Abstract
Background
X-linked hypophosphatemic rickets (XLH) is the most common cause of inherited rickets. Historically, XLH was treated with oral phosphate and calcitriol (conventional treatment). Burosumab, a fibroblast growth factor 23 (FGF-23) monoclonal antibody, was approved by the United States Food and Drug Administration (FDA) in 2018 for XLH treatment. Nevertheless, conventional treatment of XLH continues to be recommended by some specialists due to lack of published experience with burosumab in the clinical setting. We compared laboratory and radiographic changes observed following transition from conventional therapy to burosumab in pediatric XLH patients as part of routine care.
Methods
This retrospective single-center study identified and retroactively studied twelve patients aged 1–18 years old with XLH previously treated with conventional therapy and transitioned to burosumab. Laboratory studies and radiographs were obtained routinely as standard of care during two treatment periods: (1) conventional therapy and (2) burosumab treatment. Laboratory values and radiologic rickets severity scores were compared between periods.
Results
All laboratory values demonstrated improvement following 1 month of burosumab treatment, findings which were sustained over the 2-year study period. Rickets severity scores and height z-scores also improved with burosumab. There were no serious adverse events with burosumab, and adverse events overall were very infrequent and mild. One patient developed an asymptomatic mild elevation of serum phosphate while taking burosumab resulting in a temporary pause in therapy.
Conclusions
Safety and effectiveness of burosumab in treatment of XLH were demonstrated as burosumab yielded statistically significant improvement in laboratory and radiographic markers of rickets and height compared to conventional therapy.
Graphical abstract
A higher resolution version of the Graphical abstract is available as Supplementary information.

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rickets is a systemic disorder of mineral imbalance manifested by poor mineralization of the physes. Because of the involvement of the growth plate, rickets is unique to growing children who have not yet reached skeletal maturity [1]. Affected children commonly present clinically with genu varum or rarely genu valgum and often have additional skeletal deformities which may include short stature, craniotabes, craniosynostosis, wrist flaring, frontal bossing, and expansion of the costochondral junction [2]. These patients concurrently develop osteomalacia which can persist following closure of the physes and may lead to lifelong physical disability and bone pain.
Rickets is caused by a total body deficiency of calcium or phosphorus, which denies growing bone the substrates it requires in order to properly mineralize and ossify. Rickets can either be nutritional in nature, due to a dietary insufficiency of calcium, phosphorus, or vitamin D, or due to genetic disorders that cause disturbances in normal mineral homeostasis. The most common genetic form of rickets is X-linked hypophosphatemia (XLH), a condition caused by excessive urinary phosphate losses due to pathogenic variants in the PHEX gene [3, 4]. XLH is characterized by elevated urinary phosphate excretion due to inappropriately elevated circulating FGF-23. Elevated urinary phosphate excretion results in hypophosphatemia and rickets. Elevated alkaline phosphatase levels are observed and correlate with the degree of rickets. Over time, XLH patients frequently develop hyperparathyroidism due to the role of FGF-23 as a down-regulator of 1-α-hydroxylase activity and therapeutic phosphate supplementation [5].
Historical treatment of XLH has been with oral phosphate supplementation along with calcitriol (conventional therapy). With this therapy, children show signs of improvement, but correction of the rickets is limited; despite conventional therapy, children often require surgical intervention to address genu varum or valgum and typically do not reach their full height potential [3]. Conventional therapy can normalize the serum phosphate level; however, because of the ongoing urinary phosphate losses, significant side effects such as secondary hyperparathyroidism and nephrocalcinosis are often observed when targeting normal serum phosphate levels [6].
In April 2018, burosumab, a humanized monoclonal antibody targeting FGF-23, was approved for the treatment of XLH [7]. Clinical trials demonstrated improvements in laboratory and radiographic markers of XLH in patients treated with burosumab versus conventional therapy, but by definition these studies were safety and efficacy studies conducted in a controlled fashion with significant oversight to ensure adherence and follow-up [8,9,10]. Despite the superior efficacy of burosumab compared with conventional therapy demonstrated in clinical trials, utilization and promotion of conventional therapy continues in part due to lack of published evidence of safety and effectiveness in real-world settings [11]. We aimed, therefore, to assess the effectiveness of burosumab in a real-world clinical pediatric practice.
Methods
This retrospective study was conducted by identifying all pediatric patients (< 21 years of age) receiving care at the University of Wisconsin Hospitals and Clinics diagnosed with XLH and treated with burosumab between April 1, 2018, and May 31, 2020. The XLH diagnosis was confirmed in all patients by identification of a pathogenic variant in PHEX.
Prior to starting burosumab, all patients were treated with oral phosphate and calcitriol. Following a diagnosis of XLH, patients were initially prescribed 20–30 mg/kg/day of elemental phosphorus given four times daily and calcitriol 20 ng/kg/day given once or twice daily. Phosphate and calcitriol doses over time were adjusted with a goal of maximizing medical therapy without causing side effects including laboratory abnormalities (hypercalciuria, hypercalcemia, or hyperparathyroidism) or gastrointestinal symptoms; doses varied and were tailored to the patient’s lab values, radiographs, tolerance of therapy, and adherence to the medication regimen. Laboratory studies were obtained approximately every 6 months which included serum phosphate (mg/dL), creatinine (mg/dL), alkaline phosphatase (U/L), and intact parathyroid hormone (PTH) (pg/mL), as well as urine phosphate (mg/dL), calcium (mg/dL), and creatinine (mg/dL). Fractional excretion of phosphate (FEphos) was calculated as (Phosurine /Phosserum) × (Crserum/Crurine) × 100. Renal tubular reabsorption of phosphate to glomerular filtration rate (TmP/GFR) (mmol/L) was calculated as previously described [12]. Reference ranges for laboratory results are listed in Table 1 [12, 13]. Adherence to conventional therapy was assessed by parental or patient report at clinic visits.
Lower extremity radiographs were obtained as needed for routine clinical care at least once annually. All radiographs were de-identified and randomized prior to scoring by the authors. Radiographs were scored using the rickets severity score (RSS) as previously described and validated for use in XLH patients [14, 15]. As wrist radiographs were not routinely obtained, only the lower extremity images were used for analysis; these were scored from 0 to 6, with a higher score indicating a greater severity of rickets. Each radiograph was reviewed independently by 2 physician authors (a pediatric radiologist (MS) and a pediatric orthopedist (BN)) blinded to treatment and these scores were averaged. One patient was skeletally mature with natural closure of the physeal plates prior to starting burosumab and therefore was excluded from RSS analysis. Kidney ultrasounds to monitor for nephrocalcinosis were obtained every 1–2 years in all patients with XLH starting at the time of diagnosis.
Following FDA approval of burosumab and after discussion with the care team, study patients and families elected to transition from conventional therapy to burosumab. All patients discontinued phosphate supplements and calcitriol for 7 days prior to initiating burosumab per manufacturer instructions. The dose of burosumab was determined according to manufacturer instructions, 0.8 mg/kg/dose rounded to the nearest 10 mg in patients < 18 years of age and 1 mg/kg/dose rounded to the nearest 10 mg for patients 18 years old and greater. The maximum single dose utilized was 90 mg as per the manufacturer instructions. The subcutaneous injections were administered at the patient’s home by nurses or trained parents every 2 weeks if the patient was less than 18 years old or every 4 weeks if 18 years old and older. The decision to increase the burosumab dose in response to persistently low serum phosphate levels was at the discretion of the treatment team and patient/family; dosages were increased stepwise per the manufacturer instructions. In the event of a serum phosphate greater than 5 mg/dL, burosumab was held and follow-up labs were obtained every 4 weeks until serum phosphate decreased to less than 5 mg/dL, at which point burosumab was re-started at the re-initiation dose as described in the manufacturer instructions.
The same laboratory tests as above were obtained monthly for 3 months after initiation of burosumab and with any dose changes; when obtained monthly, labs were drawn 1–2 days prior to an injection. These labs were also obtained approximately every 3–6 months thereafter throughout treatment with burosumab. The exact timing of biochemical sampling every 3–6 months was variable as injections were given at home (dates of injections were not always known) and these routine monitoring labs were obtained at clinic visits. Following initiation of burosumab, lower extremity radiographs were obtained every 6–12 months. All patients in the study had baseline radiographs obtained within 1 year prior to starting burosumab and at least 2 sets of radiographs obtained after starting burosumab and these were scored as above. The frequency of ultrasonography continued unchanged after starting burosumab. Adherence to burosumab therapy was assessed by parental or patient report at clinic visits.
Throughout the study period, standing height was measured at each clinic visit and height z-score was determined using sex- and age-matched normative values [16]. Baseline height was defined as last height measured prior to starting burosumab. Mean changes from baseline were calculated following initiation of burosumab. One patient who had reached skeletal maturity while on conventional therapy was excluded from height analysis.
Statistical analyses were conducted using a 2-tailed paired t-test and were performed using Microsoft Excel (Redmond, WA). A p value < 0.05 was considered statistically significant. Standard error of the mean was calculated as the standard deviation of the sample divided by the square root of the sample size.
Approval for this study was granted by the University of Wisconsin Health Sciences Institutional Review Board.
Results
Twelve patients met inclusion criteria. Baseline characteristics of the 12 patients are detailed in Table 2. One patient was 18 years old, and the remaining patients were between 1 and 17 years old. Adherence with conventional therapy was unable to be quantified but noted to be markedly less than 100% primarily due to abdominal cramping and diarrhea or difficulty with the frequency of phosphate supplementation. Adherence with burosumab was 100% during the study period based on verbal parental and/or patient report during clinic visits.
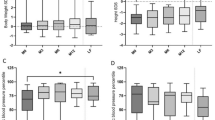
Serum phosphate, alkaline phosphatase, and PTH levels pre-, 1 month post-, and 12 months post-burosumab are displayed in Table 3. The average serum phosphate level on conventional therapy just prior to initiation of burosumab was 2.6 mg/dL. After 4 weeks on burosumab, the average serum phosphate level increased to 3.4 mg/dL (p = 0.004). This increase was sustained at 12 months post-burosumab with an average phosphate level of 3.5 mg/dL (p < 0.001). Phosphate levels over the course of the 2 years following treatment with burosumab are shown in Fig. 1a. All twelve patients had hypophosphatemia based on age- and sex-matched normative values while on conventional therapy. Three patients (25%) had normalization of their serum phosphate level while on treatment with burosumab.
Alkaline phosphatase levels decreased from an average of 593 IU/L pre-burosumab to 502 IU/L 1-month post-burosumab (p = 0.01). These levels continued to decrease to 408 IU/L after 12 months of burosumab (p = 0.001). Alkaline phosphatase levels over the course of the 2 years following treatment with burosumab are shown in Fig. 1b. Ten of the twelve patients had hyperphosphatasemia based on age- and sex-matched normative values while on conventional therapy. Nine of these ten patients (90%) had normalization of their serum alkaline phosphatase level while on treatment with burosumab.
Average PTH levels prior to starting burosumab were 83.8 pg/mL and decreased to 55.4 pg/mL 1 month after initiation of burosumab (p = 0.01). This decrease in PTH was sustained at 51.8 pg/mL following 12 months of burosumab therapy (p = 0.02). PTH levels over the course of the 2 years following treatment with burosumab are shown in Fig. 1c. Four patients previously developed hyperparathyroidism during conventional therapy. All four patients demonstrated improvement of PTH levels following conversion to burosumab with three patients exhibiting resolution of hyperparathyroidism with burosumab treatment (Fig. 2).
Urinary excretion of phosphate was measured by calculating FEphos and TmP/GFR and noted in Table 3. The average FEphos prior to starting burosumab was 33%. This decreased to 9% 1 month after treatment with burosumab (p = 0.04). At 12 months of burosumab therapy, the FEphos was calculated at 14%, continued significantly lower than pre-burosumab (p = 0.02). Correspondingly, TmP/GFR increased from 1.83 on conventional therapy to 3.50 after 1 month on burosumab (p < 0.001). At 12 months on burosumab therapy, the TmP/GFR was 3.12 (p < 0.001). FEphos and TmP/GFR over the course of the 2 years following treatment with burosumab are shown in Fig. 3. Urinary calcium excretion did not significantly change upon conversion to burosumab (Table 3).
Two patients were diagnosed with nephrocalcinosis prior to initiation of burosumab. The degree of increased echogenicity of the medullary pyramids on kidney ultrasound in these patients did not change following treatment with burosumab. No patients developed nephrocalcinosis during burosumab therapy.
The average RSS of our patient population, as measured from lower extremity radiographs, prior to starting burosumab was 3. On the first radiograph obtained post-burosumab, the average RSS decreased to 2.1. The most recent radiograph acquired while taking burosumab demonstrated an average RSS of 1.4. The RSS before and after treatment with burosumab are displayed in Fig. 4. Sample radiographs of one patient are detailed in Fig. 5. Average standing height z-scores increased significantly by 0.35, 0.6, 0.72, and 0.94 compared to baseline at months 6, 12, 18, and 24 after starting burosumab, respectively (Fig. 6). Two patients, both > 12 years old at burosumab initiation, underwent lower extremity osteotomies to correct previously identified rachitic deformities. Burosumab therapy was continued without modification throughout the perioperative period and both patients recovered uneventfully from surgery without complications. One patient developed a dental abscess while on burosumab that was successfully treated with antibiotics and oral surgery; no adjustments were made to the burosumab dosing.
Sample lower extremity (a) and knee (b) radiographs of a patient treated with burosumab. Marked improvement of genu varum and stigmata of rickets following treatment with burosumab. A — Final radiograph prior to initiation of burosumab. RSS = 4. B — Initial radiograph following initiation of burosumab. RSS = 2.5. C — Most recent radiograph. RSS = 1.5
Average standing height z-scores, expressed as change from baseline (month 0). Month 0 represents the most recent height z-score prior to initiation of burosumab. All other months are following start of burosumab. Error bars represent the standard error of the mean. *Height z-score vs. baseline (all p values < 0.01)
Because of persistent hypophosphatemia despite burosumab treatment, four patients underwent burosumab dose increases prior to the scheduled weight-adjusted dose increases. Serum phosphate levels did not meaningfully change and did not normalize following the dose increases. Alkaline phosphatase levels and RSS scores continued to improve in these patients in a similar fashion to those children who did not undergo dose increases.
One patient developed serum phosphate > 5 mg/dL (5.8 mg/dL) resulting in a pause in therapy of 4 weeks duration at which point phosphate levels decreased to < 5 mg/dL. Burosumab was successfully restarted at half dose and the patient’s subsequent laboratory values were normal; burosumab was eventually increased to full dose with no further phosphate levels > 5 mg/dL. No clinical manifestations of the elevated phosphate levels were observed.
Monitoring for adverse events and serious adverse events occurred at each clinic visit. Seven patients reported mild injection site reactions due to burosumab; no other side effects were noted during the study period. One patient with a history of migraines reported headaches during treatment with burosumab; after consultation with the patient’s neurologist, it was suspected that the burosumab was unlikely causative of the headaches. No patient discontinued burosumab or returned to conventional therapy.
Discussion
We have demonstrated statistically significant improvements in laboratory parameters as well as radiographic findings in children with XLH following transition from conventional therapy to burosumab. This study constitutes a real-world cohort of children with XLH treated with burosumab and expands on previous studies by examining radiographic changes in children treated with burosumab. This analysis confirms the use of burosumab as the treatment of choice in pediatric XLH patients.
The clinical studies in children with XLH that led to FDA approval of burosumab were safety and efficacy studies performed under ideal settings that were tightly regulated [8, 9]. Dedicated research staff ensured adherence to a calculated study design, which for many reasons often cannot be duplicated in real-world clinical settings and therefore have limited external validity [17]. While these clinical trials are necessary to determine safety and efficacy of a new medication, they do not demonstrate effectiveness, specifically that a new therapy is truly beneficial to patients in everyday clinical practice; therefore, such clinical trials should be supported by population-based observational research [18]. This is especially true in rare diseases such as XLH where a low prevalence of disease limits the numbers of patients studied in even the most robust clinical trials; additionally, this is relevant in XLH where conventional therapy adherence is not always optimal given the difficulties with the dosing frequency and side effects of the therapy. A recent consensus article recommends conventional therapy over burosumab as first-line treatment in children with XLH due to lack of published data regarding the use of burosumab [11]. This recommendation is even more noteworthy given that conventional therapy is not an FDA-approved treatment for XLH and that adverse events including nephrocalcinosis and hyperparathyroidism (both observed in our patients) are not infrequent, underscoring the need for further post-approval investigation of the real-world effectiveness of burosumab.
Martin Ramos et al. previously reported a case series of 5 children with XLH treated with burosumab for 1 year [19]. All 5 patients received conventional therapy prior to starting burosumab and had ongoing hypophosphatemia during conventional treatment. That study demonstrated normalization of serum phosphate levels in all 5 patients following the introduction of burosumab. Alkaline phosphatase levels decreased in 3 of the 5 patients and urinary phosphate excretion decreased in all 5 patients. Height z scores improved in 3 of the 5 patients and no patients had significant side effects of the therapy. The authors’ conclusion in this report was that 1 year of burosumab administration was safe and efficacious in children with XLH.
Here we report the largest real-world study of the use of burosumab in pediatric XLH. In our cohort, urinary phosphate excretion, the sine qua non of XLH, decreased significantly after initiation of burosumab. This effect was maintained throughout the 2-year study period. We observed a statistically significant improvement in mean serum phosphate levels with burosumab treatment vs. conventional therapy that was sustained. Similarly, mean alkaline phosphatase and PTH levels decreased significantly after transition to burosumab. Both values continued to decline with continued burosumab treatment up to 2 years indicating improving bony mineralization.
In contrast to the findings of Martin Ramos et al., the majority of our patients demonstrated persistent hypophosphatemia on burosumab, which was despite marked improvement in rachitic changes. Conversely, most patients displayed complete normalization of alkaline phosphatase levels after transition to burosumab. Four patients with improving alkaline phosphatase levels, urine phosphate excretion, and rachitic changes on x-ray but persistent hypophosphatemia underwent burosumab dose increases; these four patients continued with hypophosphatemia throughout the study period. These patients were all exhibiting improvement prior to the dose increase and no additional improvements were noted following the burosumab increase. Our data suggests that normal alkaline phosphatase levels are a more precise marker of treatment success and that normalizing serum phosphate levels may not be a necessary goal of therapy. Further studies will need to determine if burosumab dose increases are warranted for persistent hypophosphatemia in the patient that is otherwise responding well to treatment.
Additionally, this study noted improvement in PTH levels in all patients with hyperparathyroidism while on conventional therapy following conversion to burosumab with resolution of hyperparathyroidism in three of four patients. The mechanism of this is not clear, though likely is related to the removal of FGF-23-induced inhibition of 1-α-hydroxylase and restoration of normal calcium homeostasis. Other possibilities for the decrease in PTH include the withdrawal of phosphate supplementation or changes in dietary calcium intake (though patients were evaluated regularly by our metabolic bone clinic dietician and no significant dietary changes were noted during the study). Future studies are needed to examine this pathway and the role of burosumab in PTH regulation.
Our current study has documented the improvement in height z-scores and rachitic changes seen after transition from conventional therapy to burosumab. Our data indicate that real-world use of burosumab in skeletally immature pediatric XLH patients significantly improves linear height z-scores compared to conventional therapy, with continued improvements over time. Martin Ramos et al. were unable to comment on rachitic changes as they noted that none of their patients had active radiological lesions of rickets, attributed to the previous treatment with phosphate and calcitriol. Our results are more consistent with those seen in previously reported studies that demonstrate only partial correction of radiographic lesions with early and aggressive conventional treatment [8, 9, 20]. Furthermore, our radiographic analysis utilized the RSS, a validated tool to standardize interpretation of rachitic changes in this population. Using the RSS, we were able to conclusively demonstrate statistically significant improvement in rachitic changes after transition to burosumab, signifying consistent positive results in both clinical trial and real-world settings.
Burosumab was well-tolerated in our study population with no significant adverse effects during the study period. No worsening of nephrocalcinosis or development of nephrocalcinosis was identified following initiation of burosumab. One patient, a 3-year-old girl, developed serum phosphate levels > 5 mg/dL, which was not previously noted in the clinical trials or in the case series. The patient’s highest serum phosphate was 5.8 mg/dL; this is clearly above the acceptable upper limit as set by the manufacturer, but it is unclear that this level truly represents hyperphosphatemia, as reference ranges note that a phosphate level of 4.3–6.8 mg/dL is within the normal range for a female 1 to < 5 years of age [13]. This patient had no ill effects of the phosphate levels > 5 mg/dL and the levels quickly fell when burosumab was withheld; subsequently, she was safely able to restart therapy. Future studies are needed to address burosumab dosing adjusted to age-normalized phosphate levels.
There are several limitations of this current study. The data generated in this study are based on a retrospective, single-center experience; as is the case with most rare disease research, it is often ideal to combine data from multiple centers to be able to examine a sufficient number of patients. Our current study included a large enough cohort to determine statistical significance, but future multi-center studies are desirable to further corroborate our conclusions and to expand on findings such as improvements in hyperparathyroidism. One such study is the X-linked Hypophosphatemia Disease Monitoring Program (XLH-DMP), a prospective multi-center study currently collecting data of children and adults diagnosed with XLH over a 10-year period. The XLH-DMP does have the advantage of obtaining laboratory and imaging studies at uniform time points; while our clinical practice attempted to maintain consistency with timing of labs and radiology studies, real-world factors added to some variability in the timing of our data collection. During the initiation and dose change phases, labs were obtained precisely every 4 weeks and timed out to occur 1–2 days prior to an injection of burosumab. Though not recommended by the manufacturer, we would have ideally liked to have all patients’ lab specimens for the duration of the study obtained at the same intervals for improved data analysis. Fortunately, despite this potential confounder, our laboratory results were very similar to the phase 2 and 3 clinical trials; furthermore, the significant improvements in rickets and height after starting burosumab correlate with our improved laboratory values [8,9,10]. Additionally, we would have preferred to follow all our patients at closer intervals (such as every 3 months during growth phases while on conventional therapy) but for most of our patients this was logistically challenging and sometimes untenable [11]. Finally, we did not obtain wrist radiographs with enough frequency to calculate the full RSS, which is anticipated to be reported by the XLH-DMP.
Our study demonstrates that burosumab is safe and more effective than conventional therapy in treating real-world pediatric XLH patients and supports the use of burosumab as the first-line therapy for children with XLH. Laboratories, rachitic changes on radiographs, and height z-scores were significantly improved on burosumab compared to conventional therapy and overall burosumab was well-tolerated. Further longitudinal, long-term, multi-center studies are needed to assess real-world long-term safety and effectiveness of burosumab in larger cohorts.
Data availability
Dataset generated from retrospective medical chart review and is available upon request.
References
Shore RM, Chesney RW (2012) Rickets: part I. Pediatr Radiol 43:140–151
Carpenter TO, Shaw NJ, Portale AA, Ward LM, Abrams SA, Pettifor JM (2017) Rickets. Nat Rev Dis Primers 3:17101
Carpenter TO, Imel EA, Holm IA, Jan de Beur SM, Insogna KL (2011) A clinician’s guide to X-linked hypophosphatemia. J Bone Miner Res 26:1381–1388
(1995) A gene (PEX) with homologies to endopeptidases is mutated in patients with X-linked hypophosphatemic rickets. The HYP Consortium. Nat Genet 11:130–136
Lecoq AL, Chaumet-Riffaud P, Blanchard A, Dupeux M, Rothenbuhler A, Lambert B, Durand E, Boros E, Briot K, Silve C, Francou B, Piketty M, Chanson P, Brailly-Tabard S, Linglart A, Kamenicky P (2020) Hyperparathyroidism in patients with X-linked hypophosphatemia. J Bone Miner Res 35:1263–1273
Verge CF, Lam A, Simpson JM, Cowell CT, Howard NJ, Silink M (1991) Effects of therapy in X-linked hypophosphatemic rickets. N Engl J Med 325:1843–1848
Lamb YN (2018) Burosumab: first global approval. Drugs 78:707–714
Imel EA, Glorieux FH, Whyte MP, Munns CF, Ward LM, Nilsson O, Simmons JH, Padidela R, Namba N, Cheong HI, Pitukcheewanont P, Sochett E, Högler W, Muroya K, Tanaka H, Gottesman GS, Biggin A, Perwad F, Mao M, Chen C-Y, Skrinar A, San Martin J, Portale AA (2019) Burosumab versus conventional therapy in children with X-linked hypophosphataemia: a randomised, active-controlled, open-label, phase 3 trial. Lancet 393:2416–2427
Carpenter TO, Whyte MP, Imel EA, Boot AM, Hogler W, Linglart A, Padidela R, Van’t Hoff W, Mao M, Chen CY, Skrinar A, Kakkis E, San Martin J, Portale AA (2018) Burosumab therapy in children with X-linked hypophosphatemia. N Engl J Med 378:1987–1998
Whyte MP, Carpenter TO, Gottesman GS, Mao M, Skrinar A, San Martin J, Imel EA (2019) Efficacy and safety of burosumab in children aged 1–4 years with X-linked hypophosphataemia: a multicentre, open-label, phase 2 trial. Lancet Diabetes Endocrinol 7:189–199
Haffner D, Emma F, Eastwood DM, Duplan MB, Bacchetta J, Schnabel D, Wicart P, Bockenhauer D, Santos F, Levtchenko E, Harvengt P, Kirchhoff M, Di Rocco F, Chaussain C, Brandi ML, Savendahl L, Briot K, Kamenicky P, Rejnmark L, Linglart A (2019) Clinical practice recommendations for the diagnosis and management of X-linked hypophosphataemia. Nat Rev Nephrol 15:435–455
Payne RB (1998) Renal tubular reabsorption of phosphate (TmP/GFR): indications and interpretation. Ann Clin Biochem 35:201–206
Colantonio DA, Kyriakopoulou L, Chan MK, Daly CH, Brinc D, Venner AA, Pasic MD, Armbruster D, Adeli K (2012) Closing the gaps in pediatric laboratory reference intervals: a CALIPER database of 40 biochemical markers in a healthy and multiethnic population of children. Clin Chem 58:854–868
Thacher TD, Fischer PR, Pettifor JM, Lawson JO, Manaster BJ, Reading JC (2000) Radiographic scoring method for the assessment of the severity of nutritional rickets. J Trop Pediatr 46:132–139
Thacher TD, Pettifor JM, Tebben PJ, Creo AL, Skrinar A, Mao M, Chen CY, Chang T, San Martin J, Carpenter TO (2019) Rickets severity predicts clinical outcomes in children with X-linked hypophosphatemia: utility of the radiographic Rickets Severity Score. Bone 122:76–81
Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, Wei R, Curtin LR, Roche AF, Johnson CL (2002) 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat 11:1–190
Sherman RE, Anderson SA, Dal Pan GJ, Gray GW, Gross T, Hunter NL, LaVange L, Marinac-Dabic D, Marks PW, Robb MA, Shuren J, Temple R, Woodcock J, Yue LQ, Califf RM (2016) Real-world evidence - what is it and what can it tell us? N Engl J Med 375:2293–2297
Booth CM, Tannock IF (2014) Randomised controlled trials and population-based observational research: partners in the evolution of medical evidence. Br J Cancer 110:551–555
Martin Ramos S, Gil-Calvo M, Roldan V, Castellano Martinez A, Santos F (2020) Positive response to one-year treatment with burosumab in pediatric patients with X-linked hypophosphatemia. Front Pediatr 8:48
Makitie O, Doria A, Kooh SW, Cole WG, Daneman A, Sochett E (2003) Early treatment improves growth and biochemical and radiographic outcome in X-linked hypophosphatemic rickets. J Clin Endocrinol Metab 88:3591–3597
Author information
Authors and Affiliations
Contributions
Dr. Paloian conceptualized and designed the study, coordinated and supervised data collection, performed the data analysis, drafted the initial manuscript, and reviewed and revised the manuscript. Drs. Nemeth and Sharafinski performed the radiographic interpretations and reviewed and revised the manuscript. Ms. Modaff and Dr. Steiner conceptualized and designed the study and reviewed and revised the manuscript, revising it critically for important intellectual content.
Corresponding author
Ethics declarations
Ethics approval
Study approved by the University of Wisconsin-Madison Health Sciences Institutional Review Board.
Consent to participate
Waiver of informed consent granted by IRB.
Consent for publication
All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Conflict of interest
Neil Paloian is a member of the speaker’s bureau of Ultragenyx pharmaceuticals. Robert D. Steiner reports equity interest in and consulting fees from Acer Therapeutics and PTC Therapeutics. He also reports leading an investigator-initiated observational research study funded by Alexion via contract with Marshfield Clinic Health System, and consulting fees from Alexion, Best Doctors, E-Scape Bio, Health Advances, Precision for Value, and Travere, and honoraria from Medscape/WebMD and The France Foundation as well as employment with Prevention Genetics. The other authors have no relevant conflicts of interest or financial or proprietary interests to disclose.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Paloian, N.J., Nemeth, B., Sharafinski, M. et al. Real-world effectiveness of burosumab in children with X-linked hypophosphatemic rickets. Pediatr Nephrol 37, 2667–2677 (2022). https://doi.org/10.1007/s00467-022-05484-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-022-05484-7