Abstract
Background
Tubulointerstitial nephritis and uveitis (TINU) syndrome is a rare disease, especially in children. Owing to the short-term observational period and the small number of patients analyzed in previous reports, the long-term clinical and laboratory characteristics and renal prognosis of children with TINU syndrome remain unclear.
Methods
In this retrospective observational study, we enrolled 29 children with TINU syndrome from February 1990 to February 2019.
Results
During the median follow-up duration of 38 months, the kidney function, urinary β2 microglobulin-creatinine ratio (U-β2MG/Cr), and uveitis in the patients had significantly improved at 24, 6, and 36 months after diagnosis. Higher U-β2MG/Cr was associated with longer duration of kidney function normalization. Half of the patients required uveitis treatment for 5 years after the diagnosis.
Conclusions
Patients with severe low-molecular weight proteinuria at diagnosis needed a longer duration to achieve improvements in kidney function. Uveitis has a much longer treatment period than tubulointerstitial nephritis. This study demonstrates the good prognosis of children with TINU syndrome in terms of their long-term clinical and laboratory characteristics.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tubulointerstitial nephritis and uveitis (TINU) syndrome is a rare disease, presenting as a combination of unidentified interstitial nephritis and bilateral/anterior uveitis. Since first noted by Dobrin in 1975 [1], more than 200 patients have been reported [2]. TINU syndrome is frequently accompanied by general symptoms such as fever, weight loss, fatigue, and abdominal pain and ocular symptoms such as eye redness, eye pain, and photophobia [3]. Although the pathogenesis of this syndrome remains unclear, an autoimmune mechanism involving a common antigen in the kidney and ocular tissue seems to play a significant role [2, 4].
The renal prognosis of TINU syndrome has been reported as generally good [5, 6], despite the fact that persistent low-molecular weight proteinuria was also reported in pediatric TINU patients [7, 8]. In addition, the observational period of previous studies was insufficient to clarify the long-term renal prognosis, especially in children with TINU syndrome. Thus, in this retrospective observational study, we aim to clarify the long-term clinical and laboratory characteristics and renal prognosis of 29 pediatric patients with TINU syndrome.
Methods
Patients
In this retrospective observational study, we enrolled patients with TINU admitted in our hospital (Division of Pediatric Nephrology, Department of Pediatrics, Hokkaido University Hospital) between February 1990 and February 2019. The number of pediatric patients and the number of pediatric nephrology consultations were 37,074 and 1000, respectively. All enrolled patients met the diagnostic criteria for a definite or probable diagnosis of TINU syndrome as described by Mandeville et al. [3] and were younger than 18 years at diagnosis. From the 37 identified patients, three and five patients were excluded because they were lost to follow-up and were followed up for < 6 months, respectively. We included 29 children with TINU syndrome in this study. We obtained their clinical and laboratory characteristics from their medical records.
Evaluation of clinical and laboratory characteristics
Data regarding history, physical examinations, laboratory blood and urinary investigations, and ophthalmological clinical findings were collected for all patients. Laboratory studies included the measurement of plasma creatinine, estimated glomerular filtration rate (eGFR), erythrocyte sedimentation rate, blood hemoglobin, sialylated carbohydrate antigen KL-6, pyuria, proteinuria, glucosuria, and urinary β2 microglobulin-creatinine ratio (U-β2MG/Cr, μg/gCr). We calculated the eGFR of patients aged 2 to 18 years using the method described by Hibi et al. [9] and the eGFR of patients aged > 18 years (during follow-up) using the method described by Matsuo et al. [10]. Regarding the follow-up data, we assessed the patients’ clinical examinations, laboratory findings (eGFR, U-β2MG/Cr) and ophthalmological examination findings, as well as treatments (oral/topical corticosteroids, immunosuppressants).
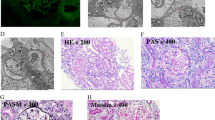
Pathological analysis
We performed kidney biopsy in patients with general symptoms and/or persistent kidney dysfunction for over 6 months. Four out of seven patients that underwent kidney biopsy had both general symptoms and persistent kidney function, and the other three patients showed persistent kidney function. Kidney biopsy specimens were obtained from seven patients with TINU syndrome. Specifically, the biopsy specimens were perfused with 4% paraformaldehyde and embedded in paraffin. Subsequently, they were sliced into 2-μm sections for light microscopy using the Periodic acid-Schiff stain. To investigate the tubulointerstitial changes, we used semi-quantitative scoring of at least ten cortical fields of Masson Trichrome-stained tissues (× 100 magnification). We used the evaluation score according to the tubulointerstitial score (TI score) [11,12,13]. The scoring system is as follows: factor 1: acute score, percentage involvement with interstitial mononuclear infiltrate; factor 2: acute score, percentage lesion with interstitial edema; factor 3: acute score, damage; and factor 4: chronicity score, interstitial fibrosis and tubular atrophy. Absence of the above features was assigned a score of 0, < 50% lesion involvement was assigned a score of 1, and > 50% involvement was assigned a score of 2. Thus, the total score ranged from 0 to 8.
Statistical analyses
Statistical analysis was performed using JMP® Pro 12 (SAS Institute Inc., Cary, NC, USA). As all data had a non-normal distribution, they were described as median (quartile), and a two-tailed, unpaired Student’s t test was applied to compare the means between the two groups (P = 0.05).
Results
Baseline clinical and laboratory characteristics (Supplementary Table 1)
For the baseline clinical characteristics of 29 enrolled patients with TINU syndrome, the median age at diagnosis and follow-up duration were 13.2 (11.6–14.6) years and 38 (24–69) months, respectively. Seven and 22 patients were diagnosed with “definite” or “probable” TINU syndromes, respectively. Seven patients showed general symptoms, such as fever (five patients, 17.2%), weight loss (two patients, 6.9%), rash (two patients, 6.9%), and fatigue (one patient, 3.4%), and 22 patients showed ocular symptoms, such as blurred vision or eye redness (19 patients, 65.5%) and loss of visual acuity (three patients, 10.3%). General symptoms preceded the ocular symptoms in four patients (13.8%) (median 1.4 months), ocular symptoms preceded the general symptoms in 24 patients (82.8%; median 3.2 months), and one patient (3.4%) had concomitant ocular and general symptoms.
For the baseline laboratory characteristics, the median eGFR was 98.1 (77.2–108.8) mL/min/1.73 m2, and nine patients (32.1 %) demonstrated kidney dysfunction (eGFR < 90 mL/min/1.73 m2). The erythrocyte sedimentation rate was elevated in 16 patients (59.3%). The median blood hemoglobin and serum KL-6 levels were 12.8 (12.1–13.5) g/dL and 291.0 (228.5–374.0) U/mL. The serum KL-6 level was elevated in three patients (11.1%). For the urinary findings, pyuria, proteinuria, and glucosuria were observed in 4 (14.8%), 2 (7.4%), and 11 (40.7%) patients, respectively. The median U-β2MG/Cr was 1255.0 (307.0–4037.5) μg/g Cr, and 27 patients (96.4%) showed elevated U-β2MG/Cr [9].
Pathological findings of kidney biopsy
Kidney biopsy was performed at an average of four (1–12) months after diagnosis in seven patients (24%) with persistent kidney dysfunction; of these, five patients received oral corticosteroid therapy for a median of 2.3 (0–7) months. Acute tubulointerstitial nephritis was seen in all patients. Regarding interstitial fibrosis and tubular atrophy, factor 4 score 1 was seen in five patients (71%), and score 2 was seen in two patients (29%). Immunofluorescent staining showed no specific deposition of IgG, IgA, IgM, C1q, C3, and C4 in all patients.
Outcomes at follow-up
The median duration of follow-up after the diagnosis was 38 (24–69) months. The observed changes in median eGFR over the follow-up period were as follows: 98.1 (77.2–108.8) mL/min/1.73 m2 at diagnosis (n = 28), 99.4 (88.6–113.3) mL/min/1.73 m2 at 6 months (n = 25), 106.0 (94.3–115.5) mL/min/1.73 m2 at 1 year (n = 24), 106.0 (100.7–119.8) mL/min/1.73 m2 at 2 years (n = 21), 113.4 (103.8–118.1) mL/min/1.73 m2 at 3 years (n = 15), and 103.7 (91.8–126.6) mL/min/1.73 m2 at 5 years (n = 10) (Fig. 1). The kidney function of the patients had significantly improved at 24 and 36 months after the diagnosis compared to that at diagnosis (p < 0.05). None of the patients required kidney replacement therapy.
The observed changes in the median U-β2MG/Cr over the follow-up period were as follows: 1255 (307–4037.5) μg/g Cr at diagnosis (n = 28), 240 (142.5–580) μg/g Cr at 6 months (n = 26), 155 (87.5–304.8) μg/g Cr at 1 year (n = 12), 140 (85–200) μg/g Cr at 2 years (n = 23), 129 (106–214.5) μg/g Cr at 3 years (n = 11), and 140 (72.5–227.5) μg/g Cr at 5 years (n = 10) (Fig. 2). The U-β2MG/Cr at 6 months and 1, 2, 3, and 5 years had significantly improved compared to that at diagnosis. On the other hand, 16 patients (72.7%) needed a long period for normalization of U-β2MG/Cr, as these patients still had elevated U-β2MG/Cr at 2 years after diagnosis.
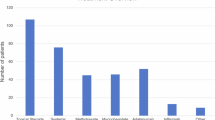
Regarding the clinical course of uveitis, the proportions of patients receiving treatment with topical/oral corticosteroid or oral methotrexate were 100% (n = 27) at diagnosis, 96.3% at 6 months (n = 27), 92.3% at 1 year (n = 26), 90.0% at 2 years (n = 20), 71.4% at 3 years (n = 14), and 50.0% at 5 years (n = 10). Statistically, the number of patients requiring treatment for uveitis was significantly lower at 36 months than at the time of diagnosis. The treatments administered were as follows: topical corticosteroid only (96.3% at diagnosis, 59.3% at 6 months, 61.5% at 1 year, 65.0% at 2 years, 57.2% at 3 years, 50.0% at 5 years), topical and oral corticosteroids (3.7% at diagnosis, 29.6% at 6 months, 26.9% at 1 year, 20.0% at 2 years, 7.1% at 3 years, 0% at 5 years), and topical and oral corticosteroids as well as oral methotrexate (0% at diagnosis, 7.4% at 6 months, 3.9% at 1 year, 5.0% at 2 years, 7.1% at 3 years, 0% at 5 years) (Fig. 3). At the time of diagnosis, the visual acuity of each patient was examined, and three patients had decreased visual acuity. The other patients had normal visual acuity during the follow-up period. One of the three patients with decreased visual acuity at the time of diagnosis had adhesions and cataracts that did not improve during the follow-up period. The other two patients with decreased visual acuity at the time of diagnosis showed improvement within 6 months.
Changes in the proportion of pediatric patients with tubulointerstitial nephritis and uveitis syndrome (expressed in percentage) receiving various treatments, such as topical corticosteroids (TCS), oral corticosteroids (OCS), and oral methotrexate (MTX), during the follow-up period. The percentage of patients receiving treatment for uveitis decreased gradually after 36 months from diagnosis. *P < 0.05 (vs. at diagnosis)
Based on the U-β2MG/Cr at the time of diagnosis, we classified 28 patients into the following two groups: group A (n = 10) comprised patients with higher U-β2MG/Cr (> 2000 μg/g Cr), and group B (n = 18) comprised patients with lower U-β2MG/Cr (<2000 μg/g Cr) (Table 1). The eGFR level at diagnosis and at 12 months after diagnosis was significantly lower in group A than in group B; however, no significant difference in kidney function between groups A and B was observed at 24 months after diagnosis. The recovery period for normalization of kidney function, which is the time required for eGFR to reach > 90 mL/min/1.73 m2, was significantly longer in group A [21.4 (0–70) months] than in group B [1.6 (0–24) months] (P = 0.0009). The treatment period for uveitis was not significantly different between the two groups [group A: 37.5 (26.5–52) months; group B: 26 (16–46) months, P = 0.5352]. In this study, there was no significant difference in the duration of treatment of uveitis between patients with eGFR of > 90 mL/min/1.73 m2 and eGFR of < 90 mL/min/1.73 m2 at the time of diagnosis (P = 0.725) and between those with urinary β2MG/Cr of > 2000 μg/g Cr and β2MG/Cr of < 2000 μg/g Cr at diagnosis (P = 0.5352). Furthermore, there was also no difference in the severity of nephritis between patients in which the duration of treatment for uveitis was > 36 months and those that were treated in < 36 months (P = 0.253). Therefore, in this study, we could not find any correlation between the severity of nephritis, such as elevated urinary β2MG/Cr and decreased eGFR, and the severity of uveitis, such as the duration of treatment for uveitis.
Discussion
This long-term study highlights several significant points. First, our patients were diagnosed with TINU syndrome mostly due to their ocular symptoms (24 patients, 82.8%) rather than due to their systemic symptoms (four patients, 14.3%). In addition, they demonstrated elevated U-β2MG/Cr compared to the median value of age-matched U-β2MG/Cr [10], which has been reported as a sensitive diagnostic marker for TINU syndrome [7, 14]. These clinical and laboratory features at diagnosis suggest the importance of considering TINU syndrome as a differential diagnosis when low-molecular weight proteinuria is observed in children with uveitis, even if there were no systemic symptoms as previously reported [7].
Second, our study clarified that kidney function was finally normalized in all patients during the median observation period of 38 months. Some recent reports of adult TINU patients describe that approximately 80% of patients experienced kidney dysfunction (chronic kidney disease stages G3–G4) at 12 months after diagnosis [4, 15]. However, our study demonstrates that a long period of kidney function normalization (25 months) was needed compared to previous reports [5, 6, 14], which may be due to differences in the number of patients analyzed and the relatively worse kidney function at diagnosis in our study patients than in the patients of a previous study [14]. Our study suggests that pediatric patients with TINU syndrome have a good kidney prognosis and that it is necessary to perform long-term follow-up, especially in patients with kidney dysfunction at the time of diagnosis.
Third, we observed the association between higher U-β2MG/Cr (> 2000 μg/g Cr) at diagnosis and longer duration for normalization of kidney function. These results were comparable to those of previous reports showing that the elevation of U-β2MG/Cr suggests continuous inflammation of the proximal tubules [16]. Therefore, especially in patients with high U-β2MG/Cr, we should recognize the necessity of long-term observation of kidney function normalization.
Finally, the improvement in ocular symptoms required a longer duration to achieve than that of systemic symptoms or kidney function. Most patients exhibited ocular symptoms in this study, and half of these patients needed to continue uveitis treatment for 5 years after the diagnosis. These results were consistent with previous reports demonstrating that uveitis in TINU has a prolonged disease course [2, 3, 14, 17]. Although not statistically significant, we observed the association between higher Uβ2MG/Cr at diagnosis and longer treatment period for uveitis. One patient who had decreased visual acuity at the time of diagnosis had adhesions and cataracts that did not improve during the follow-up period. Therefore, we should consider the possibility of uveitis and consult an ophthalmologist as soon as possible when considering the differential diagnosis of tubulointerstitial nephritis.
This study has some limitations. Given that the present investigation is a retrospective study, some patients could not be included due to the unavailability of some data or unexpected interruptions in patient follow-up. Moreover, the treatment indications, as well as the selection and dose of the therapeutic drugs, were not unified. In addition, the characteristics of our patients may be influenced by selection bias because our facility has been treating patients with this disease for many years [18, 19]. We carefully perform medical examinations to investigate ocular symptoms; hence, in our facility, many patients with TINU syndrome have been diagnosed.
In conclusion, this long-term study of children with TINU syndrome revealed that (1) most patients exhibited ocular symptoms with low-molecular weight proteinuria, but without systemic symptoms; (2) children with TINU syndrome demonstrated a good prognosis in terms of long-term clinical and laboratory characteristics; (3) severe low-molecular weight proteinuria at diagnosis was associated with longer duration of kidney function improvement; and (4) uveitis has a much longer treatment period than tubulointerstitial nephritis.
References
Dobrin RS, Vernier RL, Fish AL (1975) Acute eosinophilic interstitial nephritis and renal failure with bone marrow-lymph node granulomas and anterior uveitis. A new syndrome. Am J Med 59:325–333. https://doi.org/10.1016/0002-9343(75)90390-3
Clive DM, Vanguri VK (2018) The syndrome of tubulointerstitial nephritis with uveitis (TINU). Am J Kidney Dis 72:118–128. https://doi.org/10.1053/j.ajkd.2017.11.013
Mandeville JT, Levinson RD, Holland GN (2001) The tubulointerstitial nephritis and uveitis syndrome. Surv Ophthalmol 46:195–208. https://doi.org/10.1016/s0039-6257(01)00261-2
Tan Y, Yu F, Qu Z, Su T, Xing GQ, Wu LH, Wang FM, Liu G, Yang L, Zhao MH (2011) Modified C-reactive protein might be a target autoantigen of TINU syndrome. Clin J Am Soc Nephrol 6:93–100. https://doi.org/10.2215/CJN.09051209
Saarela V, Nuutinen M, Ala-Houhala M, Arikoski P, Ronnholm K, Jahnukainen T (2013) Tubulointerstitial nephritis and uveitis syndrome in children: a prospective multicenter study. Ophthalmology 120:1476–1481. https://doi.org/10.1016/j.ophtha.2012.12.039
Jahnukainen T, Ala-Houhala M, Karikoski R, Kataja J, Saarela V, Nuutinen M (2011) Clinical outcome and occurrence of uveitis in children with idiopathic tubulointerstitial nephritis. Pediatr Nephrol 26:291–299. https://doi.org/10.1007/s00467-010-1698-4
Takemura T, Okada M, Hino S, Fukushima K, Yamamoto S, Miyazato H, Maruyama K, Yoshioka K (1999) Course and outcome of tubulointerstitial nephritis and uveitis syndrome. Am J Kidney Dis 34:1016–1021. https://doi.org/10.1016/S0272-6386(99)70006-5
Tanaka H, Suzuki K, Nakahata T, Tateyama T, Waga S, Ito E (2001) Repeat renal biopsy in a girl with tubulointerstitial nephritis and uveitis syndrome. Pediatr Nephrol 16:885–887. https://doi.org/10.1007/s004670100697
Hibi Y, Uemura O, Nagai T, Yamakawa S, Yamasaki Y, Yamamoto M, Nakano M, Kasahara K (2015) The ratios of urinary beta2-microglobulin and NAG to creatinine vary with age in children. Pediatr Int 57:79–84. https://doi.org/10.1111/ped.12470
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, Yamagata K, Tomino Y, Yokoyama H, Hishida A, Collaborators developing the Japanese equation for estimated GFR (2009) Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis 53:982–992. https://doi.org/10.1053/j.ajkd.2008.12.034
Fisher DA (2000) The importance of early management in optimizing IQ in infants with congenital hypothyroidism. J Pediatr 136:273–274. https://doi.org/10.1067/mpd.2000.104286
Suzuki K, Tanaka H, Ito E, Waga S (2004) Repeat renal biopsy in children with severe idiopathic tubulointerstitial nephritis. Pediatr Nephrol 19:240–243. https://doi.org/10.1007/s00467-003-1362-3
Yanagihara T, Kitamura H, Aki K, Kuroda N, Fukunaga Y (2009) Serial renal biopsies in three girls with tubulointerstitial nephritis and uveitis syndrome. Pediatr Nephrol 24:1159–1164. https://doi.org/10.1007/s00467-009-1142-9
Kanno H, Ishida K, Yamada W, Shiraki I, Murase H, Yamagishi Y, Mochizuki K (2018) Clinical and genetic features of tubulointerstitial nephritis and uveitis syndrome with long-term follow-Up. J Ophthalmol 2018:4586532. https://doi.org/10.1155/2018/4586532
Li C, Su T, Chu R, Li X, Yang L (2014) Tubulointerstitial nephritis with uveitis in Chinese adults. Clin J Am Soc Nephrol 9:21–28. https://doi.org/10.2215/CJN.02540313
Zeng X, Hossain D, Bostwick DG, Herrera GA, Zhang PL (2014) Urinary β2-microglobulin is a good indicator of proximal tubule injury: a correlative study with renal biopsies. J Biomark 2014:492838. https://doi.org/10.1155/2014/492838
Pakzad-Vaezi K, Pepple KL (2017) Tubulointerstitial nephritis and uveitis. Curr Opin Ophthalmol 28:629–635. https://doi.org/10.1097/ICU.0000000000000421
Kase S, Kitaichi N, Namba K, Miyazaki A, Yoshida K, Ishikura K, Ikeda M, Nakashima T, Ohno S (2006) Elevation of serum Krebs von den Lunge-6 levels in patients with tubulointerstitial nephritis and uveitis syndrome. Am J Kidney Dis 48:935–941. https://doi.org/10.1053/j.ajkd.2006.09.013
Goda C, Kotake S, Ichiishi A, Namba K, Kitaichi N, Ohno S (2005) Clinical features in tubulointerstitial nephritis and uveitis (TINU) syndrome. Am J Ophthalmol 140:637–641. https://doi.org/10.1016/j.ajo.2005.04.019
Acknowledgements
We are grateful for the work of the past and present members of our laboratory.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in studies involving human participants were reviewed and approved by the Institutional Review Board of Hokkaido University Hospital and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Table 1
Baseline clinical and laboratory characteristics of the 29 enrolled children with TINU syndrome. Diagnostic criteria of D; Definite and P; probable. Gender F; Female, Gender M; Male. ESR; erythrocyte sedimentation rate (normal male range, 2-10 mm/h; normal female range 3-15 mm/h), Hb; blood hemoglobin, KL-6; sialylated carbohydrate antigen KL-6 (normal range < 500 U/mL), Pyuria (in urinary sediment 5 white blood cells (WBCs), > 400 times field of vision), PRO; proteinuria (> 1+ by dipstick method),GLU; glucosuria (> 1 ± by dipstick). N/A; not available. (PPTX 55.5 kb).
Rights and permissions
About this article
Cite this article
Hayashi, A., Takahashi, T., Ueda, Y. et al. Long-term clinical characteristics and renal prognosis of children with tubulointerstitial nephritis and uveitis syndrome. Pediatr Nephrol 36, 2319–2325 (2021). https://doi.org/10.1007/s00467-021-04956-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-021-04956-6