examined to determine neurodevelopmental outcomes. Analyses were performed using the Statistical Package for the Social Sciences (SPSS) version 25 and R version 4.2.2 [19]. A two-sided p-value less than 0.05 was regarded as statistically significant.
Results
Study participants’ characteristics
Table 1 presents the demographic characteristics of the study participants. The majority of participants spoke English (91%; n = 21). The most common medical comorbidity in the study cohort was prematurity (i.e., < 37 weeks gestation; 61%; n = 14). Only one patient was very premature at birth (i.e., < 32 weeks). Four participants (17%) had diagnoses of epilepsy prior to the transplant. Eleven participants (44%) were on chronic dialysis at the time of the neurodevelopmental assessment. Five patients (22%) started dialysis after the neuropsychological evaluation but prior to the transplant.
Neurodevelopmental profile of infants and toddlers awaiting a kidney transplant
Compared to the normative mean scores (M = 100, SD = 15), the study cohort’s mean scores were significantly lower for cognitive (M = 86.74, 95% CI = 80.53–92.94, p < 0.001), language (M = 79.20, 95% CI = 73.32–85.08, p < 0.001), and motor (M = 78.00, 95% CI = 70.15–85.85, p < 0.001) domains on the Bayley. Regarding specific domains, mean language (79.20 vs. 86.74; p = 0.005) and motor standard scores (78.0 vs. 86.74; p = 0.005) were each significantly lower than the mean cognitive standard scores; however, language and motor standard scores were not significantly different from each other (79.20 vs. 78.0; p = 0.49).
Figure 1 presents age equivalents for cognitive, receptive language, expressive language, fine motor, and gross motor domains in relation to the chronological age of the study participants. As illustrated, the testing age equivalent was below the chronological age for most participants in all five domains. Notably, the difference was most pronounced for receptive language and gross motor skills.
Developmental delays were more common in language and motor skills; six patients (26%) had delays in cognitive skills, 13 patients (65%) had delays in language skills, and 12 patients (57%) had delays in motor skills. When using the more stringent criteria for impairment, three patients (13%) had a cognitive impairment, 6 patients (30%) had a language impairment, and six patients (29%) had a motor impairment for age. Figure 2 presents the proportion of patients with delay or impairment in one or more domains. As illustrated, 13% of patients (n = 3) had impaired scores across all developmental domains assessed by the Bayley. Notably, these three patients had a history of epilepsy.
Effects of dialysis on neurodevelopmental profile
Within the group of patients on dialysis prior to the evaluation (n = 11), the length of dialysis at the time of neuropsychological evaluation was significantly correlated with the delay by months in the cognitive performance (r = 0.77, p = 0.009). However, we observed no statistically significant correlation between the length of dialysis and the delay by months in language and motor performances (Fig. 3). After adjusting for gestational age at birth and epilepsy status, patients on dialysis at the time of evaluation had significantly lower mean cognitive scores (78.7 (95% CI = 72.9–84.5) vs. 93.8 (95% CI = 88.6–99.0); p = 0.001) and mean motor scores (67.1 (95% CI = 57.5–76.6) vs. 85.5 (95% CI = 76.9–94.1); p = 0.01) compared to those not on dialysis. The mean language scores were also lower for patients on dialysis compared to those not on dialysis, however, the difference did not achieve statistical significance (73.6 (95% CI = 65.9–81.3) vs. 83.8 (95% CI = 76.8–90.7); p = 0.06) (Table 2) (Fig. 4).
Effect of age of onset of kidney failure on neurodevelopmental profile
The median age of dialysis initiation was 5.9 (IQR: 0.3–18.6) months. We observed lower motor and language scores in patients who started dialysis within the first 30 days of life vs. later; however, the difference did not achieve statistical significance. Similarly, we found no difference in the cognitive scores between the two groups (Table 3).
Effect of the underlying cause of kidney failure on neurodevelopmental profile
We observed no difference in the mean cognitive, language, and motor scores between patients with congenital anomalies of kidney disease (CAKUT) and non-CAKUT causes of kidney failure (Table 4).
Correlations with the future neurocognitive performance
Pre-transplant Bayley cognitive scores were positively and significantly correlated with post-transplant Full-Scale IQ (r(8) = 0.65 p = 0.04; Fig. 5), verbal comprehension (r(8) = 0.75 p = 0.02), and fluid reasoning (r(7) = 0.68 p = 0.045). Furthermore, pre-transplant Bayley language scores were positively and significantly correlated with post-transplant Full-Scale IQ (r(7) = 0.74 p = 0.03) and verbal comprehension (r(7) = 0.73 p = 0.03; Fig. 5). However, pre-transplant Bayley motor scores did not show significant correlations with any post-transplant scores.
Neurodevelopmental disorders
Of the 16 participants who reached school age (age > 5) during the study period, 44% (7 out of 16) were diagnosed with a neurodevelopmental disorder associated with/secondary to a medical condition. Of these 7 patients, 3 (18.8%) received a diagnosis of autism spectrum disorder (ASD) and co-morbid language disorder. Two of these three patients had multicystic dysplastic kidney disease and one had congenital renal dysplasia. Two additional patients of the 7 received the diagnosis of an intellectual disorder.
Discussion
We found significantly lower cognitive, language, and motor scores among infants and toddlers awaiting a kidney transplant versus same-aged peers. Compared to patients not on dialysis at the time of evaluation, we observed significantly lower cognitive and motor scores among patients on dialysis independent of prematurity and epilepsy histories. Additionally, the testing age equivalent of patients was less than their chronological age for all 5 domains. We also found that Bayley's cognitive score before the transplant was significantly correlated with Full-Scale IQ, verbal comprehension, and fluid reasoning after the transplant. Similarly, Bayley's language score before the transplant was significantly correlated with verbal comprehension scores after the transplant. Overall, the prevalence of neurodevelopmental delays in our study cohort ranged between 26 and 65%, and that of impairments ranged between 13 and 30%. The highest prevalence of delays and impairments was in the language domain, followed closely by the motor domain.
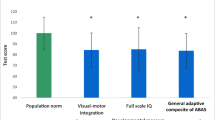
We observed cognitive delays in 26% and cognitive impairment in 13% of our study participants. Similarly, we noted language delays in 65% and motor delays in 57% of patients. This is in contrast with the rates of cognitive delays of 1–1.5% and any developmental delay of 15%, as captured by common screening measures, among preschool children in the USA [20]. Existing studies on neurocognitive delays and impairments in children with kidney disease are few and conflicting. Unlike our study, a retrospective study by Warady et al. of 28 infants with kidney failure found significant development delay in only 1 child using the Modified Developmental Assessment Test and Bayley Scales of Infant Development-Mental Scale [11]. Contrarily, a study of 15 infants and preschool children with chronic kidney disease (CKD) found that 53% had composite scores on Mullen Scales of Early Learning of > 2 standard deviations below the mean compared to only 7% of healthy controls [21]. Similarly, Popel et al. found a standard score < 70 on at least one standardized measure of neurocognitive functioning (Full-Scale IQ, Visual Motor Integration, and General Adaptive Composite) among 27% of 15 children with kidney transplant before 5 years of age [14]. The differences in the rates of delays and impairment between studies may be related to differences in instruments, the definitions used for delays/impairment, and patient characteristics (two of the three cited studies included older children). The varying data further highlight the importance of additional research to characterize neurocognitive deficits in infants and toddlers with kidney failure.
We observed a significant correlation between dialysis duration and the delay by months in cognitive performance. Earlier studies have also noted a correlation between neurocognitive deficits and the length of dialysis exposure [14, 22, 23]. After adjusting for prematurity and epilepsy histories, we found significantly lower cognitive and motor scores among infants and toddlers on dialysis compared to no dialysis. In a study of 124 preschool children with mild to moderate CKD, Hooper et al. found abnormal birth history and seizures to be associated with an increased risk of neurocognitive concerns [24]. However, our findings were independent of the histories of prematurity and epilepsy. While it is a common practice to monitor early neurodevelopmental outcomes of children with premature birth and those with epilepsy, it is less common to monitor the neurodevelopmental outcomes of children with early dialysis treatment. Current results indicate that it is necessary to have regular monitoring of neurocognitive development in these children.
Our study identified significant correlation between cognitive and language scores before the transplant and Full-Scale IQ, verbal comprehension scores, and fluid reasoning after the transplant. Since the posttransplant neuropsychological evaluation occurred at a mean of 5 years after the pretransplant evaluation, it may be that scores improved after the transplant but declined again with the progression of posttransplant CKD. However, we lack data to evaluate this possibility. Congruent with our findings, a study of 12 children who developed kidney failure within the first 16 months of life showed persistent neurocognitive deficits in school-age years [22]. The persistence of the early deficits into later years indicates the importance of early recognition and early intervention to optimize outcomes.
We observed ASD in 3 patients, constituting 19% of the study participants. In comparison, the incidence ranges between 0.6 and 1.0% for the general population [32]. There is emerging evidence suggesting that ASD and CKD may have shared pathogenesis in terms of genetic copy number variants and environmental factors [33]. A recent study evaluating co-morbidities in adults with ASD and intellectual disabilities identified CKD in 25.4% of the patients [34]. However, the prevalence of ASD in patients with childhood-onset kidney failure has not been reported before. Given that an early diagnosis of ASD can improve long-term outcomes and reduce the lifetime financial burden of ASD [35], providers should be cognizant of the possibility of ASD in this population.
Our findings align with neurocognitive deficits observed in other solid organ transplant candidates. A retrospective study of 15 infants awaiting a liver transplant for biliary atresia found significant delays in gross motor and language skills [25]. Similarly, a retrospective study of 20 children under 2 years of age awaiting a heart transplant found delays across various domains of neurocognition, including general cognitive, receptive language, expressive language, gross motor, fine motor, and visual-motor functioning [26]. Developmental delays in the setting of organ failure are likely mediated by several factors. Prolonged hospitalizations may increase stress, which has been shown to impact development [27,28,29]. Hospital stays may limit opportunities for infants, toddlers, and their families to engage in developmentally rich activities, which has historically been a factor driving developmental delays among chronically ill young children [28]. Additionally, medical procedures including dialysis, surgical procedures, medication side effects, and wounds may restrict physical activity in daily environments. Furthermore, infants and toddlers with advanced kidney disease are susceptible to central nervous system lesions, including white matter abnormalities, abnormal myelination, cerebral vascular disease, micro-bleeds, and silent infarctions, which may further enhance neurocognitive deficits [30, 31]. These data support the need for regular screening and early intervention (speech therapy, physical and occupational therapy) for children at risk of developmental delays in the context of an organ failure.
Consistent with KDIGO recommendation [6], our findings support the early identification of neurodevelopmental difficulties in infants and toddlers with kidney failure. The findings from the current investigation also highlight the importance of identifying deficits in language and motor abilities. Furthermore, our findings support close collaboration with the neuropsychology team, perhaps in a multidisciplinary care model setting, to determine timely and appropriate interventions (speech therapy, physical and occupational therapy) for children at risk of developmental delays in the context of kidney failure. Such a collaboration could also facilitate the identification of and advocacy for community-based resources. Since the deficits may persist posttransplant with increased risk of neurodevelopmental disorders, our findings also support posttransplant neuropsychological evaluations at regular intervals for evaluation of persistent deficits. The nephrologists should help families understand the value of interventions at a young age due to the significant brain neuroplasticity that is present in infants and toddlers. Language and sensory-rich activities in locations frequently visited by infants and toddlers (e.g., hospital rooms and dialysis units) may also be beneficial to help stimulate development.
Several limitations of this work warrant consideration. First, our sample size is modest. However, our sample size is consistent with previous research in infants and toddlers with kidney failure. Second, this retrospective study represents a single institution’s experience with neurocognitive assessments for infants and toddlers with kidney failure, limiting the generalizability of the results. This study may also be limited by observation bias, as the clinicians who administered the neurocognitive tests were aware of patients’ health histories. This bias, however, was likely mitigated by the administration of standardized evaluation. Additionally, the observation that the majority of study participants had participated or were participating in developmental interventions at the time of neuropsychological evaluation could have attenuated the severity of deficits. Furthermore, the pre- and posttransplant evaluations were performed using instruments that were age-appropriate but different from each other. This precluded a like-for-like comparison. Nevertheless, we found it valuable to conduct pre- and posttransplant correlation studies, as both instruments represented standardized measures of neurocognition. Finally, the retrospective nature of this investigation did not allow for tracking of prospective medical and psychosocial complications, but rather, a reliance on the available medical records and neuropsychology reports was required. Despite these limitations, this investigation significantly adds to the growing evidence of developmental delays for infants and toddlers with kidney failure. The strength of our study includes the protocol-based neuropsychological evaluation of all transplant candidates, minimizing selection bias and ensuring the generalizability of our findings.
In summary, infants and toddlers with kidney failure exhibit significant cognitive, language, and motor developmental delays with a greater prevalence of language and motor delays. Understanding the developmental functioning of these children prior to the transplant may inform treatment recommendations such as early physical therapy, occupational therapy, and speech therapy to optimize outcomes. Furthermore, documenting functioning prior to the transplant may guide posttransplant monitoring to ensure children meet appropriate developmental milestones after the transplant. Larger, multi-center studies are required to further characterize early childhood neurodevelopmental deficits associated with kidney failure. Studies are also needed to evaluate the effect of early interventions on the neurodevelopmental trajectories of this patient population.
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
USRDS Annual Data Report (2022). Annual Data Report | USRDS (nih.gov). Accessed 30 Nov 23
Chavers BM, Molony JT, Solid CA, Rheault MN, Collins AJ (2015) One-year mortality rates in US children with end-stage renal disease. Am J Nephrol 41:121–128
Kolb B, Mychasiuk R, Gibb R (2014) Brain development, experience, and behavior. Pediatr Blood Cancer 61:1720–1723
Knickmeyer RC, Gouttard S, Kang C, Evans D, Wilber K, Smith JK, Hamer RM, Lin W, Gerig G, Gilmore JH (2008) A structural MRI study of human brain development from birth to 2 years. J Neurosci 28:12176–12182
Gerber RJ, Wilks T, Erdie-Lalena C (2010) Developmental milestones: motor development. Pediatr Rev 31:267–276; quiz 277
Chadban SJ, Ahn C, Axelrod DA, Foster BJ, Kasiske BL, Kher V, Kumar D, Oberbauer R, Pascual J, Pilmore HL, Rodrigue JR, Segev DL, Sheerin NS, Tinckam KJ, Wong G, Knoll GA (2020) KDIGO clinical practice guideline on the evaluation and management of candidates for kidney transplantation. Transplantation 104:S11-s103
Davis ID, Chang PN, Nevins TE (1990) Successful renal transplantation accelerates development in young uremic children. Pediatrics 86:594–600
Lawry KW, Brouhard BH, Cunningham RJ (1994) Cognitive functioning and school performance in children with renal failure. Pediatr Nephrol 8:326–329
Elzouki A, Carroll J, Butinar D, Moosa A (1994) Improved neurological outcome in children with chronic renal disease from infancy. Pediatr Nephrol 8:205–210
Hulstijn-Dirkmaat GM, Damhuis IH, Jetten ML, Koster AM, Schröder CH (1995) The cognitive development of pre-school children treated for chronic renal failure. Pediatr Nephrol 9:464–469
Warady BA, Belden B, Kohaut E (1999) Neurodevelopmental outcome of children initiating peritoneal dialysis in early infancy. Pediatr Nephrol 13:759–765
Madden SJ, Ledermann SE, Guerrero-Blanco M, Bruce M, Trompeter RS (2003) Cognitive and psychosocial outcome of infants dialysed in infancy. Child Care Health Dev 29:55–61
Lullmann O, Conrad AL, Steinbach EJ, Wilgenbusch T, Harshman LA, van der Plas E (2023) Neurocognitive deficits may not resolve following pediatric kidney transplantation. Pediatr Transplant 27:e14505
Popel J, Joffe R, Acton BV, Bond GY, Joffe AR, Midgley J, Robertson CMT, Sauve RS, Morgan CJ (2019) Neurocognitive and functional outcomes at 5 years of age after renal transplant in early childhood. Pediatr Nephrol 34:889–895
Albers CA, Grieve AJ (2007) Test Review: Bayley, N. (2006). Bayley scales of infant and toddler development– third edition. San Antonio, TX: Harcourt Assessment. J Psychoeduc Assess 25:180–190
Bayley N & Aylward GP (2019) Bayley-4: Scales of infant and toddler development, Technical manual, 4th edn. Pearson. Bayley scales of infant and toddler development 4th Ed. pearsonassessments.com
Raiford SE (2018) The Wechsler intelligence scale for children—fifth edition integrated. In: Flanagan DP, McDonough EM (eds) Contemporary intellectual assessment: Theories, tests, and issues. The Guilford Press, pp 303–332
Park SE, Demakis GJ (2017) Wechsler preschool and primary scale of intelligence. In: Zeigler-Hill V, Shackelford TK (eds) Encyclopedia of Personality and Individual Differences. Springer International Publishing, Cham, pp 1–4
R Core Team. R: A language and environment for statistical computing. https://www.r-project.org/
Vitrikas K, Savard D, Bucaj M (2017) Developmental delay: when and how to screen. Am Fam Physician 96:36–43
Duquette PJ, Hooper SR, Icard PF, Hower SJ, Mamak EG, Wetherington CE, Gipson DS (2009) Neurodevelopmental status and adaptive behaviors in preschool children with chronic kidney disease. The Journal of Special Education 43:45–51
Johnson RJ, Warady BA (2013) Long-term neurocognitive outcomes of patients with end-stage renal disease during infancy. Pediatr Nephrol 28:1283–1291
So SK, Chang PN, Najarian JS, Mauer SM, Simmons RL, Nevins TE (1987) Growth and development in infants after renal transplantation. J Pediatr 110:343–350
Hooper SR, Gerson AC, Johnson RJ, Mendley SR, Shinnar S, Lande MB, Matheson MB, Gipson DS, Morgenstern B, Warady BA, Furth SL (2016) Neurocognitive, social-behavioral, and adaptive functioning in preschool children with mild to moderate kidney disease. J Dev Behav Pediatr 37:231–238
Caudle SE, Katzenstein JM, Karpen SJ, McLin VA (2010) Language and motor skills are impaired in infants with biliary atresia before transplantation. J Pediatr 156:936-940.e931
Antonini TN, Dreyer WJ, Caudle SE (2018) Neurodevelopmental functioning in children being evaluated for heart transplant prior to 2 years of age. Child Neuropsychol 24:46–60
Molnar-Varga M, Novak M, Szabo AJ, Kelen K, Streja E, Remport A, Mucsi I, Molnar MZ, Reusz G (2016) Neurocognitive functions of pediatric kidney transplant recipients. Pediatr Nephrol 31:1531–1538
Shields L (2001) A review of the literature from developed and developing countries relating to the effects of hospitalization on children and parents. Int Nurs Rev 48:29–37
Katz DA, Sprang G, Cooke C (2012) The cost of chronic stress in childhood: understanding and applying the concept of allostatic load. Psychodyn Psychiatry 40:469–480
Matsuda-Abedini M, Fitzpatrick K, Harrell WR, Gipson DS, Hooper SR, Belger A, Poskitt K, Miller SP, Bjornson BH (2018) Brain abnormalities in children and adolescents with chronic kidney disease. Pediatr Res 84:387–392
Moodalbail DG, Reiser KA, Detre JA, Schultz RT, Herrington JD, Davatzikos C, Doshi JJ, Erus G, Liu HS, Radcliffe J, Furth SL, Hooper SR (2013) Systematic review of structural and functional neuroimaging findings in children and adults with CKD. Clin J Am Soc Nephrol 8:1429–1448
Salari N, Rasoulpoor S, Rasoulpoor S, Shohaimi S, Jafarpour S, Abdoli N, Khaledi-Paveh B, Mohammadi M (2022) The global prevalence of autism spectrum disorder: a comprehensive systematic review and meta-analysis. Ital J Pediatr 48:112
Clothier J, Absoud M (2021) Autism spectrum disorder and kidney disease. Pediatr Nephrol 36:2987–2995
Miot S, Akbaraly T, Michelon C, Couderc S, Crepiat S, Loubersac J, Picot MC, Pernon É, Gonnier V, Jeandel C, Blain H, Baghdadli A (2019) Comorbidity burden in adults with autism spectrum disorders and intellectual disabilities-a report from the EFAAR (frailty assessment in ageing adults with autism spectrum and intellectual disabilities) study. Front Psychiatry 10:617
Horlin C, Falkmer M, Parsons R, Albrecht MA, Falkmer T (2014) The cost of autism spectrum disorders. PLoS One 9:e106552
Acknowledgements
The authors would like to thank the patients and their families.
Funding
This research was supported by the National Institutes of Health’s National Center for Advancing Translational Sciences, grant UL1TR002494. The content is solely the responsibility of the authors and does not represent the official views of the National Institutes of Health’s National Center for Advancing Translational Sciences.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This retrospective chart review study involving human participants was in accordance with the ethical standards of the institutional and national research committee. The Human Investigation Committee as part of the Institutional Review Board (IRB) of the University of Minnesota approved this study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Danielle Glad and Christopher Anzalone contributed equally as co-first authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Glad, D., Anzalone, C., Kane-Grade, F. et al. Neurodevelopmental profile of infants and toddlers awaiting a kidney transplant. Pediatr Nephrol 39, 2187–2197 (2024). https://doi.org/10.1007/s00467-024-06282-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-024-06282-z