Abstract
Background
Cisplatin is associated with acute kidney injury (AKI) and electrolyte abnormalities. Urine tissue inhibitor of metalloproteinase 2 (TIMP-2) and insulin-like growth factor-binding protein 7 (IGFBP-7) may be early cisplatin-AKI biomarkers.
Methods
We conducted a 12-site prospective cohort study with pediatric patients treated with cisplatin (May 2013–December 2017). Blood and urine (measured for TIMP-2, IGFBP-7) were collected pre-cisplatin, 24-h post-cisplatin, and near hospital discharge during the first or second cisplatin cycle (early visit (EV)) and during second-to-last or last cisplatin cycle (late visit (LV)). Primary outcome: serum creatinine (SCr)-defined AKI (≥ stage 1).
Results
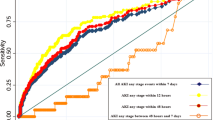
At EV (median (interquartile (IQR)) age: 6 (2–12) years; 78 (50%) female), 46/156 (29%) developed AKI; at LV, 22/127 (17%) experienced AKI. At EV, TIMP-2, IGFBP-7, and TIMP-2*IGFBP-7 pre-cisplatin infusion concentrations were significantly higher in participants with vs. those without AKI. At EV and LV, biomarker concentrations were significantly lower in participants with vs. those without AKI at post-infusion and near-hospital discharge. Biomarker values normalized to urine creatinine were higher in patients with AKI compared to without (LV post-infusion, median (IQR): TIMP-2*IGFBP-7: 0.28 (0.08–0.56) vs. 0.04 (0.02–0.12) (ng/mg creatinine)2/1000; P < .001). At EV, pre-infusion biomarker concentrations had the highest area under the curves (AUC) (range: 0.61–0.62) for AKI diagnosis; at LV, biomarkers measured post-infusion and near discharge yielded the highest AUCs (range: 0.64–0.70).
Conclusions
TIMP-2*IGFBP-7 were poor to modest at detecting AKI post-cisplatin. Additional studies are needed to determine whether raw biomarker values or biomarker values normalized to urinary creatinine are more strongly associated with patient outcomes.
Graphical abstract

A higher resolution version of the Graphical abstract is available as Supplementary information
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Many child cancer survivors experience chronic health issues resulting from their treatment [1–3]. Cisplatin is a chemotherapy drug widely used to treat pediatric cancers. Due to its nephrotoxicity, cisplatin commonly causes acute kidney injury (AKI), which is characterized by an acute serum creatinine (SCr) rise and/or electrolyte abnormalities [4–9]. However, SCr is a non-ideal AKI diagnostic test, since it rises late with AKI and is influenced by factors other than kidney injury such as age, sex, and muscle mass [10, 11]. The investigation of new AKI biomarkers is needed to aid with studying prediction, early diagnosis, and intervention of cisplatin-induced AKI.
Two biomarkers, urinary tissue inhibitor metalloproteinase-2 (TIMP-2), insulin-like growth factor-binding protein-7 (IGFBP-7), and their mathematical product (i.e., TIMP-2*IGFBP-7), were found to be early biomarkers for AKI diagnosis in various cohorts [12–18]. Notably, the Federal Drug Administration (FDA) has approved TIMP-2*IGFBP-7 as an AKI clinical test for critically ill adults [19, 20]. TIMP-2 and IGFBP-7 are tubular cell cycle arrest biomarkers that are upregulated post-kidney injury [12]. Kidney tubular cells enter the state of G1 cell cycle arrest after injury from ischemia or sepsis [21, 22]. This arrest prevents cells from proliferating with potentially damaged DNA and stops cell division until the damage can be repaired, to prevent cell death or senescence from occurring [12, 23]. However, research on this biomarker in pediatric cohorts and in the context of cisplatin-induced AKI is limited.
The Applying Biomarkers to Minimize Long-Term Effects of Childhood/Adolescent Cancer Treatment (ABLE) team project included a prospective, multi-center cohort study with cisplatin-treated pediatric patients with a goal of evaluating urine AKI biomarkers [24, 25]. In the first phase, we reported our findings on urine neutrophil gelatinase-associated lipocalin (NGAL) and kidney injury molecule-1 (KIM-1) [26]. We found urine NGAL and KIM-1 to be higher in AKI patients compared to non-AKI patients and were modest at discriminating for AKI [26]. With the aim of studying additional biomarkers, we describe TIMP-2, IGFBP-7, and TIMP-2*IGFBP-7 excretion in children receiving cisplatin and determine the diagnostic and predictive capacities of these biomarkers of SCr and electrolyte-defined AKI at two separate cisplatin infusion cycles during cancer treatment.
Methods
Design, setting, and patient recruitment
This is a prospective cohort study with cisplatin-treated pediatric patients and followed throughout cisplatin therapy, enrolled from 12 Canadian sites from May 2013 to December 2017 [24, 25]. Method details have been previously published [24, 25]. Patients included were less than 18 years old at cancer diagnosis who started cisplatin treatment, with less than two prior cisplatin cycles in the original ABLE cisplatin cohort, while patients with estimated or measured glomerular filtration rate (GFR) < 30 mL/min/1.73 m2 or kidney transplantation before cisplatin commencement were excluded [24, 25]. For this analysis, participants were excluded if they had no urine biomarker results at any study timepoint. Research ethics board approvals from all sites, and informed consent, and assent if appropriate, were obtained. Figure 1 outlines the recruitment details in a flow chart.
Flow diagram of study participants and urine collection protocol performance. The study flow diagram outlines the number of patients enrolled in the study and with available data for analyses as well as urine successfully collected and measured. At the early visit and late visit, urine specimens for the pre-infusion timepoint were collected on the day of cisplatin infusion, but before cisplatin administration; post-infusion samples were collected 1-day post-cisplatin infusion (in the morning). Samples collected near hospital discharge at the early visit were collected a median (IQR) of 3 (2–4) days post-cisplatin infusion, whereas discharge samples at the late visit were collected 2 (2–4) days post-infusion. aReasons for specimen non-collection at individual timepoints at the early visit and the late visit included insufficient quantity, participant refusal, sample misplaced, and protocol error
Study procedure
After participants were identified (early in their cisplatin therapy, shortly after cancer diagnosis), recruited, and included in the study, baseline clinical data were collected retrospectively (which occurred, at the latest, before the second cisplatin cycle of the planned cancer treatment). Information collected included baseline (pre-cisplatin) clinical data, with demographic information, cancer details, and medical history. After recruitment, participants underwent two study visits during their cancer treatment. The early visit (EV) was defined as either the first or second cisplatin cycle, while the late visit (LV) was defined as the last (or second-to-last) cisplatin cycle of cancer treatment. At each visit, blood (3 mL) and urine (30 ml) were collected at three separate timepoints: (1) pre-infusion (before cisplatin infusion on the day of infusion), (2) post-infusion (the morning post-infusion), and (3) discharge (near time of hospital discharge). Urine samples were collected at all timepoints by mid-stream collection, with cotton balls in diapers, or by perineal bag application. Clinical data including nephrotoxic medications, daily routine standard of care-measured SCr, and electrolyte values were recorded from 3 days before to 10 days post-study visit cisplatin infusion. Data regarding infections, dialysis, routinely measured monthly peak and trough SCr and electrolytes, and intensive care unit (ICU) admissions were collected during the entire cisplatin treatment period (from first to last cisplatin infusion). Further details about the study design and procedure have been previously described [24, 25].
Laboratory measurements
Study sites centrifuged and aliquoted the blood specimens (1000 g, 10 min, 21 °C). Samples, both urine and serum (unspun), were stored at − 80 °C. Specimens were then shipped to the main site in Montreal, QC, bi-annually. For batched analysis in Montreal, urine samples were thawed, centrifuged (1000 g, 10 min, 21 °C), aliquoted, and frozen at − 80 °C. Specimens were measured for serum creatinine by the isotope dilution mass spectrometry (IDMS)–traceable assay, and electrolytes (potassium, magnesium, phosphorus) at the Montreal Children’s Hospital central biochemistry laboratory, Montreal, QC.
In 2019, banked urine samples were measured for TIMP-2 and IGFBP-7 at the Cincinnati Children’s Hospital Medical Center Biomarker Laboratory, OH, USA. The commercially available enzyme-linked immunosorbent assay (ELISA) kits (Duoset DY971, DY1334-05, R&D Systems, Inc., MN, USA) were used to measure TIMP-2 and IGFBP-7, per manufacturer’s instructions [27]. The inter- and intra-assay coefficients of variation were 8.6% and 5.4% for TIMP-2 and 9.9% and 4.6% for IGFBP-7, respectively. TIMP-2 and IGFBP-7 were measured once at each study timepoint and expressed as ng/ml in the primary analyses. Urine samples were thawed two times before this analysis (once upon receipt in Montreal from study sites and again for biomarker analysis). Personnel measuring biomarkers were blinded to clinical information. If the biomarker measurements were below the reportable range, the lowest reportable value was used for analyses.
Outcomes
The primary outcome was the development of AKI per the SCr criteria of the Kidney Disease: Improving Global Outcomes (KDIGO) guidelines (Online Resource 1) [28]. Since cisplatin-induced AKI is not characterized with oliguria, the KDIGO urine output criteria were not used [28]. Taking into account the known toxicity window of cisplatin from a previous study that developed and validated a cisplatin-induced AKI risk model [29], a 10-day post-cisplatin infusion period was used to assess for AKI. At the EV, baseline SCr was defined as the lowest 3-month SCr level pre-cisplatin treatment. For patients who previously received cisplatin, baseline SCr levels were determined using values measured 3 days prior to EV infusion. At LV, baseline SCr was defined as the SCr value that was lowest 3 days prior to LV. Peak SCr was defined as the highest SCr among the 10 days post-cisplatin infusion. KDIGO AKI Stage 2 or higher was defined as severe AKI [28].
Cisplatin-induced AKI is known to cause electrolyte abnormalities, notably hypophosphatemia, hypokalemia, and hypomagnesemia. As previously described, we also classified the occurrence and severity of electrolyte abnormalities by the National Cancer Institute (NCI) Common Terminology Criteria for Adverse Events (CTCAE), version 4.0 (Online Resource 2) [30]. The secondary outcome is electrolyte-AKI (eAKI), to account for electrolyte losses occurring from AKI (acknowledging that electrolyte abnormalities may occur due to non-kidney reasons). eAKI was categorized per serum magnesium, potassium, and phosphorus values (classified as grade 1 or higher abnormality) with nadir electrolyte measurements 10 days post-cisplatin (Online Resource 2) [30]. Therefore, we defined AKI in 3 ways: (i) AKI (≥ KDIGO Stage 1), primary AKI outcome; (ii) eAKI (≥ NCI CTCAE Grade 1); and (iii) composite of both (SCr + eAKI).
Statistical analysis
AKI and SCr + eAKI rates were calculated. Variables and biomarker concentrations were compared between patients who did vs. did not develop AKI, using univariable tests, including chi-square, Fisher’s exact test, two-sample t-test, the Mann–Whitney test, the Kruskal–Wallis test, and/or Spearman’s correlation test, as appropriate. The Mann–Whitney test and Spearman’s correlation (as appropriate per variable distribution) were performed to assess relationships between biomarker concentrations with age < vs. ≥ 3 years, sex, and early vs. late cisplatin infusion cycle. Biomarker concentrations were compared at different timepoints and between patients with and without AKI with the Skillings–Mack test and Wilcoxon signed-rank tests when appropriate. The area under the receiver operating characteristic curve (AUC) with 95% confidence intervals (CIs) was calculated. Sensitivity and specificity for AKI discrimination were also assessed. We defined AUC as poor (0.5–0.7), modest (0.7–0.8), good (0.8–0.9), and excellent (0.9–1.0). We compared AUCs using the DeLong test [31]. In our previous work, we described clinical prediction models for cisplatin-AKI: at EV the clinical model included age < 3 years at EV, cancer type, pre-EV estimated GFR (eGFR), and concurrent nephrotoxins [24]; at LV, the clinical model included age < 3 years at LV, cancer type, pre-LV eGFR, and cisplatin infusion dose at LV [24]. Using multiple logistic regression, post-calculation of AUC, and the DeLong test, we compared the AUC for AKI diagnosis when only using the clinical models vs. when adding the biomarker to this model (these analyses only included participants with non-missing values). We performed four pre-planned sensitivity analyses to evaluate the robustness of results: (a) expressing biomarker concentrations as corrected for urine creatinine; (b) only including participants with biomarkers available at all EV/LV timepoints; (c) only including cisplatin naïve participants at EV; and (d) only including participants who performed LV at their last cycle (i.e., excluding those for whom LV was at the second-to-last cisplatin cycle). Statistical significance was defined as P-value < 0.05 (two-tailed). Analyses were performed with STATA® version 15.1, College Station, TX, USA.
Results
Study cohort and AKI incidence
A total of 159 participants were enrolled [24]. Of the total participants, 156 participants had biomarker data available at EV, with a median (interquartile (IQR)) age of 6 (2–12) years and 78 (50%) females (Fig. 1). A total of 127 participants had biomarker data available at LV, with a median (IQR) age of 6 (2–12) years and 62 (49%) females (Fig. 1). Eighty-nine (57%) participants had their first cisplatin cycle as EV, and 67 (43%) participants had their EV as the second cycle. The median (IQR) when LV occurred is at the third (second to fourth) cisplatin cycle. At the EV, 46/156 (29%) developed AKI. At the LV, 22/127 (17%) experienced AKI. Severe AKI developed in eleven of 156 (7%) and 7/127 (6%) at the EV and LV, respectively. At the EV and LV, 30 participants out of 156 (19%) and 15 participants out of 127 (12%) had SCr + eAKI, respectively. Patients developed AKI at a median (IQR) of 4 (2–6) days post-cisplatin at EV and 3 (2–5) days post-cisplatin at LV. Table 1 displays patient characteristics at each visit stratified by AKI status.
Associations of AKI biomarkers with age, sex, and timing of cisplatin infusion
Pre-infusion biomarker concentrations were generally lower in participants aged < 3 years, but differences were only statistically significant at the pre-infusion timepoint of the EV (Online Resource 3). Conversely, at post-infusion and hospital discharge timepoints, biomarker concentrations were overall higher in participants < 3 years old (only statistically significant at the LV for TIMP-2 and TIMP-2*IGFBP-7) (Online Resource 3). Associations between biomarkers and sex were not evident (Online Resource 3). Post-infusion and discharge timepoint IGFBP-7 concentrations were positively correlated with cisplatin infusion dose at EV and LV (Spearman’s rho range: 0.19–0.32); post-infusion TIMP-2 concentration was positively correlated with cisplatin infusion dose at the LV (Spearman’s rho: 0.30; Online Resource 3). Correlations of post-infusion and discharge sample TIMP-2*IGFBP-7 concentrations with cisplatin infusion dose were only statistically significant at the LV (Spearman’s rho = 0.36 and 0.23 for post-infusion and discharge sample, respectively).
Biomarker excretion at EV and LV
Figure 2 shows that overall, urine TIMP-2, IGFBP-7, and TIMP-2*IGFBP-7 concentrations measured pre-cisplatin infusion were higher in patients who later developed AKI (vs. those with no AKI); however, these differences were only statistically significant at the EV. Post-infusion and discharge timepoint biomarkers at the EV were extremely similar between AKI and non-AKI participants. However, at the LV, post-infusion and discharge timepoint urine TIMP-2, IGFBP-7, and TIMP-2*IGFBP-7 concentrations were significantly lower in participants with vs. without AKI (Fig. 2). At the EV, urine TIMP-2, IGFBP-7, and TIMP-2*IGFBP-7 concentrations decreased significantly across timepoints from pre-infusion to post-infusion and rose from post-infusion to time of hospital discharge in participants with and those without AKI (Fig. 2). At the LV, urine TIMP-2, IGFBP-7, and TIMP-2*IGFBP-7 concentrations decreased significantly from pre-infusion to post-infusion and rose near time of hospital discharge only in participants with no AKI (Fig. 2; Online Resource 4 outlines the statistical significance from comparing biomarker levels between timepoints). Overall, biomarker concentrations were similar at the EV and the LV (Fig. 2). Biomarker excretion by AKI severity stage is displayed in Online Resource 5. Overall, biomarker concentrations were higher in participants with stage 1 or worse (Online Resource 5).
Biomarker excretion patterns surrounding cisplatin infusion at early and late cisplatin visits by AKI status. Graph shows box-and-whisker plots (the lower end of the boxes represents the 25th percentile; the upper end of the boxes represents the 75th percentile; the middle line is the median; the upper whisker outlines the upper adjacent value; the lower whisker outlines the lower adjacent value) of urine AKI biomarkers measured at three timepoints surrounding the cisplatin infusion at the early visit (left) and the late visit (right) for AKI (gray) and non-AKI (white). X-axis (timepoints): Pre: pre-infusion, before cisplatin infusion start on the day of infusion (day 1); Post: morning post-infusion (day 2); Discharge: just prior to hospital discharge (day 2–5). The number of participants analyzed for each timepoint is indicated in boxes under each bar. Outliers were excluded. The Skillings-Mack test P-value for comparing biomarker levels across the three timepoints within AKI or non-AKI groups are indicated in boxes at the top of each panel. A Urine TIMP-2 at the early visit. B Urine IGFBP-7 at the early visit. C Urine TIMP-2*IGFBP-7 at the early visit. D Urine TIMP-2 at the late visit. E Urine IGFBP-7 at the late visit. F Urine TIMP-2*IGFBP-7 at the late visit. Asterisk indicates a significant difference between AKI and non-AKI groups for that timepoint by the Mann–Whitney test (P < .05). AKI, acute kidney injury; Discharge, hospital discharge; Post, post-infusion; Pre, pre-infusion; IGFBP-7, insulin-like growth factor-binding protein-7; TIMP-2, tissue inhibitor metalloproteinase-2
Biomarker performance for AKI discrimination
At the EV, TIMP-2, IGFBP-7, and TIMP-2*IGFBP-7 measured pre-infusion had the highest AUCs for AKI diagnosis (AUCs range: 0.61–0.62; Table 2). At the LV, AKI biomarkers measured post-infusion or near hospital discharged yielded the highest AUCs for AKI diagnosis (AUCs range: 0.64–0.70; Table 2).
The AKI clinical prediction model, including demographic, pre-cisplatin, and cancer treatment variables, had an AUC (95% CI) of 0.77 (0.68–0.86) at EV and 0.80 (0.71–0.90) at LV (Table 3). The addition of biomarkers to the clinical models did not significantly improve AUCs for AKI diagnosis (Table 3).
Biomarker performance for SCr + eAKI and severe AKI discrimination
AUCs for SCr + eAKI discrimination were similar to the results above for diagnosing AKI (AUCs ranged from 0.63 to 0.65 at EV pre-infusion; AUCs ranged from 0.66 to 0.73 at post-infusion and hospital discharge of the LV; Online Resource 6). For severe AKI, AUCs ranged between 0.43 and 0.64 at EV and between 0.60 and 0.74 at LV. The highest AUC for severe AKI was near hospital discharge (Online Resource 7).
Sensitivity analyses
When biomarkers were normalized to urine creatinine, urine TIMP-2/creatinine and TIMP-2*IGFBP-7/creatinine concentrations measured post-cisplatin infusion and near time of hospital discharge at the EV and LV were significantly higher in participants with vs. without AKI (Table 4). Urine IGFBP-7/creatinine concentrations measured pre-infusion, post-cisplatin infusion, and near time of hospital discharge at the LV were significantly higher in participants with vs. those without AKI (Table 4). Overall, AUCs were similar in direction and magnitude when biomarkers were normalized to urine creatinine (vs. when not normalized to urine creatinine, as above) (Table 4).
When analyzing only participants with biomarkers measured at all the EV and LV timepoints, results with similar direction and magnitude were found, except that biomarker concentrations measured post-cisplatin infusion and near time of hospital discharge at the LV were significantly higher in participants with vs. those without AKI (Online Resource 8).
Results were also similar when only evaluating cisplatin naïve participants at the EV, and when analyzing only participants whose LV was the last cisplatin cycle (Online Resource 9). The exception was that biomarker concentrations measured post-cisplatin infusion and near time of hospital discharge at the LV were significantly higher in participants with vs. without AKI (Online Resource 9).
Discussion
This is the first study to assess TIMP-2*IGFBP-7 at detecting AKI in children treated with cisplatin to our knowledge. It is also one of the largest cohort analyses of TIMP-2*IGFBP-7 in children in general. Urine concentrations of cell cycle arrest biomarkers measured pre-cisplatin infusion at the EV (the first or second cisplatin cycle) were higher in patients with AKI compared to those without. Biomarkers measured post-cisplatin infusion and near time of hospital discharge at the EV and LV (one of the last cisplatin cycles) were lower in patients with AKI relative to those without. Biomarker excretion patterns changed when biomarker values were normalized to urine creatinine; values were overall higher in patients with AKI compared to without. We found urine TIMP-2*IGFBP-7 had poor to modest performance in diagnosing AKI post-cisplatin and did not add predictive value compared to clinical variables alone.
Urine biomarker concentrations measured pre-cisplatin infusion at the EV were diagnostic of AKI and were higher in patients with AKI compared to without; however, AUCs for discrimination were rather low. One study of 32 adults with cancer treated with cisplatin or carboplatin also reported that patients with AKI had high levels of urinary TIMP-2*IGFBP-7 pre-chemotherapy compared to patients without AKI (AUC (95% CI): 0.86 (0.73–0.98)) [16]. Some patients in our study may be predisposed to developing AKI, from having subclinical AKI before cisplatin administration. Our findings could also indicate that patients with AKI already had tubular stress before cisplatin administration, perhaps increasing vulnerability to further cisplatin-induced kidney injury. At the LV, patients with and without AKI had similar urine biomarker levels.
We observed that biomarker concentrations measured post-cisplatin infusion were lower in patients with AKI vs. no AKI at the LV. One potential explanation is that perhaps the production of TIMP-2 and IGFBP-7 confers protection against tubular injury [32]. Therefore, a lower production of TIMP-2 and IGFBP-7 in tubular cells may contribute to susceptibility for tubular injury [32]. However, when biomarkers were normalized to urine creatinine, we saw different biomarker excretion patterns. We found patients with AKI at higher biomarker levels compared to patients without AKI, possibly due to urine creatinine concentration being relatively lower. However, AUCs remained similar. In a previous analysis of the same cohort, we showed that our findings did not markedly differ when using absolute or normalized values for urine NGAL and KIM-1 [26]. Several AKI biomarker studies have reported that their findings were not affected by urine creatinine normalization (results were similar) [33–37]. However, few studies have evaluated urine creatinine normalization for urine TIMP-2*IGFBP-7 since this biomarker was approved by the FDA without urine creatinine correction [19, 20].
Normalizing biomarker concentrations to urine creatinine concentration can be non-ideal due to the non-steady state of creatinine balance in patients with AKI. However, normalizing biomarkers to urine creatinine allows accounting for hydration status, creatinine clearance, and urine flow. Especially in patients treated with cisplatin who receive generous intravenous fluids, hydration status may influence toxicity levels, resulting in unexpected biomarker concentrations. This is still an area of debate [38, 39]. Our results indicate it might be important to report urine TIMP-2 and IGFBP-7 using raw concentrations and values normalized to urinary creatinine in children receiving cisplatin until further research can determine which of these methods is more strongly associated with patient outcomes.
There is a paucity of studies evaluating urine TIMP-2 and IGFBP-7 in adults, and no studies have been conducted in children treated with cisplatin. In the study of 32 adults with cancer treated with cisplatin or carboplatin described above, urine TIMP-2*IGFBP-7 was significantly increased in 4 participants who developed AKI at 12 h post-chemotherapy [16]. Urine TIMP-2*IGFBP-7 measured within 12 h post-chemotherapy was predictive of cisplatin-associated AKI (AUC (95% CI): 0.92 (0.80–1.00)) [16]. In a study of 45 adults with lung cancer treated with cisplatin, urine TIMP-2*IGFBP-7 concentrations were similar between patients with vs. without AKI [40], and urine TIMP-2*IGFBP-7 measured 24 h post-cisplatin was not predictive of cisplatin-associated AKI (AUC (95% CI): 0.46 (0.26–0.67)) [40]. Given the limited data in pediatrics, it is worth reviewing existing published data on TIMP-2*IGFBP-7 in pediatric AKI. In a study of 133 hospitalized children (not treated with cisplatin) who had established AKI, elevated urine TIMP-2*IGFBP-7 levels predicted 30-day mortality and the need for kidney replacement therapy [41]. In a prospective study of 144 critically ill children, urine IGFBP-7 measured within 24 h of ICU admission was predictive of severe AKI [42]. In a prospective study of 237 critically ill neonates, urinary TIMP-2*IGFBP-7 was associated with AKI and discriminated for severe AKI (threshold value of 0.045 (ng/ml)2/1000 was thought to be clinically significant) [17]. In several studies of children undergoing cardiac surgery, early post-operative urinary TIMP-2*IGFBP-7 concentrations were associated with and predicted AKI development [13, 27, 43]; however, another study in a similar population found that TIMP-2*IGFBP-7 was not associated with AKI, dialysis, or death [32]. In a prospective study of noncritically ill children treated with aminoglycosides, our research group showed urine TIMP-2*IGFBP-7 levels measured 2 days prior to AKI onset were higher in patients with AKI compared to those without [44]. Urine TIMP-2*IGFBP-7 measured 2 days prior to AKI onset resulted in an AUC (95% CI) of 0.73 (0.58–0.88) on predicting AKI [44]. In the present study, we found urine TIMP-2, IGFBP-7, and TIMP-2*IGFBP-7 were poor to modest for AKI discrimination. One reason for the lack of AKI discrimination by TIMP-2 and IGFBP-7 could be the relatively late timing (post-infusion sample ~ 18–24 h post-infusion) of measurements we performed. In the pediatric cardiac surgery setting, urinary TIMP-2*IGFBP-7 appears to peak approximately 6–12 h after surgery [27, 43]. Perhaps earlier measurements would be better at discriminating for AKI post-cisplatin. Another possible explanation for the poor discrimination we found was that changes in SCr may not be an ideal way to define AKI in this patient population; future work should determine if other filtration markers (e.g., cystatin C) may be better to define the reference standard for the presence of AKI. Future research with a larger prospective cohort should investigate the urinary biomarkers’ temporal expression pattern for early prediction and detection of AKI immediately post-cisplatin in children to understand the ideal timing of biomarker measurement.
The optimal TIMP-2*IGFBP-7 concentration cut-offs we identified for AKI discrimination were much lower than what has been proposed in the literature (cut-off at 0.3 (ng/ml)2/1000 for AKI in critically ill adults) [12, 16]. However, most cut-offs were established in ICU or cardiac surgery cohorts, with a greater probability of having higher multi-organ and acute illness severity and more infections; children receiving cisplatin infusions are generally well (i.e., able to tolerate cisplatin) on the day they are receiving cisplatin. Several studies in critically ill adults have established high specificity (95%) with a cut-off of 2.0 (ng/ml)2/1000 for AKI prediction [12, 15]. Studies of children who underwent cardiac surgery established a cut-off value of 0.7 (ng/ml)2/ [13]. In critically ill neonates, an optimal cut-off value of 0.045 was identified to discriminate for severe AKI [17]. In our study of children treated with cisplatin, we found that much lower urine TIMP-2*IGFBP-7 concentration thresholds (∼ 0.002–0.2 (ng/ml)2/1000) were optimal for AKI diagnosis. Additionally, the urine TIMP-2*IGFBP-7 concentrations reported in this study are much lower than those reported in healthy children (median (IQR): 0.27 (0.10–0.49)) [41]. Differences in optimal biomarker thresholds may be due to differences in injury mechanisms, age groups, and/or illness severity and nutritional status [13, 41]. Our study indicates a lower threshold for urine TIMP-2*IGFBP-7 is likely needed for cisplatin-treated children and highlights the crucial importance of evaluating and validating biomarkers in specific patient populations prior to widespread use.
This study has multiple strengths, including its prospective cohort design. Evaluating AKI biomarkers at several timepoints pre- and post-cisplatin was allowed by a rigorous protocol of collecting specimens and blinded measurements of biomarkers. We enrolled a relatively large cohort of children with cancer receiving cisplatin.
This study also has limitations. Biomarkers were not measured in real-time as would be done in clinical practice. The effect of extended storage duration at − 80 °C and freeze–thaw cycles on urinary TIMP-2 and IGFBP-7 stability is unknown at the present time. It is possible that the poor performance of urinary cell cycle arrest biomarkers in the present study may be due to the instability of these biomarkers during prolonged freezing, and therefore, further investigations are necessary to determine their ability as biomarkers of AKI. Our findings are not applicable to non-pediatric cancer populations. Another limitation for our study is the inability to fully explore effects of inter-patient and intra-patient physiologic variability, outside of known measurement characteristics (described in the “Methods” section). Due to the relatively low sample size and limited specimen volumes, sensitivity analysis to explore variability within our cohort was limited. Studies with larger sample size should evaluate the effect of age, sex, cisplatin dose, duration, and other nephrotoxic medications dosage on biomarkers with multivariable analyses. Also, a SCr-based definition of AKI was used in this study despite known limitations of creatinine. It is likely that patients with mild structural kidney injury were missed and misclassified as non-AKI patients. This issue remains a problem in all AKI biomarker studies—using a “bronze” reference standard to validate newer biomarkers. Another limitation of our study is the heterogeneity of the patient population, while they were all children undergoing cisplatin treatment (thus, less heterogeneous than an ICU population), the cohort comprised patients with different cancer diagnoses and cancer treatment protocols. The cohort also had a low number of patients with severe AKI, limiting the ability to investigate biomarker levels in patients with more severe tubular injury. Additionally, because patients with cancer may have decreased muscle mass, especially later in cancer therapy, SCr to define AKI may be even more problematic. Patients with subclinical AKI with an increased risk of adverse events may be recognized with early biomarker measurements, even without SCr rise. Future studies should determine the effect of subclinical AKI (those with elevated biomarkers, with no SCr rise). In addition, we did not collect daily urine samples. To balance feasibility and specimen collection, urine AKI biomarkers were at most assessed once per day. Future studies should evaluate kinetics of urine TIMP-2 and IGFBP-7 in the setting of cisplatin nephrotoxicity.
Associations between urinary cell cycle arrest biomarkers and AKI in children treated with cisplatin are only briefly described and characterized in research. We found urine TIMP-2, IGFBP-7, and TIMP-2*IGFBP-7 were poor to modest biomarkers of cisplatin-associated AKI in children, and normalizing the biomarkers to urine creatinine changed excretion patterns. Given the availability of a commercial test for TIMP-2*IGFBP-7, additional multi-center studies are needed to further explore and assess the role of and understand the usefulness of urine TIMP-2 and IGFBP-7 for AKI prediction in children receiving chemotherapy before being adopted for this use. Future research should determine whether raw biomarker values or biomarker values normalized to urinary creatinine are more strongly associated with patient outcomes and whether patient management improves by incorporating urinary biomarkers in AKI definition.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Oeffinger KC, Eshelman DA, Tomlinson GE, Buchanan GR, Foster BM (2000) Grading of late effects in young adult survivors of childhood cancer followed in an ambulatory adult setting. Cancer 88:1687–1695
Bottomley SJ, Kassner E (2003) Late effects of childhood cancer therapy. J Pediatr Nurs 18:126–133
Oeffinger KC, Mertens AC, Sklar CA, Kawashima T, Hudson MM, Meadows AT, Friedman DL, Marina N, Hobbie W, Kadan-Lottick NS, Schwartz CL, Leisenring W, Robison LL, Childhood Cancer Survivor Study (2006) Chronic health conditions in adult survivors of childhood cancer. N Engl J Med 355:1572–1582
Fujieda M, Matsunaga A, Hayashi A, Tauchi H, Chayama K, Sekine T (2009) Children’s toxicology from bench to bed--drug-induced renal injury (2): nephrotoxicity induced by cisplatin and ifosfamide in children. J Toxicol Sci 34(Suppl 2):SP251–S257
Ariceta G, Rodriguez-Soriano J, Vallo A, Navajas A (1997) Acute and chronic effects of cisplatin therapy on renal magnesium homeostasis. Med Pediatr Oncol 28:35–40
Goren MP, Wright RK, Horowitz ME (1986) Cumulative renal tubular damage associated with cisplatin nephrotoxicity. Cancer Chemother Pharmacol 18:69–73
McMahon KR, Harel-Sterling M, Pizzi M, Huynh L, Hessey E, Zappitelli M (2018) Long-term renal follow-up of children treated with cisplatin, carboplatin, or ifosfamide: a pilot study. Pediatr Nephrol 33:2311–2320
Skinner R, Parry A, Price L, Cole M, Craft AW, Pearson AD (2009) Persistent nephrotoxicity during 10-year follow-up after cisplatin or carboplatin treatment in childhood: relevance of age and dose as risk factors. Eur J Cancer 45:3213–3219
Skinner R, Pearson AD, Price L, Coulthard MG, Craft AW (1992) The influence of age on nephrotoxicity following chemotherapy in children. Br J Cancer 18:S30–S35
Jones CA, McQuillan GM, Kusek JW, Eberhardt MS, Herman WH, Coresh J, Salive M, Jones CP, Agodoa LY (1998) Serum creatinine levels in the US population: third National Health and Nutrition Examination Survey. Am J Kidney Dis 32:992–999
Dharnidharka VR, Kwon C, Stevens G (2002) Serum cystatin C is superior to serum creatinine as a marker of kidney function: a meta-analysis. Am J Kidney Dis 40:221–226
Kashani K, Al-Khafaji A, Ardiles T, Artigas A, Bagshaw SM, Bell M, Bihorac A, Birkhahn R, Cely CM, Chawla LS, Davison DL, Feldkamp T, Forni LG, Gong MN, Gunnerson KJ, Haase M, Hackett J, Honore PM, Hoste EA, Joannes-Boyau O, Joannidis M, Kim P, Koyner JL, Laskowitz DT, Lissauer ME, Marx G, McCullough PA, Mullaney S, Ostermann M, Rimmele T, Shapiro NI, Shaw AD, Shi J, Sprague AM, Vincent JL, Vinsonneau C, Wagner L, Walker MG, Wilkerson RG, Zacharowski K, Kellum JA (2013) Discovery and validation of cell cycle arrest biomarkers in human acute kidney injury. Crit Care 17:R25
Meersch M, Schmidt C, Van Aken H, Rossaint J, Gorlich D, Stege D, Malec E, Januszewska K, Zarbock A (2014) Validation of cell-cycle arrest biomarkers for acute kidney injury after pediatric cardiac surgery. PLoS One 9:e110865
Bihorac A, Chawla LS, Shaw AD, Al-Khafaji A, Davison DL, Demuth GE, Fitzgerald R, Gong MN, Graham DD, Gunnerson K, Heung M, Jortani S, Kleerup E, Koyner JL, Krell K, Letourneau J, Lissauer M, Miner J, Nguyen HB, Ortega LM, Self WH, Sellman R, Shi J, Straseski J, Szalados JE, Wilber ST, Walker MG, Wilson J, Wunderink R, Zimmerman J, Kellum JA (2014) Validation of cell-cycle arrest biomarkers for acute kidney injury using clinical adjudication. Am J Respir Crit Care Med 189:932–939
Hoste EA, McCullough PA, Kashani K, Chawla LS, Joannidis M, Shaw AD, Feldkamp T, Uettwiller-Geiger DL, McCarthy P, Shi J, Walker MG, Kellum JA (2014) Derivation and validation of cutoffs for clinical use of cell cycle arrest biomarkers. Nephrol Dial Transplant 29:2054–2061
Schanz M, Hoferer A, Shi J, Alscher MD, Kimmel M (2017) Urinary TIMP2IGFBP7 for the prediction of platinum-induced acute renal injury. Int J Nephrol Renovasc Dis 10:175–181
Chen J, Sun Y, Wang S, Dai X, Huang H, Bai Z, Li X, Wang J, Li Y (2019) The effectiveness of urinary TIMP-2 and IGFBP-7 in predicting acute kidney injury in critically ill neonates. Pediatr Res 87:1052–1059
Abitbol CL, Moxey-Mims M (2016) Chronic kidney disease: low birth weight and the global burden of kidney disease. Nat Rev Nephrol 12:199–200
Ronco C, Rizo-Topete L, Serrano-Soto M, Kashani K (2017) Pro: prevention of acute kidney injury: time for teamwork and new biomarkers. Nephrol Dial Transplant 32:408–413
Department of Health and Human Services (2014) US Food and Drug Administration. Letter to Astute Medical, Inc
Yang Q-h, Liu D-w, Long Y, Liu H-z, Chai W-z, Wang X-T (2009) Acute renal failure during sepsis: potential role of cell cycle regulation. J Infect 58:459–464
Witzgall R, Brown D, Schwarz C, Bonventre JV (1994) Localization of proliferating cell nuclear antigen, vimentin, c-Fos, and clusterin in the postischemic kidney. Evidence for a heterogenous genetic response among nephron segments, and a large pool of mitotically active and dedifferentiated cells. J Clin Invest 93:2175–2188
Rodier F, Campisi J, Bhaumik D (2007) Two faces of p53: aging and tumor suppression. Nucleic Acids Res 35:7475–7484
McMahon KR, Rassekh SR, Schultz KR, Blydt-Hansen T, Cuvelier GDE, Mammen C, Pinsk M, Carleton BC, Tsuyuki RT, Ross CJD, Palijan A, Huynh L, Yordanova M, Crepeau-Hubert F, Wang S, Boyko D, Zappitelli M, Applying Biomarkers to Minimize Long-term Effects of Childhood/Adolescent Cancer Treatment Research Study Group (2020) Epidemiologic characteristics of acute kidney injury during cisplatin infusions in children treated for cancer. JAMA Netw Open 3:e203639
McMahon KR, Rod Rassekh S, Schultz KR, Pinsk M, Blydt-Hansen T, Mammen C, Tsuyuki RT, Devarajan P, Cuvelier GD, Mitchell LG, Baruchel S, Palijan A, Carleton BC, Ross CJ, Zappitelli M, Applying Biomarkers to Minimize Long-Term Effects of Childhood/Adolescent Cancer Treatment Research Group (2017) Design and methods of the Pan-Canadian Applying Biomarkers to Minimize Long-Term Effects of Childhood/Adolescent Cancer Treatment (ABLE) nephrotoxicity study: a prospective observational cohort study. Can J Kidney Health Dis 4:2054358117690338
McMahon KR, Chui H, Rassekh SR, Schultz KR, Blydt-Hansen TD, Mammen C, Pinsk M, Cuvelier GDE, Carleton BC, Tsuyuki RT, Ross CJD, Devarajan P, Huynh L, Yordanova M, Crepeau-Hubert F, Wang S, Cockovski V, Palijan A, Zappitelli M (2021) Urine neutrophil gelatinase-associated lipocalin and kidney injury molecule-1 to detect pediatric cisplatin-associated acute kidney injury. Kidney 360(3):37–50. https://doi.org/10.34067/KID.0004802021
Dong L, Ma Q, Bennett M, Devarajan P (2017) Urinary biomarkers of cell cycle arrest are delayed predictors of acute kidney injury after pediatric cardiopulmonary bypass. Pediatr Nephrol 32:2351–2360
Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group (2012) KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl 2:1–138
Motwani SS, McMahon GM, Humphreys BD, Partridge AH, Waikar SS, Curhan GC (2018) Development and validation of a risk prediction model for acute kidney injury after the first course of cisplatin. J Clin Oncol 36:682–688
(2010) Common terminology criteria for adverse events (CTCAE), Version 4.0. National Institutes of Health National Cancer Institute, pp 1–194
DeLong ER, DeLong DM, Clarke-Pearson DL (1988) Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44:837–845
Bojan M, Pieroni L, Semeraro M, Froissart M (2020) Cell-cycle arrest biomarkers: usefulness for cardiac surgery-related acute kidney injury in neonates and infants. Pediatr Crit Care Med 21:563–570
Parikh CR, Devarajan P, Zappitelli M, Sint K, Thiessen-Philbrook H, Li S, Kim RW, Koyner JL, Coca SG, Edelstein CL, Shlipak MG, Garg AX, Krawczeski CD, TRIBE-AKI Consortium (2011) Postoperative biomarkers predict acute kidney injury and poor outcomes after pediatric cardiac surgery. J Am Soc Nephrol 22:1737–1747
Parikh CR, Thiessen-Philbrook H, Garg AX, Kadiyala D, Shlipak MG, Koyner JL, Edelstein CL, Devarajan P, Patel UD, Zappitelli M, Krawczeski CD, Passik CS, Coca SG, TRIBE-AKI Consortium (2013) Performance of kidney injury molecule-1 and liver fatty acid-binding protein and combined biomarkers of AKI after cardiac surgery. Clin J Am Soc Nephrol 8:1079–1088
Zappitelli M, Washburn KK, Arikan AA, Loftis L, Ma Q, Devarajan P, Parikh CR, Goldstein SL (2007) Urine neutrophil gelatinase-associated lipocalin is an early marker of acute kidney injury in critically ill children: a prospective cohort study. Crit Care 11:R84
Mishra J, Dent C, Tarabishi R, Mitsnefes MM, Ma Q, Kelly C, Ruff SM, Zahedi K, Shao M, Bean J, Mori K, Barasch J, Devarajan P (2005) Neutrophil gelatinase-associated lipocalin (NGAL) as a biomarker for acute renal injury after cardiac surgery. Lancet 365:1231–1238
Han WK, Waikar SS, Johnson A, Betensky RA, Dent CL, Devarajan P, Bonventre JV (2008) Urinary biomarkers in the early diagnosis of acute kidney injury. Kidney Int 73:863–869
Goldstein SL (2010) Urinary kidney injury biomarkers and urine creatinine normalization: a false premise or not? Kidney Int 78:433–435
Ralib AM, Pickering JW, Shaw GM, Devarajan P, Edelstein CL, Bonventre JV, Endre ZH (2012) Test characteristics of urinary biomarkers depend on quantitation method in acute kidney injury. J Am Soc Nephrol 23:322–333
Toprak Z, Cebeci E, Helvaci SA, Toprak ID, Kutlu Y, Sakin A, Tukek T (2017) Cisplatin nephrotoxicity is not detected by urinary cell-cycle arrest biomarkers in lung cancer patients. Int Urol Nephrol 49:1041–1047
Westhoff JH, Tonshoff B, Waldherr S, Poschl J, Teufel U, Westhoff TH, Fichtner A (2015) Urinary tissue inhibitor of metalloproteinase-2 (TIMP-2) * insulin-like growth factor-binding protein 7 (IGFBP7) predicts adverse outcome in pediatric acute kidney injury. PLoS One 10:e0143628
Bai Z, Fang F, Xu Z, Lu C, Wang X, Chen J, Pan J, Wang J, Li Y (2018) Serum and urine FGF23 and IGFBP-7 for the prediction of acute kidney injury in critically ill children. BMC Pediatr 18:192
Gist KM, Goldstein SL, Wrona J, Alten JA, Basu RK, Cooper DS, Soranno DE, Duplantis J, Altmann C, Gao Z, Faubel S (2017) Kinetics of the cell cycle arrest biomarkers (TIMP-2*IGFBP-7) for prediction of acute kidney injury in infants after cardiac surgery. Pediatr Nephrol 32:1611–1619
Chui H, Caldwell J, Yordanova M, Cockovski V, Fredric D, Harel-Sterling M, Haasz M, Al-Ismaili Z, Pizzi M, Ma Q, Devarajan P, Goldstein SL, Zappitelli M (2020) Tubular injury and cell-cycle arrest biomarkers to predict acute kidney injury in noncritically ill children receiving aminoglycosides. Biomark Med 14:879–894
Acknowledgements
We give our sincerest and deepest gratitude to all of the study participants and their families. We acknowledge the work of the following clinical research personnel for their involvement in the study: Pina Giuliano, Karen Mazil, Jessica Scheidl, Susan Talmey and Tao Wang (Alberta Children’s Hospital, Calgary, Alberta, Canada); Octavia Choi, Cecilia Crosby, Jessica Davis, Fatima Dharsee, Mateo Farfan, Rohan Kakkar, Nicole Kelly, Alecia Lim, Alicia Oger, Ritu Ratan, Jennifer Sergeant and Grace Tam (British Columbia Children’s Hospital, Vancouver, British Columbia, Canada); Nancy Coreas, Megan Friesen, Rebekah Hiebert, Jodi Karwacki, Krista Mueller, Ashley Ouelette and Kiera Unger (CancerCare Manitoba, Winnipeg, Manitoba, Canada); Barbara Desbiens, Melanie Ernst, Marie-Christine Gagnon and Nadine Roy (Centre Hospitalier Universitaire de Québec—Université Laval, Quebec, Quebec, Canada); Ernestine Chablis, Bianka Courcelle, Angélique Courtade, Catherine Desjean, Marc-Antoine Nadeau, Marie Saint-Jacques, Martine Therrien and Caroline Tra (Centre Hospitalier Universitaire Sainte-Justine, Montreal, Quebec, Canada); Sandra Blamires, Tianna Deluzio, Becky Malkin, Mariam Mikhail and Leslie Paddock (Children’s Hospital: London Health Sciences Centre, London, Ontario, Canada); Nathan Adolphe, Brooke Bowerman, Isabelle Laforest, Oluwatoni Adeniyi, Kelly-Ann Ramakko and Jenna-Lee Tremblay (Children’s Hospital of Eastern Ontario, Ottawa, Ontario, Canada); Mandy Bouchard (IWK Health Centre, Halifax, Nova Scotia, Canada); Shawde Harris and Rachel Simpson (McMaster Children’s Hospital, Hamilton, Ontario, Canada); Anelise Espirito Santo, Jackie Girgis, Dominique Lafrenière, Martine Nagy and Sandra Pepin (Montreal Children’s Hospital, MUHC, Montreal, Quebec, Canada); Linda Churcher, Dianne Cortez, Kevin Dietrich, Brenda Ennis, Nicholas Howe, Crystal Lefebvre, Nicole Orrell and Holly Sykora (Stollery Children’s Hospital, Edmonton, Alberta, Canada); Abongnwen Abianui, Rachel Alix, Beren Avci, Aparna Bhan, Eric Lee, Darshika Mistry, Niwethaa Nadesan, Nicholas Pasquale, Subitha Rajakumaran, Grace Tran, Megan Wood and Elyze Yamasaki (The Hospital for Sick Children, Toronto, Ontario, Canada). Thank you to Debbie Boyko and the EPICORE Centre team (Departments of Pharmacology and Medicine, University of Alberta, Edmonton, Canada) for data support, entry, queries and management. We would like to thank Anat Halevy, MSc (University of British Columbia, Vancouver, Canada) for the ABLE Study support. Thank you to Michael Pizzi and Olivier Pouliot (Research Institute of the MUHC team members) for their contributions. We also thank Jasmine Lee and Asaf Lebel (Hospital for Sick Children, Toronto, Canada) for their contributions. Thank you to Ma Qing and Michael Bennett (Cincinnati Children’s Hospital Medical Center) for their help with biomarker measurements. All individuals were compensated for their time.
ABLE Study Investigators: Sylvain Baruchel, MD (Hospital for Sick Children, Toronto, Canada), Eric Bouffet, MD (Hospital for Sick Children, Toronto, Canada), Tom Blydt-Hansen MD (British Columbia Children’s Hospital, Vancouver, Canada), Bruce C. Carleton, PharmD (BC Children’s Hospital Research Institute, Vancouver, Canada), Geoff D. E. Cuvelier, MD (CancerCare Manitoba, Winnipeg, Canada), Sunil Desai, MBChB (University of Alberta, Edmonton, Canada), Prasad Devarajan, MD (Cincinnati Children’s Hospital Medical Center, Cincinnati, USA), Conrad Fernandez, MD (IWK Health Centre, Halifax, Canada), Adam Fleming, MD (McMaster Children’s Hospital at Hamilton Health Sciences, Hamilton, Canada), Paul Gibson, MD (Children’s Hospital: London Health Sciences Centre, London, Canada), Caroline Laverdière, MD (Centre Hospitalier Universitaire Sainte-Justine, Montreal, Canada), Victor Lewis, MD (Alberta Children’s Hospital, Calgary, Canada), Cherry Mammen, MD, MHSc (British Columbia Children’s Hospital, Vancouver, Canada), Mary L. McBride, MSc (University of British Columbia, Vancouver, Canada), Bruno Michon, MD (Centre Hospitalier Universitaire de Québec—Université Laval, Quebec Canada), Lesley G. Mitchell, MSc (University of Alberta, Alberta, Canada), Maury Pinsk, MD (University of Manitoba, Winnipeg, Canada), Raveena Ramphal, MBChB (Children’s Hospital of Eastern Ontario, Ottawa, Canada), Shahrad Rod Rassekh MD, MHSc (British Columbia Children’s Hospital, Vancouver, Canada), Colin J. D. Ross, PhD (BC Children’s Hospital Research Institute, Vancouver, Canada), Christine Sabapathy, MD (MUHC, Montreal, Canada), Kirk R. Schultz, MD (British Columbia Children’s Hospital, Vancouver, Canada), Ross T. Tsuyuki PharmD MSc (University of Alberta, Edmonton, Canada), Michael Zappitelli, MD, MSc (Toronto Hospital for Sick Children, Toronto, Canada) and Alexandra Zorzi, MD (Children’s Hospital: London Health Sciences Centre, London, Canada).
Funding
This work was supported by a Team Grant from the Canadian Institutes of Health Research (CIHR) and its partners, the Canadian Cancer Society, the C17 Research Network, the Garron Family Cancer Center at the Hospital for Sick Children, and the Pediatric Oncology Group of Ontario, which was awarded to Kirk R. Schultz, Sylvain Baruchel, Mary L. McBride, Lesley G. Mitchell, S. Rod Rassekh, Ross T. Tsuyuki and Michael Zappitelli. A Fonds de recherche du Québec—Santé (FRQS) Doctoral Training Bursary awarded to Kelly R. McMahon also helped support this work. Colin J. Ross was supported by a Michael Smith Foundation for Health Research Scholar Award. Prasad Devarajan is supported by grant #P50 DK096418 from the National Institutes of Health (NIH).
Author information
Authors and Affiliations
Consortia
Contributions
Conceptualization: K. McMahon, S. R. Rassekh, K. Schultz, T. Blydt-Hansen, C. Mammen, M. Pinsk, G. Cuvelier, B. Carleton, R. Tsuyuki, C. Ross, A. Palijan, M. Zappitelli. Methodology: H. Chui, K. McMahon, S. R. Rassekh, T. Blydt-Hansen, C. Mammen, M. Pinsk, B. Carleton, R. Tsuyuki, P. Devarajan, L. Huynh, M. Yordanova, F. Crépeau-Hubert, V. Cockovski, A. Palijan, M. Zappitelli. Formal analysis and investigation: H. Chui, K. McMahon, S. Wang, M. Zappitelli. Writing—original draft preparation: H. Chui, K. McMahon, M. Zappitelli. Writing—review and editing: H. Chui, K. McMahon, S. R. Rassekh, K. Schultz, T. Blydt-Hansen, C. Mammen, M. Pinsk, G. Cuvelier, B. Carleton, R. Tsuyuki, C. Ross, P. Devarajan, L. Huynh, M. Yordanova, F. Crépeau-Hubert, S. Wang, V. Cockovski, A. Palijan, M. Zappitelli. Funding acquisition: K. McMahon, S. R. Rassekh, K. Schultz, T. Blydt-Hansen, G. Cuvelier, R. Tsuyuki, C. Ross, M. Zappitelli. Resources: S. R. Rassekh, K. Schultz, R. Tsuyuki, P. Devarajan, A. Palijan, M. Zappitelli. Supervision: K. McMahon, S. R. Rassekh, K. Schultz, G. Cuvelier, R. Tsuyuki, P. Devarajan, S. Wang, A. Palijan, M. Zappitelli.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in accordance with the ethical standards of the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. Approval was granted by the Pediatrics Research Ethics Board of the McGill University Health Centre (12–301-PED).
Consent to participate
Informed consent and assent if appropriate were obtained from all individual participants included in the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chui, H., McMahon, K.R., Rassekh, S.R. et al. Urinary TIMP-2*IGFBP-7 to diagnose acute kidney injury in children receiving cisplatin. Pediatr Nephrol 39, 269–282 (2024). https://doi.org/10.1007/s00467-023-06007-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-023-06007-8