Abstract
Background
Renal Angina Index (RAI) is a bedside tool for risk stratification of patients to predict acute kidney injury (AKI). Kidney biomarkers are better indicators of real-time injury and give us lead time for diagnosing impending AKI.
Methods
We enrolled consecutive children aged 2 months–14 years admitted to a tertiary hospital in northern India over 2 years. RAI was calculated on day 0 (D0) and urinary (u) and plasma (p) neutrophil gelatinase-associated lipocalin (NGAL) were measured within 6 h of admission. Children were followed for the development of severe AKI on day 3 (D3) using Kidney Disease Improving Global Outcomes criteria to define and stage AKI.
Results
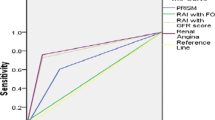
Of the 253 children enrolled and analysed, 44 (17.4%) developed D3-AKI (stage 1 in 52.2%, stage 2 in 20.5% and stage 3 in 27.3%). Renal angina (RAI ≥ 8) on D0 was present in 66.7% children who developed stage 2/3 D3-AKI vs. 43.5% in children who did not develop D3-AKI /stage 1 AKI (p = 0.065). Area under ROC (AUROC) curve for D0-RAI to predict D3-severe-AKI was 0.66 (95% CI, 0.55–0.77). AUROC curve for uNGAL and pNGAL to predict D3-severe-AKI was 0.62 (95% CI, 0.50–0.74) and 0.48 (95% CI, 0.35–0.61), respectively. The severe AKI group had greater requirement of ventilation and inotropic support with mortality being thrice higher compared to the non-AKI group.
Conclusion
RAI ≥ 8 and uNGAL had a high negative predictive value but low sensitivity for predicting D3-severe-AKI. pNGAL had a poor predictive value for D3-severe-AKI.
Graphical abstract
A higher resolution version of the Graphical abstract is available as Supplementary information

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute kidney injury (AKI) is a common cause of mortality and morbidity in hospitalised patients. According to the Assessment of Worldwide Acute Kidney Injury, Renal Angina and Epidemiology in critically ill children (AWARE) study, incidence of AKI was 26.9% amongst 4623 hospitalised patients aged 3 months–25 years age [1]. Despite increasing awareness about the disease, effective therapies are lacking. This is partially due to delay in diagnosis. Timely diagnosis of AKI is likely to provide survival advantage. The current method of detection of AKI using the KDIGO criteria is dependent on urinary output (UO) and serum creatinine (SCr) which rises 24–48 h after the initial kidney insult [2]. Researchers worldwide are therefore trying to identify clinical scores and laboratory biomarkers for an earlier identification of AKI [2].
One such clinical score is renal angina index (RAI). Basu et al. proposed that renal angina may occur when there is vascular insult to the kidney. The RAI is a bedside method which uses objective signs of kidney dysfunction and risk factors of AKI to predict onset of AKI (Supplementary Table 1). In order to operationalise the use of RAI in critically ill children, it was seen that RAI could predict AKI that develops 3 days after admission (D3-AKI) [3, 4].
Several biomarkers have been studied for early detection of AKI. These biomarkers are protein-bound substances which denote structural kidney damage rather than reduced kidney function. To date, neutrophil gelatinase-associated lipocalin (NGAL) has shown to be of value in early diagnosis of paediatric kidney injury [5,6,7]. Importantly, biomarkers provide reliable information only when utilised in the appropriate setting. Thus, biomarkers when used in the presence of renal angina may have a better predictive value [8].
We aimed to validate RAI in our population and determine the diagnostic accuracy of biomarkers: urinary NGAL (uNGAL) and plasma NGAL (pNGAL) to predict D3-AKI in critically ill children. We hypothesised that in children aged 2 months–14 years, calculation of RAI on day 0 (D0) and urinary/plasma NGAL would predict D3-severe-AKI and thus trigger prompt interventions to prevent morbidity and mortality.
Methods
We conducted a prospective cohort study in children (aged 2 months–14 years) admitted to the sick room of a paediatric emergency and Paediatric Intensive Care Unit (PICU) of a tertiary care referral teaching hospital in north India over a period of 2 years (1 January 2019–31 December 2020). Children were enrolled only if they had a hospital stay > 6 h, after written and informed parental consent. We excluded patients who denied consent, patients with known chronic kidney disease (CKD) or post-kidney transplant, lethal congenital malformations [9] or already on dialysis. Children were also excluded if they did not have SCr or UO measurements during hospital stay. The study was approved by the Institute’s Ethics Committee.
Demographic, clinical data and pre-identified laboratory variables were collected for all eligible children. RAI was calculated on D0 to risk stratify for AKI. RAI is the product of risk of AKI and signs of injury (Supplementary Table 1). RAI ≥ 8 was considered as positive for renal angina. Children were then sampled for biomarkers. The time of sample collection was noted. Fluid intake and output was calculated from the nursing charts. Older children were asked to void in a graduated container. If the patient was not catheterised, diaper weight monitoring was done in younger children. Fluid overload (FO) was calculated as per formula: % FO = 100 (fluid intake in mL − fluid output in mL) / Admission weight (g) [10]. uNGAL and pNGAL values were assayed using a commercially available Enzyme-Linked Immunosorbent Assay (ELISA) kit (Biovendor Human Lipocalin-2/NGAL ELISA kit, Czech Republic, Europe) as per the manufacturer’s instructions. Optimum cut-off values were determined using sensitivity analysis and Youden’s index [11]. The children were followed for the development of AKI on day 3 (D3) by using Kidney Disease: Improving Global Outcomes (KDIGO) criteria to define and stage AKI [12]. Children who developed D3-stage 2/3 AKI served as cases (AKI group) whilst those who did not develop D3-AKI or had stage 1 AKI served as controls (non-AKI group). All children were followed until hospital discharge or death for treatment outcomes.
Outcomes
Our primary outcome was development of D3-AKI (primary end point). The Schwartz equation was used to calculate the estimated glomerular filtration rate (eGFR) [13]. Baseline eGFR was calculated using the SCr value up to 3 months before the emergency visit. If the baseline SCr level was unavailable eGFR [12] was assumed to be 120 mL/min/1.73 m2. Our secondary outcomes were requirement of ventilation, inotropic support and kidney replacement therapy (KRT), duration of hospital stay, nephrotoxin drug exposure and incidence of urinary tract infection (UTI), pneumonia or meningitis.
Statistical analysis
We calculated a sample size of 250 children for the study based on the work of Menon et al. [8], considering error of estimate of 1.96 for constructing confidence interval (CI) of sensitivity 10% and prevalence 25%. Data was entered in Microsoft Excel. Categorical variables were reported as counts and percentages. The distribution of continuous variables was checked by Shapiro–Wilk test. All quantitative variables were presented as mean ± standard deviation or median (interquartile range) where applicable. Their 95% CI were calculated. Children who developed severe AKI (stage 2/3) on D3 and who did not develop AKI/ stage 1 AKI were compared. Proportions were compared using Chi-square test with Yates correction or Fisher’s exact test. Continuous variables between AKI and non-AKI groups were compared using Student’s t-test or Mann–Whitney U test. We constructed receiver operating characteristic (ROC) curves for RAI, uNGAL and pNGAL as continuous variable and D3-severe-AKI as categorical variable. The diagnostic accuracy of RAI for development of D3-severe-AKI was calculated at cut-off values of 8 and 12 and for uNGAL at cut-off values of 100 and 150 ng/mL. The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and likelihood ratios (LR) were calculated using medcalc software. We also calculated the diagnostic accuracy of combined RAI (at cut-off of 8 and 12) and uNGAL (at cut-off 100 and 150 ng/mL). All variables with p value less than 0.1 on univariate analysis were included in multivariable logistic regression analysis for identification of independent variables associated with mortality. A p value < 0.05 was considered significant. Statistical package SPSS-22 (IBM, New York) was used for data analysis.
Results
We screened 300 consecutive children admitted to the sick room of a paediatric emergency and PICU for eligibility into the study. Thirty-eight children were excluded (Fig. 1). We enrolled 262 children, of whom 9 children either died or left against medical advice before D3 of admission (primary end point). Hence, 253 children were analysed for outcomes.
According to the KDIGO criteria, 44 (17.4%) children developed AKI on D3. Amongst these 44 children, 23 (52.2%) developed AKI stage 1, 9 (20.5%) developed AKI stage 2 and 12 (27.3%) developed AKI stage 3. The AKI group (AKI stage 2/3) and non-AKI groups (no AKI/ stage 1 AKI) were comparable to each other with respect to demographic characteristics and presenting complaints (Table 1). On examination, the AKI group had a higher proportion of children requiring oxygen supplementation (p = 0.04) compared to the non-AKI group. D0-total leukocyte count, D3-blood urea and D3-serum creatinine was significantly higher in the AKI group. Likewise, D3-UO and D3-eGFR were significantly lower in the AKI group compared to the non-AKI group (Table 1). Final diagnosis was categorised into 18 clinical conditions. D3-AKI incidence was not significantly associated with any medical diagnosis. However, 57.1% of the children with tropical infections (vs. 18.1% in non-AKI group, p = 0.07) and 9.5% of children with nephritic syndrome (vs. 1.7% in non-AKI group, p = 0.08) developed D3-severe-AKI (Fig. 2).
D0-RAI was significantly higher in children who went on to develop D3-severe-AKI (8, IQR: 4, 20) vs. those who did not (4, IQR: 2, 8; p = 0.01). uNGAL levels on D0 were higher in the AKI group as compared to the non-AKI group but it did not reach statistical significance [33.8 ng/mL (IQR 9.9, 61.4) vs. 11.0 ng/mL (IQR 3.1, 32.3), p = 0.07]. pNGAL levels were similar between the 2 groups [149.1 ng/mL (IQR 106.3, 284.4) vs. 191.4 ng/mL (IQR 92.3, 288.2), p = 0.76] (Table 1). The sensitivity, specificity, PPV, NPV, positive likelihood ratio (+ LR) and negative likelihood ratio (− LR) of RAI (at cut-off value 8 and 12) and urinary/plasma NGAL (at a cut-off of 100 and 150 ng/mL) to predict D3-AKI are presented in Table 2. uNGAL and RAI had good specificity and NPV, but all tests had poor PPV and likelihood ratios. Urinary or plasma NGAL values at both the cut-off values of 100 and 150 ng/mL did not increase the diagnostic accuracy of RAI (at cut-off of 8 and 12) for prediction of D3-AKI (Table 3). Whilst area under ROC curve (AUROC) of RAI to differentiate D3-severe-AKI was statistically significant 0.66 (95% CI, 0.55–0.77, p = 0.02), AUROC of uNGAL [0.62 (95% CI, 0.50–0.74), p = 0.07] as well as pNGAL [0.48 (95% CI, 0.35–0.61, p = 0.76)] were not significant. Combined AUROC of RAI and uNGAL to predict D3-AKI was 0.59 (95% CI, 0.47–0.72, p = 0.16) (Table 3; Supplementary Fig. 1).
Regarding treatment outcomes, children in the AKI group had a significantly higher requirement of ventilation (RR 2.4 (95% CI, 1.1–5.2)), inotropic support (RR 4.1 (95% CI, 1.7–10.0)) and KRT (RR 1.3 (95% CI, 1.0–1.7)) compared to the non-AKI group (Table 4). Fifty-seven of 253 enrolled children died or left against medical advice. Non-survivors had significantly higher RAI and NGAL values as compared to survivors (Supplementary Table 2). However, after adjusting for requirement of ventilation, inotrope use, Glasgow coma score, AKI on D3, RAI, haemoglobin and blood sugar levels at presentation, neither the RAI nor NGAL could independently predict mortality. The independent predictors of mortality on multivariable logistic regression analysis included requirement of inotropes, D3-severe-AKI and haemoglobin levels at presentation. Relative risk of mortality was significantly higher in children who developed D3-AKI (66.7%) vs. 18.5% in the non-AKI group, RR 2.4 (95% CI, 1.3–4.5, p < 0.001) (Table 4).
Discussion
In this prospective cohort study of 253 hospitalised paediatric patients, we found an 8.3% incidence of severe AKI according to the KDIGO criteria. D0-RAI was significantly higher in children who developed D3-AKI compared to the non-AKI group. At a cut-off of 8, RAI had statistically significant discriminative ability to identify D3-AKI. However, RAI had a modest diagnostic accuracy for D3-AKI. Urinary or plasma NGAL did not improve the diagnostic accuracy of RAI. Requirement of inotropes, D3-AKI and baseline haemoglobin independently predicted mortality, but RAI or NGAL did not.
Incidence of AKI was noted to be 26.9% by AWARE investigators and 15% in a study conducted at AIIMS, New Delhi [1, 14]. The AWARE study reported 11.3% incidence of severe AKI (stages 2 and 3) which is comparable to our study [1]. Fever, vomiting and breathing difficulty were the most common presenting complaints in our study which was observed previously, too [15, 16]. We found a significant decrease in D3-UO between the AKI and non-AKI groups (Table 1). Menon et al. previously reported that patients with AKI are at a higher risk of FO on day 3 because of persistent severe fluid accumulation [8]. A total of 57.1% of the children with tropical infections developed D3-AKI. This is similar to the findings of a study done in south India where it was found that infections were responsible for 62.9% of cases of AKI [17]. Although it did not reach statistical significance, nephritic conditions were present in 9.5% children with D3-AKI. Our figures match with previous studies that reported glomerulonephritis was responsible for 7.6% of the AKI cases [17]. A higher proportion of children had sepsis, liver disease, anaemia, acute respiratory distress syndrome and diabetes in AKI versus non-AKI group. However, this difference was not statistically significant (Fig. 2). These findings could be because of the heterogeneous nature of our cohort.
A significantly higher proportion of children with severe AKI had renal angina when RAI ≥ 8 was taken as the criteria as compared to the non-AKI group (66.7% in AKI vs. 43.5% in non-AKI group). In the study by Menon et al., similar numbers were reported (80% in AKI vs. 28.8% in non-AKI) [8]. In a meta-analysis which included 10 studies, it was seen that ability of RAI ≥ 8 to predict AKI had a pooled sensitivity of 79.2% and specificity of 73.2% [18]. Recently it was reported that RAI value ≥ 12 as compared to ≥ 8 had higher specificity, Youden’s index, PPV and better discriminative ability in diagnosing D3-severe-AKI [14]. However, we did not observe a difference between the diagnostic accuracy of RAI ≥ 8 and RAI ≥ 12 to predict D3-severe-AKI except that specificity and PPV of RAI ≥ 12 was better than RAI ≥ 8 (Table 2). In another study conducted in adults in Japan and Thailand, AUROC for RAI was found to be 0.63 which is the same as our study [19]. Previous research has shown that in children developing AKI due to causes other than post-cardiac surgery, AUROC for RAI ranges from 0.6 to 0.8 [8].
We found that with a cut-off of 100 ng/mL, specificity of uNGAL was 93% (95% CI, 98.9–95.9) and NPV was 91.8 (95% CI, 90.6–92.8) (Table 2). The sensitivity and PPV were, however, low, i.e., 9.52% (95% CI, 1.2–30.4) and 11.11% (95% CI, 3–33.7), respectively. Our study failed to demonstrate predictive value of pNGAL in contrast to a few studies which have reported pNGAL value to be higher in paediatric risk, injury, failure, loss and end-stage renal disease (pRIFLE) injury/failure groups [6]. This may be explained by the heterogeneous nature of our cohort. We found that using the combination of RAI ≥ 8 and uNGAL value of 100 ng/mL did not improve the diagnostic accuracy for D3-severe-AKI. The poor predictability of urinary/plasma NGAL for AKI prediction in a non-homogeneous cohort has been seen in a recent study from the United Kingdom where the AUC for uNGAL and pNGAL to predict severe AKI was 0.75 and 0.64, respectively [20].
Our observations on the higher requirement of ventilation and inotropic support in children suffering from D3-AKI were in concordance with the published literature [21,22,23]. The requirement of KRT was lower than that in the global snapshot study but comparable to other studies from India [24, 25]. This could be attributed to the fact that the global snapshot study included high-income countries where these facilities are easily available, but limited access and financial constraints in our low-resource settings decrease the use of KRT, especially haemodialysis. However, mortality rates in our study were comparable to the findings obtained by Kaur et al. (31.09% in renal angina positive vs. 2% in renal angina negative) and in the secondary analysis of Sepsis Prevalence, Outcomes and Therapies (SPROUT) trial (52% in AKI stage 2/3 vs. 18% in no AKI/stage 1 AKI) [15, 23].
Our strengths include the prospective nature of the study and a large paediatric sample size which helped us analyse multiple aetiologies with respect to incidence of AKI. Also, we used both RAI and NGAL values to predict AKI. We examined an exhaustive repertoire of variables predisposing to D3-severe-AKI in a resource-limited setting. Despite all our efforts, our study had some limitations. Firstly, it was a single-centre study and we did not have departments such as paediatric surgery, haemato-oncology and organ transplant facilities available at our centre so we could not include these patients in our study. Secondly, method of urine collection especially in the younger children was often done by diaper weight or by parental recall in older children which was not as accurate as catheterisation. Thirdly, the majority of the study children did not have baseline SCr available to enable us to exclude pre-existing CKD. However, any child with kidney complaints including decreased UO for at least 3-month duration as defined by KDIGO, anaemia, short stature, any electrolyte abnormalities, any urinary sediment abnormalities or structural abnormalities was screened for CKD and complete investigational work-up was done at the time of enrolment and if found positive was excluded [12]. Also, it is possible that AKI was underdiagnosed because we used baseline eGFR of 120 mL/min/1.73 m2 in most children as baseline value of creatinine was not available. Had we used baseline eGFR of 90 mL/min/1.73 m2 AKI incidence could have been higher [26]. Nevertheless, our study underlines the importance of high negative predictive value of RAI in children at risk to develop AKI and appropriate management of patients to avoid FO in patients predisposed to develop AKI.
Conclusions
Incidence of D3-severe-AKI was 8.3% in children being admitted to paediatric emergency using the KDIGO criteria to define AKI. RAI ≥ 8 and uNGAL had a high specificity but low sensitivity for predicting D3-severe-AKI. pNGAL had a poor predictive value for D3-AKI. A combination of RAI ≥ 8 and uNGAL did not affect the diagnostic accuracy for predicting D3-severe-AKI. The study reaffirms increased mortality, and increased need of ventilation requirement, inotropic support and KRT in children developing AKI.
Data Availability
The authors declare that the data is transparent. The original data has been entered in Microsoft Excel and can be made available.
Code availability
Not applicable.
Abbreviations
- AKI:
-
Acute kidney injury
- ARDS:
-
Acute respiratory distress syndrome
- AUROC:
-
Area under receiver operating characteristic curve
- AWARE:
-
Assessment of Worldwide Acute Kidney Injury, Renal Angina and Epidemiology
- CI:
-
Confidence interval
- CKD:
-
Chronic kidney disease
- CrCl:
-
Creatinine clearance
- D0:
-
Day 0
- D3:
-
Day 3
- ELISA:
-
Enzyme-linked immunosorbent assay
- FO:
-
Fluid overload
- KDIGO:
-
Kidney Disease Improving Global Outcomes
- LR:
-
Likelihood ratio
- LAMA:
-
Left against medical advice
- NPV:
-
Negative predictive value
- NGAL:
-
Neutrophil gelatinase associated lipocalin
- PICU:
-
Paediatric intensive care unit
- pNGAL:
-
Plasma neutrophil gelatinase-associated lipocalin
- PPV:
-
Positive predictive value
- pRIFLE:
-
Paediatric Risk, Injury, Failure, Loss, End stage Renal disease
- RAI:
-
Renal angina index
- KRT:
-
Kidney replacement therapy
- SCr:
-
Serum creatinine
- SPROUT:
-
Sepsis Prevalence, Outcomes and Therapies
- TLC:
-
Total leucocyte count
- uNGAL:
-
Urinary neutrophil gelatinase-associated lipocalin
- UTI:
-
Urinary tract infection
- UO:
-
Urine output
References
Kaddourah A, Basu RK, Bagshaw SM, Goldstein SL (2017) Epidemiology of acute kidney injury in critically ill children and young adults. N Engl J Med 376:11–20
McCaffrey J, Dhakal AK, Milford DV, Webb NJ, Lennon R (2017) Recent developments in the detection and management of acute kidney injury. Arch Dis Child 102:91–96
Basu RK, Zappitelli M, Brunner L, Wang Y, Wong HR, Chawla LS (2014) Derivation and validation of the renal angina index to improve the prediction of acute kidney injury in critically ill children. Kidney Int 85:659–667
Chawla L, Goldstein S, Kellum J, Ronco C (2015) Renal angina: concept and development of pretest probability assessment in acute kidney injury. Crit Care 19:93
Parikh A, Rizzo J, Canetta P, Forster C, Sise M, Maarouf O,Singer E, Elger A, Elitok S, Schmidt-Ott K, Barasch J, Nickolas TL (2017) Does NGAL reduce costs? A cost analysis of urine NGAL (uNGAL) & serum creatinine (sCr) for acute kidney injury (AKI). PLoS One 12:e0178091
McCaffrey J, Coupes B, Chaloner C, Webb NJ, Barber R, Lennon R (2015) Towards a biomarker panel for the assessment of AKI in children receiving intensive care. Pediatr Nephrol 30:1861–1871
Palermo J, Dart AB, De Mello A, Devarajan P, Gottesman R, Garcia Guerra G et al (2017) Biomarkers for early acute kidney injury diagnosis and severity prediction: a pilot multicenter Canadian study of children admitted to the ICU. Pediatr Crit Care Med 18:e235–e244
Menon S, Goldstein S, Mottes T, Fei L, Kaddourah A, Terrell T et al (2016) Urinary biomarker incorporation into the renal angina index early in intensive care unit admission optimizes acute kidney injury prediction in critically ill children: a prospective cohort study. Nephrol Dial Transpl 31:586–594
Wilkinson D, de Crespigny L, Xafis V (2014) Ethical language and decision-making for prenatally diagnosed lethal malformations. Semin Fetal Neonatal Med 19:306–311
Goldstein SL, Currier H, Graf Cd, Cosio CC, Brewer ED, Sachdeva R (2001) Outcome in children receiving continuous venovenous hemofiltration. Pediatrics 107:1309–1312
Filho LT, Grande AJ, Colonetti T, Della ESP, da Rosa MI (2017) Accuracy of neutrophil gelatinase-associated lipocalin for acute kidney injury diagnosis in children: systematic review and meta-analysis. Pediatr Nephrol 32:1979–1988
Sreedharan R, Avner ED (2016) Renal Failure. In: Kleigman RM, Stanton BF, Geme JWS, Schor NF (eds) Nelson textbook of pediatrics, vol 2, 20th edn. Elsevier, Philadelphia, pp 2539–2543
Schwartz GJ, Work DF (2004) Measurement and estimation of GFR in children and adolescents. Clin J Am Soc Nephrol 4:1832–1843
Sundararaju S, Sinha A, Hari P, Lodha R, Bagga A (2019) Renal angina index in the prediction of acute kidney injury in critically ill children. Asian J Pediatr Nephrol 2:25–30
Kaur R, Dhooria GS, Pooni PA, Bhat D, Bhargava S, Kakkar S et al (2018) Utilization of the renal angina index in PICU of a developing country for prediction of subsequent severe acute kidney injury. Pediatr Nephrol 33:2185–2191
Yore MA, Strehlow MC, Yan LD, Pirrotta EA, Woods JL, Somontha K et al (2018) Characteristics and outcomes of pediatric patients presenting at Cambodian referral hospitals without appointments: an observational study. Int J Emerg Med 11:17
Krishnamurthy S, Narayanan P, Prabha S, Mondal N, Mahadevan S, Biswal N, Srinivasan S (2013) Clinical profile of acute kidney injury in a pediatric intensive care unit from Southern India: a prospective observational study. Indian J Crit Care Med 4:207–213
Raina R, Sethi SK, Mawby I, Datla N, Kumar N, Agarwal N, Tibrewal A, Chakraborty R (2021) Re-evaluating renal angina index: an authentic, evidence-based instrument for acute kidney injury assessment: critical appraisal. Front Pediatr 9:682672
Matsuura R, Srisawat N, Claure-Del Granado R, Doi K, Yoshida T, Nangaku M et al (2018) Use of the renal angina index in determining acute kidney injury. Kidney Int Rep 3:677–683
McGalliard RJ, McWilliam SJ, Maguire S, Jones CA, Jennings RJ, Siner S et al (2020) Identifying critically ill children at high risk of acute kidney injury and renal replacement therapy. PLoS One 15:e0240360
Alkandari O, Eddington KA, Hyder A, Gauvin F, Ducruet T, Gottesman R, Phan V, Zappitelli M (2011) Acute kidney injury is an independent risk factor for pediatric intensive care unit mortality, longer length of stay and prolonged mechanical ventilation in critically ill children: a two-center retrospective cohort study. Crit Care 15:R146
Fitzgerald J, Basu R, Akcan-Arikan A, Izquierdo L, Piñeres Olave B, Hassinger A et al (2016) Acute kidney injury in pediatric severe sepsis. Crit Care Med 44:2241–2250
Weiss SL, Fitzgerald JC, Pappachan J, Wheeler D, Jaramillo-Bustamante JC, Salloo A et al (2015) Global epidemiology of pediatric severe sepsis: the sepsis prevalence, outcomes, and therapies study. Am J Respir Crit Care Med 191:1147–1157
Nawaz S, Afzal K (2018) Pediatric acute kidney injury in North India: a prospective hospital based study. Saudi J Kidney Dis Transpl 29:689–697
Macedo E, Cerda J, Hingorani S, Hou J, Bagga A, Burdmann E et al (2018) Recognition and management of acute kidney injury in children: the ISN 0 by 25 Global Snapshot study. PLoS One 13:e0196586
Zaptelli M, Parikh CR, Akcan-Arikan A, Washburn KK, Moffett BS, Goldstein SL et al (2018) Ascertainment and epidemiology of acute kidney injury varies with definition interpretation. Clin J Am Soc Nephrol 3:948–954
Acknowledgements
We would like to thank Dr. Shiv Sajan Saini, Associate Professor of Pediatrics, PGIMER, Chandigarh, India for doing the statistical analysis of the study.
Funding
Tanvi Singh received partial financial assistance from the Indian Council of Medical Research, New Delhi, India as part of a postgraduate thesis grant; Vidushi Mahajan received financial assistance from the Department of Science and Technology, Chandigarh Administration, Chandigarh, India (vide no. S&T&RE/RP/147(18–19)/Sanc/02/2019/232–242 dated 7.2.2019).
Author information
Authors and Affiliations
Contributions
TS did literature search, patient enrolment, wrote the first draft and approved the final manuscript. VM conceived the idea for the study, supervised the study, edited the first draft and approved the final manuscript. JS and SG did the biochemical analysis, gave intellectual input and approved the final manuscript. SDC supported kidney replacement therapies, gave intellectual input and approved the final manuscript. SR and VG gave intellectual input and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the Institute’s Ethics Committee (IEC Regd No. ECR/658/Inst/PB/2014/RR-2017 dated 1.12.2017).
Consent to participate
The authors affirm that informed consent was properly documented from the parent/primary caregiver.
Consent for publication
The authors affirm that proper consent for publication was obtained from the participants.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.

Rights and permissions
About this article
Cite this article
Singh, T., Mahajan, V., Kaur, J. et al. Early diagnosis of kidney injury in a paediatric population: a prospective cohort study (E-DRIP STUDY). Pediatr Nephrol 37, 2771–2779 (2022). https://doi.org/10.1007/s00467-022-05442-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-022-05442-3